Back to Journals » Journal of Pain Research » Volume 13
Comparing Analgesic Effect of Intravenous Fentanyl, Femoral Nerve Block and Fascia Iliaca Block During Spinal Anesthesia Positioning in Elective Adult Patients Undergoing Femoral Fracture Surgery: a Randomized Controlled Trial
Authors Bantie M, Mola S , Girma T , Aweke Z, Neme D, Zemedkun A
Received 17 September 2020
Accepted for publication 7 November 2020
Published 26 November 2020 Volume 2020:13 Pages 3139—3146
DOI https://doi.org/10.2147/JPR.S282462
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Robert B. Raffa
Melaku Bantie,1 Simeneh Mola,2 Timsel Girma,2 Zemedu Aweke,2 Derartu Neme,2 Abebayehu Zemedkun2
1Debre Berhan University, College of Medicine and Health Science, Debre Birhan, Ethiopia; 2Dilla University, College of Medicine and Health Science, Dilla, Ethiopia
Correspondence: Simeneh Mola
Dilla University, College of Medicine and Health Science, Dilla 0419/13, Ethiopia
Tel +251 901091414
Email [email protected]
Background: Femoral fracture is the most painful bone injury and performing spinal anesthesia is extremely challenging due to very poor positioning unless we have a very good mode of analgesia. Intravenous strong opioids are commonly used but to date nerve blocks are also being utilized. The reliability and effectiveness of the aforementioned methods are not conclusive to practice worldwide. The objective of the study was to compare the analgesic effect of intravenous fentanyl, femoral nerve block (FNB) and fascia iliaca block (FICB) during positioning patients with femoral fracture for spinal anesthesia.
Methods: A randomized controlled trial study was conducted on 72 elective adult patients with femoral fracture aged 18– 65 years and ASA I and II those were allocated randomly into three groups. The intravenous fentanyl (IVFE) group received 1μg/kg IV fentanyl, FNB group received nerve stimulator guided FNB with 30 mL of 1% lidocaine with adrenaline and FICB group received FICB with 30 mL of 1% lidocaine with adrenaline. Pain intensity in numeric rating score (NRS), time to perform spinal anesthesia, quality of positioning and patient acceptance were assessed. SPSS version 26 and Kruskal–Wallis test were used to analyze data and p value < 0.05 was considered significant.
Results: NRS Pain score during positioning was significantly lower in FNB and FICB groups than IVFE group [median (IQR)]; 2 (1– 2.5), 2 (2– 3)) vs. 3 (3– 4) respectively; P< 0.001 and P=0.001. However, FNB and FICB groups were not significantly different with (P=1.000). Time to perform spinal anesthesia was significantly longer in IVFE group 9.5 (9– 10) minutes than both FNB and FICB groups 7 (6– 8), 8 (6– 8) respectively, P< 0.001. The quality of positioning was significantly lower in the IVFE group than both FNB and FICB groups (P< 0.001).
Conclusion: Preoperative FNB and FICB reduce pain score during positioning, shorten time to perform spinal anesthesia, better patient positioning and higher patient acceptance in a patient undergoing elective femoral bone fracture surgery.
Trial Registration: Pan African Clinical Trial Registry, PACTR202006669166858, registered on June 19, 2020. https://pactr.samrc.ac.za/TrialDisplay.aspx?TrialID=12127.
Keywords: femoral nerve block; FNB, fascia iliaca block; FICB, intravenous fentanyl, spinal anesthesia positioning, femoral fracture
Background
Femoral fracture is relatively common with an annual incidence of around 2.9 million worldwide, with the peak incidence of 34% between 15 and 44 years followed by 29% and 21% in between 5 and14 years and older than 60 years respectively.1
Spinal anesthesia is commonly utilized in lower extremity orthopedic surgery and has many advantages including easily performed, effective, avoiding airway related complications, reducing the incidence of deep venous thrombosis (DVT), reducing hospital mortality, minimizing hospitalization, and providing postoperative analgesia.2–4 It has well-acknowledged beneficial effects of reducing pain, reduced opioid consumption, and improved quality of early recovery.5
Despite the aforementioned advantages, the technique of performing spinal anesthesia in patients with a femoral fracture is difficult due to poor positioning secondary to pain. Correct positioning during spinal anesthesia is the prerequisite in order to perform spinal anesthesia successfully. However, it is extremely painful, causing major patient distress, accompanied by well-known physiological squeal such as sympathetic activation causing tachycardia, hypertension, and increased cardiac work that may compromise high-risk cardiac patients.6 Limb immobility and extreme pain are the deterrents for ideal positioning for this procedure.7
Most of the time anesthetists administer opioid or non-steroidal anti-inflammatory drugs (NSAID) for better tolerance of pain during positioning for spinal anesthesia.8–10 However, they have relatively high complications and clinicians are searching for other ways of minimizing pain. Nowadays studies propose that nerve blocks mainly femoral nerve block (FNB) minimize this devastating pain and increase patient safety, shorten time to perform spinal anesthesia, and provide postoperative analgesia11,12 without significant side effects.10,13
Today IV fentanyl, FNB and FICB are proposed for perioperative analgesia in patients with a femoral fracture in order to facilitate spinal anesthesia by preventing pain secondary to positioning. But available literatures are not conclusive or no single best analgesic technique that is proved to be absolutely effective, fast onset, easy to apply, minimum side effect and accessible that will apply in patients with femoral fracture.14,15 Therefore, this study aimed to compare analgesic effect of intravenous fentanyl, FNB and fascia iliaca compartment block (FICB) during positioning patients with femoral fracture for spinal anesthesia. The severity of pain in numeric rating score (NRS), time taken to perform spinal anesthesia, quality of patient positioning, and patient satisfaction were the specific objectives of our study.
Methods
This institutional-based, parallel, single-blinded, and randomized controlled trial study was conducted at Hawassa University Comprehensive Specialized Hospital, Hawassa, which is located at 280 Km south of Addis Ababa, from June 21 to August 19, 2020.
This study was conducted in accordance with declaration of Helsinki. Ethical approval was obtained from the Dilla University institutional review board and the study was registered on Pan African Clinical Trial Registry with a unique identification number of PACTR202006669166858. Verbal and written informed consents were taken from each participant.
ASA class I, II, and Age between 18–65 years patients who undergo orthopedic surgery for femoral fracture under spinal anesthesia at HUCSH were included by systematic random sampling technique. By estimating expected cases during study period from situational analysis a skip interval determined to be 2. The order of patients on the schedule list was considered as their respective serial numbers, and 1 patient from the first 2 patients were selected by simple random sampling method or lottery method. Then, similar skipping interval and pattern were followed for the next consecutive patients until we accomplished the sample size in each group. Patients having allergy history to lidocaine or fentanyl, Contraindication to spinal anesthesia (patient refusal, bleeding problem), fracture other than the femur, Bilateral femoral fracture, History of chronic pain, History of an opioid within 12hrs preoperatively, Body mass index (BMI) > 35 kg/m2), impaired cognition, Infection on cite of the block and failed block were excluded from the study.
Although comparison between three interventions (FNB, FICB and IVF) for positioning during spinal anesthesia is not novel study, there was no study which compared all of the three interventions at a time. Therefore, the sample size was estimated by conducting a pilot study of 21 patients or 7 patients per group (we use a similar protocol, blinding, controlling, and data collection tool to the main study). All outcome variables were considered for sample size calculation and the largest sample size obtained from time to perform spinal anesthesia. The result showed that time to perform spinal anesthesia (mean± SD) of 9.1±1.35, 7.6±1.40, and 8.3±1.80 minutes for IVFE, FNB, and FICB groups respectively. Using G-power (version 3.0.9.2) software and given that α = 0.05, 80% power, calculated pooled standard deviation Spooled=1.53 and effect size of d=0.401 then sample size was estimated to be 66 and with an account of 10% for dropout, the total sample size was determined to be 72 or 24 participants in each group.
Participants were assigned to one of the three groups in a 1:1:1 ratio and randomization was conducted by drawing one of the three sealed opaque envelopes containing either ‘IVFE’, ‘FNB’ or ‘FICB’ by anesthesia provider. The investigators prepared the sealed envelopes and incorporated all necessary information about the patients in addition to the type of interventions. A clear explanation about the procedures was made before allocation. In order to maintain blinding, the data collector was not allowed to be available in the operating room during the intervention.
Data Collection Procedure
The night before surgery, patients were evaluated for eligibility and informed consent was taken after proper explanation about the study, interventions, and measurements. As the patient arrives at the operation room, standard monitoring such as electrocardiography, pulse-oximeter, and Non-invasive blood pressure measurement were attached and recorded every five minutes. An infusion of lactated Ringer’s solution 20mL/kg was given and all patients were supplied with oxygen (2L/min) via a nasal cannula. NRS pain score before the intervention was recorded when the patient lied on the operation table.
IVFE group received fentanyl 1μg/kg IV, and 5 minutes later, they were placed in the sitting position to perform spinal anesthesia. FNB and FICB groups received FNB and FICB with 30 mL of 1% lidocaine with adrenaline solution respectively and 15 minutes later, they were placed in the same position as group IVFE patients. FNB was performed by nerve stimulator technique on supine position; the femoral artery pulse is palpated at the level of the inguinal ligament. After cleaning the area with alcohol and iodine a short (5-cm) insulated needle was inserted at a 45° angle to the skin in a cephalad direction until a distinct quadriceps twitch (patella dancing) is elicited with a current between 0.5mA and 0.2mA then careful aspiration was performed and 30mL of 1% lidocaine with adrenaline solution was injected. FICB was also performed once the inguinal ligament and femoral artery pulse are identified; the length of the inguinal ligament was divided into thirds. Two centimeters distal to the junction of the middle and outer thirds, a short, blunt-tipped needle was inserted in a slightly cephalad direction after cleaning with alcohol and iodine. As the needle passes through the two layers of fascia in this region (fascia lata and fascia iliaca), two “pops” were felt. Once the needle has passed through the fascia iliaca, careful aspiration was performed and 30mL of 1% lidocaine with adrenaline solution was injected.
Pain intensity was assessed using NRS and documented at 2 minutes after intervention for IVFE group, at (2, 5 and 10) minutes after nerve blocks and also during positioning for all groups. If the patient fells significant pain and not able to position due to pain additional analgesia will be given and the patient will be excluded from the study. However, all of patient data before additional analgesia will be recorded and analyzed. Intraoperative adverse events such as vomiting, hypotension, bradycardia and respiratory depression will be recorded and managed according to the protocol.
Postoperative pain was managed based on hospital standard of care including multimodal analgesia starting from paracetamol and NSAIDs to strong opioids. After completion of the surgery, patients were asked if they were comfortable with pain management done for positioning to answered either “Yes“ or “No” and the answer recorded as patient acceptance.
The primary outcomes of this study were pain NRS score (before and after) intervention and during positioning. Secondary outcomes were time to perform spinal anesthesia, patient acceptance, quality of patient positioning, and intervention associated complications.
The statistical analyses were performed using SPSS version 26 software package. Data distribution for continuous data was evaluated by Shapiro Wilk H-test. Homogeneity of variance was assessed by Leven’s test. For ordinal and asymmetric numeric data, the Kruskal–Wallis H-test was used, and post hoc analysis was done with the Mann–Whitney U-test using Holm’s sequential Bonferroni method to adjust for multiple comparisons. Symmetric numeric data were analyzed by using one way ANOVA. Data were described in terms of mean ± SD, median (Interquartile range) and numbers or percentages as appropriate. Nominal data were analyzed by using the chi-square test and post hoc analysis was done by filtering one group at a time and running a chi-square test with Bonferroni correction for patient acceptance. A p value<0.05 was considered statistically significant. The study was reported based on the CONSORT 2010 guideline.
Operational Definitions
Quality of Patient Positioning
(0 = not satisfactory, 1 = satisfactory, 2 = good, and 3 = optimal by the anesthetist performing spinal anesthesia).
Time to Perform Spinal Anesthesia
Time in minutes measured from the start of positioning maneuvers to the spinal needle removal.
Patient Acceptance
After completion of surgery each patient were asked “are you comfortable with pain management done before positioning?” ‘Yes” or “No”.
Results
A total of 91 patients were assessed for eligibility and 72 were included in the study (Figure 1). Nineteen patients were excluded from the study because seventeen of them not meet the inclusion criteria and the remaining two patients declined to participate. All groups of patients were comparable regarding with demographic data, type of fracture, the time interval from fracture to surgery, and intervention-related complications (Table 1).
 |
Table 1 Demographic Characteristics, Surgical and Anesthesia Data of Patients with Femoral Fracture at Hawassa University Comprehensive Specialized Hospital |
 |
Figure 1 Consort flow diagram of patient’s enrollment. |
Pain Score Between the Three Groups
Numeric rating pain scales score before the intervention and at two minutes after intervention did not differ significantly between groups (P= 0.882 and 0.229) respectively after the Kruskal–Wallis H-test except during positioning. Post hoc analysis with Mann–Whitney U-test using Bonferroni correction showed that pain score during positioning was significantly lower in FNB and FICB groups than IVFE group [median (IQR)]; 2(1–2.5), 2(2–3)) vs. 3(3–4) respectively; P<0.001 and P=0.001 for FNB and FICB against IVFE respectively. However, FNB and FICB groups were not significantly different with P=1.00 (Figure 2).
Time to Perform Spinal Anesthesia
Kruskal–Wallis H-test and Mann–Whitney U-test using Holm’s sequential Bonferroni method for post hoc analysis showed that; time to perform spinal anesthesia was significantly longer in IVFE group median and interquartile range (9.5(9–10) than both FNB and FICB groups (7(6–8), 8(6–8) minutes respectively) P<0.001 and P=0.002 for IVFE against FNB and FICB respectively but no significant difference was observed between FICB and FNB groups P=0.381 (Table 2).
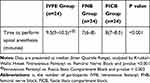 |
Table 2 Time to Perform Spinal Anesthesia of Patients with Femoral Fracture at Hawassa University Comprehensive Specialized Hospital |
Quality of Positioning
Using Kruskal–Wallis H-test and post hoc analysis with Mann–Whitney U-test and Holm’s sequential Bonferroni method showed that; quality of patient positioning was significantly lower in IVFE median and IQR (2(1–2)) group than both FNB and FICB groups (2(2–3) and 2(2–3) respectively, P<0.004 and P=0.011 for IVFE against FNB and FICB respectively, but no significant difference was observed between FNB and FICB groups P=1.000 (Table 3).
 |
Table 3 Quality of Positioning of Patients with Femoral Fracture at Hawassa University Comprehensive Specialized Hospital |
Patient Acceptance
Patient acceptance was significantly different between groups after the chi-square test at P=0.001, and post hoc analysis was done by filtering one group at a time with chi-square analysis and adjusting P-value using Bonferroni correction to control type 1 error showed a significantly lower patient acceptance in IVFE (41.7%) group than both FNB and FICB groups (87.5% and 79%) respectively, P=0.001 and P=0.008 for FNB and FICB against IVFE respectively. However, no significant difference was noticed between FNB and FICB groups P=0.439 (Figure 3).
 |
Figure 3 Patient acceptance. |
Complications Recorded in Operation Room
There were no procedure-related complications like hypotension, bradycardia, adverse systemic toxicity, vomiting, respiratory depression, nerve injury and bleeding at the site of the block (nerve blocks only).
Discussion
To our knowledge, this single-blinded, randomized controlled trial is the first study directly comparing the effect of intravenous fentanyl, FNB under nerve stimulator, and FICB to reduce pain during positioning patients with a femoral fracture for spinal anesthesia.
In our study all interventions showed a reduction in NRS pain score. However, in contrast, both FNB and FICB were more effective in providing superior analgesia than IVFE as evidenced by lower pain score during positioning, shorter time to perform spinal anesthesia, greater quality of positioning and higher patient acceptance. And there is no significant difference between FNB and FICB regarding with the above-mentioned advantages over IVFE. Previous studies, showed comparable results even if there is some methodological difference including type and amount of local anesthetics used for blocks, as discussed below.
The present study shows that FNB and FICB were effective in reducing pain during positioning than IVFE [median (IQR)]; 2(1–2.5), 2(2–3)) vs. 3(3–4) respectively, which is comparable with recent studies done by Purohit et al,17 comparing placebo-controlled FNB that showed VAS score of (mean± SD (8.25±0.36,1.47±0.16)) respectively and Hsu et al,16 comparing FNB and intravenous opioids. Madabushi et al,13 which compares FICB to IVFE also showed similar results to the present study. However pain during positioning was higher in the fentanyl group than the present study, this effect may be explained by the fact that they used a small dose of fentanyl (0.5µg/kg) than 1µg/kg in our study, despite added 0.5µg/kg fentanyl in 18 out of 30 patients.
In contrast to this study, Ghimire et al,15 reported that, FICB was more effective in reducing pain than FNB which is against the present study. The result may be explained by the fact that, lower volume (15mL) of lidocaine is used in the FNB group, and isolated proximal fracture occasionally innervated by sciatic and superior gluteal nerves which are not affected by FNB as shown by the increase VAS score in this group. They found a very low VAS score for the FICB group and the possible reason might be very low baseline mean VAS score (around 3) than above 6 (median) in the present study and also longer waiting time (20 minutes) to position for spinal anesthesia, that increases the quality of FICB.
In our study, FNB and FICB were effective in reducing the time required to perform spinal anesthesia (7(6–8) and 8(7–8.5)) than IVFE (9.5(9–10.5)) in minutes which is comparable with previous studies by Madabushi et al,13 (7.30± 3.72 and 9.77± 3.20) minutes and Purohit et al,17 for combined spinal-epidural anesthesia (13±0.5 vs. 19±0.4) minutes. Even though it is hard to compare these results because of different techniques of central neuraxial block and method of analysis but still we can infer that FNB or FICB requires a shorter time to perform spinal or combined spinal-epidural anesthesia than either placebo or IVFE.
In the present study quality of positioning was higher in patients with FNB or FICB 2(2–3) for both groups than IVFE 2(1–2) which is also comparable to previous studies by Purohit et al,17 (2.8±1.3, 1.4±0.2), Madabushi et al,13 (2.06±078, 1.25±0.85) and Hsu et al.16
This study shows that patient acceptance was greater in patients with FNB and FICB than IVFE (87.5%, 79%, and 41.7%) respectively. This is in line with previous studies done by Purohit et al,17 (90%, 20%) for FNB vs. non FNB groups and Hsu et al,16 also showed regional nerve blocks provide greater patient acceptance than intravenous opioids.
The present study is comparable to many studies that showed peripheral nerve blocks; FNB or FICB were more effective in reducing pain during positioning, shorten time to perform central neuraxial block, and increase the quality of positioning than placebo or intravenous opioids including fentanyl, alfentanil and nalbuphine.12,13,17,18
FNB and FICB can be used for a longer time by placing a catheter to the site for additional bolus, continuous infusion of local anesthetics or using long acting local anesthetics.19 Pre-spinal FICB or FNB relax quadriceps muscle thus provide superior analgesia for positioning, a better quality of positioning, and require shorter time to perform spinal anesthesia.
In this study, there is no documented complication like hypotension, vomiting, bradycardia, and respiratory depression which is similar to studies done by Kacha et al,12 and Purohit et al,17 on their placebo-controlled FICB and FNB randomized clinical trials respectively.
Today peripheral nerve blocks are recommended for positioning patients with a femoral fracture for spinal anesthesia and our study shows that FICB is as effective as nerve stimulator guided FNB that allows clinicians, who have no access for nerve stimulator can use FICB under landmark technique.
There are limitations on this study. Despite being the most popular approach in resource limited countries, Use of blind land mark technique for performance of FICB is the major limitation of this study. Another limitation of the study is the measurement tool we preferred for quality of positioning is somewhat subjective.
Conclusion and Recommendation
Preoperative FNB and FICB reduce pain score during positioning, shorten time to perform spinal anesthesia, better patient positioning, and higher patient acceptance in a patient undergoing elective femoral bone fracture surgery. We recommend FNB and FICB for spinal anesthesia positioning in a patient undergoing elective femoral bone fracture surgery. Nonetheless, it is essential to carry out further high power ultrasound-guided studies.
Abbreviation
ASA, American Society of Anesthesiologists; DVT, deep venous thrombosis; FICB, fascia iliaca compartment block; FNB, femoral nerve block; HR, heart rate; HUCSH, Hawassa University Comprehensive Specialized Hospital; IVFE, intravenous fentanyl; LAST, local anesthetic systemic toxicity; NRS, numeric rating scale; NS, nerve stimulator; NSAID, non-steroidal anti inflammatory drugs; RCT, randomized controlled trial; SPSS, Statistical Package for the Social Sciences; VAS, visual analog scale.
Data Sharing Statement
The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
Ethical approval was secured from Dilla University institutional review board. Verbal and written informed consent obtained from each respondent before actual data collection. Issues of confidentiality were maintained by removing any identifiers from the questionnaire. The participant were informed their right to participate and leave the study at any point in time.
Consent for Publication
Not applicable
Acknowledgment
We want to acknowledge Dilla University who funded and supported us in the development of this research paper.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
Dilla University has funded the research project. The sponsor has no any role other than enhancing staff research and academic activity. The sponsor didn’t take part in any action of the research project other than funding.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Agarwal-Harding KJ, Meara JG, Greenberg SL, Hagander LE, Zurakowski D, Dyer GS. Estimating the global incidence of femoral fracture from road traffic collisions: a literature review. JBJS. 2015;97(6):e31. doi:10.2106/JBJS.N.00314
2. Pu X, Sun J-M. General anesthesia vs spinal anesthesia for patients undergoing total-hip arthroplasty: A meta-analysis. Medicine. 2019;98:16. doi:10.1097/MD.0000000000014925
3. Van Waesberghe J, Stevanovic A, Rossaint R, Coburn M. General vs. neuraxial anaesthesia in hip fracture patients: a systematic review and meta-analysis. BMC Anesthesiol. 2017;17(1):87.
4. Lončarić-Katušin M, Mišković P, Lavrnja-Skolan V, Katušin J, Bakota B, Žunić J. General versus spinal anaesthesia in proximal femoral fracture surgery–treatment outcomes. Injury. 2017;48:S51–S5. doi:10.1016/S0020-1383(17)30740-4
5. Johnson MZ J. Perioperative regional anaesthesia and postoperative longer-term outcomes. F1000Research. 2016;5.
6. Diakomi MPM, Mela A, Kouskouni E, Makris A. Preoperative fascia iliaca compartment block for positioning patients with hip fractures for central nervous blockade: a randomized trial. Reg Anesth Pain Med. 2014;39(5):394–398. doi:10.1097/AAP.0000000000000133
7. Jadon A, Kedia SK, Dixit S, Chakraborty S. Comparative evaluation of femoral nerve block and intravenous fentanyl for positioning during spinal anaesthesia in surgery of femur fracture. Indian J Anaesth. 2014;58(6):705–708. doi:10.4103/0019-5049.147146
8. Benyamin RTA, Datta S, Buenaventura R, Adlaka R, Sehgal NE. Opioid complications and side effects. Pain Physician. 2008;11:S105–20.
9. Sandberg OAP. Different effects of indomethacin on healing of shaft and metaphyseal fractures. Acta Orthop. 2015;86(2):243–247. doi:10.3109/17453674.2014.973328
10. Sia S, Pelusio F, Barbagli R, Rivituso C. Analgesia before performing a spinal block in the sitting position in patients with femoral shaft fracture: a comparison between femoral nerve block and intravenous fentanyl. Anesth Analg. 2004;99(4):1221–1224. doi:10.1213/01.ANE.0000134812.00471.44
11. Iamaroon A, Raksakietisak M, Halilamien P, Hongsawad J, Boonsararuxsapong K. Femoral nerve block versus fentanyl: analgesia for positioning patients with fractured femur. Local Reg Anesth. 2010;3:21. doi:10.2147/LRA.S8600
12. Kacha NJ, Jadeja CA, Patel PJ, Chaudhari HB, Jivani JR, Pithadia VS. Comparative study for evaluating efficacy of fascia iliaca compartment block for alleviating pain of positioning for spinal anesthesia in patients with hip and proximal femur fractures. Indian J Orthop. 2018;52(2):147–153.
13. Madabushi R, Rajappa GC, Thammanna PP, Iyer SS. Fascia iliaca block vs intravenous fentanyl as an analgesic technique before positioning for spinal anesthesia in patients undergoing surgery for femur fractures-a randomized trial. J Clin Anesth. 2016;35:398–403. doi:10.1016/j.jclinane.2016.09.014
14. Faiz SHR, Derakhshan P, Imani F, Alebouyeh MR, Rahimzadeh P, Memarian A. A comparative study on the effect of femoral nerve block (FNB) versus fascia iliaca compartment block (FIC) on analgesia of patients with isolated femoral shaft fracture under spinal anesthesia. Trauma Monthly. 2018;23(5).
15. Ghimire A, Bhattarai B, Koirala S, Subedi A. Analgesia before performing subarachnoid block in the sitting position in patients with proximal femoral fracture: a comparison between fascia iliaca block and femoral nerve block. Kathmandu Univ Med J. 2015;13:152–155. doi:10.3126/kumj.v13i2.16789
16. Hsu Y-P, Hsu C-W, Chu KCW, et al. Efficacy and safety of femoral nerve block for the positioning of femur fracture patients before a spinal block - A systematic review and meta-analysis. PLoS One. 2019;14(5):e0216337–e. doi:10.1371/journal.pone.0216337
17. Purohit S, Ejjapuredi S, Badami RN. Positioning for regional anesthesia in femur fracture surgeries: how effective is femoral nerve block? A randomised control study. Int J Res Med Sci. 2017;5(8):6.
18. Singh AP, Kohli V, Bajwa SJS. Intravenous analgesia with opioids versus femoral nerve block with 0.2% ropivacaine as preemptive analgesic for fracture femur: A randomized comparative study. Anesth Essays Res. 2016;10(2):338–342. doi:10.4103/0259-1162.176403
19. Rahimzadeh P, Imani F, Sayarifard A, Sayarifard S, Faiz SH. Ultrasound-guided fascia iliaca compartment block in orthopedic fractures: bupivacaine 0.2% or 0.3%? Med J Islam Repub Iran. 2016;30:433.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

