Back to Journals » Drug Design, Development and Therapy » Volume 9
Comparative efficacy, tolerability, and survival outcomes of various radiopharmaceuticals in castration-resistant prostate cancer with bone metastasis: a meta-analysis of randomized controlled trials
Authors Tunio M , Al Asiri M, Al Hadab A, Bayoumi Y
Received 24 April 2015
Accepted for publication 3 August 2015
Published 21 September 2015 Volume 2015:9 Pages 5291—5299
DOI https://doi.org/10.2147/DDDT.S87304
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Prof. Dr. Wei Duan
Mutahir Tunio,1 Mushabbab Al Asiri,1 Abdulrehman Al Hadab,1 Yasser Bayoumi2
1Radiation Oncology, Comprehensive Cancer Center, King Fahad Medical City, Riyadh, Saudi Arabia; 2Radiation Oncology, National Cancer Institute, Cairo University, Cairo, Egypt
Background: A meta-analysis was conducted to assess the impact of radiopharmaceuticals (RPs) in castration-resistant prostate cancer (CRPC) on pain control, symptomatic skeletal events (SSEs), toxicity profile, quality of life (QoL), and overall survival (OS).
Materials and methods: The PubMed/MEDLINE, CANCERLIT, EMBASE, Cochrane Library database, and other search engines were searched to identify randomized controlled trials (RCTs) comparing RPs with control (placebo or radiation therapy) in metastatic CRPC. Data were extracted and assessed for the risk of bias (Cochrane’s risk of bias tool). Pooled data were expressed as odds ratio (OR), with 95% confidence intervals (CIs; Mantel–Haenszel fixed-effects model).
Results: Eight RCTs with a total patient population of 1,877 patients were identified. The use of RP was associated with significant reduction in pain intensity and SSE (OR: 0.63, 95% CI: 0.51–0.78, I2=27%, P<0.0001), improved QoL (OR: 0.71, 95% CI: 0.55–0.91, I2=65%, three trials, 1,178 patients, P=0.006), and a minimal improved OS (OR: 0.84, 95% CI: 0.64–1.04, I2=47%, seven trials, 1,845 patients, P=0.11). A subgroup analysis suggested an improved OS with radium-223 (OR: 0.68, 95% CI: 0.51–0.90, one trial, 921 patients) and strontium-89 (OR: 0.21, 95% CI: 0.05–0.91, one trial, 49 patients). Strontium-89 (five trials) was associated with increased rates of grade 3 and 4 thrombocytopenia (OR: 4.26, 95% CI: 2.22–8.18, P=0.01), leucopenia (OR: 7.98, 95% CI: 1.82–34.95, P=0.02), pain flare (OR: 6.82, 95% CI: 3.42–13.55, P=0.04), and emesis (OR: 3.61, 95% CI: 1.76–7.40, P=0.02).
Conclusion: The use of RPs was associated with significant reduction in SSEs and improved QoL, while the radium-223-related OS benefit warrants further large, RCTs in docetaxel naive metastatic CRPC patients.
Keywords: radiopharmaceuticals, castration-resistant prostate cancer, meta-analysis, pain control, symptomatic skeletal events, quality of life, overall survival
Introduction
Bone metastasis is a source of significant pain, functional disability, and poor quality of life (QoL) in patients with metastatic castration-resistant prostate cancer (CRPC). Systemic chemotherapy, bisphosphonates, and radiation therapy (RT) are the effective measures of palliating symptoms associated with bone metastasis.1,2 RT in the form of radiopharmaceuticals (RPs) has also been utilized to allow the targeted delivery of RT to multiple sites of metastatic disease, with evidence of significant palliative relief.3
Traditionally, beta (β)-emitting RPs (strontium-89 and samarium-153) have been widely used to control bone pain in CRPC, with pain response rates of 70%–80%; however, most of the published trials were underpowered to detect any overall survival (OS) benefit.4,5 Recently, alpha (α)-emitting RP agent, radium-223, has demonstrated a significant improvement in pain control, minimal toxicity, and OS benefit in patients with metastatic CRPC.6,7 However, there are limited data regarding the head-to-head comparisons between various RPs in metastatic CRPC patients to determine their relative efficacy, tolerability in pain palliation, and OS benefit.8,9 We undertook the present meta-analysis with the aim of determining the comparative efficacy, symptomatic skeletal event (SSE) control rates, functional mobility and QoL, OS, and toxicity profile of various RPs in CRPC patients with bone metastasis.
Materials and methods
The search criteria included the studies that were either complete randomized controlled trials (RCTs) or retrospective, if these were well controlled. The abstracts with full details were also included. The PubMed/MEDLINE, CANCERLIT, EMBASE, and Cochrane Library databases were searched using the terms castration-resistant prostate cancer, hormone-refractory prostate cancer, radiopharmaceuticals (strontium-89, samarium-153, rhenium-186, and radium-223), bone metastasis, and bone pain. These terms were then combined to search for randomized controlled reviews and meta-analyses. The relevant articles were retrieved by two reviewers. Any discrepancies between the reviewers were resolved through consensus. Then, only RCTs which met the following criteria were included:
- CRPC patients with confirmed bone metastasis.
- Patients had received RPs as part of bone pain management.
- The studies that included patients with other primary malignancies were excluded.
Outcome measures
The outcome measures were reductions in pain intensity and SSE, functional mobility and QoL, OS, and toxicity profile of the different RPs used. We hypothesized SSE as “increase in bone pain ≥50% from baseline, increase in analgesics ≥25%, worsening of daily activities of life ≥25%, new sites of bone pain, pathological bone fracture, and first request for additional RT”.
Quality assessment
The internal validity of included RCTs was evaluated using the Cochrane Risk of Bias tool, which consists of the following six domains: 1) selection bias (random sequence generation and allocation concealment), 2) performance bias (blinding of patients/participants), 3) detection bias (blinding of outcome assessment), 4) attrition bias (incomplete outcome data), 5) reporting bias, and 6) other sources of bias. Each separate domain was rated according to a “low”, “unclear”, or “high” risk of bias.10 A trial was finally rated as “low risk of bias” (all six domains rated as low risk), “high risk of bias” (one or more domains rated as high risk), and “unclear risk of bias”.
Review analysis
All analyses were carried out on an intention-to-treat analysis basis. For the categorical variables, weighted odds ratios (ORs) and their 95% confidence intervals (CIs) were calculated using the Review Manager (RevMan) software application, Version 5.3, provided by the Cochrane Collaboration (part of the meta-analytic software program Metaview: Update Software, Oxford, UK). The results were tested for heterogeneity (I2) at the significant level of P<0.05. If there was an evidence of heterogeneity (I2>50%), a random effects model was used for meta-analysis; otherwise, a fixed effects model was used. OR and 95% CI were calculated for each trial and presented in a forest plot. The publication bias was evaluated using the funnel graph, the Begg–Mazumdar-adjusted rank correlation test,11 and the Egger test.12 For heterogeneity, we carried out the Cochran’s Q-test to determine whether the studies are homogenous.
The study was exempt from Institutional ethics Committee approval.
Results
Yield of search strategy and characteristics of eligible studies
An electronic search revealed 1,241 relevant citations. After screening, 58 full-text articles were retrieved for further assessment. Finally, eight studies that met the criteria were identified (Figure 1); the total population of patients involved in these studies was 1,877. The details of included studies are shown in Tables 1 and 2.6,7,13–19 The studies were conducted in several countries. RCTs were published between 1988 and 2013; 75% were multicenter trials. All RCTs included metastatic CRPC patients with bone metastasis. All RCT studies reported on pain control and SSE; while seven RCTs reported OS and toxicity, and the QoL was reported in three RCTs. Four RCTs (50%) were rated to be in “high risk” of bias, two trials (25%) were considered to be in “low risk”, and two trials (25%) were classified as “unclear” with respect to the risk of bias (Figure 2).
  | Figure 1 Study flow diagram. |
  | Figure 2 Summary of risk bias assessment. |
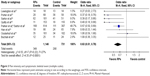
SSE control rate
All eight RCTs with a population of 1,877 patients analyzed the SSE rate as one of the outcomes. The SSE rate was significantly low in patients treated with RPs (P<0.0001). The pooled OR was 0.63 (95% CI: 0.51–0.78, I2=27%). The result of the test for heterogeneity was not statistically significant (I2=27%). The overall benefit from RPs and control groups on pain intensity and symptomatic skeletal events is shown in Figure 3.
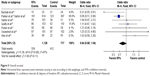
Functional mobility and QoL
Three RCTs with 1,178 patients examined the QoL as one of the outcomes. The overall functional mobility and QoL were significantly improved in patients treated with RPs (P=0.006). The pooled OR was 0.71 (95% CI: 0.55–0.91, I2=65%) as shown in Figure 4.
Overall survival
Seven RCTs, with 1,845 patients, addressed the OS as one of the outcomes. Two RCTs showed a significant improvement in the OS; five RCTs showed no difference and one RCT showed better survival in the control arm. The pooled OR was not statistically different between the RPs and control arms (0.84, 95% CI: 0.64–1.04, I2=47%, P=0.11; Figure 5).
Toxicity
Strontium-89 was used in five RCTs and samarium-153, rhenium-186, and radium-223 were used in the remaining three RCTs. Grade 3 and 4 hematological adverse events (thrombocytopenia and leucopenia) and nonhematological event (pain flare and emesis) toxicities were significantly high with strontium-89, whereas radium-223 was associated with the least grade ≥3 toxicity as shown in Table 3.
Publication bias
The funnel plot revealed a narrow funnel (Figure 6) showing no significant publication bias (P-values from the Begg–Mazumdar test and Egger test were 0.21 and 0.11, respectively).
  | Figure 6 Graph showing the publication bias. |
Discussion
Despite an initial response after the androgen deprivation therapy, most prostate patients ultimately suffer disease progression, developing CRPC. Recently, in CRPC patients, the use of second-generation androgen receptor blocking agents, particularly, the cytochrome P450 17 inhibitor abiraterone acetate and the novel antiandrogen enzalutamide have shown an improved OS and QoL in the pre- and postdocetaxel setting.20 Although several RPs with different physical properties have been used for the treatment of CRPC with bone metastasis; strontium-89 (Metastron; GE Healthcare), samarium-153 (Quadramet; GE Health Care and Dow Chemical Co, USA), and radium-223 (Xofigo; Bayer AG, Leverkusen, Germany) are currently approved in USA and many European countries.21 In the present meta-analysis, we found that the different RPs (strontium-89, samarium-153, rhenium-186, and radium-223) administered to metastatic CRPC patients were associated with significant pain relief, reduction in SSE, improved functional mobility, and QoL. In RCTs incorporating strontium-89, reductions in pain intensity and SSEs were greater when used above 150 MBq (4 mCi), and in the form of single-dose administration.13,15,22 There was no significant difference in pain relief with six monthly injections of radium-223 and a single injection of β-emitting RPs (strontium-89, samarium-153, and rhenium-183).
The pooled adjusted estimates from included RCTs showed that radium-223 and strontium-89 (one trial) were associated with significant improvement in OS.6,7,14 Interestingly, in three RCTs of strontium-89, the OS rates were better in control groups.13,15,16 Similarly, samarium-153 and rhenium-186 failed to show any OS benefit. However, it was clear in the meta-analysis that the trials using strontium-89 and samarium-153 were underpowered and mainly consisted of docetaxel naive patients. The OS benefit of strontium-89 and samarium-153 in docetaxel-treated metastatic CRPC patients deserves further exploration, as prolonged OS rates have been reported in the recent Phase II and retrospective studies incorporating strontium-89 or samarium-153 in previously treated patients with systemic chemotherapy.23–25
Further pooled adjusted estimates of acute toxicities showed that strontium-89 was associated with more acute grade ≥3 thrombocytopenia, leucopenia, pain flare, and emesis; while an isolated grade ≥3 leucopenia was observed with samarium-153. The acute toxicity of rhenium-186 was not reported in included trials; however, rhenium-186 is known to cause myelotoxicity as other β-emitting RPs.26 Radium-223 was found to be the safest RP without any statistically significant hematological and nonhematological toxicity. However, late adverse events, especially the potential risk of second malignancies, which are of great concern, were not addressed in all included studies. Few case reports have suggested the leukemogenic potential of strontium-89 in CRPC patients.27,28 The leukemogenic potential of other RPs is yet to be established. Recently, an Alpharadin in Symptomatic Prostate Cancer Patients (ALSYMPCA) trial at a 1.5-year follow-up (radium-223, n=406; placebo, n=168) reported no case of acute myelogenous leukemia, myelodysplastic syndrome, or primary bone cancer.6,7,29
The strengths of our meta-analysis were 1) completeness of the search strategy, including searching multiple databases, trial registries, and conference proceedings for RCTs comparing RPs to the control group (placebo, RT, or best supportive care) in metastatic CRPC patients, 2) patient-centered outcomes (pain intensity, SSE, and QoL), and 3) evaluation of the OS benefit and acute toxicity profile of RPs.
The limitations of our meta-analysis were 1) inherent methodological issues in the included trials (50% trials were rated to be in high risk of bias and 25% were classified as unclear with respect to the risk of bias) and 2) attrition and reporting bias in most of the included trials, which might have resulted in underestimated estimates.
Conclusion
The use of RPs was associated with significant reductions in pain intensity, SSEs, improved functional mobility, and improved QoL in metastatic CRPC patients. Radium-223 was found to be the least toxic RP and with clear survival benefit. However, the radium-223-related survival benefit warrants further large RCTs to evaluate the efficacy of radium-223 in docetaxel naive CRPC patients and to determine whether the therapeutic index of radium-223 could be improved by coupling it with other antibodies and/or nanoparticles.
Disclosure
All authors report no conflict of interest in this work.
References
Goyal J, Antonarakis ES. Bone-targeting radiopharmaceuticals for the treatment of prostate cancer with bone metastases. Cancer Lett. 2012;323(2):135–146. | ||
Saylor PJ, Lee RJ, Smith MR. Emerging therapies to prevent skeletal morbidity in men with prostate cancer. J Clin Oncol. 2011;29:3705–3714. | ||
Finlay IG, Mason MD, Shelley M. Radioisotopes for the palliation of metastatic bone cancer: a systematic review. Lancet Oncol. 2005;6:392–400. | ||
Bauman G, Charette M, Reid R, Sathya J. Radiopharmaceuticals for the palliation of painful bone metastasis-a systemic review. Radiother Oncol. 2005;75(3):258–270. | ||
Turner SL, Gruenewald S, Spry N, Gebski V; Metastron Users Group. Less pain does equal better quality of life following strontium-89 therapy for metastatic prostate cancer. Br J Cancer. 2001;84:297–302. | ||
Parker C, Nilsson S, Heinrich D, et al; ALSYMPCA Investigators. Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med. 2013;369(3):213–223. | ||
Sartor O, Coleman R, Nilsson S, et al. Effect of radium-223 dichloride on symptomatic skeletal events in patients with castration-resistant prostate cancer and bone metastases: results from a phase 3, double-blind, randomised trial. Lancet Oncol. 2014;15(7):738–746. | ||
Liepe K, Kotzerke J. A comparative study of 188Re-HEDP, 186Re-HEDP, 153Sm-EDTMP and 89Sr in the treatment of painful skeletal metastases. Nucl Med Commun. 2007;28:623–630. | ||
Liepe K, Runge R, Kotzerke J. The benefit of bone-seeking radiopharmaceuticals in the treatment of metastatic bone pain. J Cancer Res Clin Oncol. 2005;131:60–66. | ||
Higgins JP, Altman DG, Gotzsche PC, et al; Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. BMJ. 2011;343:d5928. | ||
Begg CB, Mazumdar M. Operating characteristics of rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. | ||
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple graphical test. BMJ. 1997;315:629–634. | ||
Porter AT, McEwan AJ, Powe JE, et al. Results of a randomized phase-III trial to evaluate the efficacy of strontium-89 adjuvant to local field external beam irradiation in the management of endocrine resistant metastatic prostate cancer. Int J Radiat Oncol Biol Phys. 1993;25(5):805–813. | ||
Buchali K, Correns HJ, Schuerer M, Schnorr D, Lips H, Sydow K. Results of a double blind study of 89-strontium therapy of skeletal metastases of prostatic carcinoma. Eur J Nucl Med. 1988;14(7–8):349–351. | ||
Quilty PM, Kirk D, Bolger JJ, et al. A comparison of the palliative effects of strontium-89 and external beam radiotherapy in metastatic prostate cancer. Radiother Oncol. 1994;31(1):33–40. | ||
Oosterhof GO, Roberts JT, de Reijke TM, et al. Strontium (89) chloride versus palliative local field radiotherapy in patients with hormonal escaped prostate cancer: a phase III study of the European Organisation for Research and Treatment of Cancer, Genitourinary Group. Eur Urol. 2003;44(5):519–526. | ||
Lewington VJ, McEwan AJ, Ackery DM, et al. A prospective, randomised double-blind crossover study to examine the efficacy of strontium-89 in pain palliation in patients with advanced prostate cancer metastatic to bone. Eur J Cancer. 1991;27(8):954–958. | ||
Sartor O, Reid RH, Hoskin PJ, et al; Quadramet 424Sm10/11 Study Group. Samarium-153-Lexidronam complex for treatment of painful bone metastases in hormone-refractory prostate cancer. Urology. 2004;63(5):940–945. | ||
Han SH, de Klerk JM, Tan S, et al. The PLACORHEN study: a double-blind, placebo-controlled, randomized radionuclide study with (186) Re-etidronate in hormone-resistant prostate cancer patients with painful bone metastases. Placebo Controlled Rhenium Study. J Nucl Med. 2002;43(9):1150–1156. | ||
Rodriguez-Vida A, Galazi M, Rudman S, Chowdhury S, Sternberg CN. Enzalutamide for the treatment of metastatic castration-resistant prostate cancer. Drug Des Devel Ther. 2015;9:3325–3339. | ||
Pandit-Taskar N, Larson SM, Carrasquillo JA. Bone-seeking radiopharmaceuticals for treatment of osseous metastases, Part 1: α therapy with 223Ra-dichloride. J Nucl Med. 2014;55(2):268–274. | ||
Robinson RG, Preston DF, Schiefelbein M, Baxter KG. Strontium 89 therapy for the palliation of pain due to osseous metastases. JAMA. 1995;274(5):420–424. | ||
Amato RJ, Hernandez-McClain J, Henary H. Bone-targeted therapy: phase II study of strontium-89 in combination with alternating weekly chemohormonal therapies for patients with advanced androgen-independent prostate cancer. Am J Clin Oncol. 2008;31(6):532–538. | ||
Kuroda I. Strontium-89 for prostate cancer with bone metastases: the potential of cancer control and improvement of overall survival. Ann Nucl Med. 2014;28(1):11–16. | ||
Fizazi K, Beuzeboc P, Lumbroso J, et al. Phase II trial of consolidation docetaxel and samarium-153 in patients with bone metastases from castration-resistant prostate cancer. J Clin Oncol. 2009;27(15):2429–2435. | ||
Pirayesh E, Amoui M, Mirzaee HR, et al. Phase 2 study of a high dose of 186Re-HEDP for bone pain palliation in patients with widespread skeletal metastases. J Nucl Med Technol. 2013;41(3):192–196. | ||
Kossman SE, Weiss MA. Acute myelogenous leukemia after exposure to strontium-89 for the treatment of adenocarcinoma of the prostate. Cancer. 2000;88(3):620–624. | ||
Welsh JS, Howard SP. Acute myelogenous leukemia after exposure to strontium-89 for the treatment of adenocarcinoma of the prostate. Cancer. 2000;89(1):226–227. | ||
Nilsson S, Vogelzang N, Sartor O, et al. 1.5-year post-treatment follow-up of radium-223 dichloride (Ra-223) in patients with castration-resistant prostate cancer (CRPC) and bone metastases from the phase 3 ALSYMPCA study. Poster presented at: 2014 Genitourinary Cancers Symposium; January 30–February 1, 2014; San Francisco, California. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.