Back to Journals » Risk Management and Healthcare Policy » Volume 13
Community Perception and Attitude Towards People with Schizophrenia Among Residents of Arba Minch Zuria District, Arba Minch Health and Demographic Surveillance Sites System (AM-HDSS), Ethiopia: Cross-Section Study
Authors Boti N , Hussen S , Ayele G , Mersha A , Gebeyehu S, Kassa M, Feleke T, Temesgen G
Received 10 December 2019
Accepted for publication 14 July 2020
Published 4 September 2020 Volume 2020:13 Pages 1437—1446
DOI https://doi.org/10.2147/RMHP.S241713
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Kent Rondeau
Negussie Boti,1 Sultan Hussen,1 Gistane Ayele,1 Abera Mersha,2 Selamawit Gebeyehu,1 Mekidm Kassa,1 Tesfaye Feleke,1 Gebremaryam Temesgen3
1School of Public Health, College of Medicine and Health Sciences, Arba Minch University, Arba Minch, Ethiopia; 2School of Nursing, College of Medicine and Health Sciences, Arba Minch University, Arba Minch, Ethiopia; 3Department of Midwifery, College of Medicine and Health Sciences, Arba Minch University, Arba Minch, Ethiopia
Correspondence: Negussie Boti Tel +251-920-997-752
Email [email protected]
Background: Mental health disorders have identified as being one of the public health issues throughout the world. Recent evidence reveals that more than 21 million people diagnosed with schizophrenia. However, there is little information about community perception and attitude towards people with Schizophrenia in Ethiopia.
Objective: The aim of this study was to assess the community perception and attitude towards people with Schizophrenia among residents of Arba Minch Zuria Districts, Southern Ethiopia.
Methods: A community-based cross-sectional study was conducted among 617 randomly selected adults. Interviewer-administered standard tool was used to collect the data. Descriptive statistics like frequency, mean, and median computed. A binary logistic regression model used to identify factors affecting community perception and attitude towards people with schizophrenia.
Results: Of the study population, 469 (76%) of respondents had good perception and 390 (63.2%) had positive attitudes towards people with schizophrenia. The study participants identified talkativeness and self-neglect behaviors as the most common manifestations of schizophrenia. Besides, this study identified substance misuse and head injury as the perceived cause and spiritual or traditional methods as a preferred treatment for people with schizophrenia. Moreover, the study participants preferred spiritual or traditional methods for the treatment of schizophrenia. Young age [AOR=2.03, 95% CI: 1.21, 3.40], females [AOR=2.32, 95% CI: 1.58, 3.41], good perception towards people with schizophrenia [AOR=4.95, 95% CI: 3.25, 7.54] and no formal educational status [AOR=2.75, 95% CI: 1.33, 5.70], and primary education [AOR=3.72, 95% CI: 1.87, 7.39] were significantly associated with the attitude towards people with schizophrenia.
Conclusion: The findings of this study indicate that approximately one-third of the residents had unfavorable attitudes towards people with schizophrenia. Therefore, giving special attention to male, elders and those who were educated, and individuals who have poor perceptions of people with schizophrenia is crucial.
Keywords: perception, attitude, schizophrenia, Arba Minch Zuria District, Southern Ethiopia
Introduction
Mental health disorders are health conditions that show abnormal behavior and thinking associated with distress and problems functioning in family activities.1,2 Schizophrenia is one of the most common mental illness that affects the educational and occupational performance of an individual’s.3,4
Globally, Schizophrenia affects more than 21 million people from which male accounts for more than 12 million and females account for more than 9 million.3 Schizophrenia is more common in Africa that accounts for 0.5% of the world population.4 In Ethiopia, Schizophrenia is increasingly becoming the public health problem and one of the ten top-ranked causes of morbidity.5
Despite the afore-mentioned public health implication of Schizophrenia in Africa, the issue did not get the appropriate attention, especially in Ethiopia.4 For instance, the “treatment gap” – the proportion of people with mental illness with inappropriate treatment ranges from 75% in South Africa to more than 90% in Nigeria.6 In Ethiopia, only 10% ever receive effective care among people living with schizophrenia.4
Attitude and perception of the community towards mental illness affect Schizophrenic patients to seek appropriate treatment. Furthermore, a lack of knowledge, as well as a mix of traditional rituals with the modern intervention approaches also influencing appropriate treatments.7,8 In Africa, only 35% of people with Schizophrenia have got treatment from a modern psychiatric treatment center. An unacceptable belief about the causes of mental illnesses and the type of treatment sector further worsen the poor habits of seeking appropriate treatment for schizophrenia.9
Moreover, the stigmatizing attitudes towards mental illness are highly rampant in sub-Saharan Africa, notably in the rural areas.10,11 Likewise, in Ethiopia, mental health is neglected with little attention for a long time. Consequently, most people preferred to use traditional methods for the treatment of mental illnesses.5,12
Evidence in Ethiopia reveals that due to lack of available local means of psychotic treatment means many families keep the people with schizophrenia at home under restraint until they are no longer aggressive and violent. However, many of them become wanderers and homeless when released from the detention without appropriate treatment.5,12,13
Even more, most Ethiopians’ perceived that Schizophrenia is an illness that is caused by supernatural forces and this influences their attitude towards mental illness and help-seeking behaviors.13 Other factors affect the community perception and attitude related to schizophrenic patients for instance gender, age, religion, income and educational status of an individual.13–15
However, there is little information about the community perception and attitude towards people with Schizophrenia in Ethiopia.13–15 Accordingly, assessing the community perception and attitude towards people with Schizophrenia may help to develop interventions that contribute to the creation of an enabling environment to access and utilize mental health services. Therefore, this study aimed to assess the status of the community perception and attitude towards people with schizophrenia among residents of Arba Minch Zuria District, AM-HDSS, and Southern Ethiopia.
Methods
Study Area, Design and Period
This community-based cross-sectional study conducted from January 10–24, 2019, in nine Kebeles (the lowest administrative unit of Ethiopia) of Arba Minch Zuria districts included under Arba Minch Health and Demographic Surveillance System sites (AM-HDSS). Arba Minch town located 450km from Addis Ababa, the capital city, and 275km from Hawassa, a regional town. The district was bordered on the South by the Dirashe special district, on the West by Bonke district, on the North by Dita and Chencha districts, on the Northeast by Mirab Abaya district, on the East by the Oromia Regional state, and on the Southeast by the Amaro special district. Arba Minch town located at an altitude of 130 above sea level with the average temperature of 29°C. Based on the 2007 census of Ethiopia, this district has a total population of 164,529, of whom 82,199 are men, and 82,330 are women. Arba Minch Zuria district has 31 kebeles with three different climatic zones, high land, midland and lowland, among which nine kebeles included in AM-HDSS.
Population
All households in the AM-HDSS used as the source population for this study. The study population was all heads of households (or their spouse), who are the residents in AM-HDSS during the data collection period.
Eligibility Criteria
All residents who were 18 years old and above living for at least six months in the study area during the study period were eligible, and those who were critically ill and unable to respond to the questions excluded from the study.
Sample Size and Sampling Technique
The sample size for this study determined by using single population proportion formula and the following assumptions: the proportion of the community who had poor perception towards mental illness was 37.3%,14 95% confidence level (1.96), 4% of the margin of error, and 10% non-response rate. As a result, the calculated sample size for this study was 617 individuals. To select the study participants for this study, initially, the calculated sample was proportionally allocated to the nine kebeles according to their total number of households, and the sampling frame sought from the AM-HDSS database. Then, a simple random sampling method using computer-generated random numbers were applied to identify the households for this study. Finally, heads (their spouses) interviewed by the data collectors.
Measurements
Attitude Towards People with Schizophrenia
It refers to how the community sees situations, as well as defines how they behave toward the people with schizophrenia or a mental state of readiness, organized through experience, exerting a directive or dynamic influence on the individual’s response to people with schizophrenia. It was measured based on 13 attitude related questions. To categorize community attitude towards people with schizophrenia, we used the demarcation threshold formula.
As a result, the study participants who scored ≤39 considered to have a positive attitude towards people with schizophrenia.5,13,14
Community Perception Toward People with Schizophrenia
It refers to the level of identification and interpretation of sensory information to represent and understand the presented information. Assessed by using nine items of five Likert scale perception related questionnaires. Similarly, to categorize community perception towards people with schizophrenia, we used the demarcation threshold formula. Those who scored ≤27 for nine items of five semantic differential scales considered as having a good perception towards people with schizophrenia.13,14
Data Collection Tools and Procedure
The interviewer-administered questionnaires used to collect the data, which were developed based on different works of literature.5,13-15 The questions to measure perception based on the following Vignette case of schizophrenia:
During the last six months, one of your friends has changed. He withdraws from his coworkers and friends more and more. He keeps out of everybody’s way. Contrary to his former habits, he does not take care of his appearance any longer and seems to neglect himself increasingly. He seems to be anxious and agitated. He reports to convinced that people can read other people’s thoughts and that they are also able to influence these thoughts, but he would not yet know who is controlling his thoughts. He even hears these people talking to him and giving him orders. Sometimes, they speak to one another and mock him. In his apartment, the situation is particularly bad. There he feels threatened and scared. He has not been at home for a week and hid in a hotel, which he has not dared to leave.
Based on the WHO recommendation to measure perception, a modified Vignettes case used to assess the community perception toward people with schizophrenia. The questionnaire to measure perception has nine items of five Likert scales (from 1 to 5): (1 = strongly agree, 2 = agree, 3 = neutral, 4 = disagree, and 5 = strongly disagree).
The questionnaire with 13 items of five-point Likert scales (from 1 to 5): (1 = strongly agree, 2 = agree, 3 = neutral, 4 = disagree, and 5 = strongly disagree) used to assess the community attitude towards people with schizophrenia. This tool was previously pretested and validated in Ethiopia and other sub-Saharan Africa.13,14,16
The tools first developed in the English language and then translated to the Amharic language then back to the English language to check the consistency. The ODK software used to collect the data. Eighty data collectors and five field supervisors who had direct experience and ability to speak Amharic language recruited for data collection. After three days of intensive training, the data collected by going to house-to-house to the randomly selected house numbers.
Data Quality Control
To maintain the quality of the data training gave to the supervisors and data collectors and the tools were pre-tested on 5% of the study participants in Mirab Abaya, before the actual data collection. During data collection, the collected questionnaire was checked for its completeness every day by investigators and supervisors.
Data Processing and Analysis
The collected data was cleaned and edited and then analyzed by using STATA version 14.0. Descriptive statistics like frequency, percentage, mean, median, and standard deviation computed, and bivariate logistic regression analysis conducted for each independent variable and outcome of interests. Then, p-value <0.25, context, and previous studies considered to make the variables to the multivariable analysis. In the final model, the independent variables with the p-value less than 0.05 identified as a significant predictor of the outcome variable. The crude and adjusted odds ratios with the 95% confidence intervals were computed and interpreted accordingly. Multi-collinearity tested by variance inflation factor (VIF) and goodness of fit measured by the Hosmer and Lemeshow test.
Ethical Consideration
Ethical approval obtained from the Institutional Research Ethics Review Board (IRB) of the College of Medicine and Health Sciences, Arba Minch University. This study followed the Declaration of Helsinki. Written consent obtained from all the study participants after fully informed about the objectives and procedures of the study. The confidentiality and privacy of participants fully protected. All participants were assigned a unique identification number. The study participants voluntarily participated in the study. They had the right to stop or discontinue from the study at any time.
Results
Socio‑Demographic Characteristics of the Study Participants
Among the total 617 respondents, 324 (52.5%) were male, and 559 (90.6%) of them were ever married. The mean (±SD) age of respondents was 35.61 (±10.52) years. The majority of respondents 507 (82.2%) were Gamo by ethnicity, and 423 (68.6%) were protestant Christian in their religion. Regarding their educational status, 312 (50.6%) of the participants completed primary school, and 615 (99.7%) were from rural residents (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Respondents Residing in AMU-HDSS, Southern Ethiopia, 2019 (N = 617) |
General information about schizophrenia: Around 558 (90.4%) of the study participants ever heard about schizophrenia. Regarding sources for schizophrenia, 399 (48%) of study participants heard from mass media and followed by religious institutions, which account for 113 (13.6%). From the total study participants, 401 (71.86%) listed the possible cause of schizophrenia. The majority (91.52%) and 275 (68.58%) of the study participants perceived that the predisposing factor schizophrenia was substance misuse and head injury, respectively. Furthermore, 341 (61.11%) of respondents mentioned that the preferred treatment for the people with schizophrenia was spiritual/traditional (Table 2).
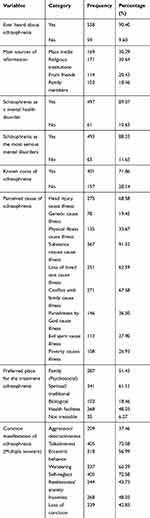 |
Table 2 Source of Information About Schizophrenia Among Respondents Residing in AMU-HDSS, Southern Ethiopia, 2019 (N = 617) |
Community Perception and Attitude Towards People with Schizophrenia
The finding of this study shows that among the study participants, 63.2% (95% CI: 59.4%, 67%) of respondents had a positive attitude towards people with schizophrenia and more than 3/4, 76.1% (95% CI: 72.6%, 79.4%), had a good perception for people with schizophrenia (Table 3).
 |
Table 3 Community Perception and Attitude Towards People with Schizophrenia Among Residents of Arba Minch Zuria District, AM-HDSS Site, Southern Ethiopia |
Community Attitude Towards People with Schizophrenia
Two hundred forty-three (39.4%) of respondents agree that a person should admit to the hospital after he/she develops signs of schizophrenia, and over half (55.9%) of those surveyed agreed that the predisposing factor for schizophrenia was substance abuse. Nearly one-fourth (22.4%) agree that people with schizophrenia could function freely in society after proper treatment. Almost half (49.1%) of respondents agree that individuals with schizophrenia are simply weak-willed and not motivated people. The majority of respondents (70.5%) agree that people with schizophrenia are dangerous, and almost half (49.4%) of the respondents disagreed that individuals with schizophrenia should change the thought process and behavior than seeking medication for treatment (Table 4).
 |
Table 4 Responses to the Item of Community Attitude Towards People with Schizophrenia Subscales Among Residents of Arba Minch Zuria District, AM-HDSS Site, Ethiopia, 2019 (N=617) |
Factors Associated with Community Attitude Towards People with Schizophrenia
After controlling the confounding effect, variables like age, sex, education status, marital status, and perception towards people with schizophrenia significantly associated with community attitude towards people with schizophrenia.
The finding of this study reveals that respondents whose age between 18 and 24 years were 2.03 times more likely to have a positive attitude towards people with schizophrenia compared to an older age group [AOR=2.03, 95% CI: 1.21,3.40]. Those who were females were 2.32 times more likely to have a positive attitude towards people with schizophrenia compared to males [AOR=2.32, 95% CI: 1.58, 3.41].
Moreover, participants with good perception towards people with schizophrenia were 4.95 times more likely to have a positive attitude towards people with schizophrenia as compared to the counterparts [AOR=4.95, 95% CI: 3.25,7.54]. Furthermore, participants with no formal education status [AOR=2.75, 95% CI: 1.33, 5.70], and primary education [AOR=3.72, 95% CI: 1.87, 7.39] were significantly associated with the attitude towards people with schizophrenia (Table 5).
 |
Table 5 Factors Associated with Community Attitude Towards People with Schizophrenia Among Residents of Arba Minch Zuria District, AM-HDSS Site, Southern Ethiopia, 2019 |
Discussion
The primary objectives of this investigation were to determine the Arba Minch Zuria District residents’ perception and attitude toward schizophrenic patients as well as to identify the factors associated with residents’ attitudes towards patients with schizophrenia. As a result, while nearly three-fourths of the residents had a good perception for people with schizophrenia, only two-third of individuals had a positive attitude for patients with schizophrenia. The study participants age, sex, educational status, and the status of perception towards people with schizophrenia were significantly affected their attitude toward patients with schizophrenia. These findings imply that the significant proportion of the community members in the study area had a negative attitude toward patients with schizophrenia.
The proportion of study participants, which accounts 76% (95% CI: 72.6%,79.4%), with good perception towards people with schizophrenia in this study, is relatively higher than the finding from the residents of Hawassa city, Southern Ethiopia, 66.5%13 and lower than finding from the Zaire Community.17 This difference might be due to the difference in time of the studies conducted, study settings of the study participants, methodological difference, and the way of people’s lives.
The finding of this study also revealed that the prevalence of a positive attitude towards people with schizophrenia among residents in Arba Minch Zuria district, 63.2% (95% CI: 59.4%, 67.0%), is higher than findings of the study done in Southern Ethiopia, 37.3%.13 However, lower than the study findings in Greek.18 The possible reason for this discrepancy might be since the current study only involved rural residents while the previous studies conducted in urban residents. The urban residents have relatively better education, economy, and access to information. Also, this finding implies that there is a satisfactory level of the community attitudes in the rural community for establishing and strengthening community-based rehabilitation for the people living with a mental health problem. It gives information and an input for the health professionals’ for better effectiveness of mental health program that requires to integrate patients into community-based services where they can live and possibly work to be self-independent in the community.
Concerning the manifestations of schizophrenia, the study participants frequently responded talkativeness and self-neglect behaviors as the manifestations of schizophrenia. This finding was in line with the study from Zaire Community.17 This result suggests that one has to exhibit behavior that draws public attention and disturbing society, recognized as having a mental disorder. Also, health professionals should give special care to people who come with the complaint of talkativeness and self-neglect.
Moreover, the participants of this study perceived substance misuse and head injury as the common causes of schizophrenia. This finding concurred the finding from Zaire Community.17 It is a matter that the identified situations exposed an individual to a stressful situation and thus increased the probability of developing schizophrenia in the long run. Based on this finding, the policymakers should develop an intervention for schizophrenia focusing on causes. The community member should keep their environment free from substance misuse and injury. There is a need to provide more knowledge and increased awareness of the causes of mental illness and dispel the myths around the predisposing factors for the disorders.
Similar to the pieces of evidence from Agaro town, Gimbi town, and Hawassa city of Ethiopia.,13,14,19 spiritual/traditional treatment identified as the most preferred place for the treatment of schizophrenia. Thus, the need for awareness sessions for the community on possible treatment options for better effectiveness of modern antipsychotic therapies. It is essential because the majority of people in this study area seek treatment from spiritual/traditional methods as a preferred method.
The current study demonstrated that youths experienced a positive attitude towards people with schizophrenia than those of older-aged participants. This study was in line with the findings from Riyadh and Saudi Arabia.10 However, not supported by the study result from Southern Ghana.20 The possible reason for this might be since the young population has better access to adequate and accurate information about mental illness.
The sex of respondents was also one of the factors associated with a positive attitude towards people with schizophrenia. Females were more likely to experience a positive attitude towards people with schizophrenia than males. This finding was congruent with the studies in Singapore, and Southern Ethiopia.2,15 However, inconsistent with the studies conducted in Southern Ghana and Riyadh, Saudi Arabia.10,20 The difference might be due to variation in study time and source of data.
Furthermore, the finding of this study revealed that the study participants with no formal education and primary education were more likely to have a positive attitude to people with schizophrenia. These findings were inconsistent with the studies conducted in Riyadh, Saudi Arabia, Singapore and Southern Ethiopia.2,2,10,13 These might be since individuals in developed countries with advanced educational levels experienced more mental health-related situations from a long time and complicated working environment.
In this study, the community perception towards people with schizophrenia was one of the factors associated with a positive attitude towards people with schizophrenia. The single most conspicuous observation to emerge from this study was those respondents who had good perception towards people with schizophrenia were more likely to have a positive attitude towards people with schizophrenia.
Limitation of the Study
As this study exclusively conducted in the rule community, the findings cannot be generalized to all people living in Ethiopia. Besides, there may be social desirability bias on the information of attitude towards people with Schizophrenia since we collected the data by using the interviewer administer technique. Due to the use of cross-sectional study design, it is hard to develop cause and effect relationships. Thus, we strongly recommend further study by employing the qualitative study design to understand well enough the community perception and attitude for patients with schizophrenia.
Conclusion
In conclusion, the findings of this study indicate that approximately one-third of the residents had unfavorable attitudes towards people with schizophrenia. Talkativeness and self-neglect behaviors were the most commonly mentioned manifestation of schizophrenia. Substance misuse and head injury were also the most perceived cause of schizophrenia in this study. Spiritual/traditional places were preferred places for the treatment of schizophrenia. Young age, female sex, having good perception and educational status of respondents were significantly associated with a positive attitude towards people with schizophrenia.
Therefore, different stakeholders working on mental health programs can keep and potentially improve mental health services in the rural community to improve the community attitude and perception. Besides, working on changing and strengthening community awareness about the correct treatment options for mental illness is also very important. Furthermore, focusing on risk factors like being females, youths, uneducated, and individuals who have poor perception towards people with schizophrenia requires special attention by health-care providers and program implementers. The interventions should consciously focus on people who misuse substances and with a head injury to reduce the occurrence of schizophrenia.
Abbreviations
AM-HDSS, Arba Minch Health and Demographic Surveillance Sites; AOR, adjusted odds ratio; CI, confidence interval; COR, crudes odds ratio; MI, mental illness; VIF, variance inflation factor.
Data Sharing Statement
The data used to support the findings of this study are available from the corresponding author upon request.
Acknowledgments
We would like to acknowledge all study participants for their voluntary participation in this study. We would like to extend our gratitude to Arba Minch University for all the support and opportunity that provided for us to conduct this study. Finally, yet importantly, we also extend our gratefulness to AM-HDSS office for providing us the sampling frame and for their continuous support during data collection. A preprint of this paper is online (https://www.medrxiv.org/content/10.1101/2019.12.18.19015271v1).
Disclosure
The authors report no conflicts of interest in this work.
References
1. American Psychiatric Association. What is Mental Illness?; June 2018.
2. Ritchie H, Roser M Mental health; 2018. Available from: https://ourworldindata.org/mental–health.
3. World Health Organization. Mental health action plan 2013–2020. Geneva: WHO; 2013. Available from: https://www.who.int/mental_health/publications/action_plan/en/. Accessed August 19, 2020.
4. Sankoh O, Sevalie S, Weston M. Mental health in Africa. Lancet Glob Health. 2018;6(9):e954–5. doi:10.1016/S2214-109X(18)30303-6
5. Ayano G, Assefa D, Haile K, et al. Mental health training for primary health care workers and implication for the success of the integration of mental health into primary care: evaluation of effect on knowledge, attitude and practices (KAP). Int J Ment Health Syst. 2017;11(1):63. doi:10.1186/s13033-017-0169-8
6. Lund C 2018. Why Africa needs to start focusing on the neglected issue of mental health [Online]. The Conversation. Available from: https://theconversation.com/why-africa-needs-to-start-focusing-on-the-neglected-issue-of-mental-health91406.
7. Van der Ham L, Wright P, Van TV, Doan VD, Broerse JE. Perceptions of mental health and help-seeking behavior in an urban community in Vietnam: an explorative study. Community Ment Health J. 2011;47(5):574–582. doi:10.1007/s10597-011-9393-x
8. Iheanacho T, Marienfeld C, Stefanovics E, Rosenheck RA. Attitudes toward mental illness and changes associated with a brief educational intervention for medical and nursing students in Nigeria. Acad Psychiatry. 2014;38(3):320–324. doi:10.1007/s40596-014-0073-3
9. Girma E, Tesfaye M. Patterns of treatment-seeking behavior for mental illnesses in Southwest Ethiopia: a hospital-based study. BMC Psychiatry. 2011;11(1):138. doi:10.1186/1471-244X-11-138
10. Barke A, Nyarko S, Klecha D. The stigma of mental illness in Southern Ghana: attitudes of the urban population and patients’ views. Soc Psychiatry Psychiatr Epidemiol. 2011;46(11):1191–1202. doi:10.1007/s00127-010-0290-3
11. Ayazi T, Lien L, Eide A, Shadar EJ, Hauff E. Community attitudes and social distance towards the mentally ill in South Sudan: a survey from a post-conflict setting with no mental health services. Soc Psychiatry Psychiatr Epidemiol. 2014;49(5):771–780. doi:10.1007/s00127-013-0775-y
12. Hailemariam KW. Perceived causes of mental illness and treatment seeking behaviors among people with mental health problems in Gebremenfes Kidus Holy Water Site. Am J Appl Psychol. 2015;3(2):34–42.
13. Ayano G, Agidew M, Duko B, Mulat H, Alemayew M. Perception, attitude and associated factors on schizophrenia and depression among residents of Hawassa City, South Ethiopia, Cross-Sectional Study. Am J Psychiatry Neurosci. 2015;3:116–124. doi:10.11648/j.ajpn.20150306.14
14. Benti M, Ebrahim J, Awoke T, Yohannis Z, Bedaso A. Community Perception towards Mental Illness among Residents of Gimbi Town, Western Ethiopia. Psychiatry J. 2016;6740346.
15. Bedaso A, Yeneabat T, Yohannis Z, Bedasso K, Feyera F. Community attitude and associated factors towards people with mental illness among residents of Worabe Town, Silte Zone, southern nation’s nationalities and people’s region, Ethiopia. PLoS One. 2016;11(3):e0149429. doi:10.1371/journal.pone.0149429
16. Venkatesh BT, Andrews T, Mayya SS, Singh MM, Parsekar SS. Perception of stigma toward mental illness in South India. J Family Med Prim Care. 2015;4(3):449. doi:10.4103/2249-4863.161352
17. Fiasorgbor AD, Aniah AS. Perceptions and beliefs about mental illness (schizophrenia) among adults in Zaare Community. Dev Country Stud. 2015;5(9):150–158.
18. Deribew A, Tamirat YS. How are mental health problems perceived by a community in Agaro town? Ethiop J Health Dev. 2005;19(2):153–159. doi:10.4314/ejhd.v19i2.9985
19. Dawood E, Modayfer O. Public attitude towards mental illness and mental health services in Riyadh, Saudi Arabia. Res Hum Soc Sci. 2016;6:63–75.
20. Yuan Q, Abdin E, Picco L, et al. Attitudes to mental illness and it’s demographic correlates among the general population in Singapore. PLoS One. 2016;11(11):e0167297. doi:10.1371/journal.pone.0167297
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.