Back to Journals » OncoTargets and Therapy » Volume 13
Combining the Fibrinogen-to-Pre-Albumin Ratio and Prognostic Nutritional Index (FPR-PNI) Predicts the Survival in Elderly Gastric Cancer Patients After Gastrectomy
Authors Zhang X, Zhao W, Chen X , Zhao M , Qi X, Li G, Shen A, Yang L
Received 23 May 2020
Accepted for publication 17 July 2020
Published 7 September 2020 Volume 2020:13 Pages 8845—8859
DOI https://doi.org/10.2147/OTT.S264199
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Federico Perche
Xunlei Zhang,1,* Wenjing Zhao,2,* Xin Chen,3,* Min Zhao,4 Xue Qi,5 Guoxing Li,3 Aiguo Shen,2 Lei Yang1
1Department of Oncology, Affiliated Tumor Hospital of Nantong University, Nantong Jiangsu, People’s Republic of China; 2Cancer Research Center, Affiliated Tumor Hospital of Nantong University, Nantong Jiangsu, People’s Republic of China; 3Department of General Surgery, Affiliated Tumor Hospital of Nantong University, Nantong Jiangsu, People’s Republic of China; 4Department of Pathology, Affiliated Tumor Hospital of Nantong University, Nantong Jiangsu, People’s Republic of China; 5Department of Oncology, Nantong Liangchun Hospital of Traditional Chinese Medicine, Nantong, Jiangsu, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Lei Yang Email [email protected]
Aiguo Shen Email [email protected]
Background: Inflammation and nutrition are important causes contributing to the progression and poor survival of gastric cancer (GC). The objective of this study is to investigate the prognostic significance of the preoperative fibrinogen-to-pre-albumin ratio (FPR) and the prognostic nutritional index (PNI) in GC patients who have undergone gastrectomy.
Methods: A total of 274 patients with resected pathological GC from January 2007 to December 2013 were enrolled in this retrospective study. Survival analysis was performed using Kaplan–Meier and log rank tests. Univariate and multivariate analyses were established to identify independent prognostic factors of 5-year survival. A predictive nomogram was used to predict prognosis of overall survival (OS), and its accuracy was determined by Harrell’s concordance index (C index).
Results: A high preoperative FPR-PNI score was significantly correlated with age, bigger tumor size, more lymphatic metastases and advanced TNM stage. Univariate analysis revealed that the GC patients with high FPR, low PNI and high FPR-PNI scores had shorter survival time. Multivariate analysis showed that FPR-PNI was an independent prognostic factor for OS in GC patients, especially in elderly patients. In the sub-analysis by age, the FPR-PNI score could significantly increase the accuracy of prognosis compared with the FPR and PNI alone in elderly GC patients.
Conclusion: The preoperative FPR-PNI score is an effective independent prognostic index for GC patients after surgery, especially in elderly patients.
Keywords: gastric cancer, prognostic nutritional index, fibrinogen-to-pre-albumin ratio, FPR-PNI, prognosis
Introduction
Gastric cancer (GC) is a malignant tumor with a high incidence, ranking fifth among all cancers and ranking third in the global cancer-related mortality rate.1 The peak incidence of GC patients is occurring in their sixties. As patients with early-stage gastric cancer often have no symptoms, the majority of patients are already diagnosed at an advanced stage. Although GC patients normally undergo radical resection and postoperative adjuvant chemotherapy, most patients will suffer recurrence and metastasis after resection, which leads to the poor level of the 5-year survival rate.2 Because of the physical conditions and different disease status, GC patients should receive individualized therapeutic regimens, which require the identification of different risk groups and more potential prognostic biomarkers. Elderly GC patients, who are often malnourished and have various comorbid conditions, with declining organ function and hypoimmunity state, usually have poor short-term outcomes.3–5 Therefore, it is important to develop prognosis evaluation biomarkers and corresponding therapeutic strategies for elderly GC patients.
Various clinicopathological prognostic factors, such as differentiation, vascular and neural invasion, depth of invasion, TNM stage, lymph node metastasis and distant metastasis, have been identified to significantly affect the outcome and survival of GC patients. However, the prognosis prediction of GC still remains unsatisfactory. In recent years, there have been many prognostic scoring systems based on blood tests that can predict the prognosis of GC to some extent, mainly including hypercoagulability, nutritional status and inflammation.6–9 Some inflammation-based prognostic variables such as the platelet–lymphocyte ratio (PLR), lymphocyte–monocyte ratio (LMR) and neutrophil–lymphocyte ratio (NLR) have also been established as predictors of long-term survival in GC patients.10–12 In addition to inflammation, nutritional status and abnormal coagulation are also related to malignant tumor occurrence and development. Fibrinogen, which is a key regulator of the hemostatic system, plays important roles in blood coagulation, cell–cell adhesion and the systemic inflammatory response.13 Many studies have shown that elevated plasma fibrinogen levels could promote tumor progression, invasion and distant metastasis and are associated with poor prognosis in GC patients.14,15 Albumin and pre-albumin, which are suppressed to synthesize by malnutrition and inflammation, are commonly used to assess the nutritional and inflammatory status. Besides, previous studies showed albumin and pre-albumin were potential prognostic factors for GC patients.16,17
The prognostic nutritional index (PNI), which is calculated by serum lymphocyte counts and albumin levels, has been introduced as an easily measurable index of nutrition status. It was reported that a low preoperative PNI score was a strong predictor for unfavorable prognosis in GC patients.18–22 Recent research suggested that the preoperative fibrinogen/pre-albumin ratio (FPR) might be a novel prognostic indicator in stage II–III GC patients, and could precisely distinguish the stage III patients who are able to benefit from adjuvant chemotherapy.23 Therefore, we proposed using a novel marker, the FPR-PNI score, representing a combination of inflammation, coagulation function and nutritional status, to investigate its prognostic impact in patients with resectable gastric cancer.24
Methods
Patients
Patients with histologically diagnosed GC who underwent gastrectomy in the Nantong Tumor Hospital between January 2007 and December 2013 were enrolled for this study. The diagnosis of GC was confirmed dependent on histological evidence and classified based on the eighth edition of the TNM-UICC/AJCC classification. The inclusion criteria were as follows: 1) all patients with GC who underwent a total or subtotal gastrectomy with standard lymphadenectomy; 2) no prior preoperation anticancer treatment, such as chemotherapy or radiotherapy; 3 no acute inflammatory disease, liver cirrhosis, chronic renal failure, autoimmune disease or hematopoietic system disease; 4) with available preoperative serum data of fibrinogen, albumin, pre-albumin and peripheral lymphocyte count; and 5) with adequate clinicopathological data and overall survival (OS) data. At last, 274 patients were enrolled in the present study. This study was approved by the Ethics Committee of Tumor Hospital Affiliated to Nantong University. All data were obtained in accordance with the Helsinki Declaration and its amendments. Informed consent was not required as the study was based on retrospective anonymous patient data and did not involve patient intervention or the use of human tissue samples.
Data Collection
Clinicopathological information of the patients was obtained from the medical records, including sex, age, tumor location, tumor size, Bormann types, differentiation, operation type, ulcer, vascular invasion, nerve invasion, depth of invasion, adjuvant chemotherapy, lymph node metastasis and TNM stage. OS was defined as the period from the surgery date to the date of death or the last follow-up. Pretreatment fasting peripheral blood samples were collected within the last one week before operation. The obtained blood samples were processed within 48 h to detect biomarkers including blood cells, fibrinogen (Fib), albumin (Alb), pre-albumin (pAlb) and total lymphocyte count (Tlc) levels. The FPR and PNI were calculated using the following equations: FPR=Fib/pAlb and PNI=Alb (g/L)+5×Tlc (109/L). The cutoff values of the FPR and PNI were set according to the receiver operating characteristic (ROC) curves, which were based on the overall survival. The FPR-PNI was calculated as follows: the patients with both an elevated FPR and a decreased PNI were assigned a score of 2; the patients with both elevated or decreased values of FPR and PNI were assigned a score of 1; and the patients with both an elevated PNI and a decreased FPR were assigned a score of 0. Subgroup analysis was conducted according to the age group (age <60 years and ≥60 years).
Statistical Analyses
Statistical analyses were performed with SPSS software (version 18.0; SPSS Inc., Chicago, IL, USA) and R 3.6.3 software (Institute for Statistics and Mathematics, Vienna, Austria). ROC curve analysis was used to evaluate the predictive values of FPR, PNI and FPR-PNI for OS, with respect to the sensitivity, cutoff value and specificity. Comparisons of the clinicopathological and laboratory parameters between groups were analyzed by the chi-square test, Mann–Whitney U-test and Kruskal–Wallis H non-parametric test. The OS rate was calculated using the Kaplan–Meier (K-M) method, and the differences in survival between subgroups were performed by the log rank test. The predictive factors for OS were evaluated by univariate and multivariate analyses via using the Cox proportional hazard model, and only those factors with a p value <0.1 in the univariate mode were further analyzed in the multivariate mode. Harrell’s concordance index (C index) and the prognostic nomogram were analyzed by the rms and survival ROC packages, respectively. A two-sided P<0.05 was considered to be statistically different.
Results
Baseline Characteristics of Patients
The clinicopathological characteristics of the 274 GC patients who underwent gastrectomy are summarized in Table 1. The enrolled cohort comprised 182 (66.4%) men and 92 (33.6%) women with a median age of 62.2 years (range, 27–83 years). The results of postoperative histology revealed that the majority of the patients were invasive depth (T3/T4) and lymph node metastases (73.7% and 68.2%, respectively). Based on the 8th American Joint Committee on Cancer (AJCC) TNM staging system, 125 (45.6%) and 149 (54.4%) patients were diagnosed as stage I–II and III. Almost half of them had poor differentiation and received adjuvant chemotherapy (54.7% and 60.6%, respectively). The median follow-up period was 66 months (range, 1–155 months).
 |
Table 1 Relationship Between Clinicopathological Features and FPR, PNI and FPR-PNI |
Evaluation of Prognostic Abilities for FPR, PNI and FPR-PNI
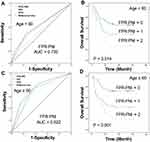
The prognostic abilities of FPR, PNI and FPR-PNI were calculated by ROC curve generation and AUC estimation. We computed the AUC values for the FPR (AUC=0.664; 95% CI=0.599–0.729; P<0.001) and PNI (AUC=0.613; 95% CI=0.546–0.680; P=0.001) (Figure 1A and C). In addition, based on the calculated optimal cutoff values (0.1036 for FPR, 48.525 for PNI), we performed corresponding survival analyses (Figure 1B and D, all P<0.01).
 |
Figure 1 Receiver operating characteristic curve (ROC) analyses of optimal cutoffs and survival analysis for GC patients. (A and B) FPR, (C and D) PNI, (E and F) FPR-PNI. |
Based on the aforementioned results, patients with FPR<0.1036 and PNI≥48.525 were assigned a FPR-PNI score of 0, patients with FPR≥0.1036 or PNI<48.525 were assigned a FPR-PNI score of 1, and patients with FPR≥0.1036 and PNI<48.525 were assigned a FAR-SIRI score of 2. Based on the FPR-PNI system, 81 (29.6%), 106 (38.7%) and 87 (31.7%) of the patients had scores of 0, 1 and 2, respectively. As shown in Figure 1E, the AUC for FPR-PNI was 0.672 (95% CI=0.609–0.736), and GC patients with higher FPR-PNI values had worse prognosis (Figure 1F, P<0.001).
Correlation of FPR, PNI and FPR-PNI with the Clinicopathological Parameters
Of the 274 enrolled patients, 99 patients with FPR<0.1036 and 105 patients with PNI<48.525 were classified into the low FPR group and the low PNI group, whereas 175 with FPR≥0.1036 and 169 with PNI≥48.525 were classified into the high FPR and the high PNI groups. As shown in Table 1, patients in the high FPR group presented as bigger tumor size (p=0.002), Bormann type III–IV (p=0.004), poor differentiation (p=0.036), more lymphatic metastasis (p<0.001) and advanced TNM stage (p<0.001). Patients in the low PNI group presented as aged (p=0.033), bigger tumor size (p=0.002), more lymphatic metastasis (p<0.001) and advanced TNM stage (p< 0.001). In addition, the analysis demonstrated that the preoperative FPR-PNI score was significantly correlated with age, tumor location, tumor size, lymph node status and TNM stage (Table 1).
Prognostic Significance of FPR, PNI and FPR-PNI in GC Patients
The Kaplan–Meier survival curve and log rank test were performed to investigate the association between FPR, PNI, FPR-PNI and postoperative survival time. As shown in Figure 1, both the high FPR group and the low PNI group were associated with poor prognosis of GC patients (p<0.001). Moreover, compared with a low score of FPR-PNI, the GC patients with a higher score of FPR-PNI had shorter survival time.
According to the univariate analysis, age (p=0.031), tumor location (p=0.001), tumor size (p<0.001), Bormann types (p=0.018), operative type (p<0.001), vascular invasion (p=0.001), depth of invasion (p=0.008), lymph node metastasis (p<0.001), TNM stage (p<0.001), PNI (p<0.001), FPR (p<0.001) and FPR-PNI (p<0.001) were identified as poor prognostic factors associated with OS. After multivariate analysis with these selected parameters using the Cox regression model, tumor location (p=0.033), operative type (p=0.001), depth of invasion (p=0.035), TNM stage (p<0.001), adjuvant chemotherapy (p=0.029) and FPR-PNI (p=0.002) were independent prognostic factors for OS in patients with GC (Table 2).
 |
Table 2 Univariate and Multivariate Analysis of Factors for OS |
Subgroup Analysis of FPR-PNI Scores by Age
Compared with the young GC patients, aged patients may have different nutritional and immune states. Therefore, we performed subgroup analysis to assess whether the prognostic accuracy of the scores varied by age <60 and ≥60 years. In the age <60 group, the AUC value was 0.600 (95% CI=0.489–0.711; P=0.077) for the FPR, 0.502 (95% CI=0.389–0.615; P=0.97) for the PNI and 0.622 (95% CI=0.513–0.731; P=0.031) for the FPR-PNI (Figures 2A and E, 3A). In addition, based on the calculated optimal cutoff values (0.1304 for FPR, 43.8 for PNI), survival analyses were performed. As shown in Figures 2B and B, the prognosis of age <60 GC patients was better in the low FPR and low FPR-PNI groups than those in the high FPR and high FPR-PNI groups (P=0.003 and P=0.014, respectively). However, no significant differences in survival time were found between high and low PNI groups (P=0.119) (Figure 2F). According to the multivariate analysis, only vascular invasion and TNM stage were independent prognostic factors for OS in age <60 GC patients (P=0.003 and P=0.002, respectively) (Table 3).
 |
Table 3 Subgroup of Univariate and Multivariate Analysis of Factors for OS by Age |
In the age ≥60 group, the AUC value was 0.694 (95% CI=0.613–0.775; P<0.001) for the FPR, 0.67 (95% CI=0.587–0.752; P<0.001) for the PNI and 0.735 (95% CI=0.658–0.731; P=0.811) for the FPR-PNI (Figures 2C and G, 3C). The optimal cutoff values were 0.1202 for the FPR and 48.65 for the PNI. The Kaplan–Meier survival curve and log rank test showed that the FPR, PNI and FPR-PNI were significantly associated with the prognosis of age ≥60 GC patients (all P<0.001) (Figures 2D and H, 3D). According to the multivariate analysis, operative type (P<0.001), depth of invasion (P=0.020), TNM stage (P<0.001) and FPR-PNI (P<0.001) were independent prognostic factors for OS in age ≥60 GC patients (Table 3).
Prognostic Nomograms for OS of GC
Significant independent indicators based on the multivariate analysis, such as tumor location, operative type, depth of invasion, TNM stage, adjuvant chemotherapy and FPR-PNI, were eventually integrated into the nomogram to predict the 3- and 5-year survival of the GC patients after surgical resection. The C index of the nomogram was 0.736 (Figure 4A). In the age ≥60 group, operative type, depth of invasion, TNM stage and FPR-PNI were embedded in the nomogram, the C index of which was 0.742 (Figure 4B).
 |
Figure 4 Prognostic nomograms with FPR-PNI score for predicting 3-year and 5-year OS in GC patients. (A) All GC patients, (B) age ≥60 GC patients. |
Discussion
To the best of our knowledge, this study firstly investigated the prognostic significance of the preoperative FPR-PNI score in gastric cancer patients. The results showed that a high preoperative FPR-PNI score was significantly correlated with a relatively higher risk of tumor progression and worse prognosis. In addition, subgroup analysis revealed that the diagnostic efficiency of FPR-PNI in the age ≥60 group was more significant than that in the age <60 group.
Systemic inflammation response (SIR) and nutrition status have been recognized significantly correlated with tumor progression and prognosis in various malignancies, including gastric cancer.25–28 Fibrinogen, as an important component of the coagulation cascade, plays an important role in SIR and tumor progression.29–31 Relevant studies indicated that elevated preoperative plasma fibrinogen was associated with tumor progression, metastasis and poor overall survival in GC patients.13,32 Serum Alb and pAlb are the most widely used markers to reflect nutritional status. Low levels of Alb and pAlb levels could result in malnutrition and confusion of immune responses, which could influence prognosis of GC.6,33 Most recently, Zhang et al investigated the prognostic significance of the preoperative FPR (fibrinogen/pre-albumin ratio) in GC patients. Their results showed that an elevated FPR was significantly associated with larger tumor size, deeper tumor invasion and more lymph node metastasis, which could be an independent prognostic factor for GC patients.23 What is more, Wu et al created a cumulative score based on preoperative fibrinogen and pre-albumin (FP score), which could be an independent predictor for disease-free survival (DFS) and OS in patients with resectable GC.34 Compared with their study, our results indicated that the GC patients with high FPR value presented as larger tumor size, Bormann type III–IV, poor differentiation, more lymphatic metastasis and advanced TNM stage. In addition, a high FPR value was correlated with poor survival time, but not an independent prognostic factor in GC patients. Lymphocytes play an important role in killing tumor cells by inducing cytotoxic cell death and host immune responses mediated by cytokine production. Previous studies showed that preoperative lymphopenia was closely related to the poor overall survival and disease-free survival rates of GC.35,36 Thus, the combination of albumin and lymphocyte, which is known as the PNI, has been considered a good prognostic marker for cancer patients.19 Some earlier studies have shown that the preoperative PNI value, serving as a useful nutritional determinant, could independently predict the OS in patients with various types of cancers, including GC.22,37,38 Consistent with their results, we demonstrated in the present study that the low PNI values were associated with aged patients, larger tumor size, more lymphatic metastasis, advanced TNM stage and poor prognosis. We believe that low PNI values in GC patients may account for fatigue, indigestion, inadequate caloric intake, fueling physical inactivity and immune dysfunction, which contribute to earlier tumor recurrence and shorter survival time.
As effective prognosis factors, the biomarkers should reflect inflammation and nutritional conditions at the same time. Although the FPR and PNI are more accurate than serum fibrinogen, Alb, pAlb and lymphocyte count alone, the two biomarkers are still not independent prognostic factors in GC patients according to our study. Therefore, we proposed the FPR-PNI score in combination with the FPR and PNI, which might reduce the influence of confounding factors, to investigate its prognostic impact in GC patients. According to our definition of the FPR-PNI, the GC patients included in this study were effectively divided into three different risk groups. The AUC of FPR-PNI is larger than that of FPR and PNI alone, suggesting the prediction efficiency of FPR-PNI is better than the other two. As shown in our study, high FPR-PNI scores were associated with elderly patients, lower tumor location, larger tumor size, lymph node metastasis and advanced TNM stage. Moreover, a high FPR-PNI score predicted poor survival time and could serve as an independent prognostic factor in GC patients. Clinicians need to pay more attention to patients with a high FPR-PNI score and provide appropriate interventions, such as sufficient nutritional support and more aggressive postoperative adjuvant treatment.
As we know, elderly GC patients, who are often malnourished and in a low state of immunity, with various comorbid conditions, have a high incidence of death from other diseases after surgeries.4,5,39-41 Previous studies showed that the OS of elderly patients with a lower PNI score was shorter than the young.42 The PNI could be a significant independent prognostic factor for predicting OS in elderly GC patients.43 Considering the difference of nutritional and immune states in elderly and young patients, which may affect the predictive accuracy of FPR-PNI in the prognosis of GC patients, we conducted the subgroup analysis for age <60 and ≥60 groups. As shown in the results, the prediction efficiency of the FPR-PNI score was significantly higher than the FPR and PNI alone in the elderly group. However, in the young group, the FPR-PNI score seems to be no better than the FPR and PNI alone. On the other hand, the FPR-PNI score was an independent prognostic factor for OS in age ≥60 GC patients, but not in age <60 GC patients. These results above suggest that the preoperative FPR-PNI score could be one of the important factors for preoperative evaluation and prognosis. In addition, perioperative rehabilitation and nutritional support can effectively improve the long-term outcomes in elderly GC patients with a high FPR-PNI score.
There were some limitations that need to be addressed in our study. Firstly, this was a single-center retrospective design, which was more susceptible to contribute to some biases. Secondly, different postoperative treatments in GC patients may influence the survival results that could make a difference in the predictive accuracy of the FPR-PNI. Thirdly, despite OS being widely known as the standard prognosis index in GC cancer, we failed to comprehensively evaluate the prognosis of GC patients owing to the lack of sufficient data on disease-free survival. Therefore, our current findings need to be verified in prospective and multicenter studies with sufficient clinicopathological and survival data.
Conclusions
In conclusion, a high score of FPR-PNI is associated with advanced stages and poor prognosis, which is an independent risk factor for overall survival in elderly GC patients. The FPR-PNI score is a convenient, inexpensive, reliable marker which can be used as a screening and prognostic indicator for elderly GC patients, providing a reference for adjuvant therapy and long-term management after surgery.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34. doi:10.3322/caac.21551
2. Soerjomataram I, Lortet-Tieulent J, Parkin DM, et al. Global burden of cancer in 2008: a systematic analysis of disability-adjusted life-years in 12 world regions. Lancet. 2012;380(9856):1840–1850. doi:10.1016/S0140-6736(12)60919-2
3. Takeshita H, Ichikawa D, Komatsu S, et al. Surgical outcomes of gastrectomy for elderly patients with gastric cancer. World J Surg. 2013;37(12):2891–2898. doi:10.1007/s00268-013-2210-7
4. Kouzu K, Tsujimoto H, Hiraki S, et al. Efficacy of totally laparoscopic distal gastrectomy for gastric cancer in elderly patients. Mol Clin Oncol. 2016;4(6):976–982. doi:10.3892/mco.2016.843
5. Gretschel S, Estevez-Schwarz L, Hunerbein M, Schneider U, Schlag PM. Gastric cancer surgery in elderly patients. World J Surg. 2006;30(8):1468–1474. doi:10.1007/s00268-005-0633-5
6. Sun KY, Xu JB, Chen SL, et al. Novel immunological and nutritional-based prognostic index for gastric cancer. World J Gastroenterol. 2015;21(19):5961–5971. doi:10.3748/wjg.v21.i19.5961
7. Nozoe T, Ninomiya M, Maeda T, Matsukuma A, Nakashima H, Ezaki T. Prognostic nutritional index: a tool to predict the biological aggressiveness of gastric carcinoma. Surg Today. 2010;40(5):440–443. doi:10.1007/s00595-009-4065-y
8. Falanga A, Santoro A, Labianca R, et al. Hypercoagulation screening as an innovative tool for risk assessment, early diagnosis and prognosis in cancer: the hypercan study. Thromb Res. 2016;140(Suppl 1):S5559. doi:10.1016/S0049-3848(16)30099-8
9. Repetto O, De Re V. Coagulation and fibrinolysis in gastric cancer. Ann N Y Acad Sci. 2017;1404(1):27–48. doi:10.1111/nyas.13454
10. Chang WJ, Du Y, Zhao X, Ma LY, Cao GW. Inflammation-related factors predicting prognosis of gastric cancer. World J Gastroenterol. 2014;20(16):4586–4596. doi:10.3748/wjg.v20.i16.4586
11. Pan QX, Su ZJ, Zhang JH, Wang CR, Ke SY. A comparison of the prognostic value of preoperative inflammation-based scores and TNM stage in patients with gastric cancer. Onco Targets Ther. 2015;8:1375–1385. doi:10.2147/OTT.S82437
12. Wang K, Diao F, Ye Z, et al. Prognostic value of systemic immune-inflammation index in patients with gastric cancer. Chin J Cancer. 2017;36(1):75. doi:10.1186/s40880-017-0243-2
13. Kijima T, Arigami T, Uchikado Y, et al. Combined fibrinogen and neutrophil-lymphocyte ratio as a prognostic marker of advanced esophageal squamous cell carcinoma. Cancer Sci. 2017;108(2):193–199. doi:10.1111/cas.13127
14. Kanda M, Tanaka C, Kobayashi D, et al. Proposal of the coagulation score as a predictor for short-term and long-term outcomes of patients with resectable gastric cancer. Ann Surg Oncol. 2017;24(2):502–509. doi:10.1245/s10434-016-5544-1
15. Guan X, Gong M, Wang X, et al. Low preoperative fibrinogen level is risk factor for neurological complications in acute aortic dissection. Medicine. 2018;97(21):e10830. doi:10.1097/MD.0000000000010830
16. Yamashita K, Ushiku H, Katada N, et al. Reduced preoperative serum albumin and absence of peritoneal dissemination may be predictive factors for long-term survival with advanced gastric cancer with positive cytology test. Eur J Surg Oncol. 2015;41(10):1324–1332. doi:10.1016/j.ejso.2015.05.021
17. Han WX, Chen ZM, Wei ZJ, Xu AM. Preoperative pre-albumin predicts prognosis of patients after gastrectomy for adenocarcinoma of esophagogastric junction. World J Surg Oncol. 2016;14(1):279. doi:10.1186/s12957-016-1035-x
18. Shen Q, Liu W, Quan H, et al. Prealbumin and lymphocyte-based prognostic score, a new tool for predicting long-term survival after curative resection of stage II/III gastric cancer. Br J Nutr. 2018;120(12):1359–1369. doi:10.1017/S0007114518002854
19. ZM G, Wang RY, Deng P, et al. TNM-PNI: a novel prognostic scoring system for patients with gastric cancer and curative D2 resection. Cancer Manag Res. 2018;10:2925–2933. doi:10.2147/CMAR.S169206
20. Luo Z, Zhou L, Balde AI, et al. Prognostic impact of preoperative prognostic nutritional index in resected advanced gastric cancer: A multicenter propensity score analysis. Eur J Surg Oncol. 2019;45(3):425–431. doi:10.1016/j.ejso.2018.09.004
21. Lee JY, Kim HI, Kim YN, et al. Clinical significance of the prognostic nutritional index for predicting short- and long-term surgical outcomes after gastrectomy: a retrospective analysis of 7781 gastric cancer patients. Medicine. 2016;95(18):e3539. doi:10.1097/MD.0000000000003539
22. Sakurai K, Ohira M, Tamura T, et al. Predictive potential of preoperative nutritional status in long-term outcome projections for patients with gastric cancer. Ann Surg Oncol. 2016;23(2):525–533. doi:10.1245/s10434-015-4814-7
23. Zhang J, Li SQ, Liao ZH, et al. Prognostic value of a novel FPR biomarker in patients with surgical stage II and III gastric cancer. Oncotarget. 2017;8(43):75195–75205. doi:10.18632/oncotarget.20661
24. Zhang J, Ding Y, Wang W, et al. Combining the fibrinogen/albumin ratio and systemic inflammation response index predicts survival in resectable gastric cancer. Gastroenterol Res Pract. 2020;2020:3207345. doi:10.1155/2020/3207345
25. Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001;357(9255):539–545. doi:10.1016/S0140-6736(00)04046-0
26. Sachlova M, Majek O, Tucek S. Prognostic value of scores based on malnutrition or systemic inflammatory response in patients with metastatic or recurrent gastric cancer. Nutr Cancer. 2014;66(8):1362–1370. doi:10.1080/01635581.2014.956261
27. Seo KW, Yoon KY. [Nutritional assessment and perioperative nutritional support in gastric cancer patients]. Korean J Gastroenterol. 2013;61(4):186–190. Korean. doi:10.4166/kjg.2013.61.4.186
28. Dias Rodrigues V, Barroso de Pinho N, Abdelhay E, Viola JP, Correia MI, Brum Martucci R. Nutrition and immune-modulatory intervention in surgical patients with gastric cancer. Nutr Clin Pract. 2017;32(1):122–129. doi:10.1177/0884533616653807
29. Tang L, Liu K, Wang J, Wang C, Zhao P, Liu J. High preoperative plasma fibrinogen levels are associated with distant metastases and impaired prognosis after curative resection in patients with colorectal cancer. J Surg Oncol. 2010;102(5):428–432. doi:10.1002/jso.21668
30. Jiang HG, Li J, Shi SB, et al. Value of fibrinogen and D-dimer in predicting recurrence and metastasis after radical surgery for non-small cell lung cancer. Med Oncol. 2014;31(7):22. doi:10.1007/s12032-014-0022-8
31. Sheng L, Luo M, Sun X, Lin N, Mao W, Su D. Serum fibrinogen is an independent prognostic factor in operable nonsmall cell lung cancer. Int J Cancer. 2013;133(11):2720–2725. doi:10.1002/ijc.28284
32. Suzuki T, Shimada H, Nanami T, et al. Hyperfibrinogenemia is associated with inflammatory mediators and poor prognosis in patients with gastric cancer. Surg Today. 2016;46(12):1394–1401. doi:10.1007/s00595-016-1339-z
33. Li B, Liu HY, Guo SH, Sun P, Gong FM, Jia BQ. Impact of early postoperative enteral nutrition on clinical outcomes in patients with gastric cancer. Genet Mol Res. 2015;14(2):7136–7141. doi:10.4238/2015.June.29.7
34. Wu ZJ, Xu H, Wang R, et al. Cumulative score based on preoperative fibrinogen and pre-albumin could predict long-term survival for patients with resectable gastric cancer. J Cancer. 2019;10(25):6244–6251. doi:10.7150/jca.35157
35. Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–444. doi:10.1038/nature07205
36. Quigley DA, Kristensen V. Predicting prognosis and therapeutic response from interactions between lymphocytes and tumor cells. Mol Oncol. 2015;9(10):2054–2062. doi:10.1016/j.molonc.2015.10.003
37. Nozoe T, Kohno M, Iguchi T, et al. The prognostic nutritional index can be a prognostic indicator in colorectal carcinoma. Surg Today. 2012;42(6):532–535. doi:10.1007/s00595-011-0061-0
38. Kanda M, Fujii T, Kodera Y, Nagai S, Takeda S, Nakao A. Nutritional predictors of postoperative outcome in pancreatic cancer. Br J Surg. 2011;98(2):268–274. doi:10.1002/bjs.7305
39. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi:10.3322/caac.21492
40. Kim MG, Kim HS, Kim BS, Kwon SJ. The impact of old age on surgical outcomes of totally laparoscopic gastrectomy for gastric cancer. Surg Endosc. 2013;27(11):3990–3997. doi:10.1007/s00464-013-3073-6
41. Sakurai K, Muguruma K, Nagahara H, et al. The outcome of surgical treatment for elderly patients with gastric carcinoma. J Surg Oncol. 2015;111(7):848–854. doi:10.1002/jso.23896
42. Sugawara K, Aikou S, Yajima S, et al. Pre- and post-operative low prognostic nutritional index influences survival in older patients with gastric carcinoma. J Geriatr Oncol. 2020;11:989–996. doi:10.1016/j.jgo.2020.02.007
43. Veerasamy N, Takamasa A, Murugan R, et al. Chemical separation of uranium and precise measurement of (234)U/(238)U and (235)U/(238)U ratios in soil samples using multi collector inductively coupled plasma mass spectrometry. Molecules. 2020;25:9. doi:10.3390/molecules25092138
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.