Back to Journals » Clinical and Experimental Gastroenterology » Volume 15
Combined Pharmacological and Endoscopic Treatment for Worsening Gastroesophageal Varices in Patients with Cirrhosis
Authors Pepe V, Angeli P, Di Pascoli M
Received 30 December 2021
Accepted for publication 24 March 2022
Published 22 April 2022 Volume 2022:15 Pages 59—65
DOI https://doi.org/10.2147/CEG.S355392
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Wing-Kin Syn
Veronica Pepe, Paolo Angeli, Marco Di Pascoli
Department of Medicine, Unit of Internal Medicine and Hepatology (UIMH), University of Padova, Padua, Italy
Correspondence: Marco Di Pascoli, Department of Medicine, Unit of Internal Medicine and Hepatology (UIMH), University of Padova, Padua, Italy, Tel +0039 0498212274, Email [email protected]
Background: At the present time, in patients with liver cirrhosis and gastroesophageal varices, primary prophylaxis of variceal bleeding made with combination therapy with non-selective β-blockers (NSBBs) and endoscopic band ligation (EBL) is not recommended. The aim of this study was to evaluate if patients with worsening varices while on NSBBs regimen benefit, in terms of bleeding and survival, from adding treatment with EBL.
Methods: Patients with cirrhosis and endoscopic finding of gastroesophageal varices with high risk feature (increased variceal size and/or development of red signs) during primary prophylaxis with NSBBs, followed at the Unit of Internal Medicine and Hepatology, University and General Hospital of Padova, Italy, from 2012 to 2019, were retrospectively evaluated. When an increased bleeding risk of the varices was confirmed, patients maintained the pharmacological therapy alone or underwent also EBL. The primary endpoint of the study was the rate of variceal bleeding, the secondary endpoint was mortality at 30 months.
Results: Compared to patients treated only with NSBBs (n=56), in patients treated also with EBL (n=45), the 30‐month probability of variceal bleeding (29.1% vs 5.1%; P =0.036) was significantly reduced, while the probability of survival was similar (59.6% vs 65.7%; P=0.61). On multivariate analysis, treatment with EBL was found to be a weak protective factor for mortality (HR 0.47, P=0.044).
Conclusion: In patients with liver cirrhosis, when varices show endoscopic feature of increased haemorrhagic risk, adding EBL to NSBBs is effective in reducing the probability of first bleeding.
Keywords: non-selective β-blockers, endoscopic band ligation, variceal bleeding, digestive bleeding, portal hypertension, endoscopic screening
Introduction
In liver cirrhosis, gastroesophageal varices are part of the porto-systemic collaterals that develop as a consequence of portal hypertension.1 In patients with cirrhosis, varices are detected in the 50% of them at diagnosis, they develop at a rate of approximately 8% per year and small varices increase in size at a similar rate.2 Variceal bleeding is one of the most dreadful complications of cirrhosis and is the consequence of variceal rupture due to increased wall tension as a result of increased intravariceal pressure, increased diameter of the varices, and reduced wall thickness. The variceal wall thickness can be evaluated visually by the presence of red wale markings, which are signs of particularly thin variceal wall.3 Therefore, when it comes to the assessment of the risk of bleeding with esophagogastroduodenoscopy (EGD), size and the presence of red signs are particularly important.
The cornerstone of primary prophylaxis of variceal bleeding are nonselective β-blockers (NSBBs) such as propranolol, nadolol and carvedilol. NSBBs reduce portal pressure by decreasing cardiac output (β1 effect) and by producing splanchnic vasoconstriction (β2 effect), thereby reducing portal blood flow. Besides, carvedilol has α1-blocking properties and has been associated with greater reduction in portal pressure. Regular measurement of portal pressure gradient to monitor and guide β -blocking therapy is not used, instead surrogate markers are used, such as a decrease in heart rate of 25% below baseline, heart rate of 55–60 beats per minute or maximally tolerated dose.2 Primary prophylaxis with NSBBs is indicated in patients with small varices and high-risk features (ie red signs or Child-Pugh C class), since they are at greater risk of bleeding.4,5 For patients with medium/large varices, both NSBBs and endoscopic band ligation (EBL) have shown to be equally effective in preventing first bleeding.6 One RCT compared the combination of NSBBs plus EBL versus EBL alone, showing no differences in the incidence of bleeding or death between the two groups, which is therefore not recommended by the latest American guidelines.7,8 The choice between NSBB and EBL depends on factors such as patient preference, contraindications or adverse events to NSBB. On the other hand, EBL does not affect portal hypertension, thus it does not reduce nor prevent other complications, supporting overall primary preference for NSBBs.
In patients with varices in whom there is indication for a primary prophylaxis regimen with medical therapy, experts indicate that EGD screening is no longer necessary once the patient has started medical therapy.8 Currently, there are no data about any possible benefit of adding, in the primary prophylaxis scenario, EBL to the NSBBs regimen when observing varices with an increased bleeding risk during the endoscopic follow-up of patients with cirrhosis. Adding a local treatment such EBL to a systemic pharmacological treatment in a patient with worsening varices despite an ongoing primary prophylaxis, theoretically could reduce the bleeding rate. Therefore, the aim of this study was to evaluate whether patients with worsening varices benefit, in terms of bleeding and survival, from adding EBL to the ongoing primary prophylactic treatment with NSBBs.
Patients and Methods
This is a retrospective study in which patients with cirrhosis and gastroesophageal varices on primary prophylaxis with NSBBs for variceal haemorrhage, followed at the Outpatients Clinic of the Unit of Internal Medicine and Hepatology (UIMH), University and General Hospital of Padova, Italy, from 2012 to 2019, were screened. Patients on primary prophylaxis with NSBBs, were screened with EGD one year after starting the therapy. EGD was performed by a team of endoscopists of the same Hospital, to detect the increase in size of varices and the development of red signs. Inclusion criteria were as follows: (a) cirrhosis as diagnosed by liver biopsy or clinical, biochemical, ultrasound and/or endoscopic findings; (b) age >18 years; (c) ongoing primary prophylaxis for variceal bleeding with NSBBs; (d) endoscopic finding of variceal worsening, defined as an increase in variceal size (from F1 to F2/F3 or from small to medium/large) and/or development of red signs. They were excluded from this analysis: (a) patients in whom NSBBs therapy was not optimized according to the latest guidelines (n=4); (b) patients affected by hepatocellular carcinoma (HCC) beyond Milan criteria or severe extrahepatic diseases (n=3).2,8 Patients, were treated according to hepatologist preference (one physician maintained the pharmacological therapy alone, a second physician opted for the combined NSBBs and EBL approach) and divided in two groups: (1) patients in whom pharmacological therapy was maintained alone (n= 56); and (2) patients in whom EBL was performed while maintaining pharmacological therapy (n=45); in these patients endoscopic follow-up was performed according to guidelines and in case of variceal recurrence a new cycle of EBL was repeated (n=2).
At the time of the inclusion, coinciding with the medical check-up at our Outpatient Clinic when the endoscopic finding of variceal worsening was registered, the following parameters were recorded: patient demographics, clinical and laboratory data, ongoing therapy with NSBBs and prognostic scores (ie, Child-Pugh and MELD-Na scores).
Patients were followed-up for 30 months or till the end of the study, liver transplantation or death. The primary endpoint of the study was the rate of variceal bleeding, defined as hematemesis and/or melena together with either endoscopic visualization of blood emitted from oesophageal varices; varices with red or white plug; presence of varices together with blood in the stomach and no other source of bleeding. The secondary endpoint was 30‐month mortality.
The study was approved by the Ethics Committee of the University and General Hospital of Padova. Due to the retrospective nature of the study, informed consent of the patients was not required by the Ethics Committee.
Statistical Analysis
Continuous data are reported as mean and standard deviation (SD), while categorical variables are reported as frequency and proportion.
Comparisons between groups were performed through the Student t test for normally distributed continuous data, the Mann‐Whitney U-test for non‐normally distributed continuous data, and the chi‐square test or Fisher’s exact test for categorical data.
Incidence of bleeding and mortality was calculated using the Kaplan‐Meier method and compared with the log‐rank test. Patients who died or were transplanted during the follow‐up were censored at the time of death or transplant. In order to deal with the presence of a competitive risk both for bleeding risk and for mortality two separate multivariate Cox regression analyses were performed using a competing risk approach with the Fine and Gray method and results expressed as P‐value, sub-distribution hazard ratios (sHR) and their 95% confidence intervals (95% CI). In the first analysis, we considered as competing events for bleeding the mortality and the liver transplant while in the second regressions the competing events for mortality were only the liver transplant. Variables found to be more strictly associated with in‐hospital mortality in the univariate analysis were included in a multivariate analysis in order to minimize the Akaike Information Criterion (AIC) index. When scores of liver disease were included in the model, their components were excluded to avoid multicollinearity.
Statistical analyses of the data were performed using R software 4.0 version (R Core Team 2020) with survival and cmprsk packages. All tests were two‐tailed, and P < 0.05 was considered statistically significant.
Results
Patients
A total of 101 patients with cirrhosis and worsening gastroesophageal varices during follow-up were included in the study. Fifty-six patients were treated with pharmacological therapy alone while 45 patients also underwent EBL. The mean follow-up of all patients was of 18.5±11.5 months (16.8±12 months in the NSBBs group and 20.3±10.6 months in the NSBBs + EBL group; P=NS).
No significant difference in clinical and laboratory data was present at baseline between the two groups (Table 1).
No differences among the two groups were observed with regard to the distribution of the type and the average dose used of NSBBs. In the NSBBs only group, the beta-blocker most frequently used was propranolol (82.2%) at the average dose of 43.1 mg/day; nadolol was used in the 8.9% of patients at the average dose of 48 mg/day; carvedilol was used in the 8.9% of patients as well, at the average dose of 31.3 mg/day. Similarly, in the NSBBs+EBL group, propranolol was the most used beta-blocker (70.5%) at the average dose of 45.8 mg/day; nadolol was used in the 11.4% of patients at the average dose of 44 mg/day; and carvedilol was used in 18.1% of patients at the average dose of 25 mg/day).
During the follow-up of 30 months, 9 (16.1%) patients in the NSBBs only group, and 6 (13.3%) in the NSBBs+EBL group underwent liver transplantation (P=NS).
Variceal Bleeding
During the follow-up period, bleeding from varices occurred in 10 patients in the group treated with NSBBs alone and in 2 patients who underwent also EBL. Compared to patients treated only with NSBBs, in patients treated also with EBL, the 30‐month probability of variceal bleeding (29.1% vs 5.1%; P =0.036) was significantly reduced (Figure 1).
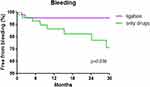 |
Figure 1 Bleeding free rate in the NSBBs only group and in the NSBB+EBL group. |
Taking into account of mortality and liver transplant as competitive events, Fine and Gray regression model for bleeding incidence confirmed that patients treated also with EBL showed a reduced risk of bleeding (sHR: 0.24; 95% CI: 0.05–1.09) though the low number of bleedings (12) implied a limited power and a non-statistical significant p-value (P: 0.065). Moreover, the basal characteristics of patients shown in Table 1 were not found to be associated with the risk of bleeding, considering the dropping in the AIC values (Table 2).
 |
Table 2 Terms Sequentially Included in the Fine and Gray Regression Models |
Survival
During the follow-up, 18 patients in the NSBBs only group and 13 in the NSBBs + EBL group died. Comparing the two groups by the Kaplan-Meier method, the 30‐month probability of survival was similar (59.6% in patients treated only with NSBBs, 65.7% in patients treated also with EBL; P = 0.61) (Figure 2). Only one patient, in the NSBBs+EBL group, died because of complications of variceal bleeding.
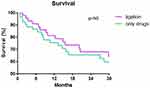 |
Figure 2 Survival rate in the NSBB only group and in the NSBB+EBL group. |
On multivariate analysis, age (HR 1.07, P<0.001) and MELD-Na > 14 (HR 5.36, P<0.001) were found to be independent predictors of mortality, while treatment with EBL was found to be a weak protective factor for mortality (HR 0.47, P=0.044) (Table 2 and 3).
 |
Table 3 Estimated sHR for Variceal Bleeding (Model 1) and Mortality (Model 2) by a Fine and Gray Regression Model |
Discussion
Amongst the complications of cirrhosis, acute variceal bleeding is one the most feared, as it is sudden, requires an intensive and prompt medical intervention and is charged with a variety of serious complications and a high mortality.9,10 Thus, significant efforts have been made during the past decades to evaluate the best prophylactic strategy. The latest guidelines recommend the use of NSBBs for patients with small varices and either NSBBs or EBL for patients with medium/large varices. Medical and endoscopic therapy are equivalent in preventing the first bleeding episode, and a few trials have evaluated the effect of the combination therapy compared to monotherapy.11 In 2005 Sarin et al randomized patients to receive EBL plus propranolol or EBL alone: during a follow-up period of 12 months, a non-significant difference in the actuarial probability of bleeding and bleed-related deaths was observed in the two groups.12 Similarly, a retrospective study showed that adding NSBBs to EBL for primary prophylaxis did not modify bleeding rate nor mortality at 16 months. Besides, the two groups of patients were compared to another group of patients with cirrhosis treated with NSBBs only, from a previous study from the same Centre, and again no difference in bleeding rate or mortality was found.13 On the other hand, another retrospective study comparing bleeding rate and mortality in 504 cirrhotic patients with cirrhosis followed-up for a long period (mean 82 months) found that patients with propranolol plus EBL had a lower probability of first variceal bleeding with no difference in mortality compared to the ones in propranolol only regimen.14 It must be considered, though, that in this study the mean dose of propranolol administered was quite low, so the benefit of adding EBL to the NSBBs in terms of bleeding could result from an underlying inadequate beta-blocking.
According to international guidelines, once that a patient has started medical therapy, endoscopic screening is no more necessary, and no previous data have evaluated the possible benefits of adding EBL to the NSBBs regimen when an increased bleeding risk of the varices has been observed during the endoscopic follow-up of patients with cirrhosis.4 Therefore, the aim of this study was to evaluate if patients with worsening varices, defined as an increase in variceal size and the development of red signs, benefit, in terms of bleeding and survival, from adding EBL to the ongoing primary prophylactic treatment with NSBBs.
Interestingly, in our study, in patients treated only with NSBBs, the risk of first bleeding episode from varices during follow-up was similar to the one showed in the meta-analysis by D’Amico et al.15 In the EBL plus NSBBs group, the number of bleeding episodes at 30 months was significantly lower than in NSBBs only group, while the survival rate was almost similar in the two groups, although a slight benefit in the NSBBs plus EBL group was observed at the multivariate analysis. The discrepancy between the prevalence of these two events in the two groups may be explained by a low rate of bleeding-related deaths due to a management of acute variceal bleeding optimized according to international guidelines, with services of urgent endoscopy available 24 hours a day, 7 days a week. If prospective randomized multicentric studies would confirm these data, these new insights could lead to a novel approach to the endoscopic follow-up and the subsequent treatment for primary prophylaxis of variceal bleeding in patients with cirrhosis.
Our study has limitations. The main ones are that it was conducted retrospectively, the decision to administer either NSBBs alone or NSBBs plus EBL depended on the choice of the single clinician and the interpretation of varices size may be subjective according to different endoscopists. Secondly, our study is monocentric and includes a relatively small group of patients. Moreover, the cost-effectiveness of this diagnostic and therapeutic approach has not been evaluated. Therefore, to address properly this relevant issue, only prospective clinical studies can be definitive.
In conclusion, our study suggests that a strategy to implement the primary prophylaxis of oesophageal varices in patients with liver cirrhosis, adding EBL to NSBBs when at endoscopy varices show worsening features that could indicate an increased haemorrhagic risk, is effective in reducing the probability of first bleeding and might be effective in reducing mortality as well. If this benefit will be eventually confirmed in randomized studies, it could be necessary to reconsider the endoscopic screening of varices, which, at the present time, is not recommended once the patient has an ongoing primary prophylaxis with NSBBs.
Abbreviations
EGD, esophagogastroduodenoscopy; NSBBs, nonselective β-blockers; EBL, endoscopic band ligation.
The study was approved by the local Ethical Committee
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Acknowledgments
This article is present on a preprint server of Research square website and can be accessed on https://www.researchsquare.com/article/rs-876974/v1. This article is not published nor is under publication elsewhere.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Dell’Era A, Bosch J. Review article: the relevance of portal pressure and other risk factors in acute gastro-oesophageal variceal bleeding. Aliment Pharmacol Ther. 2004;20(Suppl 3):8–17.
2. Gonzalez HV, Sanchez W. Esophageal Varices: primary and Secondary Prophylaxis. In: Cardenas A, Keaveny A, editors. Complications of Cirrhosis. Springer International Publishing Switzerland; 2015:83–89.
3. Hilzenrat N, Sherker AH. Esophageal varices: pathophysiology, approach, and clinical dilemmas. Int J Hepatol. 2012;2012:795063.
4. De Franchis R, Baveno V. Faculty. Expanding consensus in portal hypertension: report of the Baveno VI Consensus Workshop: stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015;63(3):743–752.
5. Merkel C, Marin R, Angeli P, et al. A placebo-controlled clinical trial of nadolol in the prophylaxis of growth of small esophageal varices in cirrhosis. Gastroenterology. 2004;127:476.
6. Gluud LL, Krag A. Banding ligation versus beta-blockers for primary prevention in oesophageal varices in adults. Cochrane Database Syst Rev. 2012;1(8):CD004544.
7. Sarin SK, Wadhawan M, Agarwal SR, Tyagi P, Sharma BC. Endoscopic variceal ligation plus propranolol versus endoscopic variceal ligation alone in primary prophylaxis of variceal bleeding. Am J Gastroenterol. 2005;100:797–804.
8. Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65(1):310–335.
9. Carbonell N, Pauwels A, Serfaty L, Fourdan O, Levy VG, Poupon R. Improved survival after variceal bleeding in patients with cirrhosis over the past two decades. Hepatology. 2004;40:652–659.
10. D’Amico G, Pasta L, Morabito A, et al. Competing risks and prognostic stages of cirrhosis: a 25-year inception cohort study of 494 patients. Aliment Pharmacol Ther. 2014;39:1180–1193.
11. European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018;69(2):406–460.
12. Sarin SK, Wadhawan M, Agarwal SR, Tyagi P, Sharma BC. Endoscopic variceal ligation plus propranolol versus endoscopic variceal ligation alone in primary prophylaxis of variceal bleeding. Am J Gastroenterol. 2005;100(4):797–804.
13. Pfisterer N, Dexheimer C, Fuchs EM, et al. Betablockers do not increase efficacy of band ligation in primary prophylaxis but they improve survival in secondary prophylaxis of variceal bleeding. Aliment Pharmacol Ther. 2018;47(7):966–979.
14. Je D, Paik YH, Gwak GY, et al. The comparison of esophageal variceal ligation plus propranolol versus propranolol alone for the primary prophylaxis of esophageal variceal bleeding. Clin Mol Hepatol. 2014;20(3):283–290.
15. D’Amico G, Pagliaro L, Bosch J. Pharmacological treatment of portal hypertension: an evidence-based approach. Semin Liver Dis. 1999;19:475–505.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

