Back to Journals » Cancer Management and Research » Volume 10
Combined microwave ablation and minimally invasive open decompression for the management of thoracic metastasis in breast cancer
Received 11 December 2017
Accepted for publication 9 April 2018
Published 31 May 2018 Volume 2018:10 Pages 1397—1401
DOI https://doi.org/10.2147/CMAR.S159561
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Lu-Zhe Sun
Bin Liu,1,* Zhenchao Yuan,1,* Chang yuan Wei2
1Department of Bone and Soft Tissue Neurosurgery, 2Department of Breast Tumor Surgery, Affiliated Tumor Hospital of Guangxi Medical University, Nanning, China
*These authors contributed equally to this work
Objective: The incidence rate of thoracic metastasis from breast cancer is increasing. Microwave ablation is one type of clinical therapy used to treat metastatic spine disease, although it can cause protein denaturation and immediate cell death, and coagulative necrosis can occur. Minimally invasive open decompression is associated with lower rates of surgical complications in comparison to traditional open surgery. Therefore, it is an alternative therapeutic option for spinal metastases. This study aimed to assess the efficacy of microwave ablation with minimally invasive open decompression in the management of breast cancer patients with thoracic metastasis.
Methods: This single-institution retrospective study investigated 23 cases of thoracic metastasis from breast cancer treated with combined microwave ablation and minimally invasive open decompression. Patients that presented with indications for surgery underwent surgical treatment. Data were collected for pain scores, the Frankel Grade classification system for acute spinal injury, the Karnofsky performance status (KPS) scale and complications due to treatment.
Results: Of the 23 patients included in this study, all were successfully treated with microwave ablation and minimal invasive open decompression using our metrics. Of those, 18 patients (78.3%) showed improvement in their KPS results while 5 (21.7%) had alleviation of KPS. All 23 patients showed improvement in their Frankel Grade, suggesting improved neurological function following surgery. Most of the patients reported pain relief. Postoperative complications occurred in 4 patients.
Conclusion: Microwave ablation combined with minimally invasive open decompression therapy for breast cancer patients with thoracic metastatic tumors is an alternative treatment that maintains or improves functional outcome in comparison to open surgery.
Keywords: breast cancer, thoracic metastatic tumors, microwave ablation, minimally invasive open decompression
Introduction
The prevalence of breast cancer in China is increasing. Fortunately, advances in systemic therapies and surgical techniques followed by radiotherapy have prolonged survival in patients who develop metastatic spinal cancer. However, the incidence of complications following open surgery increased by 25% over the same period.1 Complications mainly include extensive blood loss and postoperative-related infection.2–4 Minimally invasive open decompression can reduce the impact on the spine and alleviate pain, which can promote early movement and rehabilitation. With the development of new technologies and therapies, such as microwave ablation, it is now possible to provide an alternative to open surgery to treat spinal metastases.
Microwave ablation applies electromagnetic microwaves to the target tissue via an antenna, resulting in the agitation of ionic molecules and frictional heat. Subsequently, the target tissue undergoes coagulative necrosis. Microwave ablation is particularly effective against osteoblastic lesions. However, it has some disadvantages, including potential irreversible damage to the surrounding tissue and structures due to overheating. Therefore, strict temperature control during metastatic tumor ablation is imperative in order to prevent spinal injury. Despite this, research indicates that microwave ablation is an effective method for treating spinal metastasis.5,6 In comparison, open spinal decompression with internal fixation is strongly related to increased morbidity and mortality when used to remove spinal metastasis.7–9 Furthermore, research suggests that traditional open surgery is not essential for spinal metastasis.10 The ultimate aim of both open and minimally invasive therapies is to relieve pain and improve neurological function by surgical decompression and stabilization of the spine. Spinal metastasis usually occurs in the anterior and posterior columns of the spine, so it is necessary to carry out circumferential decompression. Both posterior and lateral minimally invasive open decompression approaches can be used to carry out circumferential decompression. Another distinct advantage of minimally invasive open decompression is that it reduces the operation time, the number of hospitalization days and the complication rates, including hemorrhage. This is especially beneficial for weak patients. The present study investigated the use of microwave ablation and minimally invasive open decompression treatment for breast cancer patients with thoracic metastases. It evaluated the efficacy of this technique by observing the patients’ functional outcome, neurological improvement, pain scores and complications.
Materials and methods
Clinical data
From January 2015 to December 2016, 23 cases of breast cancer single-stage thoracic metastatic lesions with clinical characteristics were treated using microwave ablation and minimally invasive open decompression treatment. Clinical characteristics included a Tokuhashi score greater than 8 points, pathological compression fractures, mechanical instability and radiological and/or clinical metastatic spinal cord compression. In our study, the patients’ clinical information, numerical rating scale (NRS) for pain assessment, Frankel Grade classification system score for spinal cord injury assessment, Karnofsky performance status (KPS) score and electronic medical records were collated and recorded in our center’s electronic medical record system.
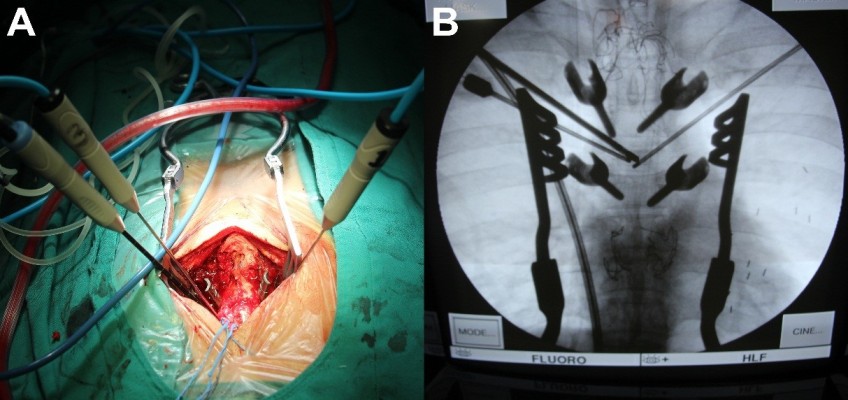
All patients signed written informed consents before surgery, which was approved by the ethics committee of Affiliated Tumor Hospital of Guangxi Medical University. X-rays, computed tomography (CT) and magnetic resonance imaging (MRI) were used to evaluate the vertebral metastatic lesions. The scope of ablation and the type of surgical procedure were planned before surgery. The adjacent normal vertebrae were implanted with pedicle screws in patients undergoing the minimally invasive open decompression procedure. The pathological diagnosis of vertebral metastases was confirmed by pedicle screw biopsy. Guidance with fluoroscopy was used to allow precise control of the ablation antenna (2.45GHz, YiGao, ECO-100A1, Nanjing, China); thermometer placement was used to reduce the rate of complications and to avoid nerve damage during microwave ablation. The ablation antenna was placed in the center of the vertebral metastases through the pedicle (Figure 1). Thermometers were distributed in the vertebral anterior, vertebral center and vertebral posterior margin to protect the spinal cord and peripheral blood vessels in the thoracic spine. Ablation treatment was administered for 15–30 min while the vertebral center temperature was controlled between 50°C and 85°C and the surrounding tissue was maintained at a safe temperature of less than 43°C. Frozen saline was used to protect the spinal cord tissue to prevent excessive temperature. Metastatic tissue was removed and polymethyl-methacrylate cement was used to fill the vertebral metastases to prevent vertebral collapse.
Data collection and outcome measures
Twenty-three patients underwent microwave ablation and minimally invasive open decompression. The patients underwent radiotherapy and chemotherapy after surgery. Patients were followed up for one month during the preoperative and postoperative period. All patients were included in the analysis. Because pain is the main complaint, we used pain improvement as a primary outcome measurement. NRS was recorded, and the Frankel Grade system was used to assess any impact on the nervous system. KPS was used to assess changes in the patients’ physical condition.
Statistical analysis
The data are expressed using mean±standard deviation. The before and after surgery parameters were identified using repeated-measures analysis of variance (ANOVA). The Mann–Whitney U test was used to compare changes in the cases where normal distribution could not be guaranteed. The chi-squared test was used to compare the categorical variables. A P-value of <0.05 was considered statistically significant. Data analysis was performed using SPSS version 22.0 (SPSS, Chicago, IL, USA).
Results
Distribution of patient characteristic data
The study subjects consisted of 23 female patients, all of whom represented cases of single-stage thoracic metastasis from breast cancer. The mean age was 51.86±10.11 years (age range 38–68 years). Mean operation time was 177.21±60.04 minutes and the mean operative blood loss was 314.34±152.63 mL.
Pain
All 23 patients underwent surgical treatment and experienced pain relief. The level of pain during the preoperative and one-month postoperative period was assessed using NRS. The preoperative NRS score was 5.86±1.74 and the postoperative NRS score was 3.00±1.31. The differences in pain before and after surgery were statistically significant (Table 1).
  | Table 1 Comparison of clinical data of patients preoperatively and postoperatively Abbreviations: NRS, numerical rating scale; KPS, Karnofsky performance status. |
Neurological symptoms
A total of 23 patients presented with neurological symptoms (8 with Frankel Grade C, 12 with Frankel Grade D and 3 with Frankel Grade E). At the conclusion of the study one-month postoperative, all 23 patients had improved by one Frankel Grade and none had worsened (2 with Frankel Grade C, 8 with Frankel Grade D and 13 with Frankel Grade E). Nerve function recovery was rapid after the surgical treatment. Significant differences were observed in neurological symptom presentation before and after surgery (Table 1).
Functional outcome (KPS)
The KPS score was used to evaluate the functional outcome. At one-week post-surgery, the KPS score was significantly greater in 18 of the 23 patients, while 5 patients showed no deterioration in functional outcome. A comparison of the functional outcome results before and after surgery showed that the differences were statistically significant (Table 1).
Complications
There were no deaths 1 month after surgery. Two of the 23 patients had cerebrospinal fluid (CSF) leaks, 1 patient displayed delayed wound healing and 1 patient contracted a urinary infection. For all of the patients, the symptoms either disappeared completely or were significantly alleviated without complications using symptomatic treatment alone. No further surgical intervention was necessary.
Discussion
The treatment of cancer with spinal metastasis is palliative. The main purpose of the treatment is to relieve pain, alleviate symptoms of nerve compression and reduce the instability of the vertebral body. This study assessed the efficacy of treating breast cancer patients with thoracic spinal metastases using microwave ablation and minimally invasive open decompression therapy. The majority of the patients reported pain relief following surgery. Neurological function improved in 56.5% of the patients. According to the KPS metric, 78.3% of the patients showed improved function. Overall, the postoperative complications were less for the patients in this study than they are for patients that undergo a traditional open surgical intervention. The study results showed that microwave ablation and minimally invasive open decompression of thoracic metastases from breast cancer significantly enhanced the patients’ quality of life, reduced patient pain and improved patient recovery.
Previous studies have reported that 80% of patients with metastatic cancer of the spine are often troubled by pain.3 Pain is primarily caused by the local inflammatory response due to tumor enlargement, periosteal tension and expansion of the epidural venous plexus. Radicular pain is often due to compression of nerve tissue from the underlying nerve roots. Moreover, pain can be directly related to the axial instability caused by bone destruction. The pain caused by spinal metastasis is often caused by a combination of one or more of these factors.4 Microwave ablation destroys sensory nerve fibers, narrows the lesion and reduces the nerve stimulating factors produced by the destruction of tumor cells, resulting in pain relief.
Spinal cord dysfunction is associated with spinal cord metastasis. Surgical decompression is still the main treatment option for neuropathy because it quickly and effectively restores nerve function.11,12 In general, spinal decompression is achieved by posterior decompression laminectomy because it can ease the compression of the spinal cord and improve neurological function. However, most spine metastases involve the anterior and middle column of the spine.13,14 With the development of spinal surgery, metastatic lesions require more aggressive methods metastatic lesions require methods of total decompression, such as circumferential compression or combined approaches (involving anterior and posterior decompression). These techniques are associated with massive bleeding events, which can affect a patient’s quality of life and delay the administration of adjuvant therapy. Microwave ablation was developed and introduced for this condition in order to overcome this surgical risk. Microwave ablation is more effective in the ablation of bone tissue, especially in sclerotic bone lesions. The ablation process is less affected by the surrounding soft tissue, and it is more penetrating and effective than other methods. The application of microwave ablation in surgery destroys most of the tumor cells, delays local recurrence and reduces tumor-related bone destruction. However, when using this procedure, it is essential to control the microwave ablation safety boundaries and protect the spinal cord nerve tissue. Although the tumor tissue is not completely ablated, the patient can still benefit from treatment, particularly if they have aggressive malignant tumors. The risk of spinal cord injury is effectively avoided by proper temperature probe placement under open conditions. Radicular compression and spinal cord dysfunction are reduced or restored using circumferential decompression. If the nerve root of the thoracic spine is invaded by the lesion, the pain can be prevented by sacrificing the nerve root. Therefore, microwave ablation is effective in the treatment of neuropathic pain and the recovery of spinal cord function.
After surgical decompression of the middle and posterior columns of the spine, the nerve root is compressed, which can result in the loss of integrity of the vertebral body structure.15 Therefore, reconstruction of vertebral integrity is critically important. The pedicle screw stabilization system provides strong fixation when utilized through a posterior approach. Vertebral resection is ideal for posterior fixation. However, this technique is associated with muscle dissection, detachment and devascularization, leading to major surgical-related complications, including bleeding, pain, infection and prolonged immobilization and recovery. Subsequently, wound healing is prolonged or inhibited, and further adjuvant radiotherapy and chemotherapeutic treatments are delayed. This can make it seem as if surgical efforts to control the tumor are ineffective. Thus, minimally invasive surgical approaches are needed.
Over the past several years, minimally invasive open decompression has been rapidly developed.16 The minimally invasive open decompression technique is mainly used to treat spinal cord compression, but there is no direct impact on spinal metastatic tumors. Additional microwave ablation therapy is required to achieve partial tumor control. The purpose of the procedure is not to entirely resect the tumor; it is only used to partially resect the tumor. Microwave ablation and circumferential decompression treatment creates sufficient space to allow polymethyl-methacrylate cement injection, facilitating little to no resistance, which can reduce the risk of bone cement leakage. Pain receptors are also simultaneously destroyed by the procedure. Injection of the polymethyl-methacrylate cement can strengthen the vertebral body to prevent pathological fractures and to establish the spinal cord barrier to prevent metastases.
In this relatively small study, no perioperative mortality was reported. The postoperative complications included cerebrospinal fluid (CSF) leaks, delayed wound healing and urinary tract infection. Symptomatic treatment resolved all of these complications. All the patients recovered postoperatively.
Limitations
This study has some limitations. Firstly, it is a retrospective observation with a relatively small sample size. Secondly, the follow-up time was relatively short. Thus, a randomized controlled trial with a longer follow-up period and a larger sample size is warranted to explore the effects of microwave ablation combined with minimally invasive open decompression for breast cancer patients with thoracic metastasis.
Conclusions
The study results suggest that the approach presented in this paper represents an improvement in the current surgical treatment procedures for thoracic metastases from breast cancer. The goals of spinal metastases tumor treatment include debulking the lesion, neuronal decompression and mechanical stabilization, all of which can be completed with microwave ablation combined with minimally invasive open decompression. To summarize, the application of microwave ablation combined with minimally invasive open decompression may be an effective alternative to the established treatment methods for breast cancer patients with thoracic metastasis.
Acknowledgments
The relevant human materials have been reviewed and approved by the ethics committee of Affiliated Tumor Hospital of Guangxi Medical University, and the study is deemed to meet the medical ethical requirements. We wish to thank the patients and families involved in this study for providing written informed consent for publication of the accompanying images. This work was supported by the Guangxi self-funded research project [grant number Z20170425 and Z20170428].
Disclosure
The authors report no conflicts of interest in this work.
References
Finkelstein JA, Zaveri G, Wai E, Vidmar M, Kreder H, Chow E. A population-based study of surgery for spinal metastases. Survival rates and complications. J Bone Jt Surg Br. 2003;85(7):1045–1050. | ||
Chen Y, Tai BC, Nayak D, et al. Blood loss in spinal tumour surgery and surgery for metastatic spinal disease: a meta-analysis. Bone Joint J. 2013;95-B(5):683–688. | ||
Mathis JM, Barr JD, Belkoff SM, Barr MS, Jensen ME, Deramond H. Percutaneous vertebroplasty: a developing standard of care for vertebral compression fractures. AJNR Am J Neuroradiol. 2001;22(2):373–381. | ||
Pascal-Moussellard H, Broc G, Pointillart V, Simeon F, Vital JM, Senegas J. Complications of vertebral metastasis surgery. Eur Spine J. 1998;7(6):438–444. | ||
Kastler A, Alnassan H, Aubry S, Kastler B. Microwave thermal ablation of spinal metastatic bone tumors. J Vasc Interv Radiol. 2014;25(9):1470–1475. | ||
Pusceddu C, Sotgia B, Fele RM, Melis L. Treatment of bone metastases with microwave thermal ablation. J Vasc Interv Radiol. 2013;24(2):229–233. | ||
Ibrahim A, Crockard A, Antonietti P, et al. Does spinal surgery improve the quality of life for those with extradural (spinal) osseous metastases? An international multicenter prospective observational study of 223 patients. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2007. J Neurosurg Spine. 2008;8(3):271–278. | ||
Wang JC, Boland P, Mitra N, et al. Single-stage posterolateral transpedicular approach for resection of epidural metastatic spine tumors involving the vertebral body with circumferential reconstruction: results in 140 patients. Invited submission from the Joint Section Meeting on Disorders. J Neurosurg Spine. 2004;1(3):287–298. | ||
Dyck PJ, Boes CJ, Mulder D, et al. History of standard scoring, notation, and summation of neuromuscular signs. A current survey and recommendation. J Peripher Nerv Syst. 2005;10(2):158–173. | ||
Rao PJ, Thayaparan GK, Fairhall JM, Mobbs RJ. Minimally invasive percutaneous fixation techniques for metastatic spinal disease. Orthop Surg. 2014;6(3):187–195. | ||
Anchala PR, Irving WD, Hillen TJ, et al. Treatment of metastatic spinal lesions with a navigational bipolar radiofrequency ablation device: a multicenter retrospective study. Pain Physician. 2014;17(17):317–327. | ||
Patchell RA, Tibbs PA, Regine WF, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet. 2005;366(9486):643–648. | ||
Algra PR, Heimans JJ, Valk J, Nauta JJ, Lachniet M, Van Kooten B. Do metastases in vertebrae begin in the body or the pedicles? Imaging study in 45 patients. AJR Am J Roentgenol. 1992;158(6):1275–1279. | ||
Feiz-Erfan I, Rhines LD, Weinberg JS. The role of surgery in the management of metastatic spinal tumors. Semin Oncol. 2008;35(2):108–117. | ||
Harrington KD. Anterior cord decompression and spinal stabilization for patients with metastatic lesions of the spine. J Neurosurg. 1984;61(1):107–117. | ||
Mobbs RJ, Sivabalan P, Li J. Minimally invasive surgery compared to open spinal fusion for the treatment of degenerative lumbar spine pathologies. J Clin Neurosci. 2012;19(6):829–835. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

