Back to Journals » International Medical Case Reports Journal » Volume 12
Combined Intravitreal Bevacizumab And Dexamethasone In Bilateral Lupus Retinopathy
Authors Shrestha R , Kharel Sitaula R , Karki P, Joshi SN , Rawal S
Received 3 July 2019
Accepted for publication 24 September 2019
Published 30 October 2019 Volume 2019:12 Pages 329—333
DOI https://doi.org/10.2147/IMCRJ.S220499
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ruchi Shrestha,1 Ranju Kharel Sitaula,1 Pratap Karki,1 Sagun Narayan Joshi,1 Suniti Rawal2
1Department of Ophthalmology, B.P.Koirala Lions Centre for Ophthalmic Studies, Institute of Medicine, Tribhuvan University Teaching Hospital, Kathmandu, Nepal; 2Department of Gynaecology and Obstreitics, Institute of Medicine, Tribhuvan University Teaching Hospital, Kathmandu, Nepal
Correspondence: Ruchi Shrestha
Department of Ophthalmology, B.P.Koirala Lions Centre for Ophthalmic Studies, Institute of Medicine, Tribhuvan University Teaching Hospital, Maharajgunj Road, Kathmandu 44600, Nepal
Tel +977-9847027650
Email [email protected]
Abstract: This paper reports and discusses a case of bilateral lupus retinopathy with macular edema in a patient diagnosed with systemic lupus retinopathy and treated with combined intravitreal bevacizumab (0.025 mL/0.625 mg) and intravitreal dexamethasone (0.05 mL/0.2 mg). The patient was a 25-year-old female with a history of diminution of vision in both eyes. Best corrected visual acuity (BCVA) of the right eye was 2/60 and of the left eye was 1/60. Fundus examination revealed bilateral swelling of the optic disc nasally, cotton wool spots, and multiple flame shaped, dot and blot hemorrhages in the disc and macula. Optical coherence tomography (OCT) revealed macular edema in both eyes. Despite being treated with immunosuppressive the visual acuity did not improve. Two doses of combined intravitreal bevacizumab (0.025 mL/0.625 mg) and dexamethasone (0.05 mL/0.2 mg) were given to the patient in both eyes at an interval of one week. Two weeks after the last intravitreal injection the BCVA was 6/24 and N8 in both eyes. Fundus examination revealed a decrease in the number and size of hemorrhages, and resolution of the blurred disc margin, cotton wool spots, and hard exudates. OCT of the macula 2 weeks after the last intravitreal injection showed a significant decrease in macular edema. The intraocular pressure was not elevated for a period of 6 months. This case would be a unique case of lupus retinopathy with macular edema receiving a combined half dose of intravitreal injection bevacizumab and dexamethasone with promising results. This could be beneficial in a set up where the patients cannot afford intraocular steroid implants.
Keywords: systemic lupus erythematosus, macular edema, bevacizumab, dexamethasone
Introduction
Systemic lupus erythematosus (SLE) is a chronic, systemic, immunologically mediated disease of unknown etiology. Around 90% of SLE patients are women and the usual age at onset is between fifteen and forty-five years. SLE may be triggered by exposure to sunlight, infection, and other stresses. Pregnancy and the use of sulfonamides and contraceptives have been associated with exacerbations of the disease.1
Keratoconjunctivitis sicca (KCS) with or without xerostomia is the most common ocular manifestation of SLE, occurring in 25% of patients.2 Retinal involvement in SLE is quite common but second only to KCS.3 A clinical study revealed that 88% of patients with lupus retinopathy had active systemic disease. Furthermore, SLE patients with retinopathy had significantly decreased survival rate compared with SLE patients without retinopathy.4
Retinopathy in SLE is suggestive of high disease activity during the course of SLE, and hence, is a marker of poor prognosis for survival. SLE patients with retinopathy have overall worse prognosis and decreased survival, compared to SLE patients without retinopathy.5
A combination of dexamethasone implant and bevacizumab therapy injected simultaneously is synergistic in increasing visual acuity, decreasing the retinal thickness, and lengthening the time between injections as compared with either medication alone without significantly raising intraocular pressure.6
The dose of intravitreal bevacizumab is 1.25 mg/0.05 mL and the dose of intravitreal dexamethasone is 0.4 mg/0.1 mL. Combined bevacizumab and dexamethasone has been given intravitreal so that they have a synergistic effect to reduce retinopathy and macular edema.
Case History
This study presents the case of a 25-year-old female who presented with bilateral progressive painless decreased vision for two months associated with headache. The patient had a history of progressive leg swelling, decreased urine output, and amenorrhea for three months. As a result, she was admitted to the medicine ward.
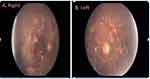
The best corrected visual acuity (BCVA) at presentation in the right eye was 2/60, N10 and in the left eye was 1/60, N10. The intraocular pressure was 14 mmHg in the right eye and 16 mmHg in both eyes by Goldman’s applanation tonometer. Bilateral anterior segment was normal, and the media were clear in both eyes. Posterior segment examination revealed bilateral optic disc swelling nasally, cotton wool spots, and multiple flame shaped, dot and blot hemorrhages in the disc and macula. The arteries were tortuous and attenuated. Multiple hard exudates around the disc and macula were noted, as can be seen in Figure 1.
 |
Figure 1 Fundus photograph showing blurred disc margin nasally, multiple hemorrhages, hard exudates, and cotton wool spots in both eyes. (A) Right eye. (B) Left eye. |
OCT revealed macular edema in both eyes. The central macular thickness in the RE was 718 µm and was 743 µm in the LE, as can be seen in Figure 2.
 |
Figure 2 Optical coherence tomography at presentation showing macular edema in both eyes. (A) Right eye. (B) Left eye. |
Blood pressure was measured as 150/100 mmHg in each arm. Further investigation revealed low hemoglobin and deranged renal function tests with high urea and creatinine levels. The patient was positive for anticardiolipin antibody, antinuclear antibody (ANA), and double standard deoxynucleic acid (dsDNA). Fibrin degradation product (FDP) D-dimer was found to be high.
Ultrasonography of the abdomen showed bilateral enlarged kidney (11.7 cm × 6 cm) with renal parenchymal disease. Gross free fluid was noted in the abdomen, suggestive of ascites. Gravid uterus contained a single gestation sac with a single embryo with gestational age of 10 weeks. This confirmed her pregnancy and justified the history of amenorrhoea. Multiple cholelithiasis and minimal pleural effusion with minimal pericardial effusion were also noted. Renal biopsy revealed diffuse lupus nephritis/ISN/RPS class 4 and membranous lupus nephritis indices (modified NIH) of activity 15/24 and chronicity 5/12. Echocardiography revealed global hypokinesia of left ventricular wall/mild cone left ventricular hypertrophy/mild tricuspid regurgitation/mild aortic regurgitation/moderate left ventricular end-systolic dimension (ejection fraction=90). Thus, with all these findings the diagnosis was confirmed as systemic lupus erythematosus with lupus nephritis, lupus retinopathy, and macular edema. Medical termination of pregnancy was done due to the life-threatening condition of the patient. The patient underwent dialysis 14 times to maintain renal function. The patient received injection of methylprednisolone 500 mg bi-daily for three days and cyclophosphamide (500 mg) two cycles at an interval of one month. The patient was maintained with cotrimoxazole 960 mg once daily, hydroxychloroquine 200 mg bi-daily, prednisolone 40 mg once daily, and amlodipine 5 mg combined with atenolol 25 mg once daily.
Systemic findings showed resolution including her blood pressure but no improvement in ocular symptoms was noted despite using immunosuppressive for a period of one month. Therefore, in order to manage macular edema, she was treated with a combination of intravitreal bevacizumab (0.025 mL/0.625 mg) and dexamethasone (0.05 mL/0.2 mg) in both eyes at an interval of one week. Two weeks after the last intravitreal injection, the BCVA was 6/24, N8 in both eyes. Fundus revealed a decrease in the number and size of hemorrhages, and resolution of blurred disc margin, cotton wool spots, and hard exudates (Figure 3).
 |
Figure 4 OCT of the macula taken after two doses of intravitreal injection showing marked resolution of macular edema in both eyes. (A) Right eye. (B) Left eye. |
The central macular thickness reduced from 713 µm to 253 µm in the RE and from 743 µm to 170 µm in the LE as seen in Figure 4. The intraocular pressure was 18 mmHg in both eyes after two doses of intravitreal injection. There was no significant intraocular pressure rise for a period of six months. The patient’s vision and fundus findings are stable in six months of follow-up.
Discussion
Retinopathy in SLE was first reported by Bergmeister in 1929.7 Since then, retinopathy is a well-known complication of SLE and reported in 50% of SLE cases8,9 prior to the steroid era.
Lupus retinopathy is one of the most common vision-threatening complications of systemic lupus erythematosus with an incidence of up to 29% in patients with active systemic disease.4 Posterior segment finding is not an uncommon finding in systemic lupus erythematosus.10 Ocular fundus is the only part of the human body where small vessels can be directly observed and lupus retinopathy reflects systemic vascular damage.11 It is unfortunate that ocular manifestations have not been included in the diagnostic scoring systems for establishing the clinical diagnosis of systemic lupus erythematosus. All cases of lupus should be evaluated for ocular involvement to detect potentially treatable and preventable complications of the disease.12 The most common pattern of retinopathy is microangiopathy similar to diabetic and hypertensive retinopathy. Earlier findings were small intraretinal hemorrhages and cotton wool spots.13 Similar to these studies, the patient in this study also had multiple intraretinal hemorrhages, cotton wool spots, hard exudates, and macular edema. Macular edema is rare, but it may be present in severe lupus retinopathy. The arteriolar attenuation is severe in preeclampsia and there is marked resolution of symptoms after termination of pregnancy. In this case the macular edema persisted despite immunosuppressive and termination of pregnancy.
There are studies on combined intravitreal dexamethasone implant with intravitreal bevacizumab for treating macular edema caused by diabetes, central retinal vein occlusion, and branch retinal vein occlusion.14 A combination of dexamethasone implant and bevacizumab therapy injected simultaneously is synergistic in increasing visual acuity, decreasing the retinal thickness, and lengthening the time between injections as compared with either medication alone.6 However, dexamethasone implant was not preferred in our scenario due to the high costs associated with it. Consequently, our patient received a simultaneous injection of intravitreal bevacizumab 0.025 mL (0.625g) with intravitreal injection of dexamethasone 0.05 mL (0.2 mg) and had a dramatic reduction in macular edema, retinal hemorrhage, and hard exudates. Instead of dexamethasone implant, we injected 0.05 mL (0.2 mg) of dexamethasone injection and 0.025 mL (0.625 mg) bevacizumab and repeated at an interval of one week. This combination had significant improvement in visual outcome and resolution of retinal edema and hemorrhage without significant rise in intraocular pressure.
This case would be a unique case of lupus retinopathy receiving combined intravitreal injection of bevacizumab and dexamethasone with promising results. This could be beneficial in a set up where the patients cannot afford intraocular steroid implants.
Conclusion
Lupus retinopathy is a sight-threatening condition and is an indicator of active disease of systemic lupus retinopathy. Combined intravitreal bevacizumab and intravitreal dexamethasone has promising results in the management of lupus retinopathy with macular edema without a significant rise in intraocular pressure.
Ethical approval
Ethical approval was taken from the Institutional review board of Institute of Medicine, Tribhuvan University. Written informed consent was taken from the patient for having the case details and accompanying images published.
Disclosure
The authors report no financial interest/support and no conflicts of interest in this work.
References
1. Foster Corbin J. Systemic lupus erythematosus. In: Jakobiec FAT, Albert DM, editors. Principles and Practice of Ophthalmology. Philadelphia, PA: WB Saunders; 1994:4429–4436.
2. Steinberg AD, Talal N. The coexistence of sjögren’s syndrome and systemic lupus erythematosus. Ann Intern Med. 1971;74(1):55–61. doi:10.7326/0003-4819-74-1-55
3. Gold DH, Morris DA, Henkind P. Ocular findings in systemic lupus erythematosus. Br J Ophthalmol. 1972;56(11):800–804. doi:10.1136/bjo.56.11.800
4. Stafford-Brady FJ, Urowitz MB, Gladman DD, Easterbrook M. Lupus retinopathy: patterns, associations, and prognosis. Arthritis Rheum. 1988;31:1105. doi:10.1002/art.1780310904
5. Sobrin L, Foster CS(1994) Systemic lupus erythematosus choroidopathy. BMJ. 1994;IV.
6. Nagpal M, Jain P, Rahud J, Mehrotra N. Outcomes of combination therapy with dexamethasone implant and bevacizumab in macular edema related to vascular occlusions. Taiwan J Ophthalmol. 2014;4:77–81. doi:10.1016/j.tjo.2014.03.008
7. Blergmeister R. Uber primare and miliare tuberkuloseder retina. Wien Med Wochenschr. 1929;79:1116.
8. Baehr G, Klemperer P, Schifrin A. A diffuse disease of the peripheral circulation (usually associated with lupus erythematosus and endocarditis). Trans Assoc Am Physicians. 1935;50:139–155.
9. Dubois EL. The clinical picture of systemic lupus erythematosus. In: Dubois EL, editor. Lupus Erythematosus. Los Angeles: University of Southern California Press; 1974:323–326.
10. Nangia PV, Viswanathan L, Kharel R, Biswas J. Retinal involvement in systemic lupus erythematosus. Lupus Open Access. 2017;2:1000129.
11. Kharel (Sitaula) R, Shah DN, Singh D. Role of lupus retinopathy in systemic lupus erythematosus. J Ophthalmic Inflamm Infect. 2016;6:15. doi:10.1186/s12348-016-0081-4
12. Sitaula R, Shah DN, Singh D. The spectrum of ocular involvement in systemic lupus erythematosus in a tertiary eye care center in Nepal. Ocul Immunol Inflammation. 2011;19(6):422–425. doi:10.3109/09273948.2011.610023
13. Ushiyama O, Ushiyama K, Koarada S, et al. Retinal disease in patients with systemic lupus erythematosus. Ann Rheum Dis. 2000;59(9):705–708. doi:10.1136/ard.59.9.705
14. Felipe L.de Andrade, Flavio S.Lopes, Gabriel C.de Andrade et al. Dexamethasone implant and bevacizumab in macular edema. Med Hypothesis Discov Innov Ophthalmol. 2016;5:1.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.