Back to Journals » Journal of Pain Research » Volume 15
Combine Approach of Proximal Fibula Osteotomy (PFO) Followed by Intra-Articular Dextrose Prolotherapy in Severe Medial Knee Osteoarthritis
Authors Rahman AN, Herman H, Kriswanto E, Faried A, Nasser MK
Received 11 January 2022
Accepted for publication 4 July 2022
Published 15 July 2022 Volume 2022:15 Pages 1983—1993
DOI https://doi.org/10.2147/JPR.S357284
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sudhir Diwan
Video abstract presented by Alif Noeriyanto Rahman.
Views: 182
Alif Noeriyanto Rahman,1,2 Herry Herman,2,3 Eri Kriswanto,2,4 Ahmad Faried,2,5 Mochammad Kamal Nasser6
1Musculoskeletal Pain Intervention and Regeneration, Faculty of Medicine Universitas Padjadjaran, Orthopaedic and Pain Intervention Center of Sentra Medika Hospital, Depok, Indonesia; 2Pain Intervention and Regeneration, Faculty of Medicine, Universitas Padjadjaran, Bandung, West Java, Indonesia; 3Department of Orthopaedic and Traumatology Hasan Sadikin General Hospital Faculty of Medicine Padjadjaran University, Bandung, West Java, Indonesia; 4Department of Orthopaedic and Traumatology Baptist Hospital, Kediri, Indonesia; 5Department of Neurosurgery, Hasan Sadikin General Hospital Faculty of Medicine Padjadjaran University, Bandung, West Java, Indonesia; 6Baptist Hospital, Kediri, Indonesia
Correspondence: Alif Noeriyanto Rahman, Musculoskeletal Pain Interventional and Regeneration, Faculty of Medicine Universitas Padjadjaran, Orthopaedic and Pain Intervention Center of Sentra Medika Hospital, RS Sentra Medika Cisalak Depok (Jl Raya Jakarta Bogor, Cisalak, Kota Depok, Jawa Barat), Depok, Indonesia, Tel +6281233889873, Email [email protected]
Background: Knee osteoarthritis (OA) is a chronic and progressive degenerative disease. It resulted from mechanical and chemical disorders that damage the joint and the underlying bone. The management of knee OA is challenging due to poor self-regeneration of connective tissues. Surgical treatment with prolotherapy approaches was conducted to treat medial compartment knee OA.
Aim: To know the injection frequency to reach a 50% improvement in VAS score and WOMAC index.
Methods: Six patients who suffered from late-stage medial compartment knee OA underwent PFO followed by twelve sessions of intra-articular dextrose prolotherapy. The subjective pain score, visual analog scale (VAS), was assessed based on the patient subjectiveness before and after treatment. Patients marked the score from 0 to 10 cm to describe the current pain state. The functional index, the Western Ontario and McMaster Universities Osteoarthritis (WOMAC) index used to evaluate the Patient’s clinical symptoms. It ranges from 0 to 96 points consisting of three main sections: pain (total 20 points), stiffness (total: eight points), and physical function disability (total 68 points). Higher scores indicate severe symptoms and function.
Results: Four patients showed pain relief and functional improvement with more than 50% scores of VAS and WOMAC after the treatment. Two patients received more than twelve doses of intra-articular dextrose prolotherapy due to a lack of progress.
Conclusion: This study provides clinical evidence for a new treatment strategy for advanced knee OA. This combined therapy improves the patient’s daily activity function and postpones the need for total knee arthroplasty (TKA).
Keywords: knee osteoarthritis, proximal fibula osteotomy, dextrose prolotherapy
Introduction
Knee osteoarthritis (OA) is a progressive and degenerative disease characterized by joint pain, stiffness, and deformity. Knee OA is the most frequent form of arthritis in older adults, leading to physical disability and high living costs. The prevalence of knee OA increases with age and in women (30.7%) than in men (15.6%) over 55 years old.1,2
Two main mechanisms contributing to the development of knee OA are biomechanical and biochemical disorders. An avascular connective tissue called articular cartilage has a unique extracellular matrix. It consists of polymeric hyaluronic acid (HA) and a high concentration of proteoglycans. These provide a suspension material for weight-bearing and shearing force. A repetitive mechanical tension of the knee joint may damage the cartilage. It also induces hypertrophy, remodeling of the subchondral bone, and secondary synovial membrane inflammation.3
A case of severe knee OA needs surgical procedures. It varies from Total Knee Arthroplasty (TKA), High Tibial Osteotomy (HTO), and Proximal Fibula Osteotomy (PFO). PFO has become the new alternative procedure to reduce pain and improves joint function in severe knee OA with a narrowing medial compartment. Compared to TKA, which is the gold standard, and HTO, PFO is not only a safe, simple, and quick procedure, but it also does not need additional insertion.4 Utomo et al reported that PFO reduced varus deformity, increased joint space ratio, and improved patient subjective scores on pain and function.5
Recent treatments have effectively increased tissue healing and slowed down the degeneration process. It includes Platelet-rich plasma (PRP) therapy, mesenchymal stem cells, ozone therapy, botulinum toxin type A, and hypertonic dextrose.6–10 Hypertonic dextrose can treat musculoskeletal pain under the name prolotherapy. Hypertonic dextrose injection is an accessible, low-cost, and safe procedure that gives a significant improvement. It was injected into the articular space to repair and restore the soft tissues in the joint by initiating the inflammation, proliferation, and regeneration of the damaged cartilage.10
However, PFO and dextrose prolotherapy did not use widely due to the lack of clinical evidence. Furthermore, this combined therapy still has many limitations. We report six cases with medial compartment knee OA. The patients underwent PFO surgery followed by intra-articular dextrose prolotherapy, assessed using subjective pain score and functional index.
Case Presentation
Method
The authors obtained written consent from the patients to describe their condition and publish the data. The inclusion criteria were patients with grade IV (late-stage) knee OA according to Kellgren and Lawrence’s classification with medial joint space narrowing. They also underwent a PFO procedure followed by a minimum of two courses (twelve doses) of intra-articular dextroses prolotherapy without any rheumatologic and inflammatory diseases such as rheumatoid arthritis. There was no response to medication and conservative treatment. All patients gave consent to participate in this study. In contrast, the exclusion criteria were that patients received irregular prolotherapy, intra-articular injection of hyaluronic acid, anticoagulant medication history, and a history of total knee arthroplasty. Six patients with late-stage medial compartment knee OA who met the inclusion criteria were assessed at the outpatient department of Kediri Baptist Hospital from February to May 2021.
Under subarachnoid block (SAB) anesthesia, the PFO procedure had done by removing a little segment (1–2 cm) of fibula 7–8 cm below the fibular head by accessing the inter-muscular space between extensor digitorum longus and peroneus longus brevis. We performed the PFO procedure only on the foot that the Patient complained about the most. After undergoing PFO, the patient received two courses of intra-articular dextrose prolotherapy. One course of intra-articular dextrose prolotherapy consists of six doses; each dose was injected once a month (month 1–6) and rest for the next six months (month 7–12) (Figure 1). The authors aimed to know if PFO combined with two courses or twelve doses of prolotherapy could reach a 50% improvement in the subjective score and functional index compared to baseline. When the cases did not show the required improvement after 12 doses, the authors decided to give one more cycle of intra-articular dextrose prolotherapy.
 |
Figure 1 One course of intra-articular dextrose prolotherapy. The prolotherapy was given once a month for six months. |
One dose of dextrose prolotherapy prepared by using a 6 mL solution containing 13% hypertonic dextrose and 0.6% lidocaine was injected into the articular. After each injection, the patient was given oral medication of acetaminophen as a pain reliever, one tablet three times a day for three days.
The visual analog scale (VAS) was rated based on the Patient’s subjective feelings before and after treatment. It has a straight line with scores from 0 to 10 cm, anchored by “no pain” on the left side (score of 0) and “very severe pain” on the right side (score of 10). The patients gave marks on the line to best describe their current pain state.11
The functional index - The Western Ontario and McMaster Universities Osteoarthritis (WOMAC) index, evaluated the Patient’s clinical symptoms. It ranges from 0 to 96 points consisting of three main sections: pain (20 points), stiffness (eight points), and physical function disability (68 points). Higher scores indicate severe symptoms and function. The result points were divided into four groups based on the severity: mild (0–24 points), moderate (25–48 points), severe (49–72 points), and very severe (73–96 points).12
Case 1
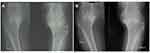
A 63-year-old female with no previous history of trauma or knee surgery visited our outpatient department in June 2018. Her body weight was 67 kg, and her height was 155 cm (body mass index [BMI]: 27.8 kg/m2). She complained of pain and stiffness over her right knee during walking for several years. The VAS score was 6–7 in resting and aggravated up to 8 when squatting, climbing stairs, and walking. She had received analgesic drugs like oral nonsteroidal anti-inflammatory drugs for several years but still suffered from recurrent right knee pain and no improvement in walking endurance. The physical examination showed varus deformity, crepitus, and bulking on the right knee without any inflammation signs. The WOMAC index was rated 55. The X-Ray image of the knees revealed grade IV OA on both knees based on Kellgren and Lawrence classification, with a more severe on the right knee (Figure 2A).
She underwent a PFO procedure on her right leg in July 2018, followed by a course of intra-articular dextrose prolotherapy every six months continuously on her right knee (one course consists of six doses, each dose was injected once a month consecutively). The intra-articular injection was given using a 6 mL solution containing 13% hypertonic dextrose and 0.6% lidocaine. The patient was given oral medication of acetaminophen as a pain reliever after each injection, one tablet three times a day for three days.
After two courses (twelve doses) of intra-articular dextrose prolotherapy, the patient said that the stiffness improved, but the pain was not markedly reduced. The VAS score was 5, and the WOMAC index was 45. We decided to continue the intra-articular dextrose prolotherapy with one more course for this Patient.
At the assessment (32 months post-surgery), the Patient had received three courses of intra-articular dextrose prolotherapy (a total of 18 doses). She reported that the pain improved and could do daily activities by herself, including working, walking, and even riding a motorbike. The VAS score improved to 1 when resting and 2 when aggravated and improved the WOMAC index to 14. The knee X-Ray showed no further medial joint space narrowing on the treated knee. On the contrary, the left knee that did not receive the treatment showed medial joint space narrowing compared to before surgery (Figure 2B).
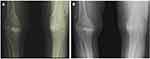
Case 2
A 65-year-old female, whose body weight was 70 kg and height was 156 cm (BMI: 28 kg/m2), came to our outpatient department with a chief complaint of pain in bilateral knees for more than a year. She had tenderness in bilateral medial knees with a VAS score of 5 when resting and aggravated up to 8 when rising from sitting. The physical examination showed varus deformity and bulking over bilateral knees without any inflammation sign. The WOMAC index was rated 40. The knee X-Ray image revealed grade IV OA on both knees and significant narrowing of medial joint space (Figure 3A).
The patient underwent a PFO procedure on both legs in June 2019, followed by a course of intra-articular dextrose prolotherapy continuously on bilateral knees (one course consisted of six doses, each dose was injected once a month consecutively). One dose of dextrose prolotherapy was prepared using a 6 mL solution containing 13% hypertonic dextrose and 0.6% lidocaine, injected into the articular. After each injection, the patient was given oral medication of acetaminophen as pain reliever, one tablet three times a day for three days.
After two courses of intra-articular dextrose prolotherapy following PFO (23 months post-surgery), she reported pain-free when resting and decreased tenderness when doing activities (VAS = 1). Her body weight had no significant change compared to the first visit. The WOMAC index was rated 9. The knee X-Ray revealed an improvement in joint space on the left knee compared to before surgery (Figure 3B).
Case 3
A 66-year-old female, who had suffered from bilateral knee pain for almost five years, visited our outpatient department. Her body weight was 65 kg, and her height was 155 cm (BMI: 27.08 kg/m2). The patient complained of bilateral knee pain, but she reported that the symptoms on the right knee were more disturbing than on the left knee. The VAS score for the right knee was 6 when resting and aggravated up to 8 when climbing stairs, whereas the left knee was 4–5. The WOMAC index was identified 49. Physical examination showed varus deformity and gait disturbance. The X-Ray revealed severe medial compartment OA of bilateral knees (Figure 4A).
The Patient underwent PFO procedure on the right leg (the right knee was more painful than the left knee, so the Patient requested surgery for the right leg) in July 2018. It was followed by a course of intra-articular dextrose prolotherapy every six months continuously on the right knee (one course consisted of six doses, each dose was injected once a month consecutively). The intra-articular injection was given using 6 mL solution containing 13% hypertonic dextrose and 0.6% lidocaine. The patient was given oral medication of acetaminophen as pain reliever after each injection, one tablet three times a day for three days.
After two courses of intra-articular dextrose prolotherapy, she still complained about the right pain, although the pain score was reduced. The VAS score decreased to 6, and the WOMAC index reduced to 32. The patient was to receive one more course of intra-articular dextrose prolotherapy.
At the follow-up (32 months post-surgery), she had received three courses of intra-articular dextrose prolotherapy (a total of 18 doses). We evaluated the treated knee, and she reported that the symptoms were improving. Although the Patient sometimes suffered from knee pain, especially when climbing stairs, she was pretty satisfied with the VAS score of 5, and the WOMAC index was rated 21. Although the Patient’s subjective complaints improved, the X-Ray showed there was no significant improvement in joint space compared to before (Figure 4B).
Case 4
A 72-year-old female with no history of trauma or knee surgery came to the outpatient department in January 2019. Her body weight was 68 kg and height was 160 cm (BMI: 26.5 kg/m2). She complained of knee pain on bilateral knees with a more severe on the left knee. The VAS score was aggravated up to 9 when walking, climbing stairs, going down the stair, and sitting. The WOMAC index was rated 88. On the physical examination, varus deformity and crepitus were identified. The X-Ray image of the knees revealed grade IV knee OA based on Kellgren and Lawrence classification with medial compartment narrowing (Figure 5A).
The patient underwent PFO procedure on both legs in January 2019 followed by a course of intra-articular dextrose prolotherapy every six months continuously on the bilateral knee (one course consisted of six doses, each dose was injected once a month consecutively). One dose dextrose prolotherapy was prepared using 6 mL solution containing 13% hypertonic dextrose and 0.6% lidocaine, injected into the articular. After each injection, the patient was given oral medication of acetaminophen as pain reliever, one tablet three times a day for three days.
At the follow-up (26 months post-surgery), the Patient received two intra-articular dextrose prolotherapy (12 doses). She mentioned that the symptoms were improving, especially when walking. The VAS score was 4, and the WOMAC index was 44. The knee X-Ray showed bilateral knees after treatment (Figure 5B).
Case 5
A 55-year-old female, whose body weight was 48 kg and height was 155 cm (BMI: 20 kg/m2), arrived at the outpatient department and complained of bilateral knee pain and stiffness for a year. The painful sensation had been especially troubling in the past 6 months and progressed until she could not walk without pain, and the analgesics drug gave no relief. The VAS score was 9 and the WOMAC index was 76. Varus deformity, crepitus, and tenderness over bilateral knees without any inflammation sign were identified, and the X-Ray images showed grade IV knee OA (Figure 6A).
The patient underwent PFO procedure on both legs in March 2019 followed by a course of intra-articular dextrose prolotherapy every six months continuously on bilateral knee (one course consisted of six doses, each dose was injected once a month consecutively). A dose dextrose prolotherapy was prepared using 6 mL solution containing 13% hypertonic dextrose and 0.6% lidocaine, injected into the articular. After each injection, the patient was given oral medication of acetaminophen as pain reliever, one tablet three times a day for three days.
At the follow-up (24 months post-surgery), she received two courses of intra-articular dextrose prolotherapy courses (12 doses). The patient reported a marked reduction of knee pain with a VAS score being 1, and the WOMAC index was rated 7. The X-Ray showed bilateral knees after treatment (Figure 6B).
Case 6
A 51-year-old female with no history of trauma or knee surgery came to the visit with a chief complaint of bilateral knee pain for several years. She also experienced stiffness over bilateral knees, especially in the morning. The symptoms were worsening until she could not walk without pain. The Patient’s body weight was 59 kg, and height was 160 cm (BMI: 23.04 kg/m2). The pain sensation reduced when resting (VAS = 5) and increased when climbing stairs, going down the stair, and even when walking (VAS = 9). The WOMAC index was rated 63. Varus deformity, tenderness, and crepitus on both knees were also identified and grade IV knee OA was showed on the X-Ray (Figure 7A).
She underwent PFO procedure on both legs in April 2019 followed by a course of intra-articular dextrose prolotherapy every six months continuously on bilateral knee (one course consisted of six doses, each dose was injected once a month consecutively). A dose dextrose prolotherapy was prepared using 6 mL solution containing 13% hypertonic dextrose and 0.6% lidocaine, injected into the articular. After each injection, the patient was given oral medication of acetaminophen as pain reliever, one tablet three times a day for three days.
At the follow-up (24 months post-surgery), she had received two courses of intra-articular dextrose prolotherapy (12 doses). The patient reported that the symptoms were improving. She did not feel knee stiffness anymore, but she still suffered from pain occasionally. Although the Patient still complained of pain, the pain intensity was decreasing, with a VAS score of 5. The WOMAC index was improved with 26. The X-Ray showed bilateral knees after treatment (Figure 7B).
Discussion
Knee OA, the most common joint disorder, causes severe pain and leads to physical disability. TKA is a gold standard for severe knee OA because of its effectiveness in reducing pain and improving knee function. However, TKA is an expensive and complex procedure requiring multiple revisions in some patients. It can also bring several complications, including infection of the wound, peripheral nerve injury, osteolysis, periprosthetic fracture, etc.13,14
Besides TKA, another treatment for knee OA is the HTO. HTO is an effective surgical procedure for mild knee OA with varus deformity. It relieves pain by diverting the weight-bearing axis to the lateral compartment. However, similar to TKA, the HTO procedure has some disadvantages encompassing wound infection, peroneal nerve paralysis, delayed union, mechanical failure, deep vein thrombosis, etc.15,16 PFO has become a new alternative surgical procedure in reducing pain, improving joint function as reported by Zhang et al. This simple surgical procedure reduces pain in the medial part by increasing the medial joint space.13
As people get older, the bone density of the knee tibial plateau reduces over time. The tibial plateau consists of two sides; the medial and lateral sides. Unlike the medial side, fibula bone supports the lateral side.13 A clinical study conducted by Zhang et al reported that the fibula supports one-sixth of body weight. Therefore, the stress distribution inside the tibial plateau becomes uneven. More medial-side stress in the tibial plateau can result in varus deformity. Moreover, the femoral condyle could shift to the medial during walking with transverse shear forces due to the tibial plateau slope arising from the nonuniform settlement.17 PFO changes the stress distribution in the knee joint and reduces the medial compartment stress by removing a little fibula segment. Pan et al, using computerized tomography (CT) and magnetic resonance imaging (MRI) for a finite element model, concluded that PFO could reduce stress in the medial compartment of the knee joint by transferring the stress pathway from the anterior medial area to posterior medial area on the tibial plateau.18 In addition, an analysis of a three-dimensional gait study demonstrated that PFO could be beneficial in delaying the progression of knee OA.19 It can also rebalance the soft tissue around the knee. After the procedure, the lateral ligaments and muscles of the knee joint will tighten, and the medial side will relax. The lateral soft tissue will pull up the femoral condyl, thus reducing the tension of the medial tibia plateau.20 Utomo et al reported that the use of PFO can significantly reduce the varus deformity, improve medial joint space, and increase patient subjective and functional scores using The Knee Injury and Osteoarthritis Outcome Score (KOOS) index and Oxford knee score.5 The common complication of PFO is an injury of the peroneal nerve and its branches because the procedure bypasses the lateral border of the fibula, where one-third of the deep the peroneal nerve is located. Therefore, the best site for the fibula osteotomy is 6–10 cm under the head of the fibula.21
There are several reasons to determine unilateral or bilateral PFO in Indonesia, such as a) National health coverage. The national health coverage procedure regulates to do the procedure on one side of the knee at one time. Therefore, two periods of time are needed to operate bilateral cases; b) the Patient’s decision. Improvement of low extremity function drives the Patient to cancel their second scheduled operation. After one leg operation, both pathological legs of the Patient show functional improvement. Thus, we do not need to do a second operation c) VAS. The operation prioritized the highest VAS score when both legs were diagnosed with bilateral knee osteoarthritis. It is related to the Indonesia health coverage policy to operate on one knee at once. The unilateral operated patients (Case 1 and 3) complained that the right knee was the most painful, although they had bilateral knee OA. Therefore, the proximal fibula osteotomy procedure was only conducted on the right leg. The VAS and WOMAC scores evaluation were conducted on the treated knee to avoid bias.22
Prolotherapy – proliferative therapy – has been reported to be an effective method to treat musculoskeletal and joint diseases.23 Although the mechanism is still unclear, Rabago et al concluded that prolotherapy provokes mild inflammation and cell stress in the weakened ligament or tendon area. It then releases cytokines and growth factors, including a new healing cascade in that area, thus stimulating the activation of fibroblast, producing collagen precursors, and strengthening the connective tissue.24 The most commonly injected solution is hypertonic dextrose. The contact of human cells and hypertonic dextrose raises the growth factors in different cells, stimulating the proliferation of chondrocytes, osteocytes, and fibroblasts. Moreover, this process excretes the extracellular matrix, which enhances the stability of joints by strengthening and tightening the ligaments and tendons.23 A single-arm clinical trial conducted by Eslamian S and Amouzandeh B (2015) reported that intra-articular hypertonic dextrose injection given in four-weeks interval in moderate knee OA resulted in statistically significant improvements in pain score, range of motion (ROM), and improved WOMAC index score.25 A systematic review of clinical trials conducted by Arias-Vazquez et al in 2019 concluded that hypertonic dextrose prolotherapy (HDP) shows to be more effective for reducing pain and improving function than local anesthetics. It also appears to be as effective as hyaluronic acid (HA), ozone, and radiofrequency but less effective than erythropoietin and Platelet-rich plasma (PRP).26 However, HDP application implies a simple technique, low cost, and can be done in the rural setting but with a meaningful pain reduction.24,26 Lidocaine as a local anesthetic, combined with other medications, has been considered a routine and safe clinical practice.27 An experimental study on rat knee joints concluded that lidocaine could inhibit both components of C-fibres and sympathetic postganglionic neuron mediated inflammation. The anti-inflammatory effects of lidocaine treat acute pain treatment. Moreover, lidocaine provides long-lasting anti-nociceptive results by inhibiting the induction of peripheral and central sensitization.28 However, lidocaine has shown to be chondrotoxic in a time and concentration-dependent manner.29 However, an experimental study in animals reported that the exposure of chondrocytes to 0.5% lidocaine produced no significant differences in cell viability compared to controls after any exposure time.30 In vivo study on the human knee by Ravnihar et al concluded that a single intra-articular knee injection of 2% lidocaine did not influence the chondrocytes viability in OA nor healthy cartilage.31 In our study, the intra-articular lidocaine injection protocol was based on a low concentration of 0.6% lidocaine, which will be diluted by 6 cc of synovial fluid to 0.3% lidocaine in the knee joint so that the risk of possible chondrotoxicity due to intra-articular lidocaine injection can be disregarded.
In this study, the authors aimed to know the injection frequency to reach a 50% improvement in VAS score and WOMAC index. No practical guidelines have been published about the number of dextrose prolotherapy doses given to the patients. Prolotherapy treatment commonly consists of six injections given every 2 to 6 weeks.25 However, based on several studies, there was a decrease in WOMAC index and pain scores after several weeks of follow-up following six injections of dextrose prolotherapy. The WOMAC index and pain scores decreased from 49.85% and 46.19% at the end of week 24 to 31.5% and 34.7% at week 52. Other studies supported the improvements attenuate over time indicating the treatment’s short-term effects.24,25,32 Therefore, the authors decided to enhance the effect of dextrose prolotherapy by giving two courses (a total of 12 injections) to assess the effectiveness. Case 2, 4, 5, and 6 improved compared to baseline in 24 months of evaluation after receiving 12 injections. The VAS score and WOMAC index were reduced by more than 50%. Some cases need more than two courses/12 injections due to a lack of subjective pain score and functional index improvement. Cases 1 and 3 did not show a decrease of 50% in VAS score and WOMAC index after receiving 12 injections. It is possible because of the severity of knee OA and the body mass index (BMI). The BMI cases 1 and 2 were 27.8 kg/m2 and 27.08 kg/m2, and are categorized as obesity I based on the Asian population.33 Zheng et al reported that obesity is a risk of knee OA and could make the condition worsen if the patients do not reduce their weight. Thus, cases 1 and 3 were decided to receive one more course (18 injections).34 After the third course, case 1 reached the target of a 50% improvement in VAS score and WOMAC index compared to baseline. Case 3 did not meet a 50% reduction in VAS score; however, she was pretty satisfied with the outcome as long as she could do prostration movements for praying. The improvement is available in Table 1.
 |
Table 1 The Characteristics of the Six Cases, Before and After Treatment |
Our cases provide clinical evidence for a new therapy for severe knee OA. We combined biomechanical advantages of PFO and hypertonic dextrose prolotherapy to treat patients with late-stage medial compartment knee OA. Both treatments are simple, quick, safe, and affordable procedures to reduce pain and increase knee function. From our six cases, all of them reported meaningful improvement at long-term follow-up based on their subjective pain scores using VAS and functional scores using the WOMAC index (Table 1). The patient’s knee function improves and the patient’s satisfaction increases in daily life. This combined therapy can offer an alternative to treat late-stage medial compartment knee OA rather than a complex surgical procedure. However, the patient can still undergo TKA if needed. This report presents the first case series with PFO procedure followed by dextrose prolotherapy to the best of our knowledge.
Limitation
The limitations of these clinical observation cases include the following: 1) a small number of patients to report a strong clinical effect. 2) The absence of standardization of knee X-Ray images to do radiographic measurement (Tibio-femoral angle before and after treatment, joint space ratio before and after treatment). 3) This observational study did not eliminate the dependent factors such as body weight, height, and other diseases.
Further studies with randomized, double-blind control trials and larger case populations are needed to reduce biases, errors, and the significance of the therapies.
Conclusion
We report six elderly patients with severe knee OA who received intra-articular dextrose prolotherapy following the PFO procedure and showed pain relief and functional improvement as a long-term outcome. This case series suggests that the treatment strategy may be useful to treat severe OA with varus deformity and postpone the need for TKA for those who cannot undergo HTO or TKA for various reasons.
Ethics Approval and Consent to Participate
The Institutional Review Board of Baptist Hospital Kediri approved this case series. We also obtained and informed consent from the patients and their relatives.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Brooks PM. The burden of musculoskeletal disease - a global perspective. Clin Rheumatol. 2006;25(6):778–781. doi:10.1007/s10067-006-0240-3
2. Litwic A, Edwards MH, Dennison EM, Cooper C. Epidemiology and burden of osteoarthritis. Br Med Bull. 2013;105(1):185–199. doi:10.1093/bmb/lds038
3. Di Nicola V. Degenerative osteoarthritis a reversible chronic disease. Regen Ther. 2020;15:149–160. doi:10.1016/j.reth.2020.07.007
4. Zhang YZ. Innovations in orthopedics and traumatology in China. Chin Med J. 2015;128(21):2841–2842. doi:10.4103/0366-6999.168015
5. Utomo DN, Mahyudin F, Wijaya AM, Widhiyanto L. Proximal fibula osteotomy as an alternative to TKA and HTO in late-stage varus type of knee osteoarthritis. J Orthop. 2018;15(3):858–861. doi:10.1016/j.jor.2018.08.014
6. Shen L, Yuan T, Chen S, Xie X, Zhang C. The temporal effect of platelet-rich plasma on pain and physical function in the treatment of knee osteoarthritis: systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res. 2017;12(1):1–12. doi:10.1186/s13018-017-0521-3
7. Nguyen C, Lefèvre-Colau MM, Poiraudeau S, Rannou F. Evidence and recommendations for use of intra-articular injections for knee osteoarthritis. Ann Phys Rehabil Med. 2016;59(3):184–189. doi:10.1016/j.rehab.2016.02.008
8. Cui GH, Wang YY, Li CJ, Shi CH, Wang WS. Efficacy of mesenchymal stem cells in treating patients with osteoarthritis of the knee: a meta-analysis. Exp Ther Med. 2016;12(5):3390–3400. doi:10.3892/etm.2016.3791
9. Duymus TM, Mutlu S, Dernek B, Komur B, Aydogmus S, Kesiktas FN. Choice of intra-articular injection in treatment of knee osteoarthritis: platelet-rich plasma, hyaluronic acid or ozone options. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):485–492. doi:10.1007/s00167-016-4110-5
10. Sit RWS, Wu RWK, Rabago D, et al. Efficacy of intra-articular hypertonic dextrose (Prolotherapy) for knee osteoarthritis: a randomized controlled trial. Ann Fam Med. 2020;18(3):235–242. doi:10.1370/afm.2520
11. Boonstra AM, Preuper HRS, Balk GA, Stewart RE. Cut-off points for mild, moderate, and severe pain on the visual analogue scale for pain in patients with chronic musculoskeletal pain. Pain. 2014;155(12):2545–2550. doi:10.1016/j.pain.2014.09.014
12. Salaffi F, Leardini G, Canesi B, et al. Reliability and validity of the Western Ontario and McMaster Universities (WOMAC) osteoarthritis index in Italian patients with osteoarthritis of the knee. Osteoarthr Cartil. 2003;11(8):551–560. doi:10.1016/S1063-4584(03)00089-X
13. Yang ZY, Chen W, Li CX, et al. Medial compartment decompression by fibular osteotomy to treat medial compartment knee osteoarthritis: a pilot study. Orthopedics. 2015;38(12):e1110–4. doi:10.3928/01477447-20151120-08
14. Richardson SS, Kahlenberg CA, Blevins JL, et al. Complications associated with staged versus simultaneous bilateral total knee arthroplasty: an analysis of 7747 patients. Knee. 2019;26(5):1096–1101. doi:10.1016/j.knee.2019.06.008
15. Duivenvoorden T, Brouwer RW, Baan A, et al. Comparison of closing-wedge and opening-wedge high tibial osteotomy for medial compartment osteoarthritis of the knee. J Bone Jt Surg. 2014;96(17):1425–1432. doi:10.2106/JBJS.M.00786
16. Hernigou P, Giber D, Dubory A, Auregan JC. Safety of simultaneous versus staged bilateral opening-wedge high tibial osteotomy with locked plate and immediate weight bearing. Int Orthop. 2020;44(1):109–117. doi:10.1007/s00264-019-04385-z
17. Wang X, Wei L, Lv Z, et al. Proximal fibular osteotomy: a new surgery for pain relief and improvement of joint function in patients with knee osteoarthritis. J Int Med Res. 2017;45(1):282–289. doi:10.1177/0300060516676630
18. Pan D, Tianye L, Peng Y, et al. Effects of proximal fibular osteotomy on stress changes in mild knee osteoarthritis with varus deformity: a finite element analysis. J Orthop Surg Res. 2020;15(1):1–10. doi:10.1186/s13018-020-01894-1
19. Nie Y, Ma J, Huang ZY, et al. Upper partial fibulectomy improves knee biomechanics and function and decreases knee pain of osteoarthritis: a pilot and biomechanical study. J Biomech. 2018;71:22–29. doi:10.1016/j.jbiomech.2017.12.004
20. Guo J, Zhang L, Qin D, et al. Changes in ankle joint alignment after proximal fibular osteotomy. PLoS One. 2019;14(3):e0214002.
21. Ryan W, Mahony N, Delaney M, O’Brien M, Murray P. Relationship of the common peroneal nerve and its branches to the head and neck of the fibula. Clin Anat. 2003;16(6):501–505. doi:10.1002/ca.10155
22. Pratiwi AB, Setiyaningsih H, Kok MO, Hoekstra T, Mukti AG, Pisani E. Is Indonesia achieving universal health coverage? Secondary analysis of national data on insurance coverage, health spending and service availability. BMJ Open. 2021;11(10):10. doi:10.1136/bmjopen-2021-050565
23. Rabago D, Patterson JJ, Mundt M, et al. Dextrose prolotherapy for knee osteoarthritis: a randomized controlled trial. Ann Fam Med. 2013;11(3):229–237. doi:10.1370/afm.1504
24. Rabago D, Zgierska A, Fortney L, et al. Hypertonic dextrose injections (prolotherapy) for knee osteoarthritis: results of a single-arm uncontrolled study with 1-year follow-up. J Altern Complement Med. 2012;18(4):408–414. doi:10.1089/acm.2011.0030
25. Eslamian F, Amouzandeh B. Therapeutic effects of prolotherapy with intra-articular dextrose injection in patients with moderate knee osteoarthritis: a single-arm study with 6 months follow up. Ther Adv Musculoskelet Dis. 2015;7(2):35–44. doi:10.1177/1759720X14566618
26. Arias-Vázquez PI, Tovilla-Zárate CA, Legorreta-Ramírez BG, et al. Prolotherapy for knee osteoarthritis using hypertonic dextrose vs other interventional treatments: systematic review of clinical trials. Adv Rheumatol. 2019;59(1):39. doi:10.1186/s42358-019-0083-7
27. Convery PN, Milligan KR, Quinn P, Sjövall J, Gustafsson U. Efficacy and uptake of ropivacaine and bupivacaine after single intra-articular injection in the knee joint. Br J Anaesth. 2001;87(4):570–576. doi:10.1093/bja/87.4.570
28. Pietruck C, Grond S, Xie GX, Palmer PP. Local anesthetics differentially inhibit sympathetic neuron-mediated and C fiber-mediated synovial neurogenic plasma extravasation. Anesth Analg. 2003;96(5):1397–1402. doi:10.1213/01.ANE.0000060454.34258.D3
29. Dragoo JL, Braun HJ, Kim HJ, Phan HD, Golish SR. The in vitro chondrotoxicity of single-dose local anesthetics. Am J Sports Med. 2012;40(4):794–799. doi:10.1177/0363546511434571
30. Di Salvo A, Chiaradia E, Della Rocca G, et al. Intra-articular administration of lidocaine plus Adrenaline in dogs: pharmacokinetic profile and evaluation of toxicity in vivo and in vitro. Vet J. 2016;208:70–75. doi:10.1016/j.tvjl.2015.09.004
31. Ravnihar K, Marš T, Pirkmajer S, et al. The influence of a single intra-articular lidocaine injection on the viability of articular cartilage in the knee. Cartilage. 2020;13(1_suppl):456S–463S. doi:10.1177/1947603520904759
32. Samson DJ, Grant MD, Ratko TA, Bonnell CJ, Ziegler KM, Aronson N. Treatment of primary and secondary osteoarthritis of the knee. Evid Rep Technol Assess. 2007;157:1–157.
33. Lim JU, Lee JH, Kim JS, et al. Comparison of World Health Organization and Asia-Pacific body mass index classifications in COPD patient. Respirology. 2017;22:4.
34. Zheng H, Chen C. Body mass index and risk of knee osteoarthritis: systematic review and meta-analysis of prospective studies. BMJ Open. 2015;5(12):12. doi:10.1136/bmjopen-2014-007568
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.