Back to Journals » Cancer Management and Research » Volume 12
Combination of Hematology Indicators and Oncological Characteristics as a New Promising Prognostic Factor in Localized Clear Cell Renal Cell Carcinoma
Authors Kang X , Shi H , Wang D, Xiao Z, Tian J, Bi X, Jiang W, Li C, Ma J, Zheng S, Sun Y, Shou J
Received 25 May 2020
Accepted for publication 24 September 2020
Published 12 October 2020 Volume 2020:12 Pages 10023—10033
DOI https://doi.org/10.2147/CMAR.S264400
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Lu-Zhe Sun
Xiangpeng Kang,1 Hongzhe Shi,1 Dong Wang,1 Zejun Xiao,1 Jun Tian,1 Xingang Bi,1 Weixing Jiang,1 Changling Li,1 Jianhui Ma,1 Shan Zheng,2 Yueping Sun,3 Jianzhong Shou1
1Department of Urinary Surgery, National Cancer Center, National Clinical Research Center for Cancer, Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100021, People’s Republic of China; 2Department of Pathology, National Cancer Center, National Clinical Research Center for Cancer, Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100021, People’s Republic of China; 3Institute of Medical Information, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100020, People’s Republic of China
Correspondence: Yueping Sun Email [email protected]
Jianzhong Shou Email [email protected]
Purpose: This study aimed to construct a predictive model for recurrence and metastasis in patients with localized clear cell renal cell carcinoma (ccRCC) based on multiple preoperative blood indexes and oncological characteristics.
Patients and Methods: Overall, 442 patients with localized ccRCC between 2013 and 2015 were included. Using least absolute shrinkage and selection operator (LASSO) Cox regression analysis, the top three risk factors from the peripheral blood indicators were screened to construct a risk score, and a prognostic model was established. Harrell’s concordance index (C-index) was applied to evaluate the predictive accuracy of the model for predicting disease-free survival (DFS) in ccRCC.
Results: Out of 38 blood indexes, the top three predictors were fibrinogen (FIB), C-reactive protein (CRP) and neutrophil-lymphocyte ratio (NLR). The FIB-CRP-NLR (FCN) score (hazard ratio [HR]: 1.86, 95% confidence interval [CI]: 1.21– 2.9, P = 0.005) was an independent prognostic factor in multivariate analysis. Furthermore, the FIB-CRP-NLR-T-Grade (FCNTG) risk model combining FCN score, T stage and Furhman grade achieved a higher prognostic accuracy (mean C-index, 0.728) than both the FCN score alone (mean C-index, 0.675) and the stage, size, grade, and necrosis (SSIGN) score (mean C-index, 0.686) in the validation cohort.
Conclusion: The FCN score combining peripheral blood indicators of inflammation and coagulation is an independent prognostic marker of ccRCC. The FCNTG model, which systemically incorporates preoperative blood indexes to oncological characteristics, shows its advantages of convenience and high prediction efficiency.
Keywords: clear cell renal cell carcinoma, prognosis, fibrinogen, C-reactive protein, neutrophil-lymphocyte ratio
Introduction
Renal cell carcinoma (RCC) is the third most common urological cancer, with an estimated more than 70,000 new cases and 14,000 deaths per year.1 Although most patients with localized clear cell renal cell carcinoma (ccRCC) present as slow-growing tumors, one-quarter of patients experience disease recurrence and metastasis after complete surgical resection.2 Clinical staging with tools such as the University of Los Angeles Integrated Staging System (UISS) and the Mayo Clinic Stage, Size, Grade, and Necrosis (SSIGN) score are valuable for prognostication.3 However, these models did not take into account of the cancer-related inflammation and coagulation factors, which comprising an essential component of the tumor microenvironment.4,5 To date, some studies have evaluated the prognostic role of pretreatment blood parameters including C-reactive protein (CRP), neutrophil-lymphocyte ratio (NLR), fibrinogen (FIB) and erythrocyte sedimentation rate (ESR).6–10 Nevertheless, these studies evaluated only one or two indexes, and the mechanism was unclear.
We have reported that the plasma concentrations of FIB, CRP and neutrophils were positively correlated with the circulating tumor cells (CTCs), which was a prerequisite for recurrence and metastasis.11 In this study, we evaluated the preoperative blood indexes to explore a risk classification for predicting disease-free survival (DFS) in patients with stage I–III ccRCC.
Patients and Methods
Patients
This retrospective cohort study collected 712 patients with stage I–III ccRCC who underwent partial or radical nephrectomy at the Cancer Institute and Hospital of the Chinese Academy of Medical Sciences (CAMS) from March 2013 to March 2015. The clinical data, including general demographic factors, preoperative peripheral blood indicators, and clinicopathological parameters were collected.
The inclusion criteria of the study were as follows: (1) no primary cancer of any other organs before the operation; (2) no chronic inflammatory allergic disease; (3) no history of taking anticoagulants such as for cardiovascular or cerebrovascular thrombosis; (4) exact pathological diagnosis of ccRCC; (5) complete resection of the tumor, which was defined as a negative incisal margin; (6) complete clinicopathological characteristics and follow-up data; and (7) no evidence of extrarenal metastasis. Finally, 442 patients with stage I–III ccRCC were enrolled in this study (Figure 1). The study protocol was approved by the Ethics Committee of the Cancer Institute and Hospital of the CAMS, and all patients provided informed consent.
 |
Figure 1 Study flowchart. |
Clinicopathological Data
The clinicopathologic parameters were investigated retrospectively including age, sex, the clinical and histopathological characteristics and preoperative peripheral blood indexes (Table 1). The pathological characteristics were evaluated according to the 2010 Fuhrman grading system, and the 2010 American Joint Committee on Cancer TNM classification.12 Additionally, peripheral blood samples were obtained within 2 weeks before the operation in our hospital.
 |
Table 1 Baseline Characteristics of 442 Patients |
Follow-Up
All patients were followed up regularly. Follow-up assessments were routinely performed in intervals of 3–6 months for the first 2 years and then once a year thereafter, in accordance with the standard follow-up procedures of our institution. Physical examination, routine laboratory tests, and imaging screenings, such as chest X-ray and abdominal computed tomography (CT), were performed in every follow-up. The endpoint was the DFS time, which was calculated as the interval between surgery and the last follow-up or the date of recurrence, metastasis or death.
Statistical Analysis
The dataset was split into training and validation cohorts with repeated random sampling until there was no significant difference (P value > 0.05) between the two cohorts with respect to all variables (Table 1). The P value was calculated using Welch’s t-test for continuous variables and χ2 test or Fisher’s exact test for categorical variables.
The blood indexes were selected by least absolute shrinkage and selection operator (LASSO) Cox regression (R software and “glmnet” package). Then, the optimal cut-off values were determined by X-tile. Furthermore, we evaluated the prognostic accuracy of the risk model using Harrell’s concordance index (C-index), which is appropriate for censored data.13 All statistical tests were two-sided, a P value < 0.05 was statistically significant. Both the multivariable Cox regression model and the C-index were completed with R version 3.6.2. and mean C-index calculation using Stata 14.0 (Stata Corp. Texas, USA).
Results
Patient Demographics
The median follow-up time (interquartile range) was 58.7 months (range 51.7 to 65.1 months). Overall, 58 (13.1%) patients had tumor recurrence, metastasis or death, including 36 patients with distant metastasis, 15 patients with local recurrence and 7 patients died of other causes. In all, 35 (7.9%) patients died due to various reasons during the follow-up period. The time to progress (TTP) which was calculated as the interval between surgery and the date of recurrence or metastasis. The 5-year TTP rates were 88.3% (95% confidence interval [CI]: 84.9–91.1%), and the 5-year DFS rates was 86.9% (95% CI: 83.3–89.7%).
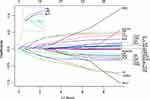
FCN Score, and the Relationship Between FCN Score and Clinical Characteristics
The top three important prognostic markers screened by LASSO Cox regression out of 38 blood indexes were FIB, CRP, and NLR (Figure 2). The optimal cutoff values for FIB, CRP and NLR were 2.77 g/L, 0.2 mg/dL and 1.68, respectively. Thus, patients with low levels of all three indicators, FIB < 2.77 g/L, CRP < 0.2 mg/dL, and NLR < 1.68, were scored as 0. Patients were scored 1, 2, and 3 on the basis of these three indicators, respectively. Higher FCN score was significantly associated with larger tumor size (P = 0.04), more advanced T stage (P = 0.019) and higher SSIGN score (P = 0.002) (Table 2).
 |
Table 2 Association of FCN Score with Tumor Pathological Characteristics, TNM and SSIGN Score in the Training Cohort |
Prognostic Risk Model Combining FCN Score, T Stage and Furhman Grade
The multivariate Cox regression analysis in the training cohort further showed that FCN score (hazard ratio [HR]: 1.86, 95% CI: 1.21–2.9, P = 0.005) and T stage (HR: 1.53, 95% CI: 1.23–1.9, P < 0.001) were independent risk factors for DFS in patients with ccRCC (Figure 3). Additionally, the basophils count, body mass index (BMI), diabetes status, systemic inflammatory marker (SIM) score and modified Glasgow prognostic score (mGPS) calculated according to the cutoffs in the literature,14–16 were unindependent risk factors in multivariate analysis (P > 0.05). Therefore, the FIB-CRP-NLR-T-Grade (FCNTG) risk model combining FCN score, T stage and Furhman grade was constructed (Figure 4).
 |
Figure 3 Multivariate Cox regression analysis in the training cohort. The FCN score and T stage were independent risk factors for DFS in patients with ccRCC. |
 |
Figure 4 The FIB-CRP-NLR-T-Grade (FCNTG) risk model combining FCN score, T stage and Furhman grade. |
Comparison of Predictive Accuracy Between the FCNTG Model and the FCN Score Alone
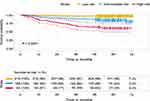
The predictive power for prognosis of DFS between the FCNTG model and other variables were compared. The mean C-index of the FCNTG model was 0.728 (95% CI: 0.625–0.834), which was significantly higher than that of the single FCN score (mean C-index: 0.675, 95% CI: 0.574–0.776) (Table 3; Figure 5A).
 |
Table 3 Concordance Index Analysis of the Prognostic Accuracy of FCNTG and Other Variables for DFS in Indicated Sets |
Comparison of Predictive Accuracy Between the FCNTG Model and the SSIGN Score
As shown in Table 3, the C-index of the FCNTG model for predicting DFS in the validation cohort was 0.728 (95% CI, 0.625–0.834), which was significantly higher than that of the SSIGN score (0.686, 95% CI: 0.582–0.789). The calibration curve showed good agreement between prediction and observation in the probability of 3-year DFS (Figure 5B) and 5-year DFS (Figure 5C). In the overall data, the 5-year DFS rates of patients with low-, intermediate-, and high-risk kidney cancer grouped by the FCNTG model were 97%, 84% and 61%, respectively (P < 0.0001) (Figure 6).
Discussion
As malignant tumors are the result of genetic mutations, it is necessary to comprehensively consider the immune status of the body and the biological characteristics of the tumor to improve the accuracy of prognostic predictions for malignant tumors.17,18 The commonly used SSIGN score and UISS exclude the hematological indicators that reflect the state of the body, which may lead to their limited predictive effectiveness.19 Some studies have reported the predictive value of hematology indicators, such as basophil, SIM score, and mGPS which is the incorporation of CRP and albumin levels.14,16,20–22 Furthermore, The FIB, D-dimers, and ESR are all related to the poor prognosis of patients with RCC.7,9,23,24 However, it is unclear which indicator or set of indicators provide the greatest accuracy for prognosis, and the mechanism has not been clarified.
Machine learning methods can detect more effective prognostic factors that are difficult to identify from the complex combination of multiple parameters.25 Therefore, in this study, we applied a Cox proportional hazards model using LASSO penalization to screen 38 blood indexes; this approach favored the selection of blood indicators with powerful prognostic value, and the three strongest blood indexes, FIB, CRP, and NLR, were all related to coagulation and inflammation status. It has been suggested that FIB, an extracellular matrix component, promotes the growth of cancer cells in the tumor microenvironment by binding to fibroblast growth factor 2 and vascular endothelial growth factor.26 The CRP concentration may be elevated owing to hepatic CRP synthesis, which is stimulated by cancer cell-derived inflammatory cytokines.27 Neutrophils may also contribute to tumor development and progression by providing an adequate tumor microenvironment via the production of cytokines and chemokines.28 Our previous research also pointed out that the abnormality of inflammation and coagulation indexes is correlated with viable CTCs, which is the premise of tumor recurrence and metastasis, and the neutrophil extracellular traps (NETs) induced by circulating neutrophils could protect the survival of circulating tumor cells, thus promoting postoperative recurrence and metastasis in patients with RCC.11 Therefore, it is reasonable to construct a prognostic model for local renal cell carcinoma based on the combination of hematological indicators FIB, CRP, and NLR.
In this study, although the basophils count, BMI, diabetes status, SIM score and mGPS were positively associated with the risk of recurrence and metastasis in multivariate Cox regression analysis, but these indicators were not independent prognostic risk factors. Finally, we constructed an FCNTG model to predict the prognosis of patients with localized ccRCC which combined peripheral blood indicators of inflammation and coagulation and oncology staging information. The predictive effectiveness of the FCNTG model (C-index, 0.728) was higher than that of the SSIGN score (C-index, 0.686), and the 5-year DFS rates of the patients with low-, intermediate-, and high-risk kidney cancer grouped by the FCNTG model were 97%, 84%, and 61%, respectively. Therefore, the FCNTG model combining peripheral blood markers and tumor stage was consistent with the idea that integrating multiple markers may provide higher accuracy,29 and the model showed the advantages of convenience and high prediction efficiency.
The limitations of this study are as follows: first, the inherent bias associated with its retrospective design. Second, the number of cases is relatively small. In the future, we hope to accumulate more cases and carry out multicenter and prospective studies to further verify the predictive performance of the model.
In conclusion, we found the FIB, CRP, and NLR indexes could reflect the antitumor status of patients with kidney cancer. Furthermore, the FCNTG model, which combines inflammatory and coagulation indicators with tumor stage and grade information, improves the accuracy of prognostic predictions for patients with ccRCC.
Abbreviations
RCC, renal cell carcinoma; ccRCC, clear cell renal cell carcinoma; BMI, body mass index; CI, confidence interval; C-index, concordance index; SSIGN, stage, size, grade, and necrosis; DFS, disease-free survival; CTCs, circulating tumor cells; WBC, white blood cell count; Hb, hemoglobin; PLT, platelet count; PDW, platelet distribution width; PCT, platelet hematocrit, HCT, hematocrit; NEUT, neutrophil count; NETU%, neutrophil percentage; LYMPH, lymphocyte count; MONO, monocyte count; MONO%, monocyte percentage; NLR, neutrophil-lymphocyte ratio; EOS, eosinophils count; BAS, basophils count; AST, aspartate aminotransferase; ALT, alanine aminotransferase; ALP, alkaline phosphatase; GGT, glutamyl transferase; LDH, lactate dehydrogenase; TBIL, total bilirubin; TP, total protein; Alb, albumin; URIC, uric acid; BUN, blood urea nitrogen; CRE, creatinine; IgA, immunoglobulin A; IgG, immunoglobulin G; IgM, immunoglobulin M; CRP, C-reactive protein; PT, prothrombin time; APTT, activated partial thromboplastin time; FIB, fibrinogen; PLR, platelet-lymphocyte ratio; FAR, fibrinogen-albumin ratio; ESR, erythrocyte sedimentation rate; LMR, lymphocyte-monocyte ratio; SIM score, systemic inflammatory marker score; mGPS, modified Glasgow prognostic score.
Funding
This work was supported by the Chinese Academy of Medical Sciences (CAMS) Initiative for Innovative Medicine [2016-I2M-1-007], Beijing hope run special fund of cancer foundation of China [LC2018L02], and the Chinese Academy of Medical Sciences (CAMS) Initiative for Innovative Medicine [2016-I2M-2-005].
Disclosure
The authors report no conflicts of interest in this work.
References
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(11):1. doi:10.3322/caac.21551
2. Finelli A, Ismaila N, Bro B, et al. Management of small renal masses: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2017;35(6):668–680. doi:10.1200/JCO.2016.69.9645
3. Frank I, Blute ML, Cheville JC, Lohse CM, Weaver AL, Zincke H. An outcome prediction model for patients with clear cell renal cell carcinoma treated with radical nephrectomy based on tumor stage, size, grade and necrosis: the SSIGN score. J Urol. 2002;168(6):2395–2400. doi:10.1016/S0022-5347(05)64153-5
4. Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A. Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis. 2009;30(7):1073–1081. doi:10.1093/carcin/bgp127
5. Dolan RD, McSorley ST, Horgan PG, Laird B, McMillan DC. The role of the systemic inflammatory response in predicting outcomes in patients with advanced inoperable cancer: systematic review and meta-analysis. Crit Rev Oncol Hematol. 2017;116:134–146. doi:10.1016/j.critrevonc.2017.06.002
6. Dalpiaz O, Luef T, Seles M, et al. Critical evaluation of the potential prognostic value of the pretreatment-derived neutrophil-lymphocyte ratio under consideration of C-reactive protein levels in clear cell renal cell carcinoma. Br J Cancer. 2017;116(1):85–90.
7. Guo S, He X, Chen Q, et al. The C-reactive protein/albumin ratio, a validated prognostic score, predicts outcome of surgical renal cell carcinoma patients. BMC Cancer. 2017;17(1):171. doi:10.1186/s12885-017-3119-6
8. Ohno Y, Nakashima J, Ohori M, Hatano T, Tachibana M. Pretreatment neutrophil-to-lymphocyte ratio as an independent predictor of recurrence in patients with nonmetastatic renal cell carcinoma. J Urol. 2010;184(3):873–878.
9. Erdem S, Amasyali AS, Aytac O, Onem K, Issever H, Sanli O. Increased preoperative levels of plasma fibrinogen and D dimer in patients with renal cell carcinoma is associated with poor survival and adverse tumor characteristics. Urol Oncol. 2014;32(7):1031–1040. doi:10.1016/j.urolonc.2014.03.013
10. Pichler M, Hutterer GC, Stoeckigt C, et al. Validation of the pre-treatment neutrophil-lymphocyte ratio as a prognostic factor in a large European cohort of renal cell carcinoma patients. Br J Cancer. 2013;108(4):901–907. doi:10.1038/bjc.2013.28
11. Wen L, Guo L, Zhang W, et al. Cooperation between the inflammation and coagulation systems promotes the survival of circulating tumor cells in renal cell carcinoma patients. Front Oncol. 2019;9:504. doi:10.3389/fonc.2019.00504
12. Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17(6):1471–1474. doi:10.1245/s10434-010-0985-4
13. Harrell FE, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15(4):361–387. doi:10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4
14. Ferro M, Di Lorenzo G, Vartolomei MD, et al. Absolute basophil count is associated with time to recurrence in patients with high-grade T1 bladder cancer receiving bacillus Calmette-Guérin after transurethral resection of the bladder tumor. World J Urol. 2020;38(1):143–150. doi:10.1007/s00345-019-02754-2
15. Cantiello F, Russo GI, Vartolomei MD, et al. Systemic inflammatory markers and oncologic outcomes in patients with high-risk non-muscle-invasive urothelial bladder cancer. Eur Urol Oncol. 2018;1(5):403–410. doi:10.1016/j.euo.2018.06.006
16. Ferro M, De Cobelli O, Buonerba C, et al. Modified glasgow prognostic score is associated with risk of recurrence in bladder cancer patients after radical cystectomy: a multicenter experience. Medicine. 2015;94(42):e1861. doi:10.1097/MD.0000000000001861
17. Elinav E, Nowarski R, Thaiss CA, Hu B, Jin C, Flavell RA. Inflammation-induced cancer: crosstalk between tumours, immune cells and microorganisms. Nat Rev Cancer. 2013;13(11):759–771. doi:10.1038/nrc3611
18. Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–674. doi:10.1016/j.cell.2011.02.013
19. Zigeuner R, Hutterer G, Chromecki T, et al. External validation of the mayo clinic stage, size, grade, and necrosis (SSIGN) score for clear-cell renal cell carcinoma in a single European centre applying routine pathology. Eur Urol. 2010;57(1):102–109. doi:10.1016/j.eururo.2008.11.033
20. Teishima J, Ohara S, Shinmei S, et al. Normalization of C-reactive protein levels following cytoreductive nephrectomy in patients with metastatic renal cell carcinoma treated with tyrosine kinase inhibitors is associated with improved overall survival. Urol Oncol. 2018;36:7. doi:10.1016/j.urolonc.2018.04.008
21. Hu H, Yao X, Xie X, et al. Prognostic value of preoperative NLR, dNLR, PLR and CRP in surgical renal cell carcinoma patients. World J Urol. 2017;35(2):261–270. doi:10.1007/s00345-016-1864-9
22. Liu R, Zhou X, Zou L, et al. Clinicopathological and prognostic significance of preoperative plasma fibrinogen level in patients with upper urinary tract urothelial carcinoma: a retrospective tumor marker prognostic study. Int J Surg. 2019;65:88–93. doi:10.1016/j.ijsu.2019.03.022
23. Tanaka N, Kikuchi E, Matsumoto K, et al. Prognostic value of plasma fibrinogen levels in patients with localized upper tract urothelial carcinoma. BJU Int. 2013;111(6):857–864. doi:10.1111/j.1464-410X.2012.11353.x
24. Azuma T, Matayoshi Y, Odani K, et al. Preoperative neutrophil-lymphocyte ratio as an independent prognostic marker for patients with upper urinary tract urothelial carcinoma. Clin Genitourin Cancer. 2013;11(3):337–341. doi:10.1016/j.clgc.2013.04.003
25. Cruz JA, Wishart DS. Applications of machine learning in cancer prediction and prognosis. Cancer Inform. 2007;2:59–77.
26. Sahni A, Simpson-Haidaris PJ, Sahni SK, Vaday GG, Francis CW. Fibrinogen synthesized by cancer cells augments the proliferative effect of fibroblast growth factor-2 (FGF-2). J Thromb Haemost. 2008;6(1):176–183. doi:10.1111/j.1538-7836.2007.02808.x
27. Ohno Y. Role of systemic inflammatory response markers in urological malignancy. Int J Urol. 2019;26(1):31–47.
28. Gregory AD, Houghton AM. Tumor-associated neutrophils: new targets for cancer therapy. Cancer Res. 2011;71(7):2411–2416. doi:10.1158/0008-5472.CAN-10-2583
29. Rakha EA, Reis-Filho JS, Ellis IO. Combinatorial biomarker expression in breast cancer. Breast Cancer Res Treat. 2010;120(2):293–308. doi:10.1007/s10549-010-0746-x
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.