Back to Journals » International Journal of General Medicine » Volume 15
Colistin Therapy, Survival and Renal Replacement Therapy in Burn Patients: A 10-Year Single-Center Cohort Study
Authors Mariano F , Malvasio V, Risso D, Depetris N, Pensa A, Fucale G, Gennari F, Biancone L, Stella M
Received 12 January 2022
Accepted for publication 24 March 2022
Published 25 May 2022 Volume 2022:15 Pages 5211—5221
DOI https://doi.org/10.2147/IJGM.S357427
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Filippo Mariano,1,2,* Valeria Malvasio,3,4,* Daniela Risso,3 Nadia Depetris,5 Anna Pensa,3,6 Giacomo Fucale,7 Fabrizio Gennari,4 Luigi Biancone,1,2 Maurizio Stella3
1Nephrology, Dialysis and Transplantation U, Department of General and Specialized Medicine, City of Science and Health, CTO Hospital, Torino, Italy; 2Department of Medical Sciences, University of Torino, Torino, Italy; 3Burn Center and Plastic Surgery, Department of General and Specialized Surgery, City of Science and Health, CTO Hospital, Torino, Italy; 4Department of Pediatric General Surgery, City of Science and Health, Regina Margherita Children’s Hospital, Torino, Italy; 5Anesthesia and Intensive Care 3, Department of Anesthesia and Intensive Care, City of Science and Health, CTO Hospital, Torino, Italy; 6Department of Surgical Sciences, University of Torino, Torino, Italy; 7Laboratory of Microbiology and Virology, City of Science and Health, Molinette Hospital, Torino, Italy
*These authors contributed equally to this work
Correspondence: Filippo Mariano, Nephrology, Dialysis and Transplantation U, AOU City of Science and Health, CTO Hospital, Via G. Zuretti 29, Torino, 10126, Italy, Tel +39-011-6933-674, Fax +39-011-6933-672, Email [email protected]
Purpose: Colistin is still a therapeutic cornerstone against multidrug-resistant gram-negative bacteria (MDRGN), mostly when other antibiotics do not gain adequate activity on these strains. In the present study, we evaluated in a cohort of burn patients the relationship between colistin therapy, survival and requirement of renal replacement therapy (CRRT).
Patients and Methods: Retrospective study of 133 burn patients treated with iv colistimethate sodium (loading dose 9.0 × 106 IU, maintenance dose 4.5 × 106 IU BID) and 35 treated with other antibiotics for MDRGN infection including Acinetobacter baumannii, Pseudomonas aeruginosa, and Klebsiella pneumoniae between January 2008 and December 2017. Multivariate analysis with logistic regression was used to determine the effect of the predictors such as age, total body surface area (TBSA), third-degree burn areas, Revised Baux score, Charlson comorbidity score, length of stay, colistin dose and duration of treatment, mechanical ventilation, and need of CRRT on in-hospital mortality. To investigate the relationship between colistin and renal function, we focused on survivor patients as the completion of the therapeutic course of colistin represented the basic requirement to analyze its impact on the kidney.
Results: Out of 133 colistin- and 35 other antibiotics-treated patients, 83 (62.4%) and 31 (88.6%) survived, and 53 (39.8%) and 3 (9.7%) required CRRT, respectively. The severity of burns, as well as CRRT requirement and mortality, was significantly higher in colistin-treated patients than in other antibiotics-treated patients. Age and TBSA% were the significant predictors of mortality. Out of 83 colistin-treated survivors, 19 (22.9%) required CRRT (9 before and 10 after the start of colistin), and 64 (77.1%) had a normal renal function. No difference about the colistin dose and baseline characteristics, but the revised Baux score was found between the 9 patients requiring CRRT before the colistin course and the 10 patients after. Similarly, among the 64 patients not undergoing CRRT, no difference was found between the patients treated with the cumulative dose of colistin < 99.0 × 106 IU (n = 33, median daily dose of 4.0 × 106 IU) and > 99.0 × 106 IU (n = 31, median daily dose of 9.0 × 106 IU) about the baseline characteristics and the daily median plasma creatinine over 24 days of therapy.
Conclusion: Colistin therapy was associated with more severe burns, mortality, and CRRT requirement. A short course therapy, at appropriate cumulative dosage, can lead to clinical success without a significant association with severe renal impairment.
Keywords: colistin, burns, acute kidney injury, MDRGN infection, CRRT, clinical outcome
Plain Language Summary
Colistin is still a therapeutic cornerstone against multidrug-resistant gram-negative bacteria (MDRGN), and we reviewed our experience in 133 severe burn patients evaluating the relationship between colistin therapy, survival, and renal function.
Out of them, 50 did not survive. Non-survivors were significantly older and had a higher severity of burns and acute kidney injury rate than the 83 survivor patients.
To investigate the renal function, we focused on the 83 survivor patients as the completion of the therapeutic course of colistin represented the basic requirement to analyze its impact on the kidney. Out of these, 19 underwent renal replacement therapy. No difference in colistin dose and baseline characteristics, except revised Baux score, was found between the 9 patients who started CRRT before and the 10 patients after the colistin course. Similarly, for the 64 remaining patients, we found no difference between the patients treated with the cumulative dose of colistin <99.0 × 106 IU (n = 33, median daily dose of 4.0 × 106 U) and >99.0 × 106 U (n = 31, median daily dose of 9.0 × 106 IU) about the baseline characteristics. Similarly, no significant difference in the daily median plasma creatinine over 24 days of therapy was present between the two groups.
Colistin therapy was associated with more severe burns, mortality, and CRRT requirement. A short course therapy, at appropriate cumulative dosage, can lead to clinical success without a significant association with severe renal impairment.
Introduction
Multidrug-resistant gram-negative (MDRGN) bacteria are recognized as important threats in intensive care units and burn centers.1–3 Impaired host defense, loss of protective skin and mucosal barrier, and depressed immune system response make burn patients particularly exposed.2–4 Infections sustained by MDRGN bacteria in burn patients remain a challenge with high morbidity, mortality, and a longer hospital stay.4–7
Polymyxins B and E, known as colistin, are still a therapeutic cornerstone against multidrug-resistant gram-negative bacteria.8,9 In burn patients, colistin treatment continues to assume a key role as salvage therapy, mostly when other antibiotics do not gain an adequate activity on these strains and even if the availability of possible alternative drugs (aminoglycosides, fosfomycin, minocycline and more recently developed molecules) has improved the possibility to survive septic challenges.
Data regarding colistin optimal dosing strategies,10–12 potential adverse effects on renal function12,13 and factors influencing survival in burn patients with MDRGN bacteria sepsis remain undefined. Besides, controversies still exist concerning the duration of colistin therapy as well as its role in AKI development.12–14 In 2019 American College of Clinical Pharmacy (ACCP), European Society of Clinical Microbiology and Infectious Diseases (ESCMID), Infectious Diseases Society of America (IDSA), International Society for Anti-infective Pharmacology (ISAP), Society of Critical Care Medicine (SCCM), and Society of Infectious Diseases Pharmacists (SIDP) reported the first consensus therapeutic guidelines for optimal use of polymyxin (Colistin and Polymyxin B) in adult patients, focusing their attention on pharmacokinetic and pharmacodynamic properties, pharmacokinetic targets, dosing, dosage adjustment, monitoring, use of polymyxin-based combination therapy, intrathecal therapy, inhalation therapy, toxicity, and prevention of renal failure.15
As recently stated, the most important risk factor for polymyxin-associated severe AKI is the magnitude of polymyxin exposure, in terms of higher colistin doses (colistin dose ~150,000 IU/kg/day), a cumulative dose, and the association of other potentially nephrotoxic agents.15 A short-course therapeutic approach can reduce ecological pressure and diminish the side effects, including nephrotoxicity.16–18 Therefore, it has been suggested to shorten the duration of antibiotic therapy, from the traditional 14–21 days to a short course differently defined from 7 to 14 days.16,17
In the present study, we report our experience on colistin use in 133 patients treated at Burn Center of Torino (Italy) from 2008 to 2017. We aimed to determine the predictors of in-hospital mortality and the impact of colistin on the requirement of renal replacement therapy (CRRT). As the completion of the therapeutic course represented the basic requirement to analyze the potential nephrotoxicity of colistin treatment, we focused on the survivor patients to investigate the relationship between colistin therapy and renal function.
Materials and Methods
Study Design
We retrospectively collected data for the 133 burn patients admitted to our Burn Intensive Care Unit with MDRGN infection with the only residual sensibility to colistin, and consecutively treated with colistin between January 1, 2008 and December 31, 2017.
As a control group, we also retrospectively collected data for the 35 burn patients admitted to our Burn Intensive Care Unit with MDRGN infection and consecutively treated with other antibiotics but colistin between January 1, 2015 and December 31, 2017. The other antibiotics included tigecycline, ceftazidime/avibactam, ceftobiprole, or ceftolozane/tazobactam. The period from 2015 to 2017 was chosen on the basis of the availability of these antibiotics specifically active against MDRGN on the Italian market starting from 2015.
We found significantly increased indexes of burn severity, mortality and CRRT requirement in Colistin treated group in comparison with the other antibiotics-treated group. As acute renal impairment is associated with increased mortality, therefore colistin may be a major mortality contributor by its potential nephrotoxic effect. Because many patients on colistin have died, colistin could not be captured as a major AKI contributor.
Therefore, for further analysis, we decided to consider only the 83 colistin-treated survivor patients as the completion of the therapeutic course represented the basic requirement to analyze the potential nephrotoxicity of colistin treatment.
For renal dysfunction, we considered the most severe stage of AKI in terms of CRRT requirement when metabolic and fluid demands exceed the kidney capacity to meet them, and in the remaining patients we determined the daily plasma creatinine level.19
Figure 1 shows the flowchart of the study.
 |
Figure 1 Flow-chart of patients treated for MDRGN infection. aCeftazidime/avibactam, ceftobiprole, or ceftolozane/tazobactam/tigecycline/others. |
Patients Population
All included patients were adults (defined as older than 14 years or with a body mass >50 kg). According to an indication of the manufacturer (Laboratori UCB S.p.A., Pianezza (TO), Italy) revised on May 30, 1995, and published on G.U. 36/95, before 2014 in patients on CRRT the administered colistin dose was 3.0–4.5 × 106 IU/day. Then, after 2014, according to the published available data, colistin was administered intravenously with a loading dose of 9.0 × 106 IU and at a maintenance dose of 4.5 × 106 IU twice a day.15,20–24
All patients were treated according to EUCAST’s recommendation. Breakpoints for colistin for Pseudomonas aeruginosa, Acinetobacter baumannii and Enterobacteriaceae were a susceptible breakpoint of 2 mg/L or lower and a resistant breakpoint greater than 2 mg/L.25
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of the City of Health and Science of Torino (dossier no. CS2/908 on August 6, 2018).
The consent to retrospectively review the medical notes and analyze the collected data was obtained from the patient or substitute decision-maker following local ethics committee regulations.
Data Collection
The following information was collected utilizing the institutional electronic medical record system: age, sex, height and weight, total body surface area (TBSA), third-degree burn areas, cause of burn, inhalation injury, mechanical ventilation, Revised Baux score, Charlson comorbidity score, length of stay, mortality, need of continuous renal replacement therapy (CRRT), colistin dose and duration of treatment.
Laboratory data included daily serum creatinine levels for 24 days after starting colistin therapy.
Mortality was calculated as in-hospital mortality, and all non-survivor patients died in the Intensive Care Unit or Burn Center ward.
For renal function, we considered only the requirement of CRRT in surviving patients. This choice was due to the difficult judgment on the cause of renal impairment, related to the septic process, colistin toxicity, and/or per se fatal outcome.
Statistical Analysis
Continuous data are expressed as median with interquartile range (IQR, Q1 to Q3), and categorical data as frequencies and percentages. The normal distribution of samples was tested with the Kolmogorov–Smirnov test.
Comparison between colistin-treated and other antibiotics-treated groups, and for colistin-treated patients between groups’ survivors and non-survivors was performed using independent t-test or Mann–Whitney U-test for continuous variables according to data distribution (age, total body surface area (TBSA), third-degree burn areas, Revised Baux score, Charlson comorbidity score, length of stay, colistin dose and duration of treatment) and Fisher's exact test for categorical variables (sex, mechanical ventilation, need of CRRT, mortality).
Multivariate analysis with logistic regression was used to determine the effect of the considered predictors on in-hospital mortality. Firstly, univariate analysis was performed to evaluate the predictive effect of each factor. Next, factors with a p-value <0.05 from the univariate test were included in full multiple logistic models.
Statistical computing and graphics were performed by Statistica v.10.1 (StatSoft, Tulsa, OK, USA).
Results
Demographic Characteristics of Burn Patients Treated for MDRGN Infection
Table 1 shows the demographic characteristics of patients with MDRGN infection treated with colistin (n = 133) and with other antibiotics (n = 35). The median age of 133 patients was 58 years with a TBSA of 35% (range, 20–45), third-degree areas of 20% (range, 10–30), and most patients were male (66%).
 |
Table 1 Baseline Characteristics of 168 Burn Patients with MDRGN Infection According to Treatment with Colistin or Other Antibiotics |
The indexes of burn severity (TBSA%), third-degree area, revised Baux score, Baux index, as well as mechanical ventilation, CRRT requirement and mortality, were significantly higher in colistin treated patients than in other antibiotics-treated patients (Table 1).
For burn etiologies, in the colistin-treated group, 119 (89.4%) cases were due to flame, 7 (5.3%) to electrocution and 7 (5.3%) to scald. In the other antibiotics-treated group, 33 (94.3%) cases were due to flame and 2 (5.7%) to scald.
As shown in Table 2, in patients of the colistin group (76%), skin was the most common site of infection, followed by lung and blood for both groups.
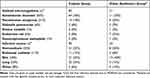 |
Table 2 Microorganism Isolates and Infection Sources of 83 Survivors of Colistin Group and 31 Survivors of Other Antibiotics Group |
Pathogens responsible for infection in the colistin group were Acinetobacter baumannii (76%), followed by Pseudomonas aeruginosa (18%), and Klebsiella pneumoniae (6%). Besides the above bacteria, in the other antibiotics-treated group, the involved microorganisms also included Escherichia coli, Stenotrophomonas, and Proteus (Table 2).
On the other hand, considering only the patients not undergoing CRRT, in non-survivors, TBSA% and third-degree areas were superimposable between the subgroups colistin- and other antibiotics-treated patients (Table 3, first two left columns), whereas in survivors, these indexes were significantly higher (as well as expected mortality) in the subgroup treated with colistin than in the subgroup treated with other antibiotics (Table 3, last two right columns).
 |
Table 3 Baseline Characteristics and Renal Function of Colistin- (n = 80) and Other Antibiotics (n = 32)-Treated Patients Not Undergoing CRRT |
Demographic Characteristics of Burn Survivor Patients of the Colistin Group
Of the 133 patients with MDRGN infection treated with colistin, 83 patients survived and 50 patients died. Table 4 compares the demographic characteristics of survivors and non-survivors. Non-survivors were significantly older, they had a higher percentage of third-degree burn areas, an higher expected mortality (revised Baux score) and Charlson comorbidity score, and a more frequent need for CRRT.
 |
Table 4 Analysis of Baseline Characteristics of 133 Burn Patients Treated with Colistin According to Survival |
Moreover, non-survivors presented a lower colistin dose, and shorter therapy duration (Table 4). These last data reflected the period before 2014 when available pharmacokinetic data indicated lower colistin dose for CRRT patients (dose 1.5 × 106 IU BID) than actual,15–25 and that in the deceased patients, the colistin course was not completed. By logistic regression analysis, age, percentage of the third-degree burn area, shorter course of colistin, and CRRT requirement were significantly correlated with mortality (Table 5).
 |
Table 5 Analysis of Risk Factors for Mortality as Identified Using Multivariate Logistic Regression Test (N = 133 Patients Treated with Colistin) |
Renal Function in Survivor Patients According to the Dose of Colistin and Timing of Therapy
In the 83 survivor patients treated with colistin, renal function was stable in 64, whereas 19 required CRRT (Figure 1). In the 64 patients with stable renal function, the median daily dose of colistin was 9.0 × 106 IU, and the median cumulative dose was 99.0 × 106 IU. According to the cumulative dose of colistin of 99.0 × 106 IU, we compared the patients’ group treated with <99.0 × 106 IU (group low dose, n = 33, median daily dose of 4.0 × 106 IU) with that >99.0 × 106 IU (group high dose, n = 31, median daily dose of 9.0 × 106 IU). We found no difference between the two groups in baseline characteristics (Table 6), as well as in the outcome of the renal function expressed in median daily creatinine levels up to 24 days of colistin therapy (Figure 2).
 |
Table 6 Baseline Characteristics of 64 Burn Survivor Patients Treated with Colistin Not Undergoing CRRT According to the Median Cumulative Dose of Colistin of 99.0 × 106 U |
In the remaining 19 patients requiring CRRT, 10 started CRRT after colistin therapy and 9 patients before. According to the timing of colistin therapy, no difference was found between the two groups for the length of therapy, cumulative dose and median dose of colistin, and baseline characteristics, but revised Baux score (Table 7).
 |
Table 7 Baseline Characteristics of 19 Burn Survivor Patients Who Underwent CRRT According to the Timing of Colistin Therapy |
Discussion
In the present cohort study of 133 severe burn patients treated with colistin, the predictors of mortality were as usual as those well known for the burn population. As colistin therapy may represent a further risk factor of acute kidney injury (AKI), its appropriate dosage requires careful analysis.
MDRGN bacteria infection is known to promote the epidemic spread and nosocomial transmission. Outbreaks caused by these microorganisms are difficult to control and treat, especially in burn centers, due to the physiological and clinical characteristics of patients.
The impact on mortality and morbidity of Acinetobacter baumannii and other MDRGN bacteria has been debated. Burn is a complex pathology, where several clinical aspects and severity of patient illness may influence mortality. Although studies provided evidence that MDRGN bacteria infection increase mortality,4,26,27 other investigations support the possibility that the clinical course of critically ill patients may be influenced by other variables and that subsequently, the acquisition of infection with MDRGN bacteria may not independently lead to poorer short- and long-term outcome.7,28–30 Our data showed that in colistin-treated patients the overall mortality rate of 37.6% (50/133 patients) was related to older age, a higher percentage of third-degree burn areas, and severity of AKI, all well-known risk factors for death in the general burn population.31,32 In the same way, by comparing colistin- and other antibiotic-treated groups, we found that a higher mortality rate and the severity of the burn were more frequently associated with MDRGN strains such as Acinetobacter baumannii, Pseudomonas aeruginosa and Klebsiella pneumoniae maintaining colistin as a unique sensitivity to antibiotics. In effect, the patients of the control group presented different types of MDRGN strains, and they were also treated with the new antibiotics specifically active against MDRGN when appropriate. However, most importantly, they were significantly less severely burned, and subsequently with a lower rate of mortality (see Tables 2 and 3).
Nephrotoxicity is the most common adverse effect associated with colistin use and is related to duration and dosage.16,33,34 In burn patients, it is not easy to discriminate how much kidney damage (and subsequent CRRT requirement and increased mortality) was due to the septic process, or colistin adverse effects. Even if we are aware that this may represent a bias, for all these reasons we focused on survivors as the completion of the therapeutic course of colistin represented the basic requirement to analyze its potential nephrotoxicity.
It has been recently stated that the amplitude of colistin exposure represents one of the main factors for polymyxin-associated AKI.16–18,25 The cutoff values varied between the studies, in general, high dose corresponded to intravenous colistin daily dose ≥9.0 × 106 IU for more than 10 days.25 For the 64 surviving patients who did not undergo CRRT, the median cumulative dose of 99.0 × 106 IU was administered. As shown in Table 6 and Figure 2, by comparing the group higher dose (>99.0 × 106 IU) and lower dose (<99.0 × 106 IU), no differences were found in baseline characteristics and the follow-up of creatinine up to the 24th day of therapy. Concerning the 19 patients who survived and required CRRT, we compared the group of patients who started CRRT after colistin therapy (10 patients) with that including the subjects who started CRRT before (n = 9 patients) (see Table 7). Similar to that seen in the 64 patients with stable renal function, no significant difference was found in terms of length of therapy, cumulative dose and a median daily dose of colistin, and baseline characteristics, but revised Baux score, which describes the severity of illness.35
According to previous reports,29–33,35 all these findings suggest that renal impairment in burn patients was associated with the severity of the burn and with the impact of infection sustained by MDRGN strains with the only residual sensibility to colistin. In addition, in our series of patients we did not find any significant association between colistin dose and renal impairment. Furthermore, according to previous reports,36–42 our data suggest that a cumulative dose of 100 × 106 IU, at a daily effective dose of 9.0 × 106 IU should not expose the patients to a significantly increased risk of colistin nephrotoxicity.
Our study suffers from some limitations. Firstly, it is a single-center, and it is a retrospective study subjected to all limitations for possible bias related to the selection of patients, Secondly, we are aware that the different periods’ length analyzed for colistin- and other antibiotics-treated patients would be another potential bias. Thirdly, AKI may be sustained by multifactorial causes besides colistin nephrotoxicity, such as low hematocrit, low serum albumin, and fluid overload.14,19,27,39,43 And fourthly, over the long stay in Burn Center, other confounding factors including concurrent pharmacological treatments and infections could play a role.
Notwithstanding these limitations, our study presents points of strength. Firstly, our study includes a relatively large population well characterized by several clinical and biological parameters. Secondly, a standardized dosing protocol for intravenous colistin was applied to all patients according to renal dysfunction, or renal replacement therapy and with the dosing protocol updated in time according to the data available.4,15,20–25
Conclusions
MDRGN infection represents a severe complication of the burn course, requiring a prompt diagnosis and an appropriate therapeutic approach. Colistin is still a life-saving drug, more frequently associated with more severe burns, higher mortality, and renal injury. A short course therapy at appropriate cumulative dosage can lead to clinical success without any significant association with severe renal impairment.
Abbreviations
AKI, acute kidney injury; CMS, colistimethate sodium; CRRT, continuous renal replacement Therapy; MDRGN bacteria, multidrug-resistant Gram-negative bacteria; TBSA, total body surface area.
Data Sharing Statement
The data used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of the City of Health and Science of Torino (dossier no. CS2/908 on August 6, 2018). The consent to retrospectively review the medical notes and analyze the collected data was obtained from all the patient or substitute decision-maker following local ethics committee regulations.
Consent for Publication
We state that the details of any images, videos, recordings, etc can be published, and that the person(s) providing consent have been shown the article contents to be published.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no external funding. This work is supported by a grant to FM from the Italian Ministry of University and Research (MIUR, ex 60%).
Disclosure
The authors declare that they have no financial and/or non-financial competing interests.
References
1. Zhang P, Zou B, Liou YC, Huang C. The pathogenesis and diagnosis of sepsis post burn injury. Burns Trauma. 2021;9:tkaa047. doi:10.1093/burnst/tkaa047
2. Corcione S, Pensa A, Castiglione A, et al. Epidemiology, prevalence and risk factors for infections in burn patients: results from a regional burn centre’s analysis. J Chemother. 2021;33:62–66. doi:10.1080/1120009X.2020.1780776
3. Papathanakos G, Andrianopoulos I, Papathanasiou A, Priavali E, Koulenti D, Koulouras V. Colistin-resistant Acinetobacter baumannii bacteremia: a serious threat for critically ill patients. Microorganism. 2020;8:287. doi:10.3390/microorganisms8020287
4. Munier AL, Biard L, Legrand M, et al. Incidence, risk factors and outcome of multi-drug resistant Acinetobacter Baumannii nosocomial infections during an outbreak in a burn unit. Int J Infect Dis. 2019;79:179–184. doi:10.1016/j.ijid.2018.11.371
5. Corcione S, Baietto L, Malvasio V, et al. Pharmacokinetics of colistin methanesulfonate (CMS) in burn patients. J Antimicrob Chemother. 2017;72:319–321. doi:10.1093/jac/dkw361
6. Lima WG, Alves GCS, Sanches C, Fernandes SOA, de Paiva MC. Carbapenem-resistant Acinetobacter baumannii in patients with burn injury: a systematic review and meta-analysis. Burns. 2019;45:1495–1508. doi:10.1016/j.burns.2019.07.006
7. Albrecht MC, Griffith ME, Murray CK, et al. Impact of Acinetobacter infection on the mortality of burn patients. J Am Coll Surg. 2006;203:546–550. doi:10.1016/j.jamcollsurg.2006.06.013
8. Giacobbe DR, Saffioti C, Losito AR, et al. Use of colistin in adult patients: a cross-sectional study. J Glob Antimicrob Resist. 2020;20:43–49. doi:10.1016/j.jgar.2019.06.009
9. Butler DA, Biagi M, Tan X, Qasmieh S, Bulman ZP, Wenzler E. Multidrug resistant Acinetobacter baumannii: resistance by any other name would still be hard to treat. Curr Infect Dis Rep. 2019;21:46. doi:10.1007/s11908-019-0706-5
10. Garonzik SM, Li J, Thamlikitkul V, et al. Population pharmacokinetics of colistin methanesulfonate and formed colistin in critically ill patients from a multicenter study provide dosing suggestions for various categories of patients. Antimicrob Agents Chemother. 2011;55:3284–3294. doi:10.1128/AAC.01733-10
11. Gibson GA, Bauer SR, Neuner EA, Bass SN, Lam SW. Influence of colistin dose on global cure in patients with bacteriemia due to carbapenem-resistant gram-negative bacilli. Antimicrob Agents Chemother. 2015;60:431–436. doi:10.1128/AAC.01414-15
12. Wilkinson RE, Hill DM, Hickerson WL. Outcome analysis of colistin- treated burn center patients. Burns. 2017;43:1244–1249. doi:10.1016/j.burns.2017.03.006
13. Vauchel T, Pirracchio R, Chaussard M, et al. Impact of Acinetobacter baumannii outbreak on kidney events in a burn unit: a targeted machine learning analysis. Am J Infect Control. 2019;47:435–438. doi:10.1016/j.ajic.2018.09.010
14. Palmieri T, Lavrentieva A, Greenhalgh DG. Acute kidney injury in critically burn patients. Risk factors, progression and impact on mortality. Burns. 2010;36:205–211. doi:10.1016/j.burns.2009.08.012
15. Tsuji BT, Pogue JM, Zavascki A, et al. International consensus guidelines for the optimal use of the polymyxins: endorsed by the American College of Clinical Pharmacy (ACCP), European Society of Clinical Microbiology and Infectious Diseases (ESCMID), Infectious Diseases Society of America (IDSA), International Society for Anti-infective Pharmacology (ISAP), Society of Critical Care Medicine (SCCM), and Society of Infectious Diseases Pharmacists (SIDP). Pharmacotherapy. 2019;39:10–39. doi:10.1002/phar.2209
16. Tsuji BT, Pogue JM, Zavascki AP, et al. Polymyxin acute kidney injury: dosing and other strategies to reduce toxicity. Antibiotics. 2019;8(1):24. doi:10.3390/antibiotics8010024
17. Katip W, Uitrakul S, Oberdorfer P. Short-course versus long-course colistin for treatment of carbapenem-resistant A. baumannii in cancer patient. Antibiotics. 2021;10(5):484. doi:10.3390/antibiotics10050484
18. Katip W, Oberdorfer P. Clinical efficacy and nephrotoxicity of colistin alone versus colistin plus vancomycin in critically ill patients infected with carbapenem-resistant Acinetobacter baumannii: a propensity score-matched analysis. Pharmaceutics. 2021;13:162. doi:10.3390/pharmaceutics13020162
19. Ostermann M, Bellomo R, Burdmann EA, et al. Conference participants. Controversies in acute kidney injury: conclusions from a Kidney Disease: improving Global Outcomes (KDIGO) conference. Kidney Int. 2020;98:294–309. doi:10.1016/j.kint.2020.04.020
20. Fiaccadori E, Pistolesi V, Mariano F, et al. Regional citrate anticoagulation for renal replacement therapies in patients with acute kidney injury: a position statement of the Work Group “Renal Replacement Therapies in Critically Ill Patients” of the Italian Society of Nephrology. J Nephrol. 2015;28:151–164. doi:10.1007/s40620-014-0160-2
21. Mariano F, Leporati M, Carignano P, Stella M, Vincenti M, Biancone L. Efficient removal of colistin A and B in critically ill patients undergoing CVVHDF and sorbent technologies. J Nephrol. 2015;28:623–631. doi:10.1007/s40620-014-0143-3
22. Honore PM, Jacobs R, Lochy S, et al. Acute respiratory muscle weakness and apnea in a critically ill patient induced by colistin neurotoxicity: key potential role of hemoadsorption elimination during continuous venovenous hemofiltration. Int J Nephrol Renovasc Dis. 2013;6:107–111. doi:10.2147/IJNRD.S42791
23. Leporati M, Bua RO, Mariano F, et al. Determination by LC-MS/MS of colistins A and B in plasma and ultrafiltrate from critically ill patients undergoing continuous venovenous hemodiafiltration. Ther Drug Monit. 2014;36:182–191. doi:10.1097/FTD.0b013e3182a8997c
24. Mariano F, Hollo’ Z, Depetris N, et al. Coupled-plasma filtration and adsorption for severe burn patients with septic shock and acute kidney injury treated with renal replacement therapy. Burns. 2020;46:190–198. doi:10.1016/j.burns.2019.05.017
25. EUCAST. European Committee on Antimicrobial Susceptibility Testing breakpoint tables for interpretation of MICs and zone diameters. Version 7.1; 2017. Available from: http://www.eucast.org/clinical_breakpoints/.
26. Morris S, Cerceo E. Trends, epidemiology, and management of multi-drug resistant gram-negative bacterial infections in the hospitalized setting. Antibiotics. 2020;9:196. doi:10.3390/antibiotics9040196
27. Alp E, Coruh A, Gunay GK, Yontar Y, Doganay M. Risk factors for nosocomial infection and mortality in burn patients: 10 years of experience at a university hospital. J Burn Care Res. 2012;33:379–385. doi:10.1097/BCR.0b013e318234966c
28. Paramythiotou E, Routsi C. Association between infections caused by multidrug-resistant gram-negative bacteria and mortality in critically ill patients. World J Crit Care Med. 2016;5:111–120. doi:10.5492/wjccm.v5.i2.111
29. Strassle PD, Williams FN, Napravnik S, et al. Improved survival of patients with extensive burns: trends in patients characteristics and mortality among burn patients in a tertiary care burn facility, 2004–2013. J Burn Care Res. 2017;38:187–193. doi:10.1097/BCR.0000000000000456
30. Mariano F, De Biase C, Hollo Z, et al. Long-term preservation of renal function in septic shock burn patients requiring renal replacement therapy for acute kidney injury. J Clin Med. 2021;10(24):5760. doi:10.3390/jcm10245760
31. Christofides C, Moore R, Nel M. Baux score as a predictor of mortality at the CHBAH adult burns unit. J Surg Res. 2020;251:53–62. doi:10.1016/j.jss.2020.01.018
32. Goei H, van Baar ME, Dokter J, et al. Burns in the elderly: a nationwide study on management and clinical outcomes. Burns Trauma. 2020;8:tkaa027. doi:10.1093/burnst/tkaa027
33. Wagenlehner F, Lucenteforte E, Pea F, et al. Systematic review on estimated rates of nephrotoxicity and neurotoxicity in patients treated with polymyxins. Clin Microbiol Infect. 2021;27:671–676.
34. Ordooei Javan A, Shokouhi S, Sahraei Z. A review on colistin nephrotoxicity. Eur J Clin Pharmacol. 2015;71:801–810. doi:10.1007/s00228-015-1865-4
35. Dokter J, Meijs J, Oen IM, van Baar ME, van der Vlies CH, Boxma H. External validation of the revised Baux score for the prediction of mortality in patients with acute burn injury. J Trauma Acute Care Surg. 2014;76:840–845. doi:10.1097/TA.0000000000000124
36. Gunay E, Kaya S, Baysal B, Yuksel E, Arac E. Evaluation of prognosis and nephrotoxicity in patients treated with colistin in intensive care unit. Ren Fail. 2020;42:704–709. doi:10.1080/0886022X.2020.1795878
37. Ganapathy H, Pal SK, Teare L, Dziewulski P. Use of colistin in treating multi-resistant Gram-negative organism in a specialised burns unit. Burns. 2010;36:522–527. doi:10.1016/j.burns.2009.07.010
38. Joannidis M, Druml V, Forni LG, et al. Prevention of acute kidney injury and protection of renal function in the intensive care unit: update 2017: expert opinion of the Working Group on Prevention, AKI section, European Society of Intensive Care Medicine. Intensive Care Med. 2017;43:730–749. doi:10.1007/s00134-017-4832-y
39. Wu G, Xiao Y, Wang C, et al. Risk factors for acute kidney injury in patients with burn injury: a meta-analysis and systematic review. J Burn Care Res. 2017;38:271–282. doi:10.1097/BCR.0000000000000438
40. Lee YJ, Wi YM, Kwon YJ, Kim SR, Chang SH, Cho S. Association between colistin dose and development of nephrotoxicity. Crit Care Med. 2015;43:1187–1193. doi:10.1097/CCM.0000000000000931
41. Miano TA, Lautenbach E, Wilson FP, Guo W, Borovskiy Y, Hennessy S. Attributable risk and time course of colistin-associated acute kidney injury. Clin J Am Soc Nephrol. 2018;13:542–550. doi:10.2215/CJN.06980717
42. Chien HT, Lin YC, Sheu CC, Hsieh KP, Chang JS. Is colistin-associated acute kidney injury clinically important in adults? A systematic review and meta-analysis. Int J Antimicrob Agents. 2020;55:105889. doi:10.1016/j.ijantimicag.2020.105889
43. Tsai SY, Lio CF, Shih SC, et al. The predisposing factors of AKI for prophylactic strategies in burn care. Peer J. 2020;8:e9984. doi:10.7717/peerj.9984
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

