Back to Journals » Neuropsychiatric Disease and Treatment » Volume 15
Cognitive impairment in eating disorder patients of short and long-term duration: a case–control study
Authors Grau A , Magallón-Neri E, Faus G, Feixas G
Received 30 December 2018
Accepted for publication 11 March 2019
Published 21 May 2019 Volume 2019:15 Pages 1329—1341
DOI https://doi.org/10.2147/NDT.S199927
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Antoni Grau,1,2 Ernesto Magallón-Neri,3,4 Gustavo Faus,1,2 Guillem Feixas3,4
1ITA Mental Health Specialist, Madrid, Spain; 2ITA Foundation, Barcelona, Spain; 3Department of Clinical Psychology and Psychobiology, Faculty of Psychology, University of Barcelona, Barcelona, Spain; 4Institute of Neurosciences, University of Barcelona, Barcelona, Spain
Introduction: Several studies have noted the potentially negative effect of eating disorders (ED) on cognitive performance.
Objective: To compare the impact of the duration of abnormal eating behaviors on cognitive performance in a sample of people with short- and long-term eating disorders and in two control groups matched for age.
Method: The neuropsychological performance of 82 women diagnosed with an eating disorder were compared with two control groups from the community of 66 healthy women. Time of duration of the disorder was less than two years in half of the clinical sample, and more than 10 years in the other half. The following instruments were used to measure neuropsychological performance: the Matrix Test, the Stroop task, the Trail-Making Test, the Tower of London Test, the Posner Spatial Task, the Rey’s Complex Figure, the Wechsler Vocabulary Test, and the Hayling Completion Test.
Results: It showed that persons with long-term ED presented more impaired neuropsychological profiles, but not in all areas. In contrast, the short-term ED group presented similar profiles to the control groups.
Discussion: This study highlights the positive association between cognitive impairment and time of evolution of ED, above all in perceptual measures and non-verbal memory. Considering the effect of the evolution of ED cognitive performance (especially in long-term patients) may further our understanding of the development of the disorder and the factors that may favor its persistence.
Keywords: eating disorder, cognitive impairment, long-duration ED
Introduction
Eating disorders (ED) may be associated with a series of physical, social, relational, family, and psychological problems.1 Patients with long-term evolution of ED present a degree of dysfunction comparable to that of serious mental disorders such as schizophrenia and/or chronic affective disorders.2 Increased mortality,3 social isolation, and lack of employment are some of the main problems affecting this persistent ED subgroup.4 Recently, a number of studies on neuropsychological functioning in these disorders have stressed the importance of etiological factors in explaining certain peculiarities in the cognitive style recorded at ED onset.5,6 In people with ED, cognitive rigidity and obsessiveness have been related to prototypical compulsive behaviors such as calorie counting, hyperactivity, body checking, and ritualistic eating behavior.7 The presence of impulsiveness, especially in persons with bulimia nervosa (BN) and binge eating, has been associated with the feeling of urgency that precedes episodes of overeating.8 Others have reported the presence of cognitive impairment in certain functions.9
The specificity of cognitive impairment associated with each type of ED and the effects associated with its evolution are issues that have been widely debated, but no consensus has been reached.9 (p102) This is partly because the empirical evidence in the study of cognitive styles in ED is limited in comparison with other psychiatric disorders such as depression or schizophrenia,10 and also because most studies diverge substantially in terms of their recruitment methodology, their diagnostic criteria, and the psychometric instruments used. Taken together, these factors may constitute a real problem in the study of specific functions such as cognitive flexibility and cognitive inhibition. Patients show a strong tendency to migrate among the eating disorder categories.11 This observation gave rise to the Transdiagnostic Model, which forms the basis for the cognitive-behavioral treatment of ED.12 This model proposes that there are a series of characteristics common to all types of behavioral disorders which explain this frequent transition between diagnoses; for example, persons with AN or BN and binge eaters share an over-evaluation of the figure and weight and exercise strict food control. The presence of these common factors has meant that the samples recruited for studies have tended to include eating disorders of all types. Many studies only assess one type of ED (mainly anorexia nervosa),13–15 and the few studies that have included different types of ED have been carried out with small samples; therefore, their level of representativeness is low and no sound conclusions can be drawn.16 All this means that this field of research is still very much in development. Furthermore, the presence of comorbidities such as anxiety, depression, addictions, obsessive-compulsive disorder,17 or personality disorders,18 may strongly mediate the course of psychopathology and may affect the results of assessments of overall cognitive performance.5(p82),9(p102)
Among the possible causes of neuropsychological impairments in ED are the symptoms of ED themselves (malnutrition, emetic behaviors, etc.), cognitive style (described as an endophenotype), and the effect of chronicity.19 In the same way, some neurological processes such as the cognitive deficits in attention, executive functions, and mentalizing found in some studies may constitute vulnerability factors. Gillberg et al20 concluded that these factors were independent of body mass index (BMI), ED diagnosis (Anorexia Nervosa [AN], Bulimia Nervosa [BN], or Eating Disorders Not Otherwise Specified [EDNOS]) at the time of evaluation, and of the chronicity of the disorder, because the neuropsychological impairment persisted despite ED remission.
In this study of specific neuropsychological functions, we will focus on intelligence quotient (IQ), executive functioning (attention, fluency and verbal inhibition, planning, cognitive flexibility), central coherence and visual-perceptive skills (visual memory), according to the domains proposed by the “Ravello Profile” battery.21 This battery was designed to be the Gold standard instrument in ED neuropsychological evaluation and it has been used in numerous publications.22–24
The use of IQ in the assessment of people with ED is controversial. Despite the heterogeneity both in the samples studied and the results obtained, the most recent systematic review25 places the IQ of patients with AN at between 5.9 and 10.8 points above the general population. Paradoxically, a recent study suggested that an above average IQ increases the risk of developing an AN.26 IQ scores do not differ substantially between BN and AN patients.26(p484)
Within executive functions, attention problems may be the most important in persons with ED.27–29 These individuals are known to develop selective attention with a degree of hypervigilance about caloric nutrition and also to stimuli related to the body and shape.
Cognitive flexibility is another of the neuropsychological characteristics that may be affected in EDs. In the study by Tchanturia et al14(p549) of biases in set shifting, patients showed low tolerance to the changes that remain after recovery from the disorder. This feature was even found in healthy first-degree relatives of patients with ED (even post recovery) who may present an eating disorder endophenotype.5,30(p848) In BN it is also present, though associated more with problems of response inhibition. Due to the difficulty of transition from one state to another (set shifting), responses associated with high damage avoidance, inflexibility of thought expressed by rigidity in behavioral habits related to food and high perfectionism were found.5(818) Moreover, the weak central coherence found in ED patients is a cognitive style biased toward a local or analytical, detail-focused processing of information that is unable to integrate incoming information.31
These two characteristics (inflexibility and low central coherence), together with the presence of important interpersonal deficits support the hypothesis that the functioning of some AN patients may be similar to that of patients diagnosed with Autism Spectrum Disorder.32,33
ED groups frequently present biases toward the memory of words related to the body or body shape.34 Independently of these biases, some authors have found deficits in visual memory both in short and long term.35
Using a series of neuropsychological assessment instruments, this study aims to evaluate cognitive function of people with EDs of short and long duration with the specific aim of evaluating their level impairment. By comparing them to two healthy age-matched control groups we want to test our hypothesis that cognitive disturbances are present in patients with ED. We also expect to find higher levels of cognitive impairment in those in the long-term condition (as compared to both those in the ED short-term condition and the control groups).
Method
Participants
Two clinical groups of patients with ED (100% women) were recruited at the Eating Disorders Institute of Barcelona. This Center offers one of the nation’s leading programs for the treatment of eating disorders and provides health service for children, adolescents and adults of all the autonomous communities of Spain. The Center offers highly-specialized individual, group, family, art, and nutritional therapies, and, embracing a comprehensive continuum of care, it supports individuals and families at every stage of treatment and recovery. During the time the study lasted, a total of 223 patients were admitted.
The first clinical group consisted of patients with short-term ED (ST-ED; n=41) defined as a period of less than two years of evolution of any ED. The chronic or long-term duration subgroup (LT-ED; n=41) had a history of over 10 years of any ED. None of the participants included was taking medications that could have cognitive side effects (eg, antipsychotics or stimulants).
The clinical groups were compared with two control groups from the community (100% female) divided according to age. The junior control (JC) group was used in order to make comparisons with the clinical short-term group, and the senior control (SC) group was compared with the chronic group. Both control groups comprised 33 participants.
We used non-probability sampling, with consecutive enrollment, including in all the study all eligible cases who agreed to participate. All patients met DSM-IV criteria for ED36 when admitted. At the moment of the assessment, the patients were in the third month of the treatment, considering the average period of inpatient treatment is six months. All patients had a BMI equal to or greater than 18.5 (M: 20.8, SD: 5.4)
Exclusion criteria were a history of neurological or severe illness that might interfere with the diagnosis or evidence of an acute state of psychosis or addictive disorders or moderate-to-severe difficulties in learning. The healthy control groups had no history of psychiatric or neurological disorders, nor any eating behavior problems. Informed written consent was obtained from all participants throughout the procedure in accordance with ethical principles. The study was approved by the bioethics committee of the University of Barcelona (IRB number: IRB00003099). Information obtained by the study is protected under the legal frame of data protection valued by the institution and by the Declaration of Helsinki. In order to protect the identity of each participant, only alphanumeric identifications were recorded in database. All participants were informed that their participation was voluntary and that they were free to abandon the study at any time. No economic compensation was given.
Instruments
Clinical assessment
The Structured Clinical Interview for DSM-IV Mental Disorders (SCID-I)37 was administered to assess the presence of ED and other related Axis I psychiatric disorders. Absence of ED in control groups was assessed by the SCOFF screening instrument.38
Neuropsychological assessment
For the cognitive assessment of eating disorders, a neuropsychological battery comprising eight tests was used, partially based on the computer protocol “Psychology Experiment Building Language” (PEBL)39 software. The PEBL neuropsychological tests have shown good psychometric properties, reliability and validity.40 The PEBL tests used were Matrix Rotation, Stroop, Trail Making Test, Tower of London and Posner Spatial cueing task, applied to both clinical (LT-ED and ST-ED) and control groups (SC, JC). The cut-off point for cognitive impairment on PEBL assessment was set at one standard deviation below (Percentile 16) or above (Percentile 84) the mean performance of the senior and junior control groups, depending on the specific test.41 Moreover, the Rey complex figure test (copy, immediate, and delayed recall), the Wechsler vocabulary test, and Brixton-Hayling tests have also shown moderate-to-good psychometric properties, reliability and validity. They were applied only to clinical groups, and their cut-off points for identifying cognitive impairment were extracted from normative data.
PEBL Matrix Rotation
This subtest comprises twenty point matrixes. In half of them, alongside the original figure, the same pattern appears rotated 90 degrees to the left. The other matrixes present different matrixes for comparison, and the participant must decide whether it is the same element or is different. The answers are scored as right or wrong, and the reaction time is recorded.
PEBL Stroop test
In summary, the Stroop task is a cognitive test of attention and concentration which evaluates both cognitive inhibition and flexibility. There are two conditions: condition 1 (Name cost), consistent: ink color and word name coincide; condition 2 (Color cost): inconsistent: ink color and word name do not coincide. The Stroop effect is obtained by subtracting the reaction time of condition 1 from that of condition 2.
PEBL Trail-Making-Test (TMT)
This subtest comprises four types of nonverbal reasoning tasks: pattern completion, classification, analogy, and serial reasoning. The TMT is typically thought to measure visual attention, mental flexibility, and executive functioning. It involves connecting dots arranged in a numbered sequence in ascending order (Part A) or numbers and letters that alternate (Part B). Traditionally, performance on the TMT has been timed with a stop-watch and the experimenter redirects the participant when they make an error. The respondent looks at a matrix from which a section is missing and completes it either by saying the number or by pointing to one of five response options.
PEBL Tower of London test (ToL)
The ToL Test assesses spatial planning, rule learning, inhibition of impulsive and perseverative responding, and the ability to establish and maintain the instructional set. This test requires planning and judgment in order to arrive at the most efficient solution by moving colored beads from their initial position to a new set of predetermined or goal positions.42
PEBL Posner Spatial Task
The Posner task is a classical experimental paradigm which measures visual attention. Several versions of this paradigm are currently available in the field of experimental psychology, modified according to the phenomenon or psychiatric disorder to be studied.43 Inside the study of EDs, stimuli are typically transformed into words related to eating and the figure.44 We applied this test in order to measure differences in visual attention between the study groups, independently of the bias caused by the semantic contents of stimuli associated with eating and the figure.
Rey Complex Figure Test (RCFT)
The RCFT assesses visual-spatial processing and recall by measuring visuoperceptual organization and visual memory. The figure is a geometric shape consisting of global features (ie, a large rectangle) and local features (ie, geometric details inside and outside the large rectangle). In the first trial (copy), participants must copy the figure. Immediately afterwards, they must reproduce it from memory without the possibility of visualizing the model (immediate recall). After 30 mins, they reproduce the figure again from memory (delayed recall). In this study, this test was used as a test of visual memory. The cut-off used to consider cognitive impairment was 18 points (Percentile 30) on both immediate and delayed recall.45
Wechsler vocabulary test
This subtest is composed of 66 words of increasing difficulty, presented orally and visually. The scores (0–2) reflect the sophistication of the definition. Measures of verbal knowledge and concept formation were used. The cut-off point for cognitive impairment was set at 20% of the raw scores obtained to allow for the natural decline due to age.
Hayling Sentence Completion test
The Hayling Sentence Completion Task measures verbal inhibition. The first part, which assesses initiation speed, requires the completion of sentences with a congruent verbal response. The second part, which assesses verbal inhibition, requires the completion of sentences with an incongruent verbal response. The cut-off point for cognitive impairment was set at one standard deviation below the mean performance of the control group, as suggested in Abusamra, Miranda, and Ferreres.46
Procedure
The sample was recruited between September 2013 and May 2014. To recruit the clinical group, a group of patients at our institution who were receiving interdisciplinary treatment for ED was invited to participate on a voluntary basis. Both short and long evolution groups completed self-administered questionnaires and neuropsychological tests. The administration of all the tests began exactly at 10:30 h, 1.5 hrs after their last intake in order to control for the effect of hunger-satiation. The junior control group was recruited from two secondary schools in Barcelona. To acknowledge the schools’ willingness to participate, our institute held two workshops for their students on the subject of ED prevention. The senior control group was recruited via newspaper advertisements or by word of mouth among acquaintances of the patient group or workers at the psychological care center. Their sociodemographic profiles were similar to those of their contrast group. These persons also participated on a voluntary basis.
Nevertheless, in order to avoid overload, only some of the neuropsychological tests were applied. Some of the tests were lost during the application process due to unforeseen causes such as participants’ tiredness, refusal to continue because of frustration with certain tasks or interruptions that invalidated the test such as the need to go to the bathroom. In addition, some controls were unable to finish certain cognitive tasks on the day of the application. Nevertheless, differences between the subjects included in the analyses and those that were not did not show any significant difference in their sociodemographic or clinical features.
Data analysis
Raw scores were transformed to z-scores with SPSS. Of the moderate and extreme outliers identified; only the ones with a firm extreme category in each test variable were removed. The Student independent samples t-test was used to calculate the differences between two groups, the chi-squared and Fisher’s exact tests for contrast of absolute frequencies, and contrast of proportion was applied to identify differences in relative frequencies (percentages) between groups. MANOVA multivariate analysis was not applied because the results of the M Box’s matrix covariance were significant. Therefore, we applied a first analysis with ANCOVA taking into account age and level of education as covariates. We then performed an ANOVA with Scheffé’s post-hoc in order to assess differences in neuropsychological profile between three or more groups. We also used the more conservative Brown–Forsythe or Welch statistic. Finally, effect size was calculated with Cohen’s d or ϕ for contingency table analysis.
Results
The total sample comprised 148 participants (100% women) divided into four groups, two clinical (long and short ED duration) and two control groups (senior and junior). Table 1 shows their sociodemographic features; there were no significant differences between clinical groups and their respective control groups in terms of age, years of evolution, or education, except that more subjects in the short-term ED group had not progressed beyond secondary studies than in the other groups.
 | Table 1 Sociodemographic features in clinical and control groups |
Eating disorder status
BMI was 20.2 (SD=1.60) in the LT-ED group and 20.4 (SD=1.8) in the ST-ED group (Table 2). As regards years of clinical evolution of the ED, the long-term ED group had a mean of 14.8 years and the short-term ED group little more than one year of evolution. Moreover, Table 2 shows the distribution of ED diagnoses according to clinical group; there were no significant differences in the different ED diagnoses between the groups.
 | Table 2 Clinical features and diagnoses in clinical sample |
Clinical diagnoses (Axis: I and II) and pattern of substance use in the clinical samples
Table 2 also shows that 47% of the subjects in both clinical groups presented psychiatric comorbidity. Most (45%) presented only one disorder in addition to ED, and only 2% had more than two comorbid psychiatric diagnoses. In the long duration ED group, 54% presented comorbid disorders, and in the short duration ED group 39%. In the short duration ED group, Axis II comorbidity appeared only in Cluster B (12%). In the long duration ED group, 58% presented Axis II comorbidity (34% Cluster B, 22% Cluster C and 2% with not otherwise specified personality disorder). As regards substance abuse no significant differences were found between clinical groups.
Table 3 presents the descriptive results of performance in cognitive tests in each of the control and clinical groups. Regarding people rate that answered neuropsychological tests. In the group of 148 subjects, 89.8% answered the Matrix rotation test, 85.8% Stroop, ToL and Posner, 87.8% TMT, 69.5% Rey Complex Figure, 79% Wechsler Vocabulary, and 75.6% Hayling.
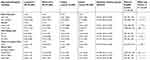 | Table 3 Means and standard deviations in each neuropsychological variable by group |
 |
No significant differences were found between the two clinical groups in the matrix rotation reasoning test, of the Stroop name test, the Trail Making Test, Posner mean neutral and invalid scores, or the Wechsler vocabulary test. However, significant differences in both clinical groups were found on the Stroop color test, Posner mean invalid score, and on the copy, memory and delayed recall scores and total score on the Rey Figure, and on the Hayling test.
The LT-ED and senior control groups presented significant differences in the number of matrix rotation and Stroop name tests, part B of TMT, and ToL total score. In contrast, no significant differences were found in any neuropsychological variables between ST-ED and junior control groups.
The number of subjects considered to have cognitive impairment is shown in Table 4. The group with the most subjects classified as cognitively impaired was the long-term duration ED clinical group.
 | Table 4 Absolute frequencies of persons and relative percentages with cognitive impairment by group |
Nevertheless, significant differences with medium effect sizes were found on the matrix rotation test, Stroop test, TMT, ToL, Posner Neutral test, and on total scores of memory, and delayed recall on the Rey Figure test between the two clinical groups. The Hayling and Wechsler vocabulary tests did not present significant differences.
Discussion
In this study, cognitive impairment was more frequent in patients with long-term eating disorders, above all with regard to perceptual measures and non-verbal memory. The absence of differences on the Wechsler vocabulary test indicates a similar premorbid level of intelligence in the two groups of ED patients. This suggests that the differences found in the percentage of cognitively impaired patients may be related to the years of duration of the disorder and that our two patient groups started with a similar cognitive reserve.47
These differences are also emphasized in the contrast with the control groups without ED. Even though the clinical groups shared similar features except for age and illness evolution (a feature deliberately differentiated within the study design), comorbidity with personality disorders, especially cluster B, was clearly more frequent in the long-term ED clinical group. This variable may be of special importance for a more detailed assessment of the personality disturbances that are regularly associated with poor prognosis.18(p177) We aim to examine this issue in an upcoming project.
Regarding the contrasts between groups (LT vs SC and ST vs JC), significant differences were found only between the LT-ED and senior control groups in verbal reasoning and non-verbal, serial, spatial planning, cognitive flexibility, new rule learning, cognitive inhibition, and answer perseverance. These differences were less clear in the comparison of the ST-ED group and their corresponding controls. These results suggest that the evolution and maintenance of the disorder over time may play an important role in the development of cognitive impairment.
To our knowledge, these features have not been reported in previous studies, which have found systematically greater disturbances in ED patients than in controls.6(p417),9(p100)
Our findings underline the importance of considering the effect of the duration of a disorder on its evolution. Some studies advocate identifying cognitive alterations in persons with ED that may constitute an endophenotype.30(p473) One of the prerequisites for considering a characteristic as an endophenotype is that it must be state-independent.48 These authors found low cognitive flexibility even in recovered patients, suggesting that this is a stable trait which is independent of the state of the disease. However, the lack of differences between our short evolution clinical group and our healthy control group violates the criterion of state-independence and seems to rule out low cognitive flexibility as a possible endophenotype of eating disorders.
The poorer performance presented by the long-term evolution clinical group on characteristics of eating disorders may suggest a direct extrapolation towards some prototypical behaviors in eating disorders. Some authors have associated low cognitive flexibility with a rigid and stereotyped eating style based on idiosyncratic rules and less likely to be modified by therapy.49
Furthermore, this cognitive inflexibility is considered one of the factors that worsens prognosis.50 This is hardly surprising, as cognitive rigidity is a variable that is at odds with the notion of change and is likely to present resistance to therapy.
Regarding the visual-perceptive difficulties found in long-term evolution ED group, it is well known that these alterations are involved in the body image distortion typical of these disorders.51 Specifically, Smeets, and Kosslyn52 showed that this distortion cannot be explained at the level of perception but should be attributed to alterations in visual memory. Indeed, the results of this present study show poorer performance in visual memory in the long-term clinical group.
Some of the differences found in body image alterations indicate that these long-term ED patients process and organize information less efficiently than their counterparts with shorter duration. This deficit in processing complex visual information may contribute to explaining the presence of body image alterations frequently reported in the literature.
These results should be interpreted with caution, due to the possible effect of comorbidity on neuropsychological performance. However, the only comorbid conditions in which significant differences were observed between the two clinical groups were personality disorders. In this regard, a recent meta-analysis has shown the diagnosis of personality disorder to be closely associated with significant cognitive deterioration.53 In the same study, samples of patients with borderline personality disorder and any co-occurring eating disorder performed worse on executive function tasks. Other variables such as the severity of eating symptoms should also be taken into account when interpreting the results of our study.
One of the limitations of our study is the fact that the sample was recruited from a single private health care institution. However, we sought to match the proportions between groups according to their sociodemographic characteristics. Another limitation is the application of some tests only in the clinical groups and not in the control groups, such as the vocabulary test, the Rey Figure test and Hayling test. This limits the range when comparing different cognitive indexes in controls and patients with some degree of ED. Nevertheless, we were able to compare clinical groups with regard to most of the variables presented in this study.
In this study, we did not aim to link specific ED symptoms with the presence of cognitive deficits. Over ten years of ED, the symptoms are likely to vary, with some disappearing and others emerging. We believe that variables such as malnutrition, the presence of purging maneuvers or substance abuse may explain some of these dysfunctions. New studies should aim to isolate these factors. Moreover, the impact of comorbidities such as anxiety, depression or substance use disorders,17(p297) and especially personality disorders18(p176) in the LT-ED group should be considered in further studies.
Another limitation of the study is the use of the DSM-IV diagnostic system. At the time of the study, the Spanish version of the DSM-5 was not available. Future studies based on the DSM-5 are likely to reduce the number of unspecified eating disorders and should thus increase the predictive value of the diagnosis.
Although the groups were relatively small, one of the strengths of the study is that they were homogeneous in terms of their sociodemographic characteristics. Moreover, this study specifically compared two clinical groups of ED patients, basing the assessment on the evolution of the disorder rather than on the specific ED subtype. Further studies focusing on the ED subtypes defined by DSM-5 and monitoring the long-term evolution of patients across categories would extend our knowledge about cognitive impairment in EDs.
Another feature of this study worth highlighting is the use of the PEBL platform in Spanish-speaking patients, as well as the development and translation of specific scripts that have not been previously used to measure neurocognitive performance in Spanish speakers.
Finally, we should bear in mind the possible reversibility of some of the deficits observed. Promising developments such as cognitive remediation therapy may prove effective in reversing these difficulties.54 Interventions in this area should prioritize long duration ED. Because of the difficulties found in visual processing information and its possible transfer to the perception of one’s own body, new therapies based on the use of virtual reality may represent a promising alternative. Some authors55 have already put forward proposals these individuals which may have an important bearing on the success of the rehabilitation of key areas in patients’ autonomy such as their occupation or their social life.
Conclusions
The assessment of the effect of ED evolution (especially in long-term patients) and its associated cognitive aspects may shed light on both the development and the maintenance of the disorder. These cognitive effects should be borne in mind in the attempts to design effective treatments for ED, personalizing the therapy by adjusting the objectives and timing related to the patient’s cognitive functioning.
Acknowledgments
This study was supported in part by different grants: to the first author from ITA Foundation, and a postdoctoral research fellowship to the second author from the University of Barcelona.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Treasure J, Zipfel S, Micali N, et al. Anorexia nervosa. Nat Rev Dis Prim. 2015;1:15074. doi:10.1038/nrdp.2015.74
2. Arkell J, Robinson P. A pilot case series using qualitative and quantitative methods: biological, psychological and social outcome in severe and enduring eating disorder (anorexia nervosa). Int J Eat Disord. 2008;41(7):650–656. doi:10.1002/eat.20546
3. Franko DL, Keshaviah A, Eddy KT, et al. longitudinal investigation of mortality in anorexia nervosa and bulimia nervosa. Am J Psychiatry. 2013;170(8):917–925. doi:10.1176/appi.ajp.2013.12070868
4. Robinson PH. Community Treatment of Eating Disorders. London: Willey-Blackwell; 2006:204.
5. Kanakam N, Treasure J. A review of cognitive neuropsychiatry in the taxonomy of eating disorders: state, trait, or genetic? Cogn Neuropsychiatry. 2013;18(1–2):83–114. doi:10.1080/13546805.2012.682362
6. Jáuregui-Lobera I. Neuropsychology of eating disorders: 1995-2012. Neuropsychiatr Dis Treat. 2013;9:415–430. doi:10.2147/NDT.S42714
7. Altman SE, Shankman SA. What is the association between obsessive-compulsive disorder and eating disorders? Clin Psychol Rev. 2009;29(7):638–646. doi:10.1016/j.cpr.2009.08.001
8. Gay P, Rochat L, Billieux J, d’Acremont M, Van der Linden M. Heterogeneous inhibition processes involved in different facets of self-reported impulsivity: evidence from a community sample. Acta Psychol (Amst). 2008;129(3):332–339. doi:10.1016/j.actpsy.2008.08.010
9. Zakzanis KK, Campbell Z, Polsinelli A. Quantitative evidence for distinct cognitive impairment in anorexia nervosa and bulimia nervosa. J Neuropsychol. 2010;4(1):89–106. doi:10.1348/174866409X459674
10. Bora E, Yücel M, Pantelis C. Cognitive impairment in schizophrenia and affective psychoses: implications for DSM-V criteria and beyond. Schizophr Bull. 2009;36(1):36–42. doi:10.1093/schbul/sbp094
11. Grave RD. Eating Disorders: progress and Challenges. Eur J Intern Med. 2011;22(2):153–160. doi:10.1016/j.ejim.2010.12.010
12. Fairburn C. Cognitive Behaviour Therapy and Eating Disorders. New York, NY: Guilford Press; 2008:324 p.
13. Gillberg IC, Råstam M, Wentz E, Gillberg C. Cognitive and executive functions in anorexia nervosa ten years after onset of eating disorder. J Clin Exp Neuropsychol. 2007;29(2):170–178. doi:10.1080/13803390600584632
14. Tchanturia K, Morris RG, Anderluh MB, Collier DA, Nikolaou V, Treasure J. Set shifting in anorexia nervosa: an examination before and after weight gain, in full recovery and relationship to childhood and adult OCPD traits. J Psychiatr Res. 2004;38(5):545–552. doi:10.1016/j.jpsychires.2004.03.001
15. Tenconi E, Santonastaso P, Degortes D, et al. Set-shifting abilities, central coherence, and handedness in anorexia nervosa patients, their unaffected siblings and healthy controls: exploring putative endophenotypes. World J Biol Psychiatry. 2010;11(6):813–823. doi:10.3109/15622975.2010.483250
16. Guillaume S, Sang CNT, Jaussent I, et al. Is decision making really impaired in eating disorders? Neuropsychology. 2010;24(6):808–812. doi:10.1037/a0019806
17. Ulfvebrand S, Birgegard A, Norring C, Hogdahl L, von Hausswolff-Juhlin Y. Psychiatric comorbidity in women and men with eating disorders results from a large clinical database. Psychiatry Res. 2015;230(2):294–299. doi:10.1016/j.psychres.2015.09.008
18. Magallón-Neri E, González E, Canalda G, et al. Prevalence and severity of categorical and dimensional personality disorders in adolescents with eating disorders. Eur Eat Disord Rev. 2014;22(3):176–184. doi:10.1002/erv.2268
19. Tchanturia K, Campbell IC, Morris R, Treasure J. Neuropsychological studies in anorexia nervosa. Int J Eat Disord. 2005;37(Suppl:S72–6):discussion S87–S89. doi:10.1002/eat.20119
20. Gillberg IC, Billstedt E, Wentz E, Anckarsater H, Rastam M, Gillberg C. Attention, executive functions, and mentalizing in anorexia nervosa eighteen years after onset of eating disorder. J Clin Exp Neuropsychol. 2010;32(4):358–365. doi:10.1080/13803390903066857
21. Rose M, Davis J, Frampton I, Lask B. The Ravello profile: development of a global standard neuropsychological assessment for young people with anorexia nervosa. Clin Child Psychol Psychiatry. 2011;16(2):195–202. doi:10.1177/1359104511401191
22. Dahlgren CL, Lask B, Landrø NI, Rø Ø. Neuropsychological functioning in adolescents with anorexia nervosa before and after cognitive remediation therapy: a feasibility trial. Int J Eat Disord. 2013;46(6):576–581. doi:10.1002/eat.22155
23. Stedal K, Rose M, Frampton I, Landrø NI, Lask B. The neuropsychological profile of children, adolescents, and young adults with anorexia nervosa. Arch Clin Neuropsychol. 2012;27(3):329–337. doi:10.1093/arclin/acs032
24. Van Noort BM, Pfeiffer E, Lehmkuhl U, Kappel V. Eine internationale neuropsychologische testbatterie für kinder, jugendliche und erwachsene mit anorexia nervosa—die deutsche adaptation des ravello profils. [An international neuropsychological assessment tool for children, adolescents, and adults with anorexia nervosa—the German adaptation of the Ravello profile.]. Z Kinder Jugendpsychiatr Psychother. 2013;41(6):371–381. doi:10.1024/1422-4917/a000253
25. Lopez C, Stahl D, Tchanturia K. Estimated intelligence quotient in anorexia nervosa: a systematic review and meta-analysis of the literature. Ann Gen Psychiatry. 2010;9(40):1–10. doi:10.1186/1744-859X-9-40
26. Schilder CMT, van Elburg AA, Snellen WM, Sternheim LC, Hoek HW, Danner UN. Intellectual functioning of adolescent and adult patients with eating disorders. Int J Eat Disord. 2017;50(5):481–489. doi:10.1002/eat.22594
27. Tchanturia K, Davies H, Roberts M, et al. Poor cognitive flexibility in eating disorders: examining the evidence using the Wisconsin Card Sorting Task. PLoS One. 2012;7(1):e28331. doi:10.1371/journal.pone.0028331
28. Pretorius N, Dimmer M, Power E, Eisler I, Simic M, Tchanturia K. Evaluation of a cognitive remediation therapy group for adolescents with anorexia nervosa: pilot study. Eur Eat Disord Rev. 2012;20(4):321–325. doi:10.1002/erv.2176
29. Alvarado N, Silva C, Clave P, et al. Revista Latinoamericana de Psicología Funciones ejecutivas y sintomatología asociada con los trastornos de la conducta alimentaria. Rev Latinoam Psicol. 2014;46(3):189–197. doi:10.1016/S0120-0534(14)70022-6
30. Kanakam N, Raoult C, Collier D, Treasure J. Set shifting and central coherence as neurocognitive endophenotypes in eating disorders: a preliminary investigation in twins. World J Biol Psychiatry. 2013;14(6):464–475. doi:10.3109/15622975.2012.665478
31. Lopez C, Tchanturia K, Stahl D, Treasure J. Weak central coherence in eating disorders: a step towards looking for an endophenotype of eating disorders. J Clin Exp Neuropsychol. 2009;31(1):117–125. doi:10.1080/13803390802036092
32. Oldershaw A, Hambrook D, Stahl D, Tchanturia K, Treasure J, Schmidt U. Neuroscience and biobehavioral reviews the socio-emotional processing stream in Anorexia Nervosa. Neurosci Biobehav Rev. 2011;35(3):970–988. doi:10.1016/j.neubiorev.2010.11.001
33. Westwood H, Mandy W, Tchanturia K. The association between symptoms of autism and neuropsychological performance in females with Anorexia Nervosa. Psychiatry Res. 2017;258:531–537. doi:10.1016/j.psychres.2017.09.005
34. Aspen V, Darcy AM, Lock J. A review of attention biases in women with eating disorders. Cogn Emot. 2013;27(5):820–838. doi:10.1080/02699931.2012.749777
35. Weider S, Indredavik MS, Lydersen S, Hestad K. Neuropsychological function in patients with anorexia nervosa or bulimia nervosa. Int J Eat Disord. 2015;48(4):397–405. doi:10.1002/eat.22283
36.
37. First M, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. User’s Guide for the Structured Clinical Interview for the DSM-IV Axis II Personality Disorders. Washington, DC: American Psychiatric Press; 1997.
38. Morgan JF, Reid F, Lacey JH. The SCOFF questionnaire: assessment of a new screening tool for eating disorders. BMJ. 1999;319(7223):1467–1468.
39. Mueller ST, Piper BJ. The Psychology Experiment Building Language (PEBL) and PEBL test battery. J Neurosci Methods. 2014;222:250–259. doi:10.1016/j.jneumeth.2013.10.024
40. Piper BJ, Mueller ST, Geerken AR, et al. Reliability and validity of neurobehavioral function on the Psychology Experimental Building Language test battery in young adults. PeerJ. 2015;3:e1460. doi:10.7717/peerj.1460
41. Fowler L, Blackwell A, Jaffa A, et al. Profile of neurocognitive impairments associated with female in-patients with anorexia nervosa. Psychol Med. 2006;36(4):517–522. doi:10.1017/S0033291705006379
42. Shallice T. Specific impairments of planning. Philos Trans R Soc Lond B Biol Sci. 1982;298(1089):199–209. doi:10.1098/rstb.1982.0082
43. Fuentes LJ, Vivas AB, Langley LK, Chen Q, Gonzalez-Salinas C. Inhibitory mechanisms in the attentional networks: a multidisciplinary approach. In: Posner MI, editor. Cognitive Neuroscience of Attention.
44. Fan J, McCandliss BD, Sommer T, Raz A, Posner MI. Testing the efficiency and independence of attentional networks. J Cogn Neurosci. 2002;14(3):340–347. doi:10.1162/089892902317361886
45. Rey A. Test de copia de una figura compleja. Manual de la adaptación Española. Madrid: TEA ediciones; 1987.
46. Abusamra V, Miranda MA, Ferreres A. Evaluación de la iniciación e inhibición verbal en español. Adaptación y normas del test de Hayling. Rev Arg Neuropsicología. 2007;9:19–32.
47. Lojo-Seoane C, Facal D, Juncos-Rabadán O, Pereiro AX. El nivel de vocabulario como indicador de reserva cognitiva en la evaluación del deterioro cognitivo ligero. Anal Psicol. 2014;30(3):1115–1121.
48. Gottesman II, Gould TD. The endophenotype concept in psychiatry: etymology and strategic intentions. Am J Psychiatry. 2003;160(4):636–645. doi:10.1176/appi.ajp.160.4.636
49. Kaye WH, Fudge JL, Paulus M. New insights into symptoms and neurocircuit function of anorexia nervosa. Nat Rev Neurosci. 2009;10(8):573–584. doi:10.1038/nrn2682
50. Danner UN, Sanders N, Smeets PAM, et al. Neuropsychological weaknesses in anorexia nervosa: set-shifting, central coherence, and decision making in currently ill and recovered women. Int J Eat Disord. 2012;45(5):685–694. doi:10.1002/eat.22007
51. Cipolletta S, Malighetti C, Serino S, Riva G, Winter D. Intrapersonal, interpersonal, and physical space in anorexia nervosa: a virtual reality and repertory grid investigation. Psychiatry Res. 2017;252:87–93. doi:10.1016/j.psychres.2017.02.060
52. Smeets MAM, Kosslyn SM. Hemispheric differences in body image in anorexia nervosa. Int J Eat Disord. 2001;29(4):409–416. doi:10.1002/eat.1037
53. Unoka Z, Richman M. Neuropsychological deficits in BPD patients and the moderator effects of co-ocurring mental disorders: a meta-analysis. Clin Psychol Rev. 2016;44:1–12. doi:10.1016/j.cpr.2015.11.009
54. Danner UN, Dingemans AE, Steinglass J. Cognitive remediation therapy for eating disorders. Curr Opin Psychiatry. 2015;28(6):468–472. doi:10.1097/YCO.0000000000000192
55. Wiederhold BK, Riva G, Gutiérrez-Maldonado J. Virtual reality in the assessment and treatment of weight-related disorders. Cyberpsychol Behav Soc Netw. 2016;19(2):67–73. doi:10.1089/cyber.2016.0012
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
