Back to Journals » Neuropsychiatric Disease and Treatment » Volume 10
Clinical utility of the Chinese Strengths and Weaknesses of ADHD-Symptoms and Normal-behaviors questionnaire (SWAN) when compared with DISC-IV
Authors Chan G, Lai KY , Luk ES, Hung S, Leung PW
Received 10 April 2014
Accepted for publication 19 May 2014
Published 21 August 2014 Volume 2014:10 Pages 1533—1542
DOI https://doi.org/10.2147/NDT.S65879
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Grace Fong-Chun Chan,1 Kelly Yee-Ching Lai,2 Ernest Siu-Luen Luk,3 Se-Fong Hung,2 Patrick Wing-Leung Leung4
1Department of Psychiatry, Alice Ho Miu Ling Nethersole Hospital, 2Department of Psychiatry, The Chinese University of Hong Kong, 3Private practice, 4Clinical and Health Psychology Centre, Department of Psychology, The Chinese University of Hong Kong, Hong Kong Special Administrative Region
Background: Attention-deficit/hyperactivity disorder (ADHD) is a common and impairing child and adolescent psychiatric disorder. Early identification and prompt treatment are essential. Rating scales are commonly used by clinicians and researchers to assess ADHD children.
Objective: In the current study, we aimed to examine the clinical utility of the Chinese version of the Strengths and Weaknesses of ADHD Symptoms and Normal Behaviors (SWAN) questionnaire. We validated its subscale scores against the Diagnostic Interview Schedule for Children Version IV (DISC-IV) and looked into its ability to identify ADHD in a psychiatric clinic setting. We also tested age and gender effects on SWAN scores. Specific subscale cutoff scores of SWAN were subsequently determined.
Method: A total of 290 children aged 6–12 years old studying in local mainstream primary schools were recruited from a clinic setting and interviewed with the parent version of DISC-IV. Their parents and teachers completed the corresponding version of SWAN.
Results: Both parent and teacher versions of SWAN were found to have good concurrent validity with DISC-IV. It could identify ADHD well in a clinic sample. Gender-specific cutoff scores were determined. Sensitivities and specificities were found to be satisfactory. SWAN was also found to perform equally well in identifying ADHD in those with and without comorbid Autistic Spectrum Disorder.
Conclusion: SWAN was proven to be a useful tool to aid the assessment of ADHD in a clinic sample.
Keywords: ADHD, SWAN, DISC-IV, validity
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is one of the most commonly diagnosed childhood psychiatric disorders. It is characterized by the presence of abnormal levels of inattention, hyperactivity, and impulsivity, and is pervasive across situations, persistent over time, and significantly impairs functioning. The fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM–IV) defines three subtypes of ADHD: (1) predominantly inattentive, (2) predominantly hyperactive–impulsive, and (3) combined types.1 These categories are retained in the latest fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).2
Age and gender have been reported to influence the prevalence and presentation of ADHD. A meta-analysis by Willcutt looked into the age effect on ADHD symptoms across different age groups: 3–5 years old, 6–12 years old, 13–18 years old, and ≥19 years old.3 Results supported that ADHD inattentive symptoms were relatively stable over time while ADHD hyperactive–impulsive symptoms declined gradually across different age groups. In terms of gender, the meta-analysis by Gaub and Carlson suggested that ADHD girls displayed greater intellectual impairment, lower levels of hyperactivity, and lower rates of other externalizing behaviors.4 Another more recent meta-analysis reported that in comparison to ADHD boys, ADHD girls had lower ratings on hyperactivity–impulsivity, inattention, and externalizing problems, but greater intellectual impairments and more internalizing problems than ADHD boys.5 Subsequent studies also consistently showed that ADHD girls were generally less symptomatic and less impaired than boys.6,7 In view of the gender difference, some researchers suggested that there should be cutoffs in assessments specific to each gender. The study by Waschbusch and King reported that a subset of ADHD girls was uniquely identified by gender-specific norms only.8
Many rating scales have been developed to measure the symptom severity of ADHD, including Connors’ Rating Scale,9,10 Swanson, Nolan, and Pelham (SNAP) rating scale,11 ADHD Rating Scale,12 and Vanderbilt Rating Scale.13 A potential problem with these questionnaires is that these scales ask about the presence of problem behaviors, and therefore run the risk of being skewed. With statistical analyses that assume a normal data distribution, the skewness may contribute to erroneous results and lead to over-identification.
In order to overcome this problem, Swanson et al developed the Strengths and Weaknesses of ADHD-Symptoms and Normal-Behaviors (SWAN) questionnaire.14 SWAN was developed from the SNAP Rating Scale. Without changing the content, each item of the SNAP Rating Scale was reworded in order to capture the strength corresponding to the weakness, and each item was rated from “far below average” (+3) to “far above average” (−3) relative to children of the same age. This was based on the idea that each item/symptom described an underlying dimension of behavior. Using SWAN, the original author yielded a distribution of ADHD scores that approximated a normal distribution in a community sample of elementary school-aged children. Factor analysis for the summary scores derived from SWAN resulted in 2 factors representing inattention and hyperactivity/impulsivity. The two subscale scores of SWAN matched the purpose of reflecting the two dimensions of ADHD. Furthermore, different from other commonly used instruments, by providing a dimensional measurement of attention and activity level, SWAN has been particularly useful in studies examining the clinical, genetics, neuroimaging, and neurocognitive studies of ADHD.15,16
Despite SWAN appearing to be a useful tool in the assessment of ADHD, its clinical utility in a clinic setting was understudied both internationally and locally. A study published in 2011 tested the psychometric properties of SWAN in a preschool sample17 and reported high internal consistency and moderate test–retest reliability. It demonstrated adequate convergent and discriminant validity in correlation with the Strengths and Difficulties Questionnaire (SDQ). A Hungarian study showed excellent internal consistency and moderate-to-good correlation with the relevant subscales of the Child Behavior Checklist and SDQ.18 However, all these studies recruited community samples only. Up to now, the only translation that was tested in a clinic sample was the French one.19 However, they recruited only 88 ADHD subjects without another psychiatric control and they reported the cutoff of the total score of the parent version only.
Regarding the local situation, SWAN was translated into Chinese by a previous study in the authors’ center.20 A community sample of 3,722 subjects was collected, and the mean scores of SWAN in both genders were calculated. A comparison was made with a clinic sample of 219 clinically diagnosed ADHD children. It confirmed a two-factor model. Cutoff scores were calculated yielding a sensitivity (SE) range of 55%–83% and specificity (SP) of 66%–89%. However, there were important limitations in this previous study. Firstly, the clinic ADHD sample was based on clinical diagnosis without specification of the ADHD subtype. Secondly, the cutoff scores were based on the comparison between the clinic ADHD group and the community control group. Thus, it could only conclude that SWAN was able to differentiate children with ADHD from normal children, while its ability to differentiate ADHD from other psychiatric diagnoses (non-ADHD) remained unanswered.
To summarize the current literature, SWAN was considered to be useful in the assessment of ADHD, with a unique characteristic in measuring the symptoms of ADHD on a continuum of weaknesses to strengths. However, its clinical utility was understudied. The cutoff total score of the parent version was determined in the French study,19 but the total score could not help to distinguish the different subtypes of ADHD. Only the SWAN subscale scores could serve this purpose but the determination of subscale cutoff scores would require the comparison of SWAN subscale scores among subjects of different ADHD subtypes. Up to now, this had not been done. Besides, gender- and age-specific cutoff scores of SWAN were not available from the literature. All of these factors hindered the utility of this useful assessment tool.
Objectives
The aim of this study was to examine the clinical utility of SWAN in a clinic setting.
Firstly, we aimed to validate the subscale scores of SWAN against Diagnostic Interview Schedule for Children Version IV (DISC-IV) so that SWAN can be used to identify ADHD subtypes according to the diagnostic algorithm. Secondly, we aimed to look into SWAN’s ability to differentiate ADHD from a non-ADHD psychiatric control. Lastly, we aimed to test the age and gender effect on SWAN scores. Specific subscale cutoff scores of SWAN were determined correspondingly.
No community control was included in this study as SWAN has been proven to be able to differentiate ADHD from a community control in the authors’ previous study.20
Methods
Participants
Subjects were children aged 6 to 12 years old studying in mainstream primary schools, who were newly referred to a child psychiatric clinic at Alice Ho Miu Ling Nethersole Hospital for assessment during the period July 2012 to April 2013. They were stratified into males and females and consecutively recruited. This stratification was to compensate for the male to female ratio of ADHD cases in the clinic, as well as the referral pattern in general. The parents of the potential subjects were approached by the principal investigator for consent to enroll in the study. The recruitment process continued until an adequate number of male and female cases and controls were recruited. In order to avoid the influence of ADHD medication on the clinical status, all the recruited subjects were drug naïve.
Children suffering from mental retardation, psychosis, or severe medical illnesses, including epilepsy, cerebral palsy, or medical illness that required long-term medication, were excluded. Though DSM-5 was not published at the time of this study, Autistic Spectrum Disorder (ASD) was not excluded since there was growing evidence to support the comorbidity between ASD and ADHD.21–26 It was also common to see co-occurrence of the two disorders in daily clinical practice. As a result, ASD was not excluded so as to enhance the clinical applicability of the current study results.
Ethical approval was obtained from the relevant institutional board on human subjects.
Sample size calculation
The validation of the SWAN-inattentive subscale (SWAN-IA) was based on the estimate provided in the previous study20 – a large effect size (Cohen’s d=0.8) on the mean difference of SWAN scores between the control and ADHD group in each gender. A total sample of 104 subjects – with equal case–control proportions for both genders – was required to achieve 80% power and 0.05 two-sided significance criteria.
The same criteria were applied to validate the SWAN-hyperactivity–impulsivity subscale (SWAN-HI). Since each subject would provide both SWAN-IA and SWAN-HI data, it was estimated that a cohort of subjects would be shared in validating both subscales.
Procedures
The purpose of the current study was explained to the parents and their written consent was sought. The principal investigator, who was blind to the clinical diagnosis of the children, interviewed the parents of the children with the parent version of the DISC-IV ADHD module in order to determine the presence or absence of ADHD diagnosis, and constituted the ADHD and non-ADHD psychiatric control groups, respectively. Parents would complete the parent version of SWAN (PSWAN). The teacher SWAN questionnaire (TSWAN) was given to the child’s class teacher for completion via the parents. Teachers would either mail or fax the questionnaires to the principal investigator.
Measures
DISC-IV is a highly structured respondent-based instrument initially designed for use by non-clinicians in large-scale epidemiological surveys to assess psychiatric diagnosis in children and adolescents according to DSM-IV criteria, occurring both in the past 12 months and in the past 4 weeks. There are parallel versions of the instrument, including a parent version for use in children aged 6–17 years old and a youth version for direct administration to subjects aged 9–17 years old. It was originally used in an English-speaking population in the US, and was later translated into different languages, including a Cantonese version in Hong Kong. There is extensive evidence supporting the reliability and validity of its various versions.27,28
In the current study, the ADHD module of DISC-IV was used to confirm ADHD diagnosis. The principal investigator was trained on how to administer the interview. The parent version of DISC-IV was employed since the test–retest reliability for ADHD diagnosis was found to be excellent in the parent version but poor in the youth version. DISC-IV consisted of two subsections, one for inattention (DISC-IA) and one for hyperactivity–impulsivity (DISC-HI), each having its own age of onset section and impairment section. Upon administration, DISC-IV first assesses if one has adequate numbers of inattentive and/or hyperactivity–impulsivity symptoms presented with adequate duration in two or more settings with onset before 7 years old. These responses are combined by the scoring program to determine whether a particular diagnostic criterion is fulfilled. Multiple symptoms (symptom count) are often used to determine whether a criterion is satisfied. The number of criteria satisfied are reported as the criterion count. Apart from this, the program asks about the impairments in different settings. The scoring program reports the symptom count, criterion count, and impairment criterion. The impairment criterion used in the current study was one severe or at least two intermediate impairments in six domains of daily functioning. This impairment criterion was recommended by the DISC Development Group in 2001.
Statistical methods
Data analysis was performed using SPSS® 20.0 statistical software (IBM Corporation, Armonk, NY, USA). In the comparison of demographical information and SWAN scores, Student’s t-test and chi-square test were used. Analysis of variance was used to determine the SWAN score difference among different subgroups. Spearman’s and Pearson’s correlation were used to determine the correlation between SWAN scores and DISC-IV diagnosis, criterion, and symptom counts. Receiver operating characteristic curves were generated to determine the cutoff scores of SWAN to differentiate children with ADHD from children with other psychiatric diagnoses. SE and SP of the cutoff scores were also determined. Statistical tests were based on a two-tailed test assumption. P<0.05 was considered significant unless stated otherwise.
Results
Figure 1 presents a flow chart of the recruitment process. During the study period, a total of 334 subjects were approached for interview, 86.8% of whom consented to join the study (140 male subjects and 150 female subjects). Between the refused and recruited groups, there were no significant differences in age (t=0.39, P=0.70, df=332) and gender distribution (χ2=3.61, P=0.06).
Out of the 140 male subjects, 54 were non-ADHD psychiatric controls, 85 were ADHD cases, and one was excluded because he did not exhibit clinically significant impairment. Concerning the subtypes of the ADHD cases, 47 were the combined subtype, 28 were the inattentive subtype, and ten were the hyperactivity–impulsivity subtype. As a result, the number of subjects who fulfilled DISC-IA criteria was 47+28=75; the number of subjects who fulfilled DISC-HI criteria was 47+10=57.
For female subjects, 95 of them were ADHD cases and 55 of them were non-ADHD psychiatric controls. Concerning the subtypes of the ADHD cases, 50 were the combined subtype, 42 were the inattentive subtype, and three were the hyperactivity–impulsivity subtype. As a result, the number of subjects who fulfilled DISC-IA criteria was 50+42=92; the number of subjects who fulfilled DISC-HI criteria was 50+3=53.
For both genders, there was no significant difference in age between the ADHD and non-ADHD psychiatric control groups (t=0.38, P=0.71, df=137 for males and t=−1.48, P=0.14, df=148 for females).
According to clinical diagnosis, the non-ADHD psychiatric control group comprised a full range of common child psychiatric diagnoses except ADHD. The most common diagnosis within the control group was ASD, which accounted for around 50% of the controls. Other common diagnoses included oppositional defiant disorder, anxiety disorders, and emotional disorders. Regarding the clinical comorbidity of the ADHD group, ASD was the most common comorbid diagnosis.
Distribution of SWAN scores
By applying the one sample Kolmogorov–Smirnov test, the distributions of the SWAN subscale scores were confirmed to be normally distributed in both male and female subjects.
Age and gender effects
There was no significant age effect on PSWAN and TSWAN subscale scores in both the ADHD and non-ADHD psychiatric control groups (r=−0.14 to 0.01, P=0.06–0.92). This was likely because the subjects recruited were aged 6–12 years old only – preschool or adolescent subjects were not included, thus the age effect on ADHD symptoms across age groups was not found here. This was also in line with the result of the previous local SWAN study.20
A significant gender effect was found in the non-ADHD psychiatric control group for both TSWAN-IA (t=2.54, P=0.01, df=103) and TSWAN-HI (t=3.03, P=0.003, df=103), with boys having significantly higher TSWAN scores. However, the gender effect was not significant for PSWAN-IA (t=−0.32, P=0.75, df=107) and PSWAN-HI (t=1.16, P=0.25, df=107). In the ADHD group, TSWAN-HI (t=3.11, P=0.002, df=170) was significantly higher in boys than girls. But there were no significant differences between gender in PSWAN-IA (t=0.14, P=0.89, df=178), PSWAN-HI (t=1.66, P=0.10, df=178), and TSWAN-IA scores (t=1.81, P=0.07, df=170). All the statistically significant differences had at least moderate effect sizes (Cohen’s d=0.48–0.59). All the insignificant results had a Cohen’s d score of <0.30.
In view of the variable gender differences found, an analysis of variance was performed to determine the main effects of the different versions of SWAN (ie, PSWAN and TSWAN), ADHD diagnosis, and gender on SWAN-IA and SWAN-HI scores. For SWAN-IA, the main effects of the different versions (F=17.82, P<0.001, df=1), ADHD diagnosis (F=313.79, P<0.001, df=1), and gender (F=4.08, P=0.04, df=1) were all significant (ηp2=0.06, ηp2=0.54, and ηp2=0.02, respectively). For SWAN-HI, the main effects of the different versions (F=55.91, P<0.001, df=1), ADHD diagnosis (F=178.26, P<0.001, df=1), and gender (F=15.39, P<0.001, df=1) were all significant (ηp2=0.17, ηp2=0.40, and ηp2=0.05, respectively).
The significant main effect of ADHD diagnosis implied that SWAN subscales were significantly affected by the presence/absence of ADHD diagnosis. The significant main effects of gender and the different versions on SWAN scores indicated the need to perform the subsequent analysis in separate gender and individual (ie, PSWAN and TSWAN) versions of SWAN, and the need to identify gender-specific cutoff scores for each version of SWAN.
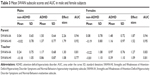
Correlation of SWAN and DISC-IV
We determined the correlation of SWAN subscales scores with the respective categorical DISC-IV diagnosis in inattentive and hyperactivity-impulsivity symptom domains by Spearman’s correlation. Statistically significant correlations were found (all P<0.001). For male subjects, the correlation coefficients of PSWAN-IA and TSWAN-IA with DISC-IA were 0.763 and 0.545, respectively, and the correlation coefficients of PSWAN-HI and TSWAN-HI with DISC-HI were 0.714 and 0.466, respectively. For female subjects, the correlation coefficients of PSWAN-IA and TSWAN-IA with DISC-IA were 0.743 and 0.556, respectively, and the correlation coefficients of PSWAN-HI and TSWAN-HI with DISC-HI were 0.746 and 0.518, respectively (Table 1).
The correlation of SWAN subscale scores with the respective symptom and criterion counts of DISC-IV were then determined by Pearson’s correlation. Statistically significant correlations were found for both symptom and criterion counts (all P<0.001) with correlation coefficients of 0.550–0.796 and 0.516–0.777 for male and female subjects, respectively (Table 2).
SWAN score differences according to DISC diagnosis in inattentive (DISC-IA) and hyperactivity/impulsivity (DISC-HI) symptom domains
Using Student’s t-test, there was significant difference (all P<0.001) in SWAN-IA scores found between those who fulfilled DISC-IA criteria versus those who did not. This was true for both PSWAN-IA (t=13.23, df=137, Cohen’s d=2.24 for males and t=12.71, df=148, Cohen’s d=2.09 for females) and TSWAN-IA (t=6.99, df=130, Cohen’s d=1.21 for males and t=7.61, df=143, Cohen’s d=1.25 for females). Similarly, significant differences (all P<0.001) were also found in SWAN-HI scores between those who fulfilled DISC-HI criteria versus those who did not. Again, this was true for both PSWAN-HI (t=10.96, df=137, Cohen’s d=1.91 for males and t=12.11, df=148, Cohen’s d=2.13 for females) and TSWAN-HI (t=6.14, df=130, Cohen’s d=1.10 for males and t=6.95, df=143, Cohen’s d=1.21 for females).
Whether SWAN score can identify ADHD in children with ASD
An analysis of variance was used to look into any difference in SWAN scores among non-ADHD psychiatric controls with ASD, non-ADHD psychiatric controls without ASD, ADHD with ASD, and ADHD without ASD in males and females separately. Significant differences (all P<0.001) were found among groups in PSWAN-IA (F=57.87, df=138 for males and F=42.73, df=149 for females), PSWAN-HI (F=37.01, df=138 for males and F=26.54, df=149 for females), TSWAN-IA (F=19.52, df=131 for males and F=19.84, df=144 for females), and TSWAN-HI (F=12.75, df=131 for males and F=13.18, df=144 for females). Post-hoc analysis was done to look into the significant differences. For male subjects, significant differences were found between subjects with and without ADHD (P<0.001–0.040) in both subscales in both versions, while presence of ASD did not result in any significant difference (P=0.556–1.000). For female subjects, significant differences were found between subjects with and without ADHD (all P<0.001–0.002) in both subscales in both versions, while presence of ASD did not result in any significant difference (P=0.541–1.000).
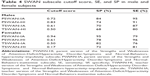
Receiver operating characteristic curves and area under curve
Receiver operating characteristic curves were generated to determine the discriminant capacity of SWAN subscale cutoff scores. Cutoff scores would be reported as specific to gender and individual versions of SWAN due to the significant main effects of gender and the different versions.
The area under the curve results were excellent and ranged from 0.95 (PSWAN-HI for female subjects) to 0.77 (TSWAN-HI for male subjects) (Table 3). Regarding the cutoff scores, they were calculated by choosing the maximal sum of SE and SP. The cutoff scores for male subjects were 0.72 (SP 84%, SE 95%) for PSWAN-IA, 0.83 (SP 74%, SE 91%) for PSWAN-HI, 0.61 (SP 70%, SE 87%) for TSWAN-IA, and 0.50 (SP 68%, SE 80%) for TSWAN-HI. For female subjects, the cutoff scores were 0.94 (SP 95%, SE 79%) for PSWAN-IA, 0.61 (SP 78%, 96%) for PSWAN-HI, 0.50 (SP 82%, 76%) for TSWAN-IA, and 0.17 (SP 72%; SE 81%) for TSWAN-HI (Table 4). All the above scores were the mean scores across the nine items in the respective subscale.
Discussion
ADHD, being a common and impairing disorder, not only influences the functioning of affected children but also the quality of life of their parents.29 It is important to have a valid and reliable tool for assessment.
The previous SWAN study in Hong Kong confirmed the reliability and two-factor structure of SWAN.20 This was the first study to look into the validity of the Chinese version of SWAN by comparing it with a structured interview. The current study determined the clinical utility of SWAN, by recruiting a sufficient number of girls, to determine gender-specific subscale cutoff scores in a clinic sample. It was demonstrated that SWAN can reliably differentiate ADHD from non-ADHD psychiatric controls. Moreover, the SE and SP found in the current study (SE 76%–96%, SP 68%–95%) were generally similar or better than the other rating scales for ADHD, including ADHD Rating Scale (SE 63%–84%, SP 49%–86%), Connors’ Rating Scale (SE 78%–92%, SP 91%–94%),30 Vanderbilt Rating Scale (SE 67%–80%, SP 75%–86%),31 and the previous local study (SE 55%–83%, SP 66%–89%) and international studies on SWAN (SE 86%, SP 88%).19,20
Furthermore, there was a lack of data on the performance of ADHD rating scales in children with ASD. This study provided important data to support that SWAN could be used to identify ADHD symptoms even in the presence of ASD, as the presence of ASD diagnosis did not affect the performance of SWAN in differentiating ADHD from non-ADHD.
When compared with the structured interview, SWAN subscale scores were found to have strong correlations with the corresponding categorical DISC diagnosis in IA and HI symptom domains, the respective symptom counts and criterion counts. It was concluded that SWAN, being a simple rating scale, was found to have good concurrent validity with the highly structured interview DISC-IV.
Moreover, with validation of the subscale scores in this study, the subscale scores could be used for assessment of the corresponding inattentive and hyperactivity–impulsivity symptom dimension and aid the identification of the ADHD subtype according to the diagnostic algorithm.
This study was initially done according to DSM-IV as it was the latest diagnostic system available at the time of study. After publication of DSM-5, the authors tried to map DSM-IV with DSM-5 ADHD diagnostic criteria. The major differences between DSM-IV and DSM-5 for diagnosis of ADHD in the target age group (6–12 years old) were: (1) DSM-5 no longer excludes ASD, (2) DSM-5 requires onset age before 12 years old instead of 7 years old, and (3) DSM-5 requires the evidence that the symptoms interfere with or reduce the quality of social, academic, or occupational functioning, whereas DSM-IV requires a more severe impairment condition to be considered clinically significant. In the current sample, ASD was not excluded during the recruitment. No ADHD subject was excluded due to age of onset after 7 years old. Only one boy was excluded from the ADHD group due to clinically insignificant impairment according to DSM-IV, but when the analyses were run again with inclusion of this subject, there were no significant changes in the results. Therefore, the results found in the current study are still applicable in a clinic sample aged 6–12 years old even with DSM-5 diagnostic criteria.
Conclusion
In the current study, the results show that SWAN has good concurrent validity with the highly structured interview DISC-IV and it can reliably identify ADHD in a psychiatric clinic with satisfactory SE and SP. With the gender-specific subscale cutoff scores determined in the current study, SWAN can be used to identify ADHD subtypes according to the diagnostic algorithm.
The use of ADHD rating scales in an ASD population is an understudied area. This study provides evidence that SWAN can reliably identify ADHD even in children with ASD.
Therefore, SWAN is a useful tool to aid assessment of ADHD in a clinic sample.
Disclosure
The authors report there are no conflicts of interest in this work.
References
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th Edition: DSM-IV. Washington, DC: American Psychiatric Association; 1994. | ||
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-V. Washington, DC: American Psychiatric Association; 2013. | ||
Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics. 2012;9(3): 490–499. | ||
Gaub M, Carlson CL. Gender differences in ADHD: a meta-analysis and critical review. J Am Acad Child Adolesc Psychiatry. 1997;36(8): 1036–1045. | ||
Gershon J. A meta-analytic review of gender differences in ADHD. J Atten Disord. 2002;5(3):143–154. | ||
Graetz BW, Sawyer MG, Baghurst P. Gender difference among children with DSM-IV ADHD in Australia. J Am Acad Child Adolesc Psychiatry. 2005;44(2):159–168. | ||
Newcorn JH, Halperin JM, Jensen PS, et al. Symptom profiles in children with ADHD: effects of comorbidity and gender. J Am Acad Child Adolesc Psychiatry. 2001;40(2):137–146. | ||
Waschbusch DA, King S. Should sex-specific norms be used to assess attention-deficit/hyperactivity disorder or oppositional defiant disorder? J Consult Clin Psychol. 2006;74(1):179–185. | ||
Conners CK, Sitarenios G, Parker JD, Epstein JN. The revised Conners’ Parent Rating Scale (CPRS-R): Factor structure, reliability, and criterion validity. J Abnorm Child Psychol. 1998;26(4):257–268. | ||
Conners CK, Sitarenios G, Parker JD, Epstein JN. Revision and restandardization of the Conners’ Teacher Rating Scale (CTRS-R): Factor structure, reliability, and criterion validity. J Abnorm Child Psychol. 1998;26(4):279–291. | ||
Swanson J. School based Assessment and Intervention for ADD students. Irvine, CA: KC; 1992. | ||
DuPaul GJ, Power TJ, Anastopoulos AD, Reid R. ADHD Rating Scale-IV: Checklists, Norms and Clinical Interpretation. New York: Guilford; 1998. | ||
Wolraich ML, Lambert W, Doffing M, Bickman L, Simmons T, Worley K. Psychometric Properties of the Vanderbilt ADHD Diagnostic Parents Rating Scale in a Referred Population. J Pediatr Psychol. 2003;28(8):559–568. | ||
Swanson J, Schuck S, Mann M, et al. Categorical and Dimensional Definitions and Evaluations of Symptoms of ADHD: The SNAP and the SWAN Rating Scales. 2005. Available from: http://www.adhd.net/SNAP_SWAN.pdf. Accessed June 24, 2014. | ||
Hay DA, Bennett KS, Levy F, Sergeant J, Swanson J. A twin study of attention-deficit/hyperactivity disorder dimensions rated by the strengths and weaknesses of ADHD-symptoms and normal-behavior (SWAN) scale. Biol Psychiatry. 2007;61(5):700–705. | ||
Volkow ND, Wang GJ, Kollins SH, et al. Evaluating dopamine reward pathway in ADHD: clinical implications. JAMA. 2009;302(10): 1084–1091. | ||
Lakes KD, Swanson J, Riggs M. The reliability and validity of the English and Spanish strengths and weaknesses of ADHD and normal behavior rating scales in a preschool sample: continuum measures of hyperactivity and inattention. J Atten Disord. 2011;16(6):510–516. | ||
Lakatos K, Birkas E, Toth I, Gervai J. [Screening childhood behavior problems using short questionnaires II: The Hungarian version of the SWAN-scale (strengths and weaknesses of ADHD-symptoms and normal-behavior) for screening attention deficit/hyperactivity disorder]. Psychiatria Hungarica. 2010;25(6):493–502. Hungarian. | ||
Robaey P, Amre D, Schachar R, Simard L. French version of the strengths and weaknesses of ADHD and normal behaviors (SWAN-F) questionnaire. J Can Acad Child Adolesc Psychiatry. 2007;16(2):80–89. | ||
Lai KY, Leung PW, Luk ES, Wong AS, Law LS, Ho KK. Validation of the Chinese strengths and weaknesses of ADHD-symptoms and normal-behaviors questionnaire in Hong Kong. J Atten Disord. 2013;17(3): 194–202. | ||
Gargaro BA, Rinehart NJ, Bradshaw JL, Tonge BJ, Sheppard DM. Autism and ADHD: how far have we come in the comorbidity debate Neurosci Biobehav Rev. 2011;35(5):1081–1088. | ||
Lecavalier L, Gadow KD, DeVincent CJ, Edwards MC. Validation of DSM-IV model of psychiatric syndromes in children with autism spectrum disorders. J Autism Dev Disord. 2009;39(2):278–289. | ||
de Bruin EI, Ferdinand RF, Meester S, de Nijs PF, Verheij F. High rates of psychiatric co-morbidity in PDD-NOS. J Autism Dev Disord. 2007;37(5):877–886. | ||
Gjevik E, Eldevik S, Fjaeran-Granum T, Sponheim E. Kiddie-SADS reveals high rates of DSM-IV disorders in children and adolescents with autism spectrum disorders. J Autism Dev Disord. 2011;41(6): 761–769. | ||
Reiersen AM, Constantino JN, Volk HE, Todd RD. Autistic traits in a population-based ADHD twin sample. J Child Psychol Psychiatry. 2007;48(5):464–472. | ||
Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):921–929. | ||
Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39(1):28–38. | ||
Ho TP, Leung PW, Lee CC, et al. Test–retest reliability of the Chinese version of the Diagnostic Interview Schedule for Children-Version 4 (DISC-IV). J Child Psychol Psychiatry. 2005;46(10):1135–1138. | ||
Xiang YT, Luk ES, Lai KY. Quality of life in parents of children with attention-deficit-hyperactivity disorder in Hong Kong. Aust N Z J Psychiatry. 2009;43(8):731–738. | ||
Collett BR, Ohan JL, Myers KL. Ten-year review of rating scales. V: scales assessing attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2003;42(9):1015–1037. | ||
Bard DE, Wolraich ML, Neas B, Doffing M, Beck L. The psychometric properties of the Vanderbilt attention-deficit hyperactivity disorder diagnostic parent rating scale in a community population. J Dev Behav Pediatr. 2013;34(2):72–82. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.