Back to Journals » OncoTargets and Therapy » Volume 9
Clinical utility of letrozole in the treatment of breast cancer: a Chinese perspective
Received 21 August 2015
Accepted for publication 30 December 2015
Published 1 March 2016 Volume 2016:9 Pages 1077—1084
DOI https://doi.org/10.2147/OTT.S81087
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Daniele Santini
Dong-xu He,1 Xin Ma2
1National Engineering Laboratory for Cereal Fermentation Technology, 2School of Pharmaceutical Sciences, Jiangnan University, Wuxi, People’s Republic of China
Abstract: The incidence rate of breast cancers in People’s Republic of China has increased in the last decade, and many cases are responsive to hormone therapies. The third-generation aromatase inhibitor letrozole inhibits estrogen production, and is more efficacious than the estrogen receptor inhibitor tamoxifen. In recent years, letrozole has been widely used to treat postmenopausal breast cancers in People’s Republic of China. Also, metastatic, premenopausal, and male breast cancers have been effectively treated by a combination of letrozole with cytotoxic, radiation, or other therapies. In this review, we provide a perspective and summary of recent advances in the use of letrozole for breast cancer in Chinese patients.
Keywords: breast cancer, Chinese, letrozole
General introduction to letrozole
Breast cancer is one of the most frequently diagnosed cancers globally, and the leading cause of cancer death among females.1 Based on the diverse expression of estrogen receptor-α (ER-α), progesterone receptor, human epidermal growth factor receptor-2 (HER2), claudin, cytokeratin, and other molecular markers, a growing number of recognized biological subtypes of breast cancer have been identified, such as luminal A, luminal B, HER2, basal-like, and claudin-low. Luminal A and luminal B are common subtypes that express ER (ER+), and they depend on estrogens to support cancer development and progression. Cutting off the estrogen supply to ER+ breast cancer cells leads to tumor regression. One strategy is to antagonize ER, predominantly with tamoxifen, which has become the gold standard for the treatment of ER+ breast cancer patients over the past decades.2–5 On the other hand, estrogen deprivation therapy, which inhibits estrogen production, is emerging as another important treatment strategy for estrogen-dependent breast cancer.6,7
Letrozole and breast cancer
Elimination of estrogen production can be achieved by aromatase inhibitors. These inhibitors antagonize the conversion of androgens into estrogen by targeting the aromatase enzyme and have been increasingly used to inhibit estrogen production in breast cancers.6 Compounds that inhibit aromatase have been developed from the first- to the third-generation inhibitors, and letrozole (Femara®; Novartis Pharmaceuticals Basel, Switzerland) is a third-generation aromatase inhibitor with high selectivity. Specifically, because aromatase in peripheral tissues provides the major source of estrogens in postmenopausal women, and letrozole inhibits aromatase activity in these tissues by >99% in vivo,8 letrozole is most widely used in advanced, recurrent, or metastatic breast cancers in postmenopausal patients. In premenopausal women, high levels of estrogens are produced primarily from the ovaries, where compensatory feedback loops for gonadotropin production dampen the effectiveness of letrozole.9
In recent decades, trials of letrozole in hormone-dependent breast cancer have shown encouraging progress compared with the ER antagonist tamoxifen. Letrozole has been used as a second-line therapy for patients with advanced breast cancer after other types of endocrine therapy such as tamoxifen, and it significantly improves disease-free and distant disease-free survival10,11 and increases the overall objective response rate (RR).12 Also, some studies have reported that the efficacy of letrozole is superior to tamoxifen as first-line therapy. Letrozole shows better efficacy than tamoxifen in terms of delayed time to progression, time to treatment failure, and increased overall objective RR in advanced and metastatic breast cancer.13,14 Furthermore, other trials indicate a better outcome among women treated with letrozole than among those treated with tamoxifen in both adjuvant15,16 and neoadjuvant17,18 settings.
The efficacy of letrozole can be enhanced by combination with other chemotherapeutic agents. For example, letrozole plus lapatinib, which is an HER2 inhibitor, has shown good results in progression-free survival, objective RR, and clinical benefit rate (CBR) in HER2+ and ER+ metastatic breast cancer.19,20 Also, combination with the rapamycin (mTOR) inhibitors temsirolimus21 and everolimus22 as well as the cyclin-dependent kinase inhibitor palbociclib23 improves letrozole efficacy. However, not every combination yields positive results. Bevacizumab, which is an angiogenesis inhibitor, has no effect on the efficacy of letrozole.24
Letrozole in People’s Republic of China
Overview of breast cancer status in People’s Republic of China
The incidence rate of breast cancer in People’s Republic of China has increased in this decade for multifactorial reasons, which include environmental pollution, changes in dietary structure, and exposure to exogenous estrogen, as well as the availability of early detection services that have contributed to increased reporting.25,26
The latest incidence rate of breast cancer (in 2011) was 37.86 per 100,000 (a total of 248,000 cases; an age-standardized rate [ASR] of 28.51 per 100,000). It is the most frequently diagnosed cancer in People’s Republic of China. The mortality from breast cancer was 9.21 per 100,000 total cancer deaths (a total of 60,000 deaths; ASR, 6.57 per 100,000).27
Age and area are two major risk factors for breast cancer in People’s Republic of China. Females aged between 25 and 59 years are a high-risk population, and the incidence rate peaks in the 55–59 year age-group (~80 per 100,000).26 In addition, urban areas have a higher incidence rate at 46.74 per 100,000 (ASR, 33.66 per 100,000) compared to 28.43 per 100,000 (ASR, 22.59 per 100,000) in rural areas.27 Also, the incidence rates in the western, middle, and eastern areas of People’s Republic of China differ. The eastern and middle areas have similar higher incidence rates of 35.57 and 35.58 per 100,000 (ASR, 26.21 and 26.36 per 100,000), respectively, compared to the western area at 23.47 per 100,000 (ASR, 18.03 per 100,000).
Application of letrozole in People’s Republic of China
Clinical studies from both global and Chinese trials have shown that letrozole is effective and tolerated in ER+ breast cancers, so letrozole has ranked among the top ten for anticancer drug consumption in People’s Republic of China during the recent years.28–30 Letrozole manufactured locally (Jiangsu Hengrui Medicine Co., Ltd., Lianyungang, Jiangsu, People’s Republic of China) is chosen by many patients because its price is lower than Femara® from Novartis Pharmaceuticals. Studies have shown that the pharmacokinetics, side effects, and efficacy do not significantly differ between letrozole made locally and by Novartis.31,32
Neoadjuvant treatment with letrozole in People’s Republic of China
The incidence rate of breast cancer in postmenopausal women in People’s Republic of China is gradually increasing, partly because of population aging, increased breast cancer awareness, and screening activity. However, older patients have less efficient cellular repair, organ function, and drug catabolism. Also, cardiovascular disease, diabetes, hypertension, and other infirmities occur frequently. Therefore, such patients are vulnerable to chemotherapy-related cytotoxicity and side effects. In addition, extensive surgery is rarely offered to older patients due to concerns about the increased risk of surgical morbidity and mortality. Therefore, endocrine treatments in the neoadjuvant setting are now the treatment of choice in People’s Republic of China to treat older ER+ breast cancer patients; such treatment allows good disease control and less extensive surgery, and is fairly well tolerated.
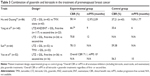
Several clinical trials have been performed in postmenopausal breast cancer patients (tumor node metastatsis stages I–III) to compare the efficacy of letrozole and tamoxifen in the neoadjuvant setting.33–37 Patients were given 2.5 mg/day letrozole or 20 mg/day tamoxifen for 60–90 days. The overall RR of the two regimes was calculated as a percentage of the complete and partial response in all patients, and then compared. The results showed that both letrozole and tamoxifen are well tolerated, but letrozole is more effective, with a higher RR than tamoxifen (Table 1). The differences between letrozole and tamoxifen were similar in groups from different parts of People’s Republic of China, while the RR values varied between groups, perhaps due to methodological differences in the measurement of response and the small sample sizes.
  | Table 1 Trials comparing efficacy of letrozole and tamoxifen in China |
Furthermore, a nonrandomized study has evaluated the efficacy of letrozole for postmenopausal women with advanced breast cancer in whom neoadjuvant tamoxifen therapy failed.38 Patients failing to respond to first-line endocrine therapy were treated with letrozole, anastrozole, or exemestane as second-line therapy. The CBR (percentage of patients with complete or partial response and stable disease) was 72.73% in the letrozole group, similar to the anastrozole (62.5%) and exemestane (78.57%) groups. The results of this study thus show that letrozole is effective as a second-line therapy in tamoxifen-resistant patients. Nevertheless, outcomes of first- and second-line treatments of letrozole are different as demonstrated in the aforementioned studies.33–37 Another systematic study also showed first-line application of letrozole achieved longer progression-free survival period (9 months) and higher CBR (80.9%) than second-line treatment (progression-free survival period: 3 months; CBR: 28.6%).39
In addition, similar with the Phase III BIG 1-98 trial,16,40 effectiveness of sequential therapy of tamoxifen and letrozole was compared with letrozole monotherapy in Chinese breast cancer patients.41 The patients received tamoxifen for 2–3 years and were sequentially treated with letrozole for 2–3 years, and they yielded a lower rate of recurrence and side effects compared with patients treated with 5 years of monotherapy of letrozole, suggesting that the effect of letrozole could be enhanced with combination of tamoxifen. However, these results are inconsistent with results from updated BIG 1-98 trial,40 which showed that 8-year sequential treatments involving tamoxifen and letrozole did not statistically improve outcome compared with letrozole monotherapy, but the sequential treatments could still reduce individual patient’s risk of recurrence. Therefore, whether sequential therapy of tamoxifen and letrozole can yield better outcome in Chinese population still needs validation in larger population and with longer duration of trial.
Letrozole treatment for metastatic breast cancer
Letrozole has been combined with cytotoxic chemotherapeutic agents to treat ER+ metastatic breast cancers, regardless of the menopausal status of patients.
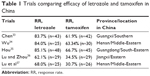
In Han’s studies,42 capecitabine and letrozole were used together as second-line therapy for metastatic breast cancer patients, in whom the first round of anthracycline- and taxane-based therapy failed. Letrozole was given at 2.5 mg/day for 6 months, and capecitabine was given at 2,510 mg/m2/day for 14 days. The treatments yielded a CBR of 86%. Also, an RR of 48% and a median time to progression (TTP) of 12.2 months were found; side effects were usually mild to moderate. Similarly, in another study,43 patients who were resistant to anthracycline and tamoxifen chemotherapy and with metastatic events were identified, then 2,510 mg/m2/day capecitabine was given for 14 days together with letrozole (2.5 mg/day for 5 years). The results were: CBR, 52.5%; RR, 22.5%; and TTP, 178 days. In People’s Republic of China, capecitabine is frequently used as a second-line agent to treat metastatic breast cancers. Previous studies have shown a CBR for capecitabine of 37.31% in a Chinese population with advanced breast cancer.44 Therefore, the two previously mentioned studies42,43 suggest that letrozole can improve the efficacy of capecitabine. Treatment with zoledronic acid accompanied by letrozole in patients with bone metastasis has been reported in three studies (Table 2).45–47 Patients had been treated with chemotherapy, radiotherapy, surgery, or tamoxifen, and this was followed by bone metastasis. Then letrozole was given with or without zoledronic acid. The results showed that letrozole had better efficacy in decreasing bone metastasis when combined with zoledronic acid, thus again demonstrating the benefit of combining letrozole with chemotherapy as second-line therapy for metastatic breast cancers. Moreover, zoledronic acid was used in one Chinese trial to relieve the side effects caused by letrozole. Bone mineral density and life quality were improved by zoledronic acid during letrozole treatment.48 The results were supported by a recent foreign Phase III study, indicating zoledronic acid increased bone mineral density and disease-free survival of early breast cancer patients receiving adjuvant letrozole.49
In recent years, based on the effectiveness of letrozole in treating ER+ breast cancer, some Chinese trials began to use a combined chemo-letrozole regime as first-line therapy for patients with advanced breast cancer. In a study of advanced breast cancer patients with lymph node, skin, bone, lung, and liver metastasis, letrozole (2.5 mg/day for at least 56 days) treatment was accompanied by pirarubicin, a topoisomerase II inhibitor (40 mg/m2/day for 42 days).50 The results gave a CBR of 58.7%, an RR of 30.4%, and a TTP of 10 months, indicating that the letrozole and pirarubicin combination is effective in treating metastatic breast cancers, with minor side effects reported in only a few patients. Furthermore, in another two studies, letrozole was combined with paclitaxel and cisplatin to treat metastatic breast cancer, giving an RR of 54.84%,51 a CBR of 73.08%,52 and a Karnofsky value improved by 64.52%51 with good tolerability. Therefore, these results further indicate that chemo-letrozole combined regimes are effective and well tolerated in patients with metastatic breast cancer.
Letrozole treatment in premenopausal women with breast cancer
In People’s Republic of China, breast cancer rates increase rapidly before menopause; more than half of breast cancers are found in premenopausal women between 25 and 55 years of age, 10–15 years earlier than in Western patients.26 Ovarian functional ablation plus tamoxifen treatment have been used to treat premenopausal breast cancer.53 Recently, the effect of ovarian functional ablation plus letrozole treatment was studied in premenopausal Chinese patients with breast cancer (Table 3).54–57 Goserelin (3.6 mg/28 days) was used to ablate ovarian function, and 2.5 mg/day letrozole was given at the same time. The results of these studies indicate that letrozole plus goserelin benefit premenopausal patients by increasing the CBR and prolonging the median progression-free survival.
Patients in these studies had received systemic cytotoxic, radiation, or endocrine therapy before the goserelin plus letrozole treatment, so letrozole was used as either first- or second-line therapy. The results of the studies by Yang et al55 and Yao et al57 suggested that the efficacy of letrozole as first-line therapy is better than that of second-line therapy in combination with goserelin.
Overall, the treatment was generally well tolerated; in three studies,54–56 no patients quit the trials due to intolerable side effects. However, in another study,57 two patients withdrew because of grade II hot flushes and grade II face and foot edema.
Although ovarian functional ablation plus letrozole strategies are commonly used, some recent studies applied letrozole in combination with chemotherapy or surgery in premenopausal breast cancer patients. Letrozole combined with paclitaxel and cisplatin was effective in treating premenopausal breast cancer patients.51,52 In addition, letrozole treatment after radical mastectomy of breast cancer achieved an RR of 60%, significantly higher than tamoxifen treatment after surgery (35%).58 Therefore, these studies suggest new strategies for letrozole treatment.
Letrozole in male patients with breast cancer
Male breast cancer accounts for 1%–2% of all breast cancers with ~0.1% cancer mortality.59,60 The incidence rate of male breast cancer is highest in Africa, followed by North America and Europe, and lowest in Asia.59 The epidemiology of breast cancer in Chinese males has not been frequently studied. One study reported that the incidence rate of male breast cancer in southwest People’s Republic of China (Chongqing Province) changed from 1.96% in 2007 to 6.5% in 2010,61 suggesting an increasing trend.
Because of the small sample size for male breast cancer, it is difficult to organize randomized clinical trials to investigate systematic treatment. Therefore, male breast cancer patients are usually treated with regimes based on those for female patients. In the Chinese Clinical Oncology Society, several successful cases of the treatment of male breast cancer patients have been reported. Because >90% of male breast cancers express ER,62 hormone therapy is frequently used, and letrozole is one frequently used therapy.
In one study,63 the effect of aromatase inhibitors (including letrozole) was compared with that of tamoxifen in treating male breast cancer. However, unlike studies in female breast cancer indicating that aromatase inhibitors are better than tamoxifen, the 5-year progression-free survival rates (69.4% vs 77.0%) and overall survival rates (75.0% vs 83.4%) were not significantly different between aromatase inhibitors and tamoxifen. Nevertheless, the study indeed suggests that aromatase inhibitors, including letrozole, are effective agents and can increase the survival rate of males with breast cancer.
Metastatic breast cancer was treated with letrozole in another two male cases.64,65 In one case, the patient was treated with cyclophosphamide, perarubicin, and carboplatin as rescue therapy. Castration was performed after stabilization of the disease. Then letrozole (2.5 mg/day) was given for 4 months, which yielded a partial response.64 In the other case,65 the patient was also treated with cyclophosphamide, perarubicin, carboplatin, and castration. Then letrozole was given for 4 years, and a partial response was initially obtained. Unfortunately, after 4 years of treatment, a lung metastasis recurred. Therefore, these data suggest that long-term use of letrozole may lead to letrozole resistance, while during the early period of treatment, chemotherapy, castration, and letrozole are effective and well tolerated in metastatic breast cancer in males. So, it is necessary to search for a backup regime for letrozole resistance; in Zhang’s study,65 paclitaxel was used to treat the recurrence after letrozole, but follow-up information is not yet available.
Management of side effects
Long-term use of letrozole may lead to hypoestrogenism, which is associated with side effects such as sweating, hot flashes, arthralgia, and fatigue. Adverse effects in bone, joint, and muscle are common. Vitamin D and calcium, bisphosphonates, and appropriate physical exercise are prescribed for patients with osteoporosis or joint and muscle pain. Nonsteroidal anti-inflammatory drugs can be used in patients with serious symptoms.66
Sweating and hot flashes negatively influence the quality of life of breast cancer patients. Drugs such as venlafaxine,67 tibolone,68 and vitamin E69 are prescribed by oncologists and pharmacologists in People’s Republic of China to relieve the symptoms. Furthermore, traditional Chinese medicine is one of the most frequently chosen options in dealing with various diseases. Several clinical studies have reported the effectiveness of Chinese medicine in treating the sweating, hot flashes, irritability, and insomnia caused by letrozole treatment, probably by improving the function and metabolism of the kidney,70 liver,71 or both.72 Although these Chinese medicines can improve the quality of life of breast cancer patients, their mechanisms of action and applicability in cancer patients need further clarification with bigger sample sizes.
Conclusion
Letrozole is widely used in People’s Republic of China to treat breast cancers. Dozens of clinical trials have demonstrated the means by which letrozole application reduces cancer and improves the quality of life in Chinese patients with breast cancer. The results of most of these studies are not only encouraging and consistent with those from other countries, but also explain the response features of the Chinese population to letrozole. Furthermore, some of the investigations have not been frequently reported in studies overseas. For example, the prevention of bone metastasis by zoledronic acid and letrozole, and the treatment of male breast cancers are promising areas worthy of exploration in more patients. Indeed, the number of enrolled patients is small in most of the Chinese trials outlined earlier, which inevitably introduces statistical errors. Also, the duration of these trials was short and trials with study period >5 years are seldom reported, resulting in a lack of evidence on letrozole resistance and long-term adverse events. Moreover, the US Food and Drug Administration has recently approved palbociclib to treat metastatic breast cancer together with letrozole. Such new treatment yields significantly longer progression-free survival than with letrozole alone,73 but there has been no reports on the effect of this treatment on Chinese population. Therefore, we anticipate further studies with larger populations, longer durations, and new methods to improve the lives of breast cancer patients in People’s Republic of China.
Disclosure
The authors report no conflicts of interest in this work.
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108. | ||
Early Breast Cancer Trialists’ Collaborative Group. Tamoxifen for early breast cancer. Cochrane Database Syst Rev. 2001;(1):CD000486. | ||
Early Breast Cancer Trialists’ Collaborative Group. Tamoxifen for early breast cancer: an overview of the randomised trials. Lancet. 1998;351:1451–1467. | ||
Pritchard KI. Breast cancer prevention with selective estrogen receptor modulators: a perspective. Ann N Y Acad Sci. 2001;949:89–98. | ||
Wickerham L. Tamoxifen – an update on current data and where it can now be used. Breast Cancer Res Treat. 2002;75(Suppl 1):S7–S12. | ||
Osborne C, Tripathy D. Aromatase inhibitors: rationale and use in breast cancer. Annu Rev Med. 2005;56:103–116. | ||
Osborne CK, Schiff R. Estrogen-receptor biology: continuing progress and therapeutic implications. J Clin Oncol. 2005;23:1616–1622. | ||
Haynes BP, Dowsett M, Miller WR, Dixon JM, Bhatnagar AS. The pharmacology of letrozole. J Steroid Biochem Mol Biol. 2003;87:35–45. | ||
Miller WR, Larionov AA. Understanding the mechanisms of aromatase inhibitor resistance. Breast Cancer Res. 2012;14(1):201. | ||
Goss PE, Ingle JN, Martino S, et al. A randomized trial of letrozole in postmenopausal women after five years of tamoxifen therapy for early-stage breast cancer. N Engl J Med. 2003;349:1793–1802. | ||
Goss PE, Ingle JN, Martino S, et al. Randomized trial of letrozole following tamoxifen as extended adjuvant therapy in receptor-positive breast cancer: updated findings from NCIC CTG MA.17. J Natl Cancer Inst. 2005;97:1262–1271. | ||
Dombernowsky P, Smith I, Falkson G, et al. Letrozole, a new oral aromatase inhibitor for advanced breast cancer: double-blind randomized trial showing a dose effect and improved efficacy and tolerability compared with megestrol acetate. J Clin Oncol. 1998;16:453–461. | ||
Mouridsen H, Gershanovich M, Sun Y, et al. Superior efficacy of letrozole versus tamoxifen as first-line therapy for postmenopausal women with advanced breast cancer: results of a phase III study of the International Letrozole Breast Cancer Group. J Clin Oncol. 2001;19:2596–2606. | ||
Mouridsen H, Gershanovich M, Sun Y, et al. Phase III study of letrozole versus tamoxifen as first-line therapy of advanced breast cancer in postmenopausal women: analysis of survival and update of efficacy from the International Letrozole Breast Cancer Group. J Clin Oncol. 2003;21:2101–2109. | ||
Thurlimann B, Keshaviah A, Coates AS, et al. A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. N Engl J Med. 2005;353:2747–2757. | ||
Coates AS, Keshaviah A, Thurlimann B, et al. Five years of letrozole compared with tamoxifen as initial adjuvant therapy for postmenopausal women with endocrine-responsive early breast cancer: update of study BIG 1-98. J Clin Oncol. 2007;25:486–492. | ||
Ellis MJ, Coop A, Singh B, et al. Letrozole is more effective neoadjuvant endocrine therapy than tamoxifen for ErbB-1- and/or ErbB-2-positive, estrogen receptor-positive primary breast cancer: evidence from a phase III randomized trial. J Clin Oncol. 2001;19:3808–3816. | ||
Eiermann W, Paepke S, Appfelstaedt J, et al. Preoperative treatment of postmenopausal breast cancer patients with letrozole: a randomized double-blind multicenter study. Ann Oncol. 2001;12:1527–1532. | ||
Johnston S, Pippen J Jr, Pivot X, et al. Lapatinib combined with letrozole versus letrozole and placebo as first-line therapy for postmenopausal hormone receptor-positive metastatic breast cancer. J Clin Oncol. 2009;27:5538–5546. | ||
Schwartzberg LS, Franco SX, Florance A, O’Rourke L, Maltzman J, Johnston S. Lapatinib plus letrozole as first-line therapy for HER-2+ hormone receptor-positive metastatic breast cancer. Oncologist. 2010;15:122–129. | ||
Wolff AC, Lazar AA, Bondarenko I, et al. Randomized phase III placebo-controlled trial of letrozole plus oral temsirolimus as first-line endocrine therapy in postmenopausal women with locally advanced or metastatic breast cancer. J Clin Oncol. 2013;31:195–202. | ||
Baselga J, Semiglazov V, van DP, et al. Phase II randomized study of neoadjuvant everolimus plus letrozole compared with placebo plus letrozole in patients with estrogen receptor-positive breast cancer. J Clin Oncol. 2009;27:2630–2637. | ||
Finn RS, Crown JP, Lang I, et al. The cyclin-dependent kinase 4/6 inhibitor palbociclib in combination with letrozole versus letrozole alone as first-line treatment of oestrogen receptor-positive, HER2-negative, advanced breast cancer (PALOMA-1/TRIO-18): a randomised phase 2 study. Lancet Oncol. 2015;16:25–35. | ||
Martin M, Loibl S, von MG, et al. Phase III trial evaluating the addition of bevacizumab to endocrine therapy as first-line treatment for advanced breast cancer: the letrozole/fulvestrant and avastin (LEA) study. J Clin Oncol. 2015;33:1045–1052. | ||
Li N, Zheng RS, Zhang SW, et al. [Analysis and prediction of breast cancer incidence trend in China]. Zhonghua Yu Fang Yi Xue Za Zhi. 2012;46:703–707. Chinese. | ||
Zeng H, Zheng R, Zhang S, Zou X, Chen W. Female breast cancer statistics of 2010 in China: estimates based on data from 145 population-based cancer registries. J Thorac Dis. 2014;6:466–470. | ||
Chen W, Zheng R, Zeng H, Zhang S, He J. Annual report on status of cancer in China, 2011. Chin J Cancer Res. 2015;27:2–12. | ||
Yang H, Shi XF, Zhao YC. [Consumption of antineoplastic drugs in our hospital in 2001–2005]. China Pharmacy. 2007;18(5):331–333. Chinese. | ||
Du CX, Cai H, Ren DY. [Consumption of antineoplastic drugs in our hospital in 2006]. Sichuan J Cancer Control. 2007;3:168170. Chinese. | ||
Gui C, Liu GL. [Analysis of the medication on anticancer drugs in Shanghai sample hospitals from 2011 to 2013]. Drugs Clinic. 2015;12(2):28–32. Chinese. | ||
Hu LR, Fan F, Zhao T, Ding XM. [Cost and efficacy of domestic and imported Letrozole]. JiangXi Med J. 2011;46(4):362–364. Chinese. | ||
Jiang CM, Li GX, Zhao CY. [Domestic letrozole as an endocrine treatment of breast cancer: bioequivalence study of domestic and imported letrozole tablets]. Anti-tumor Pharm. 2014;4(4):302–308. Chinese. | ||
Chen JB. [Clinical observation of hormonal neoadjuvant treatment of tamoxifen and letrozole in postmenopausal breast cancer patients]. J Med Theory Practice. 2014;8:1069–1070. Chinese. | ||
Wu Y. [Comparison of letrozole with tamoxifen in hormonal neoadjuvant treatment of postmenopausal breast cancer patients]. Nei Mongol J Traditional Chinese. 2014;10:6–7. Chinese. | ||
Hou XL. [Comparative study of letrozole and tamoxifen in the neoadjuvant endocrinotherapy of breast cancer]. China Modern Doctor. 2012;28:48–49. Chinese. | ||
Lu S, Zhou W. [Clinical observation of letrozole in neoadjuvant endocrine therapy for elderly breast cancer]. Pract J Cancer. 2012;27(6):632–637. Chinese. | ||
Lu J, Li JR, Zhang LF, Wang Y, Zhang YY. [Efficacy of Neoadjuvant endocrinotherapy for postmenopausal patients with advanced breast cancer]. J Basic Clin Oncol. 2014;27(3):234–236. Chinese. | ||
Gong C, Chen Y, Jia WJ, Su FX. [Aromatase inhibitors neoadjuvant endocrine therapy for tamoxifen resistance in senile patients with locally advanced breast cancer]. Lingnan Mod Clin Surg. 2010;10(5):346–348. Chinese. | ||
Zhang M, Yan M, Lü H, Niu L, Zeng H, Cui S. [Efficacies of aromatase inhibitors in the treatment of hormone dependent metastatic breast cancer in postmenopausal women: a report of 148 cases]. Natl Med J China. 2015;22:1765–1767. Chinese. | ||
Regan MM, Neven P, Giobbie-Hurder A, et al. Assessment of letrozole and tamoxifen alone and in sequence for postmenopausal women with steroid hormone receptor-positive breast cancer: the BIG 1-98 randomised clinical trial at 8.1 years median follow-up. Lancet Oncol. 2011;12:1101–1108. | ||
Luo N. [Clinical Comparative study between sequential therapy of tamoxifen and letrozole with letrozole monotherapy for breast cancer]. Med Recap. 2015;18:3410–3412. Chinese. | ||
Han QX. [Combination of xeloda and letrozole in treating drug resistant advanced breast cancer]. Chin Phys. 2008;4(10):51–51. Chinese. | ||
Guo XQ, Zhang LQ, Jiang J, Xu SX, Shi YF. Combination of capecitabine in treating 40 cases of postmenopausal breast cancer patients with anthracycline-resistant. Pract Clin Med. 2008;11(9):70–71. Chinese. | ||
Liu DG, Guan ZZ, Song ST, et al. A clinical study of xeloda as second line treatment for patients with advanced breast cancer. Chin J Cancer. 2001;20(12):1405–1408. Chinese. | ||
Sun JB, Ren YH. [Effect of zoledronic acid combined with aromatizing enzyme inhibitors in the treatment for post-menopause breast cancer patients with bone metastasis]. J Qiqihar Univ Med. 2014;35(1):56–57. Chinese. | ||
Tang FL. [Effect of zoledronic acid combined with letrozole in the treatment for post-menopause breast cancer patients with bone metastasis]. Chinese Foreign Health Abstract. 2013;48:164–164. Chinese. | ||
Chen SQ, Liang HT, Zhou R. [Effect of letrozole combined with zoledronic acid in the treatment for post-menopause breast cancer patients with bone metastasis]. Ningxia Med J. 2012;34(9):923–924. Chinese. | ||
Deng SK, Tong XQ, Gan XM, Ming SF. [Improvement in life quality of postmenopausal women with breast cancer operation by zoledronic acid and letrozole]. China Pharm. 2014;5:801–804. Chinese. | ||
Coleman R, Boer R, Eidtmann H, et al. Zoledronic acid (zoledronate) for postmenopausal women with early breast cancer receiving adjuvant letrozole (ZO-FAST study): final 60-month results. Ann Oncol. 2013;24(2):398–405. | ||
Qu RW. [Combination of letrozole and pirarubicin in treating advanced breast cancer]. Chinese Commun Doctors. 2008;9(10):56–56. Chinese. | ||
Liu F, Cao DM. [Letrozole and paclitaxel plus cisplatin treatment for metastatic breast cancer]. Pract Pharm Clin Rem. 2014;17:44–46. Chinese. | ||
Ma HL. [Letrozole and paclitaxel plus cisplatin treatment for metastatic breast cancer]. China J Modern Drug Appl. 2014;8(16):153–154. Chinese. | ||
Klijin JG, Beex LV, Mauriac L. Combined treatment with buserelin and tamoxifen in premenopausal metastatic breast cancer: a randomized study. J Natl Cancer Inst. 2000;11(92):903–911. | ||
Hu XM, Ouyang QC. [Clinical observation on ovarian function castration combined aromatase inhibitor therapy for premenopausal metastatic breast cancer]. Chin J Med Guide. 2014;16(12):1494–1498. Chinese. | ||
Yang TT, Wang T, Bian L, et al. [Ovarian function castration combined with aromatase inhibitors in the treatment of metastatic breast cancer in premenopausal women]. Chin Clin Oncol. 2013;18(6):521–524. Chinese. | ||
Sun QY. [Clinical observation on goserelin plus letrozole treatment in high-risk breast cancer in premenopausal women]. Med Inform. 2015;28(9):206–206. Chinese. | ||
Yao SY, Xu BH, Li Q, et al. Goserelin plus letrozole as first- or second-line hormonal treatment in premenopausal patients with advanced breast cancer. Endocrine J. 2011;58(6):509–516. | ||
Chen G. [Hormonal neoadjuvant treatment with letrozole after radical mastectomy of breast cancer]. China J Pharm Econ. 2014;9:14–15. Chinese. | ||
Contractor KB, Kaur K, Rodrigues GS, Kulkarni DM, Singhal H. Male breast cancer: is the scenario changing? World J Surg Oncol. 2008;58(6):1–11. | ||
Gradishar W. Male breast cancer. In: Harris J, Lippman M, Morrow M, Osborne C, editors. Diseases of the Breast. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2000:661–667. | ||
Jin LB, Lu LJ, Kong L, et al. The 5-year incidence of male breast cancer in Southwest of China from 2007 to 2011. Chinese-German J Clin Oncol. 2013;12:524–527. | ||
Rodríguez JR, Quintela IP, Cortijo GP, Guerrero MB, Aranda E. Fulvestrant in advanced male breast cancer. Ann Oncol. 2009;20(11):1896–1897. | ||
Chen F, Qiu LZ. [Biological and clinical implications of aromatase inhibitors in early male breast cancer patients]. Natl Med J China. 2014;94(4):273–275. Chinese. | ||
Shen G, Song ST, Jiang ZF, Song ZW, Wei CZ, Wang T. [One case in treatment of advanced male breast cancer with castration plus letrozole]. Natl Med J China. 2004;84(3):202–202. Chinese. | ||
Zhang DX. [One case of breast cancer in elder male]. J Baotou Med College. 2008;24(3):247–256. Chinese. | ||
Wang T, Ye QN, Jiang ZF. [Long-term endocrine therapy-related adverse drug reactions in patients after breast cancer surgery and treatment strategies]. Adverse Drug React J. 2014;16(5):290–293. Chinese. | ||
Shan S. [Venlafaxine in treatment of hot flashes of postmenopausal women]. China Med News. 2005;20(3):9–9. Chinese. | ||
Xu RT. [Postmenopausal for drug treatment of menopause syndrome patients clinical analysis]. Seek Med Ask Med. 2013;7(11):134–134. Chinese. | ||
Duan YL, Zhao WH. [Treatment of menopause syndrome by vitamin E]. Clin Med. 1997;4:50–50. Chinese. | ||
Ren XM, Bian WH. [Treatment of side effect caused by letrozole with Chinese medicine]. Hum J Tradit Chin Med. 2011;27(6):67–68. Chinese. | ||
Guo HT, Qiao J. [Chinese treatment of side effects caused by Western medicine treatment of breast cancer]. Guangming J Chin Med. 2013;28:101–102. Chinese. | ||
Hao SF. [Clinical observation of Chinese medicine in combination of letrozole to treat advanced breast cancer]. Chin Arch Tradit Chin Med. 2004;22(11):2089–2089. Chinese. | ||
Finn RS, Crown JP, Lang I, et al. The cyclin-dependent kinase 4/6 inhibitor palbociclib in combination with letrozole versus letrozole alone as first-line treatment of oestrogen receptor-positive, HER2-negative, advanced breast cancer (PALOMA-1/TRIO-18): a randomised phase 2 study. Lancet Oncol. 2015;16:25–35. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.