Back to Journals » International Journal of General Medicine » Volume 15
Clinical Symptoms, Etiology and Prognosis of Acute Bilateral Posterior Circulation Cerebral Infarction
Authors Zhao Y, Han Y, Sun W, Zhang Y
Received 28 November 2021
Accepted for publication 21 February 2022
Published 10 March 2022 Volume 2022:15 Pages 2787—2793
DOI https://doi.org/10.2147/IJGM.S351560
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Yuan Zhao, Yanfei Han, Weidong Sun, Yongbo Zhang
Department of Neurology, Beijing Friendship Hospital, Capital Medical University, Beijing, People’s Republic of China
Correspondence: Yongbo Zhang, Tel +86 10-63139807, Email [email protected]
Background: Acute BPCCI was previously presented only as a case report. The prognosis of acute BPCCI is related to many factors, such as gender, age, NIHSS, Hypertension and so on. We first systematically analyzed the clinical symptoms, imaging, etiology and prognosis of acute BPCCI and identified a statistically significant factor.
Methods: A total of 72 acute BPCCI patients admitted to the Department of Neurology, Beijing Friendship hospital, Capital Medical University were included. The demographics, risk factors, clinical manifestations, National Institute of Health stroke scale (NIHSS) on admission, imaging findings, and the modified Rankin Scale (mRS) at the third month after onset were collected. The mRS score greater than 3 indicated poor prognosis. The factors affecting their prognosis were analyzed.
Results: We included 72 Chinese patients with acute BPCCI (82% male). The most common symptoms and signs of the patients were dizziness and unilateral limb weakness. Patients with acute BPCCI involving cerebellum accounted for 85% of the patients. The number of patients with large-artery atherosclerosis was 46 (64%), the number of patients with cardiogenic embolism was 12 (17%), and the number of patients with other causes and unknown causes was 14 (19%). After multivariate regression analyses, NIHSS score (odds ratio 0.725, 95% confidence interval 0.586– 0.896, P = 0.003) was closely related with the prognosis of acute BPCCI.
Conclusion: Our study found that the symptoms and signs of acute BPCCI were nonspecific and mainly depended on imaging diagnosis. Acute BPCCI involving cerebellum was the most common case of acute BPCCI. The main cause of acute BPCCI was large-artery atherosclerosis. NIHSS score is identified as a statistically significant factor. The higher NIHSS score on admission showed the worse prognosis. Therefore, an acute BPCCI patient with a high NIHSS score should be paid more attention at the time of diagnosis.
Keywords: BPCCI, prognosis, etiology, clinical symptoms
Introduction
Stroke is the main cause of long-term disability in adults and the second leading cause of death in the world. Posterior circulation cerebral infarction is a kind of cerebral infarction involving the vertebrobasilar system. About 20–25% of ischemic stroke occurs in the posterior circulation system.1–3 Since posterior circulation cerebral infarction affects the structure of posterior circulation brain (including brain stem, cerebellum, thalamus and temporal occipital region), the prognosis of acute posterior circulation cerebral infarction (PCCI) is poor, and the morbidity and mortality are high. In the past studies, acute BPCCI was presented only as a case report. However, systematic analysis of acute BPCCI was not shown in previous reports. In order to provide guidance for future clinical treatment of acute BPCCI, we analyzed factors that can indicate a patient’s prognosis at the time of diagnosis. In particular, we first systematically analyzed the clinical symptoms, imaging, etiology and prognosis of acute BPCCI.
Materials and Methods
This study was approved by the Ethics Committee of Beijing Friendship Hospital (2019-P2-244-01). This is a retrospective study, and all participants’ information is protected. The study does not involve personal privacy or commercial interests. It is difficult to trace the recruitment and sign informed consent, so ethics committee of Beijing Friendship Hospital agreed to waive informed consent in this clinical trial. All research programmes and procedures are carried out in accordance with the Helsinki declaration.
Selection and Grouping of Patients
Patients with acute cerebral infarction treated in neurology department of our hospital from March 2013 to August 2019 were selected by our retrospective study. The brain MRI, cerebrovascular examination including the cranio-cervical computed tomography angiography (CTA), the cranio-cervical magnetic resonance angiography (MRA) or digital subtraction angiography (DSA), cardiac examination including electrocardiogram (ECG), 24-hour Holter, transthoracic echocardiography or transesophageal echocardiography were collected. Inclusion criteria were: 1. the patients were confirmed as acute BPCCI by diffusion weighted image (DWI) of MRI; 2. acute BPCCI is defined as BPCCI within 7 days after the onset of the disease. Exclusion criteria were: 1. the location of acute cerebral infarction is unilateral or involving anterior circulation; 2. latrogenic or craniocerebral trauma with cerebral infarction; 3. other intracranial lesions (such as subdural hematoma, intracranial tumor), severe dementia; 4. bone and joint diseases affecting limb function; 5. sequelae of previous cerebral infarction; 6. demyelinating disease; 7. patients with incomplete examination; 8. patients received intravenous, arterial thrombolysis or intravascular treatment in the acute stage of cerebral infarction. We excluded patients who had received intravenous, arterial thrombolysis or intravascular treatment in the acute stage of cerebral infarction, as we considered those might affect the prognosis of patients.
NIHSS score on admission and mRS score at the third month after onset were recorded for all patients who met the criteria. The end point of the study was functional result assessed by mRS score at the third month after onset.
After the collection of the medical data, according to the postcirculation vascular dominance zone segmentation criteria used in New England Medical Center Posterior Circulation registry (NEMC-PCR),4 acute BPCCI patients were divided into 4 groups: (a) proximal territory group (b) middle territory group (c) distal territory group (d) mixed territory group. The proximal territory includes regions supplied by the intracranial VA (vertebral artery): the medulla oblongata and the PICA (posterior inferior cerebellar artery) supplied cerebellum. The middle territory includes brain regions supplied by the BA (basilar artery) up to its SCA (superior cerebellar artery) branches: the pons and the AICA (anterior inferior cerebellar artery)-supplied cerebellum. The distal territory includes regions supplied by the rostral BA, SCAs, PCAs (posterior cerebral arteries) and their penetrating branches: midbrain, thalamus, SCA-supplied cerebellum and PCA territories.1
Since there were many cases of cerebellar infarction, we made a further classification. According to whether bilateral cerebral infarction area involved cerebellum or not, acute BPCCI patients were divided into 4 groups: (a) bilateral cerebellar infarction group without other posterior circulation infarction, (b) bilateral cerebellar infarction group with other posterior circulation infarction, (c) unilateral cerebellar infarction group with infarction of other posterior circulation blood supply area on the opposite side, (d) bilateral posterior circulation group without involving cerebellum.
Cardiac Assessment
Our collected data include chest film or chest computed tomography (CT), 12 lead ECG, 24-hour Holter, transthoracic echocardiography. The main sources of cardiogenic emboli include:5 atrial fibrillation, prosthetic heart valves, intracardiac thrombus, myocardial infarction, mitral stenosis, atrial myxoma, dilated cardiomyopathy (ejection fraction less than 35%), left ventricular aneurysm and infective endocarditis. The rare sources of cardiogenic emboli include:5 patent foramen ovale, atrial septal aneurysm, recent, Spontaneous echo contrast, mitral valve prolapse, mitral annular calcification, calcific aortic stenosis and ventricular dyskinesia (ejection fraction more than 35%). Thoracic aortic emboli are defined as lesions with a thickness of more than 4.0 mm or irregular walls of 3.0 mm on the thoracic aortic arch.
Evaluation of Cerebral Vessels and Brain MRI
Sixty-seven patients just had results of CTA, and the other 5 of 72 patients just had results of MRA due to renal insufficiency. DSA was performed in 10 patients. All patients were examined by MRI. Brain MRI examinations were performed in a 3T scanner (Ingenia; Philips Healthcare, Best, The Netherlands) with a 15-channel phased-array head coil. A standardized stroke MRI protocol was used in all patients which included (1) transverse, coronal, and sagittal localizing sequences; (2) T1-weighted images; (3) T2-weighted images; (4) DWI; (5) fluid attenuated inversion recovery (FLAIR) images.
Etiological Classification of Cerebral Infarction
According to the clinical data, imaging data and the TOAST classification,6 we classified the causes of acute BPCCI as follow: (1) large-artery atherosclerosis (LAA) (the stenosis of atherosclerosis is greater than or equal 50% or occlusion corresponding to clinical manifestations, but excluding heart disease); (2) cardioembolism (there is no evidence of pericardial sclerosis of the great arteries and there is a potential source of cardiac emboli); (3) small-vessel occlusion has the risk factors of cerebrovascular disease, the maximum diameter of the lesion is less than 1.5cm, and there is no atherosclerotic stenosis, except for cardiogenic embolism; (4) stroke of other determined etiology which has rare causes of a stroke, such as vasculopathies, hematologic or coagulation disorders; (5) stroke of undetermined etiology which has more than two identified causes, unidentified causes, or incomplete evaluation.
Assessment of Prognosis
The end point of the study was functional result assessed by mRS score at the third month after onset. According to the mRS score, the prognosis was classified as no disability (mRS=0-1), mild disability (mRS = 2–3), severe disability (mRS = 4–5) and death (mRS = 6). The mRS score greater than 3 indicated poor prognosis.7
Statistical Analysis
Kruskal Wallis is used to test the normality of index. Mean is used for the quantitative data of normal distribution, and t-test method is used to compare the quantitative data of normal distribution between groups. The quantitative data of the non-normal distribution are expressed by median m (P25, P75). Wilcoxon signed rank test is used to compare the quantitative data of non-normal distribution between groups. Results are expressed as frequency for the qualitative data. The qualitative data were tested by chi-square test. Logistic regression analysis was used to evaluate the prognostic factors. The results were expressed by odds ratio (or) and 95% confidence interval (CI). All statistical results were expressed by bilateral P < 0.05. Statistical analyses were performed using the SPSS (version 23.0) statistical package.
Result
Clinical Symptom Analysis
In this study, 72 patients were enrolled, including 59 (82%) males with an average age of 63.05 ± 9.12 and 13 (18%) females with an average age of 72.24 ± 7.55. The average age of all patients was 64.71 ± 9.50. The average NIHSS score of all patients on admission was 3.81 ± 5.66. The risk factors include: history of hypertension (54 patients), smoking history (42 patients), history of diabetes (39 patients), history of hyperlipidemia (21 patients), history of cerebral infarction (16 patients) and history of coronary heart disease (11 patients). The symptoms or signs of onset were dizziness (38 patients), limb weakness (24 patients including 2 patients having bilateral limb weakness), dysarthria (14 patients), hemianopsia (7 patients), ataxia (6 patients), consciousness (6 patients), headache (4 patients), memory loss (2 patients) and visual deformation (1 patient).
Etiological Analysis
The number of patients with large-artery atherosclerosis was 46 (64%), the number of patients with cardiogenic embolism was 12 (17%), and the number of patients with other causes and unknown causes was 14 (19%). Thus, the main cause of acute BPCCI was large-artery atherosclerosis.
Analysis of Infarct Site
According to NEMC-PCR, 72 acute BPCCI patients were divided into 4 groups: (a) proximal territory group comprising 8 (11%) patients, (b) middle territory group comprising 6 (8%) patients, (c) distal territory group comprising 26 (36%) patients, (d) mixed territory group comprising 32 (45%) patients. The territory of acute BPCCI was mainly in the mixed territory, followed by the distal territory.
Further, according to whether bilateral cerebral infarction area involved cerebellum or not, acute BPCCI patients were divided into 4 groups: (a) bilateral cerebellar infarction group without other posterior circulation infarction comprising 9 (13%) patients, (b) bilateral cerebellar infarction group with other posterior circulation infarction comprising 20 (28%) patients, (c) unilateral cerebellar infarction group with infarction of other posterior circulation blood supply area on the opposite side comprising 32 (44%) patients, (d) bilateral posterior circulation group without involving cerebellum comprising 11 (15%) patients.
Patients with bilateral cerebellar infarction (a+b) accounted for 41% of patients with acute BPCCI. Patients with acute BPCCI involving cerebellum (a+b+c) accounted for 85% of patients with acute BPCCI.
Analysis of Factors Influencing Prognosis
We performed univariate and multivariate analysis to identify factors associated with the prognosis of acute BPCCI. Table 1 shows the result of the univariate analysis, and Table 2 shows the result of the multivariate analysis.
 |
Table 1 Factors Related to the Prognosis of BPCCI |
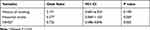 |
Table 2 Logistic Regression Analysis of Factors Related to the Prognosis of BPCCI |
The baseline data of two groups (good prognosis and poor prognosis) of acute BPCCI cases are shown in Table 1. The prognosis of acute BPCCI is related to many factors, such as gender, age, NIHSS, Hypertension and so on. In our study, gender, age, history of hypertension, diabetes, coronary heart disease, hyperlipidemia, hospitalization days, three causes of cerebral infarction and location of cerebral infarction were not statistically significant (P > 0.05). History of smoking (x2=4.157 p = 0.041), historical stroke (x2=5.493 p = 0.019) and NIHSS score on admission (Z=−3.498 p = 0.000) were statistically significant in the two groups in the univariate analysis (Table 1).
After adjusting the factors of history of smoking and historical stroke according to multivariate regression analysis, it was shown that the NIHSS score on admission (odds ratio 0.725, 95% Confidence Interval 0.586–0.896, P = 0.003) was closely related with the prognosis of acute BPCCI. Thus, the NIHSS score is identified as a statistically significant factor. The higher NIHSS score on admission showed the worse prognosis (Table 2).
Discussion
With the popularization of the brain MRI in China, more and more patients with acute BPCCI have been found. From March 2013 to August 2019, 2831 cases of acute cerebral infarction were treated in neurology department of our hospital, including 183 cases of acute bilateral cerebral infarction and 72 cases of acute BPCCI. The treated acute BPCCI patients accounted for 2.5% of the treated patients with acute cerebral infarction and 40% of the treated patients with acute bilateral cerebral infarction. Since the ratio of acute BPCCI to acute cerebral infarction is low, previous reports rarely described the clinical presentation, etiologic factors and prognosis of acute BPCCI. In particular, the reported cases of acute BPCCI were not systematically analyzed. Here, we first focused on the systematic analysis of acute BPCCI. In order to provide guidance for future clinical treatment of acute BPCCI, we systematically analyzed the clinical symptoms, imaging, etiology and prognosis of acute BPCCI.
In our study, 82% of the 72 patients were male. It was reported that men in the Arab world were most often victims of stroke (between 55.9% and 75%).8 In the NEMC-PCR, the patients of PCCI comprised 256 men (63%) and 151 women (37%).4 Two previous studies on bilateral cerebellar infarction showed that 85% and 64% of the patients were male, respectively.9,10 A report of PCCI from China showed that male patients accounted for 74.5%.11 The reason of the large proportion of male patients may be hormonal factors including estrogen, which seems to have protective effects on both the vascular and cerebral systems.8
We found that the most common symptoms and signs of acute BPCCI in our patients were dizziness and unilateral limb weakness. The symptoms and signs of acute BPCCI were not discussed in previous reports. However, it was reported that the most common signs of PCCI were unilateral limb weakness, facial paralysis, gait ataxia, dysarthria and nystagmus,1,3 and the most common symptoms were vertigo/dizziness, nausea, vomiting, headache and change of consciousness.1,3 Thus, we think that the common symptoms and signs of acute BPCCI are consistent with the common symptoms and signs of PCCI. The symptoms and signs of acute BPCCI are nonspecific, and it is difficult to distinguish acute BPCCI from PCCI only by observing symptoms and signs. Further, acute BPCCI can be identified by imaging examination.
Besides, we noticed that acute BPCCI involving cerebellum was the most common case (85%) of acute BPCCI, and acute BPCCI cases with bilateral cerebellar infarction accounted for 41% of cases with acute BPCCI. The cerebellum is supplied by 3 major vessels: posterior inferior cerebellar artery (PICA), anterior inferior cerebellar artery (AICA), and superior cerebellar artery (SCA). Strokes can occur in any of these vascular territories. Sometimes there is more than one vascular territory involved.12 Since the cerebellum has more major vessels for blood supply than other territories of posterior circulation, acute BPCCI is more likely to involve cerebellum than other territories of posterior circulation. It is reported that the prognosis of bilateral cerebellar infarction is worse than that of unilateral cerebellar infarction.9 In our study, the statistical result does not show that the prognosis of acute BPCCI involving bilateral cerebellum is worse than that of other acute BPCCI.
Further, we found that the most common cause of acute BPCCI was large-artery atherosclerosis in the study. The cause of acute BPCCI is related to the anatomical structure of the vertebrobasilar artery. The posterior circulation is mainly supplied by vertebrobasilar artery, and blood in the posterior circulation vessels at the distal end of the initial part of the basilar artery is all sent out from the basilar artery to both sides. Besides, there are some variations in the vascular distribution of the posterior circulation, and one side of the vessels supplies the other side through the midline. Due to the above anatomical structure of the vertebrobasilar artery, large-artery atherosclerosis became the most common cause of acute BPCCI.
Further, in our study, the territory of acute BPCCI was mainly the mixed territory, followed by the distal territory. This can be explained by the anatomical characteristics of the vertebrobasilar arterial system. Basilar artery (BA) originates at the pontomedullary junction by the union of the two VAs.1 It travels rostrally along the anterior surface of the medulla and the pons until it bifurcates into the two posterior cerebral arteries.1 Therefore, two or more territories may be involved if the basilar artery is atherosclerosis or embolism. The proximal territory includes regions supplied by the intracranial VA: the medulla oblongata and the PICA-supplied cerebellum. The middle territory includes brain regions supplied by the BA up to its SCA branches: the pons and the AICA-supplied cerebellum. The distal territory includes regions supplied by the rostral BA, SCAs, PCAs and their penetrating branches: midbrain, thalamus, SCA-supplied cerebellum and PCA territories. We think that acute BPCCI is related to the area of territory of blood supply. Since the mixed territory had the largest area and the distal territory had the second large area, the mixed territory and the distal territory were more affected than the proximal territory and the middle territory. Our result was similar to the large registry study from the United States, which suggested that infarcts most often include the distal territory in PCCI.3
Further, we found that the NIHSS score was a statistically significant factor, and the higher NIHSS score on admission showed the worse prognosis. Several studies showed that the NIHSS had limitations in the assessment of stroke severity in PCCI, because it was highly weighted toward deficits in anterior circulation cerebral infarction (ACCI) such as aphasia and hemiparesis, whereas signs of PCCI, including bulbar deficits and ataxia, received fewer points.13–16 However, our study showed that the NIHSS score on admission was closely related with the prognosis of acute BPCCI, as the P value of mean of the NIHSS score was smaller than 0.05 in statistics.
Our study has several limitations. We used 24-hour Holter and transthoracic echocardiography in our study. In order to improve the detection rate of cardiogenic embolism, we suggest that transesophageal echocardiography and 72 hour Holter can be used in the screening of cardiogenic emboli. Since the study was a retrospective study and had a relatively small number of cases, selection bias and recall bias may present in our study. In the future research, we should enlarge the sample size and carry out prospective research.
Conclusions
In summary, our study first systematically analyzed the clinical symptoms, imaging, etiology and prognosis of acute BPCCI. We found that the clinical manifestations and signs of acute BPCCI were nonspecific and mainly depended on imaging diagnosis. Acute BPCCI involving cerebellum was the most common case of acute BPCCI. In our study, the main cause (64%) of acute BPCCI was large-artery atherosclerosis. The territory of acute BPCCI was mainly in the mixed territory, followed by the distal territory. The NIHSS score is identified as a statistically significant factor. The higher NIHSS score on admission showed the worse prognosis. Therefore, we suggest that an acute BPCCI patient with a high NIHSS score should be paid more attention at the time of diagnosis.
Funding
This work was supported by the grants from National Natural Science Foundation of China (81671191; 81371355) and Beijing Natural Science Foundation (7082028).
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Sparaco M, Ciolli L, Zini A. Posterior circulation ischaemic stroke - a review part I: anatomy, aetiology and clinical presentations. Neurol Sci. 2019;40(10):1995–2006. doi:10.1007/s10072-019-03977-2
2. Sparaco M, Ciolli L, Zini A. Posterior circulation ischemic stroke - a review part II: imaging and acute treatment. Neurol Sci. 2019;40(10):2007–2015. doi:10.1007/s10072-019-03936-x
3. Merwick Á, Werring D. Posterior circulation ischaemic stroke. BMJ. 2014;348:g3175. doi:10.1136/bmj.g3175
4. Caplan LR, Wityk RJ, Glass TA, et al. New England Medical Center Posterior Circulation registry. Ann Neurol. 2004;56(3):389–398. doi:10.1002/ana.20204
5. Smajlović D. Strokes in young adults: epidemiology and prevention. Vasc Health Risk Manag. 2015;11:157–164. doi:10.2147/VHRM.S53203
6. Adams HP
7. Banks JL, Marotta CA. Outcomes validity and reliability of the modified Rankin scale: implications for stroke clinical trials: a literature review and synthesis. Stroke. 2007;38(3):1091–1096. doi:10.1161/01.STR.0000258355.23810.c6
8. Kharbach A, Obtel M, Lahlou L, et al. Ischemic stroke in Morocco: a systematic review. BMC Neurol. 2019;19(1):349. doi:10.1186/s12883-019-1558-1
9. Hong JM, Bang OY, Chung CS, et al. Frequency and clinical significance of acute bilateral cerebellar infarcts. Cerebrovasc Dis. 2008;26(5):541–548. doi:10.1159/000160211
10. Wang PQ, Ding ZG, Zhang GB, et al. A study on lesion pattern of bilateral cerebellar infarct. Eur Rev Med Pharmacol Sci. 2015;19(10):1845–1851.
11. Han Y, Xu M, Zhao Y, et al. Long-term outcome and prognostic factors of posterior circulation ischemia patients: results from a single center retrospective study. Vascular. 2020;28(1):25–30. doi:10.1177/1708538119866604
12. Datar S, Rabinstein AA. Cerebellar infarction. Neurol Clin. 2014;32(4):979–991. doi:10.1016/j.ncl.2014.07.007
13. Sarraj A, Medrek S, Albright K, et al. Posterior circulation stroke is associated with prolonged door-to-needle time. Int J Stroke. 2015;10(5):672–678. doi:10.1111/j.1747-4949.2012.00952.x
14. Sarikaya H, Arnold M, Engelter ST, et al. Outcomes of intravenous thrombolysis in posterior versus anterior circulation stroke. Stroke. 2011;42(9):2498–2502. doi:10.1161/STROKEAHA.110.607614
15. Libman RB, Kwiatkowski TG, Hansen MD, et al. Differences between anterior and posterior circulation stroke in TOAST. Cerebrovasc Dis. 2001;11(4):311–316. doi:10.1159/000047659
16. Förster A, Gass A, Kern R, et al. Thrombolysis in posterior circulation stroke: stroke subtypes and patterns, complications and outcome. Cerebrovasc Dis. 2011;32(4):349–353. doi:10.1159/000330346
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
