Back to Journals » Journal of Multidisciplinary Healthcare » Volume 15
Clinical Survey of Current Perioperative Body Temperature Management: What Major Factors Influence Effective Hypothermia Prevention Practice?
Authors Deng X, Yan J, Wang S , Li Y , Shi Y
Received 27 May 2022
Accepted for publication 29 July 2022
Published 8 August 2022 Volume 2022:15 Pages 1689—1696
DOI https://doi.org/10.2147/JMDH.S376423
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Xiaoqian Deng,1 Junyu Yan,2 Shaungwen Wang,3 Yifan Li,3 Yun Shi4
1Department of Anesthesiology, West China Hospital, Sichuan University and The Research Units of West China (2018RU012), Chinese Academy of Medical Sciences, Chengdu, People’s Republic of China; 2Department of Anesthesiology, Karamay Hospital of Integrated Traditional Chinese and Western Medicine, Karamay, People’s Republic of China; 3West China School of Medicine, Sichuan University, Chengdu, People’s Republic of China; 4Department of Anesthesiology, Children’s Hospital of Fudan University, Fudan University, Shanghai, People’s Republic of China
Correspondence: Yun Shi, Department of Anesthesiology, Children’s Hospital of Fudan University, Fudan University, 399 Wanyuan Road, Minhang District, Shanghai, 201102, People’s Republic of China, Email [email protected]
Purpose: Inadvertent intraoperative hypothermia (IIH) is generally associated with several postoperative complications. Inspite of the existing guidelines, the global incidence of IIH remains unacceptably high. Understanding the conditions that influence temperature management is critical for developing future interventions to improve the postoperative patient outcomes. This study aimed to identify the major factors that hinder the implementation of IIH prevention practices.
Methods: Through a literature research, pilot small-sample investigation, and expert suggestions, 11 factors that may hinder the implementation of IIH prevention practices were identified. A questionnaire was developed, and each question was used to assess each factor. After approval by the Research Ethics Board, the questionnaires were sent to the staff anaesthesiologists at two academic hospitals via WeChat. Each answer was coded according to the degree to which the factor was affected, as anticipated. Finally, the answers were analysed based on the 80/20 rule to identify the major barriers to effective temperature management.
Results: We included 195 participants. Knowledge, memory, attention and decision processes, beliefs about consequences, and environmental context and resources were the major factors, with cumulative composition ratios of 24%, 43.4%, 57.7%, and 70.7%, respectively. Meanwhile, behavioural regulation and social influence were the secondary factors, with cumulative composition ratios of 80.4% and 87.5%, respectively. Reinforcement, confidence in capacity, duty realisation, skills, and intention were the general factors with cumulative composition ratios of 94.3%, 99.8%, 100%, 100%, and 100%, respectively.
Conclusion: Four factors–knowledge, memory, attention and decision process, beliefs about consequences, and environmental context and resources–were the major factors that influence the effective hypothermia prevention practice.
Relevance to Clinical Practice: These major factors will be used in further studies as a basis to develop the corresponding solutions and improve the patient outcomes in clinical practice.
Keywords: intraoperative hypothermia, body temperature, temperature management, 80/20 rule
Introduction
Inadvertent intraoperative hypothermia (IIH) is defined as a core temperature lower than 36°C. IIH is one of the most prevalent events faced by anaesthesiologists, with a current prevalence of 20%–70%,1–4 even up to 90% decades ago.5,6 It is a risk factor for a series of postoperative complications, including bleeding and blood product transfusion,7,8 cardiovascular events,9,10 postoperative infection,10,11 shivering,12 drug metabolism disorder,13 prolonged stay in the postanaesthetic recovery unit14 and increased length of hospital stay,10,11,15 etc. All of these unfavourable consequences lead to increased hospitalisation expense,16–18 patient discomfort, and complains.7,15 Thus, it has been recommended and incorporated into the clinical anaesthesia practice to maintain a normal intraoperative body temperature.19
Along with the awareness of the adverse outcomes of hypothermia, an increasing number of studies have investigated the effective and feasible methods to prevent IIH,20 including use of prewarming device,21 use of monitor devices, application of passive and active warming methods,22 implementation of supportive heat-conserving measures, and recognition of the specific risk factors for IIH.23 Different countries have published evidence-based guidelines to preserve the intraoperative body temperature.24–28 However, the prevalence of IIH remains unacceptably high, with an average of 40–55% in advanced countries across Europe,25 Australia,4,29 and the United States.7,10 This is similar the situation in China. The incidence of IIH in adult patients who underwent elective surgery is 39%–44.3%,30 as reported in two multicentre prospective observational studies that were recently conducted in 29 hospitals in Beijing and 28 major teaching hospitals in China, representing the best clinical practice and healthcare resources in China.
Obviously, decreasing the incidence of IIH and improving the quality of healthcare are urgently needed. However, a large gap exists between guideline implementation and the intended clinical outcome. Eleven factors were found to influence the IIH prevention in clinical practice.31,32 Hence, the specific improvement measures will be developed if the most influential factors are identified.
The 80/20 rule was proposed by Italian economist Vilfredo Pareto at the beginning of the 20th century.33 According to this rule, 20% of the problems are the main reasons for 80% of serious adverse consequences. This principle is often used in hospital management to identify the primary factors that cause adverse consequences and thus establish the most effective improvement measures.34,35 This survey aimed to investigate the current intraoperative body temperature management to identify the primary factors that will be targeted in order to make changes and improvements in clinical anaesthesia practice, based on the 80/20 rule.
Methods
Design
A qualitative study, using an online questionnaire, was conducted to identify the major factors that hinder individuals from performing effective temperature management. Eleven factors (knowledge, social influence, environmental context and resources, memory, attention and decision process, beliefs about consequences, reinforcement, behavioural regulation, skills, confidence of capacity, duty realisation, and intention) were investigated, with each questionnaire item containing two to three questions. Most questions were designed as required choice questions, whereas others were designed as optional short questions.
Participants and Recruitment
The study was conducted at the Children’s Hospital of Fudan University (CHOFU) and the West China Hospital of Sichuan University (WCHSU). All staff anaesthesiologists were recruited for the study. The questionnaires were sent out between January 1, 2021 and March 15, 2021 using a web-based platform (WenjuanXing). Only the completed questionnaires were included in the analysis.
Analysis
The participants were required to answer whether they were affected by the listed factors when they developed temperature management strategies. The factor was scored depending on the extent to which the participants were affected. Scores of 3, 2, 1, and 0 indicated always, often, occasionally, or never, respectively. All factors were sorted in descending order. The composition percentage and cumulative composition percentages were calculated in this order. According to the 80/20 rule, the factors with a cumulative composition percentage of 0–80% are the major factors, the factors with a cumulative composition percentage of 80–90% are the secondary factors, and the factors with a cumulative composition percentage of 90–100% are the general factors.
Results
Participant Characteristics
A total of 231 invitations to participate were sent, but only 195 (84.4%) participants completed the questionnaires, which were all included in the analysis. Forty-two participants were recruited from the CHOFU, while 153 were recruited from the WCHSU. The participants’ characteristics are listed in Table 1.
 |
Table 1 Characterizations of Participants. CHOFU, Children’s Hospital of Fudan University, WCHFU, West China Hospital, Sichuan University |
Findings
Major Factors
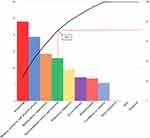
The factors were sorted in descending order: knowledge, memory, attention and decision process, beliefs about consequences, environmental context and resources, behavioural regulation, social influence, reinforcement, confidence in capacity, duty realisation, skills, and intention (Figure 1). Knowledge, memory, attention and decision processes, beliefs about consequences, environmental context, and resources were the major factors, with cumulative composition ratios of 24%, 43.4%, 57.7%, and 70.7%, respectively.
In this study, 159 (81.5%) participants were aware of the side effects of IIH, 69% of whom had unfavourable clinical outcomes. The three most concerning issues were delays in postanaesthetic care unit (58%), coagulation disorders (39%), and postoperative infection (22%). Other concerning issues were as follows: acidosis, shivering, insufficient oxygen supply, cardiac events, and postoperative nausea and vomiting. However, 101 (51.8%) participants did not know how to identify an IIH, 46% recognised that a lower temperature indicates hypothermia, and 12% even considered a temperature of 34°C as the threshold. Furthermore, 158 participants (81%) were not familiar of any guidelines for temperature management.
A total of 186 (95.4%) participants reported that they sometimes neglect the need for preventing hypothermia. Performance of emergency surgeries, patient handover, and caring for more than one patient were the primary situations that made 118 (60.5%), 116 (59.5%), and 93 (47.7%) participants, respectively, neglect the need to implement temperature management strategies.
Only 79 (40.5%) participants were convinced that their temperature management strategies could influence the clinical outcomes. Meanwhile, fewer participants (24, 12.3%) believed that their clinical practice would affect the patient’s body temperature.
A total of 193 (99.0%) participants reported that their temperature management strategies might not be effective owing to the environmental context and the insufficiency of resources. Moreover, 64 (32.8%), 52 (26.7%), and 50 (25.6) participants reported shortage of temperature monitors, warmed surgical dressing, and forced-air warming devices, respectively.
Only 25 (12.8%) participants frequently monitored their body temperature and performed it as a daily routine. A total of 141 (72.3%) participants reported that they only paid attention to patients who were at high risk of IIH. Of these, 100 (71%) illustrated a high risk of IIH. The three most frequently referred high-risk factors were major surgery (68, 68%), patients’ age (41, 41%), and room temperature (31, 31%). Only three (1.5%) participants proposed that failure to implement hypothermia prevention in clinical practice was also a high-risk factor for IIH.
Secondary Factors
Behavioural regulation and social influence were the secondary factors, with cumulative composition ratios of 80.4% and 87.5%, respectively.
Exactly 126 (64.6%) participants reported that public lectures were frequently launched at their institutes. However, only 25 (12.8%) participants reported the standardisation of temperature management practices in the department.
A total of 154 (79.0%) participants reported some resistance from their team members, which hindered their temperature management practice. The frequently mentioned team members were surgeons, followed by operating nurses, as reported by 141 (72%) and 64 (32.8%) participants, respectively.
General Factors
Reinforcement, confidence in capacity, duty realisation, skills, and intention were the general factors with cumulative composition ratios of 94.3%, 99.8%, 100%, 100%, and 100%, respectively.
IIH was complained and recorded when it occurred as reported by 177 (90.7%) and 129 (66.2%) participants, respectively. A total of 147 (75.4%) participants always or often felt confident in their capacity to perform temperature management. A total of 184 participants took more than three measures to protect body temperature. The three frequently used devices included forced-air warming devices, water-filled mattresses, and electric warming blankets.
Discussion
To our knowledge, IIH is one of the most common adverse events related to surgery owing to the large gap between guideline implementation and the intended clinical outcomes. Many factors affect the anaesthesiologists when they develop temperature management strategies, such as knowledge, environmental context and resources, skills, etc.31,32 Undoubtedly, great progress will be made if measures are taken to improve these factors. However, we aimed to use the “Pareto rule” to understand the contradiction and identify the primary reason for the poor temperature management so that close attention can be paid to resolving them. However, the result is not always the same, because the contradiction is not consistent. If the main contradiction is solved by certain means, new major contradictions will appear. Therefore, it does not only imply that these major factors should be improved, and that the other factors can have a positive effect on temperature management without improving them; rather, when these contradictions are alleviated, other problems may become the primary contradictions; hence, the Pareto rule can be used to identify them and finally improve the temperature management and patient clinical outcomes.
For this purpose, the 11 factors that were widely accepted to affect the implementation of body temperature management were determined based on literature research, a previous pilot investigation, and expert suggestions. Second, a questionnaire composed of 28 items was developed, with 1–2 items corresponding to each factor. Knowledge refers to the awareness of the existence of something, including the definition of hypothermia and temperature management guidelines. Social influence is an interpersonal process that may change an individual’s thoughts, feelings, or decisions. Environmental context and resources refer to the apparatus and materials. Memory, attention, and decision process refer to the ability of an individual to retain focus and choose between two or more alternatives. Beliefs of consequences refer to the belief in the reality of the outcomes of a given situation. Reinforcement refers to the dependent relationship between a response and a given behaviour to increase the probability of the response. Behavioural regulation refers to the rules that aim to manage or change a certain behaviour. Skills refer to an individual’s ability. Confidence in capacity refers to the beliefs about the validity of the ability. Duty realisation refers to the awareness of personal duties in a work setting. Intention refers to the personal subjective willingness to take action. After a pilot test and minor revisions, the questionnaires were sent to the Department of Anesthesiology at the two institutes. Data were collected and analysed using the 80/20 rule. The questionnaire survey was aimed at determining the primary factors that prevent participants from managing temperature effectively. These factors were the most urgent and effective in improving the quality of our clinical practice.
In our study, knowledge, memory, attention and decision processes, beliefs about consequences, environmental context, and resources were the major factors. Behavioural regulation and social influence were the secondary factors. Reinforcement, confidence in capacity, duty realisation, skills, and intentions were the general factors.
Most participants were aware of the side effects of IIH (knowledge). They considered themselves responsible for maintaining normothermia (duty realisation), and they were also willing to make efforts to achieve (intention). However, we found that most participants did not read any guidelines for managing IIH, which was also reported in other study.31,32 They did not know how to identify an IIH (knowledge) and usually used a lower threshold temperature. Thus, they underestimated the incidence and side effects of IIH; they might aim a lower temperature goal when managing patients with IIH. Several guidelines have been published in different countries.24–27 Hence, it is easy to identify the risk factors, temperature management strategies, prevention methods, etc. based on these guidelines. Thus, it is important for clinical workers to read the guidelines in details.19
One of the most important findings of our survey is that most anaesthesiologists do not routinely measure or monitor a patient’s body temperature (memory, attention, and decision process), although all of them know that IIH will lead to adverse health outcomes (knowledge). However, most anticipants only measure or monitor the body temperature of a high-risk patient. The three most important risk factors were reported to be major surgery, patient’s age, and room temperature. These participants tended to pay attention to temperature management depending on the inherent characteristics of surgery and the patient. Certainly, these factors increase the risk of IIH.36 However, anaesthesia itself and the inability to take appropriate measures to prevent IIH are also important risk factor,37 which were only proposed by three participants. Moreover, a high-risk patient is indicated for passive or positive warming measures rather than for body temperature monitoring. It is clearly recommended in some guidelines that the body temperature of all patients should be measured or monitored.28,38 This is the only method to detect IIH, and is quick, objective, and convenient. Active or passive warming methods should be used when high-risk patients are identified. This also indicates that unfamiliarity with the guidelines (knowledge) impacts clinical practice (memory, attention, and decision processes). However, since it is not a routine practice, these anticipants admit that they sometimes forget to manage the patient’s temperature, depending on their emotions and working conditions (attention, memory, and decision processes). The Chinese Anesthesiologists Association reported that the average number of anaesthesiologists per 1,0000 Chinese individuals was 0.5, while the average numbers of anaesthesiologists were 2.5 in the United States and 2.8 in the United Kingdom. In this situation, many anticipants do not take much time or energy to think about the temperature management practice, or even forget to manage the patient’s temperature. In our study, participants reported that they often neglect the need to manage the patient’s temperature during emergency situations patient handovers, or when caring for more than one patient. However, this did not justify the absence of temperature monitoring or management. On the contrary, awareness of the high prevalence and wide range of complications of IIH (knowledge), beliefs about the validity of the outcomes (beliefs of consequences), and using temperature as a routine monitoring index (behavioural regulation) can compensate for the oversight due to work overload.
In addition to these two factors, we also found two important factors that prevent anaesthesiologists from managing temperature effectively. A shortage of materials and apparatus (environmental context and resources) is an objective factor. Although the survey was conducted in two high-ranking academic hospitals in China, insufficient materials and apparatus remain problematic. More anaesthesiologists in primary hospitals are affected when they are developing temperature management strategies. They are willing to take responsibility of performing temperature management (duty realisation), to ensure that the patient’s temperature is maintained (intention), and to implement appropriate prevention methods (skills); however, it is still difficult to reach an optimal outcome if the health resources are limited. Another subjective factor is that the participants were unsure whether their temperature management strategy will affect the body temperature and clinical outcomes (beliefs about consequences), although most participants know the side effects of IIH (knowledge) and how to manage it (skills). This is probably due to several reasons. 1) The participants were all anaesthesiologists who were not usually responsible for managing postoperative complications (reinforcement). 2) They encountered problems in achieving successful temperature outcomes, such as insufficient materials and equipment (environmental context and resources), and team cooperation (social influence). If the participants are not sure of the positive consequences of active temperature protection, it will certainly steer the decision-making process, especially when they have to face and resolve the abovementioned problems.
Interestingly, good teamwork (social influence), especially that between surgeons, is a secondary factor. Most surgeons do not like using a forced-air device before the patient is prepped and draped, which are usually time consuming.31,32 Similarly, in our institute, many surgeons refuse to set the temperature to >26°C. However, this temperature may still be too low, which is related to the high incidence of IIH in certain populations, such as neonates.39 Temperature management might fail due to poor team cooperation.29,40
Conclusion
In this study, knowledge, memory, attention and decision processes, beliefs about consequences, and environmental contexts and resources were the major factors that had the greatest influence on the anaesthesiologists’ hypothermia prevention practices. Hence, more efforts and measures should be implemented to improve these areas.
Data Sharing Statement
The datasets generated in the study are available from the corresponding author upon reasonable request.
Ethical Approval and Informed Consent
This study was approved by the research ethics boards of the two institutes. It was also registered at www.chictr.org.cn (registration number: ChiCTR2100042565). Signed informed consent was obtained from all participants. All participants volunteered to participate and could withdraw from the study at any time. Participants were informed that their personal information would be kept confidential. De-identified data were stored in a locked cabinet in the laboratory.
Funding
This study was funded by the National Natural Science Foundation of China (no. 72074162).
Disclosure
The authors declare that they have no conflict of interest.
References
1. Leijtens B, Koëter M, Kremers K, Koëter S. High incidence of postoperative hypothermia in total knee and total Hip arthroplasty: a prospective observational study. J Arthroplasty. 2013;28(6):895–898. doi:10.1016/j.arth.2012.10.006
2. Burns SM, Piotrowski K, Caraffa G, Wojnakowski M. Incidence of postoperative hypothermia and the relationship to clinical variables. J Perianesth Nurs. 2010;25(5):286–289. doi:10.1016/j.jopan.2010.07.001
3. Healy K, O’Sullivan A, McCarthy L. A nurse-led audit on the incidence and management of inadvertent hypothermia in an operating theatre department of an Irish hospital. J Perioper Pract. 2019;29(3):54–60. doi:10.1177/1750458918793295
4. Jed Duff KW, Edward K-L, Williams R, Sutherland-Fraser S. Incidence of perioperative inadvertent hypothermia and compliance with evidence-based recommendations at four Australian hospitals: a retrospective chart audit. Acorn. 2014;27(3):16–23.
5. Burger L, Fitzpatrick J. Prevention of inadvertent perioperative hypothermia. Br J Nurs. 2009;18(18):1114, 6–9. doi:10.12968/bjon.2009.18.18.44553
6. Tappen RM, Andre SP. Inadvertent hypothermia in elderly surgical patients. Aorn j. 1996;63(3):639–644. doi:10.1016/S0001-2092(06)63411-X
7. Sun Z, Honar H, Sessler DI, et al. Intraoperative core temperature patterns, transfusion requirement, and hospital duration in patients warmed with forced air. Anesthesiology. 2015;122(2):276–285. doi:10.1097/ALN.0000000000000551
8. Rajagopalan S, Mascha E, Na J, Sessler DI. The effects of mild perioperative hypothermia on blood loss and transfusion requirement. Anesthesiology. 2008;108(1):71–77. doi:10.1097/01.anes.0000296719.73450.52
9. Frank SM, Fleisher LA, Breslow MJ, et al. Perioperative maintenance of normothermia reduces the incidence of morbid cardiac events. A randomized clinical trial. Jama. 1997;277(14):1127–1134.
10. Scott AV, Stonemetz JL, Wasey JO, et al. Compliance with Surgical Care Improvement Project for body temperature management (SCIP Inf-10) Is associated with improved clinical outcomes. Anesthesiology. 2015;123(1):116–125. doi:10.1097/ALN.0000000000000681
11. Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med. 1996;334(19):1209–1215. doi:10.1056/NEJM199605093341901
12. National Collaborating Centre for N, Supportive C. National Institute for Health and Clinical Excellence: Guidance. The Management of Inadvertent Perioperative Hypothermia in Adults. London: Royal College of Nursing (UK) Copyright © 2008, National Collaborating Centre for Nursing and Supportive Care; 2008.
13. Leslie K, Sessler DI, Bjorksten AR, Moayeri A. Mild hypothermia alters propofol pharmacokinetics and increases the duration of action of atracurium. Anesth Analg. 1995;80(5):1007–1014. doi:10.1097/00000539-199505000-00027
14. Becerra A, Valencia L, Saavedra P, Rodriguez-Perez A, Villar J. Effect of prewarming on body temperature in short-term bladder or prostatic transurethral resection under general anesthesia: a randomized, double-blind, controlled trial. Sci Rep. 2021;11(1):20762. doi:10.1038/s41598-021-00350-2
15. Doufas AG. Consequences of inadvertent perioperative hypothermia. Best Pract Res Clin Anaesthesiol. 2003;17(4):535–549. doi:10.1016/S1521-6896(03)00052-1
16. Mahoney CB, Odom J. Maintaining intraoperative normothermia: a meta-analysis of outcomes with costs. Aana j. 1999;67(2):155–163.
17. Wong PF, Kumar S, Bohra A, Whetter D, Leaper DJ. Randomized clinical trial of perioperative systemic warming in major elective abdominal surgery. Br J Surg. 2007;94(4):421–426. doi:10.1002/bjs.5631
18. Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307(14):1513–1516. doi:10.1001/jama.2012.362
19. Hopf HW. Perioperative temperature management: time for a new standard of care? Anesthesiology. 2015;122(2):229–230. doi:10.1097/ALN.0000000000000552
20. Wang R, Ping FM, Liu YM, et al. Effect of competence health cultivation on the prevention and control of inadvertent perioperative hypothermia. Rev Assoc Med Bras. 2020;66(7):924–930. doi:10.1590/1806-9282.66.7.924
21. Becerra A, Valencia L, Villar J, Rodriguez-Perez A. Short-periods of pre-warming in laparoscopic surgery. A non-randomized clinical trial evaluating current clinical practice. J Clin Med. 2021;10(5):1047. doi:10.3390/jcm10051047
22. Yoo JH, Ok SY, Kim SH, et al. Efficacy of active forced air warming during induction of anesthesia to prevent inadvertent perioperative hypothermia in intraoperative warming patients: comparison with passive warming, a randomized controlled trial. Medicine. 2021;100(12):e25235. doi:10.1097/MD.0000000000025235
23. Liu M, Qi L. The related factors and countermeasures of hypothermia in patients during the anesthesia recovery period. Am J Transl Res. 2021;13(4):3459–3465.
24. Forbes SS, Eskicioglu C, Nathens AB, et al. Evidence-based guidelines for prevention of perioperative hypothermia. J Am Coll Surg. 2009;209(4):492–503.e1. doi:10.1016/j.jamcollsurg.2009.07.002
25. Torossian A, Bräuer A, Höcker J, Bein B, Wulf H, Horn EP. Preventing inadvertent perioperative hypothermia. Dtsch Arztebl Int. 2015;112(10):166–172. doi:10.3238/arztebl.2015.0166
26. Rehberi IP. The Turkish Anaesthesiology and Reanimation Society Guidelines for the prevention of inadvertent perioperative hypothermia. Turk J Anaesthesiol Reanim. 2013;41(5):188–190. doi:10.5152/TJAR.2013.64
27. National Institute for H, Care E. Addendum to Clinical Guideline CG65, Inadvertent Perioperative Hypothermia. London: National Institute for Health and Care Excellence (UK) Copyright © National Institute for Health and Care Excellence; 2016.
28. Calvo Vecino JM, Casans Frances R, Ripolles Melchor J, et al. Clinical practice guideline. Unintentional perioperative hypothermia. Rev Esp Anestesiol Reanim. 2018;65(10):564–588. doi:10.1016/j.redar.2018.07.006
29. Munday J, Hines SJ, Chang AM. Evidence utilisation project: management of inadvertent perioperative hypothermia. The challenges of implementing best practice recommendations in the perioperative environment. Int J Evid Based Healthc. 2013;11(4):305–311. doi:10.1111/1744-1609.12035
30. Yi J, Lei Y, Xu S, et al. Intraoperative hypothermia and its clinical outcomes in patients undergoing general anesthesia: national study in China. PLoS One. 2017;12(6):e0177221. doi:10.1371/journal.pone.0177221
31. Munday J, Delaforce A, Forbes G, Keogh S. Barriers and enablers to the implementation of perioperative hypothermia prevention practices from the perspectives of the multidisciplinary team: a qualitative study using the Theoretical Domains Framework. J Multidiscip Healthc. 2019;12:395–417. doi:10.2147/JMDH.S209687
32. Boet S, Patey AM, Baron JS, et al. Factors that influence effective perioperative temperature management by anesthesiologists: a qualitative study using the Theoretical Domains Framework. Can J Anaesth. 2017;64(6):581–596. doi:10.1007/s12630-017-0845-9
33. Harvey HB, Sotardi ST. The pareto principle. J Am Coll Radiol. 2018;15(6):931. doi:10.1016/j.jacr.2018.02.026
34. Lovse L, Poitras S, Dobransky J, Huang A, Beaule PE. Should the pareto principle be applied as a cost savings method in hip and knee arthroplasty? J Arthroplasty. 2019;34(12):2841–2845. doi:10.1016/j.arth.2019.07.034
35. Liu X, Lu H, Wang Y, et al. Factors affecting patient satisfaction with ecdemic medical care: a cross-sectional study in Nanchang, China. Patient Prefer Adherence. 2018;12:1373–1382. doi:10.2147/PPA.S167244
36. Macario A, Dexter F. What are the most important risk factors for a patient’s developing intraoperative hypothermia? Anesth Analg. 2002;94(1):215–220. doi:10.1097/00000539-200201000-00042
37. Yi J, Xiang Z, Deng X, et al. Incidence of inadvertent intraoperative hypothermia and its risk factors in patients undergoing general anesthesia in Beijing: a prospective regional survey. PLoS One. 2015;10(9):e0136136. doi:10.1371/journal.pone.0136136
38. Croke L. Guideline for prevention of hypothermia. AORN J. 2019;110(1):P8–P10. doi:10.1002/aorn.12761
39. Duryea EL, Nelson DB, Wyckoff MH, et al. The impact of ambient operating room temperature on neonatal and maternal hypothermia and associated morbidities: a randomized controlled trial. Am J Obstet Gynecol. 2016;214(4):505e1- e7. doi:10.1016/j.ajog.2016.01.190
40. Tveit C, Belew J, Noble C. Prewarming in a pediatric hospital: process improvement through interprofessional collaboration. J Perianesth Nurs. 2015;30(1):33–38. doi:10.1016/j.jopan.2014.01.008
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.