Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 15
Clinical Retrospective Analysis of 243 Patients with Rhinofacial Ulcers
Authors Ma W , Zhan R , Sui C, Zhou F, Liu H, Zhang X, Ruan Z, Wang Y, Cai X
Received 27 April 2022
Accepted for publication 14 July 2022
Published 1 August 2022 Volume 2022:15 Pages 1475—1483
DOI https://doi.org/10.2147/CCID.S371029
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Weiyuan Ma,1 Ruyu Zhan,2 Changlin Sui,3 Fushan Zhou,2 Haidong Liu,4 Xiuwen Zhang,5 Zhenqiang Ruan,6 Yukun Wang,7 Xiaolan Cai8
1Department of Dermatology, Affiliated Hospital of Weifang Medical University, Weifang, Shandong, People’s Republic of China; 2Scientific Research Center, Anxi County Hospital, Quanzhou, Fujian, People’s Republic of China; 3Department of Dermatology, Yantai Yuhuangding Hospital, Yantai, Shandong, People’s Republic of China; 4Department of Dermatology, Liaocheng People’s Hospital, Liaocheng, Shandong, People’s Republic of China; 5Department of Dermatology, Weihai Municipal Hospital, Weihai, Shandong, People’s Republic of China; 6Department of Dermatology, Jinan Dermatosis Prevention and Control Hospital, Jinan, Shandong, People’s Republic of China; 7Department of Dermatology, Qilu Hospital of Shandong University, Jinan, Shandong, People’s Republic of China; 8Department of Otolaryngology, Qilu Hospital of Shandong University, Jinan, Shandong, People’s Republic of China
Correspondence: Weiyuan Ma, Department of Dermatology, Affiliated Hospital of Weifang Medical University, Weifang, Shandong, People’s Republic of China, Email [email protected]
Purpose: The clinical and pathological data of patients with rhinofacial ulcers were retrospectively reviewed and analyzed to lay the foundation for standardized clinical treatment.
Patients and Methods: We retrospectively analyzed the clinical data, etiology, pathological features, treatment methods, and prognosis of 243 patients with rhinofacial ulcers treated in the Departments of Otorhinolaryngology and Dermatology at six hospitals in Shandong Province, China from July 2014 to October 2021. The clinical characteristics and treatment methods of the rhinofacial ulcers were summarized to provide a basis for standardizing patients’ diagnosis and treatment.
Results: The male-to-female ratio of the 243 patients was 2.04:1, and their ages ranged from 25 to 91 years. The most common sites were the cheek, nasal dorsum, and upper lip. The common primary diseases were basal-cell carcinoma, squamous-cell carcinoma, and odontogenic fistula, but rare triggers played important roles in some cases, such as infection, autoimmune diseases, and adverse drug reactions. Surgical treatment was feasible for tumor ulcers; 71 patients with basal-cell carcinoma and 50 with squamous-cell carcinoma were treated with Mohs micrographic surgery. During the follow-up period of 1– 84 months, most of the rhinofacial ulcers were cured, while natural killer/T-cell lymphoma, angiosarcoma, and melanoma were important causes of death.
Conclusion: Various causes may lead to rhinofacial skin ulcers, and some cases lacking specificity of clinical manifestations are easily misdiagnosed in clinical practice. Histopathological biopsy is valuable for confirming the diagnosis, after which correct etiological treatment is very important.
Keywords: skin, diagnosis, treatment, otorhinolaryngology, dermatology
Introduction
Skin and mucosal ulcers are localized defects and ulcers on the skin and mucosal surfaces caused by various factors. The surface of an ulcer is often covered with pus, necrotic tissue, or crust, and scars are often left after healing. Skin and mucous membrane ulcers can develop from primary skin and mucous membrane tumors, lymphopoietic tumors involving the skin and mucous membranes, inflammatory diseases, and various infections.1 Skin ulcers can also develop throughout the body. Facial ulcers are uncommon, but are often misdiagnosed and mistreated. Neoplastic ulcers, such as squamous-cell carcinoma and natural killer (NK)/T-cell lymphoma, and infectious ulcers, eg, mucormycosis, delay the opportune treatment time, which seriously affects the physical and mental health of patients and even endangers their lives.2–4 Therefore, it is necessary to detail the characteristics of rhinofacial ulcers to alert clinicians.
In this study, we retrospectively summarized and analyzed the clinical data of 243 patients with rhinofacial ulcers treated at multiple hospitals in Shandong Province, China, with the aims of exploring the common etiology, clinical manifestations, treatment methods, and prognosis of rhinofacial skin ulcers in Shandong province and to providing a basis for the clinical diagnosis and treatment of rhinofacial skin ulcers.
Materials and Methods
Ethics Statements
This study was approved by the Ethics Committee of the Affiliated Hospital of the Weifang Medical University and conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all the patients before the commencement of the study.
Study Design and Population
This retrospective study included 243 patients who were diagnosed with rhinofacial ulcers at the Departments of Otorhinolaryngology and Dermatology of the Affiliated Hospital of Weifang Medical University, Yantai Yuhuangding Hospital, Liaocheng People’s Hospital, Weihai Municipal Hospital, Jinan Dermatosis Prevention and Control Hospital and Qilu Hospital of Shandong University between July 2014 and October 2021. All patients underwent histopathological examination of the skin. For patients with tumors and infections, a histopathological examination was performed, and further immunohistochemistry and pathogenic microbiological examinations were performed to confirm the diagnosis. All patients with odontogenic fistulas underwent panoramic dental radiography. Patients diagnosed with malignant tumors were further subjected to cervical ultrasonography and enhanced computed tomography to exclude the possibility of lymph node metastasis.
Treatment
Each patient received a treatment plan after the diagnosis was confirmed. For skin basal-cell carcinoma, squamous-cell carcinoma, and melanoma, Mohs micrographic surgery was performed whenever possible. The specific procedure of Mohs micrographic surgery was as follows: the tumor quadrants were marked, and the tumor was resected by expanding 1–5 mm along the visible edge of the tumor. The excised tumor was marked and sent for rapid frozen pathological examination, and the tumor margins and bases were examined under a microscope. After the residual tumor had been accurately located and resected according to the pathological results, a rapid pathological examination was performed again until the pseudopodia in the lateral and deep extensions of the tumor had been completely removed.
In patients who could not tolerate long-term surgery because of their age or health status and those with small tumors, conventional surgery was performed to expand the resection, and the scope and depth of resection followed the relevant guidelines and consensuses. Local random flaps or skin grafts were prepared to repair large skin and soft-tissue defects intraoperatively. Additionally, some patients with malignant tumors underwent postoperative radiotherapy, chemotherapy, and biological targeted therapy after surgery.
In patients with deep mycosis, such as sporotrichosis and phaeohyphomycosis, oral itraconazole capsules or injection of liposomal amphotericin B was administered after pathogenic fungi were identified. Anti-inflammatory treatments, eg, glucocorticoids, were administered to patients with inflammatory diseases, such as gangrenous pyoderma. Comorbidities, eg, solid tumors, lymphoid hematopoietic system tumors, and rheumatic immune diseases, were actively investigated. All patients with NK/T-cell lymphoma were transferred to the Department of Haematology for chemotherapy. Patients with odontogenic fistulas were transferred for oral and maxillofacial surgeries.
Data Collection and Analysis
The medical records and pathological sections of all patients were collected to retrospectively analyze patients’ age and sex, sites of ulcers, clinical manifestations, pathological diagnosis, and treatment methods. The prognosis and outcome of each patient were tracked by outpatient or telephone follow-up.
Results
Age of Onset and Final Diagnosis
There were 163 men and 80 women, with a male-to-female ratio of 2.04:1. Rhinofacial ulcers occurred more often in middle-aged and elderly people (aged 41–70 years) than in younger people and were more common in men than in women. The age of onset was 25–91 years, with 4 patients (1.6%) aged 25–30 years, 22 patients (9.1%) aged 31–40 years, 56 patients (23.0%) aged 41–50 years, 59 patients (24.3%) aged 51–60 years, 68 patients (28.0%) aged 61–70 years, 24 patients (9.9%) aged 71–80 years, 9 patients (3.7%) aged 81–90 years, and 1 patient (0.4%) aged >90 years. The average age of onset was 67.8 years and the median age was 59 years. The duration of ulcer of disease ranged from 3 months to 32 years, with an average of 2.3 years.
The final diagnoses of 243 patients are listed in Table 1. Based on findings of the histopathological examination, 172 patients (70.8%) were diagnosed with skin primary cutaneous malignancies, including 88 (51.1%) with basal-cell carcinoma, 61 (35.5%) with squamous-cell carcinoma, 21 (12.2%) with melanoma, and 2 (1.2%) with senile cutaneous angiosarcoma; 8 patients (3.3%) were secondary to reactive hyperplasia of the capillary endothelium, which was related to tumor treatment; 24 patients (9.9%) were diagnosed with deep cutaneous mycosis, including 19 (79.2%) with sporotrichosis, 2 (8.3%) with phaeohyphomycosis, 3 (12.5%) with mucormycosis; 3 patients (1.2%) were diagnosed with pyoderma gangrene; 10 patients were diagnosed with NK/T-cell lymphoma (4.1%); and 26 patients were diagnosed with odontogenic fistula (10.7%). The most common causes of rhinofacial ulcers were tumors, odontogenic fistulas, and fungal infections. The top three types of tumors were basal-cell carcinoma, squamous-cell carcinoma, and melanoma.
 |
Table 1 Distribution of the Final Diagnoses of 243 Rhinofacial Ulcers [n (%)] |
Onset Site
The locations of rhinofacial ulcers in the 243 patients are listed in Table 2. The most common sites of rhinofacial ulcers were the nasal dorsum (66 cases, 27.2%), cheeks on both sides of the nasal dorsum (58 cases, 23.9%), and nasal root (27 cases, 11.1%). The sites of the nasal dorsum, both sides of the nasal dorsum, and the upper lip were common in men, whereas, the nasal dorsum, both sides of the nasal dorsum, and the nasal root were common in women. These results showed that skin ulcers were more likely to be on the nasal dorsum and on both sides of the nasal dorsum in both sexes. In men, ulcers were more likely to be on the upper lip than on other areas, which was presumed to be related to the higher number of male smokers.
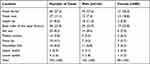 |
Table 2 Locations of 243 Rhinofacial Skin Ulcers [n (%)] |
Clinical Characteristics of the Ulcers
The smallest ulcer measured 0.2 cm × 0.2 cm in area, and the largest measured 3.5 cm × 3.0 cm. Fifty-one patients (21.0%) complained of pruritus, 80 (32.9%) complained of pain, and 112 patients (46.1%) had no symptoms. Black crusts were observed on the surfaces of 18 ulcers (7.4%), and 94 (38.7%) ulcers showed yellow purulent secretions.
Among the 88 ulcers related to basal-cell carcinoma, 74 had obvious suggestive manifestations: the edge of the ulcer showed a pearl string-like or dike shape, with dendritic telangiectasia, accompanied by blue-gray, brown, and black pigmentation (Figure 1A and B). These characteristics were highly suggestive of basal-cell carcinoma. Squamous-cell carcinomas were characterized by papules, nodules, plaques, or ulcers on the surface (Figure 1C). One case of keratoacanthoma-like squamous-cell carcinoma showed a crater-like ulcer (Figure 1D). All 21 cases of melanoma manifested as black patches, with the formation of nodular or sunken ulcers in the center of the black patches (Figure 1E). The ulcers in 3 cases of gangrenous pyoderma were deep and irregular in shape, with foul-smelling yellow-green pus and scabs and purplish-red surrounding skin, which were accompanied by obvious pain. Ulcers caused by sporotrichosis were covered with thick scabs (Figure 1F). Odontogenic fistulas often occurred on the nose and face, manifesting as nodules and ulcers (Figure 1G–J). Additionally, the black scab on the ulcer was suggestive of NK/T cell lymphoma, vasculitis, and deep fungal infection.
Histopathological Changes
Basal- and squamous-cell carcinomas in rhinofacial ulcers were classified according to histopathological findings. Different sizes of basal-like basophilic clumps in the dermis were observed under a microscope in basal-cell carcinoma. The tumor cells were arranged in a palisade shape, with contraction gaps at the edge of the tumor mass, and some melanin granules were observed. BerEP4 expression was often detected by immunohistochemistry. In squamous-cell carcinoma, squamous epithelial cell clumps of different sizes and varying degrees of differentiation were observed in the dermis under a microscope. CK5/6 expression was detected using immunohistochemistry. The pathological classifications of the ulcers in this study are listed in Tables 3 and 4.
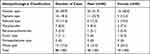 |
Table 3 Histopathological Classification of 88 Basal-Cell Carcinomas [n (%)] |
 |
Table 4 Histopathological Classification of 61 Squamous-Cell Carcinomas [n (%)] |
Triggers and Pre-Existing Skin Lesions
Among the 21 patients with melanoma, 7 cases developed on the basis of the pigmented nevus at the site of the ulcer, and 14 had no history of a pigmented nevus. Among the 24 patients with deep mycosis, 18 patients with sporotrichosis had a history of injury from crops or firewood, and the other two patients with sporotrichosis or other fungal diseases had no history of trauma. Three patients with mucormycosis had diabetes and high glycated hemoglobin A1c levels. One patient who had been diagnosed with lupus nephritis accompanied by diabetes, received long-term oral tacrolimus treatment. All 26 patients with odontogenic fistulas had a history of pulpitis (Figure 1G–J). All 8 patients with vascular endothelial reactive hyperplasia with ulceration had visceral tumors, including 5 cases of lung adenocarcinoma and 3 cases of liver cancer, all of which were treated with programmed death-1 (PD-1) inhibitors, such as camrelizumab. Among the 3 patients with gangrenous pyoderma, 2 patients had myelodysplastic syndrome, and 1 patient was followed up for 3 years without systemic disease.
Prognosis
All patients were followed up for 1–84 months. None of the 71 patients with basal-cell carcinoma who underwent Mohs micrographic surgery showed a recurrence or metastasis. Seventeen patients with basal-cell carcinoma underwent conventional extended resection, in which 4 patients had a recurrence in situ but without metastasis. Fifty patients with squamous-cell carcinoma underwent Mohs micrographic surgery, 2 of whom had a recurrence in situ, and 1 had a lung metastasis who died 15 months postoperatively. Eleven patients with squamous-cell carcinoma underwent conventional extended resection, and 3 of them experienced recurrence in situ. Twenty-one patients with melanoma were followed up for 0.5–5 years after extended surgical resection. Among them, 7 patients had no metastasis or recurrence, and 14 died of visceral metastasis of melanoma, and the average survival time was 3.9 years. Two elderly patients with cutaneous angiosarcoma on the face and scalp had recurrence at 2 months and 6 months, respectively, and died of visceral metastasis respectively at 19 months and 21 months after surgery, respectively. All patients with sporotrichosis were cured without recurrence after 4.2 months in average. Patients with phaeohyphomycosis or mucormycosis were lost to follow-up. Among the 10 patients with NK/T-cell lymphoma, 5 were lost to follow-up and 5 patients died; the average survival time was 11 months. Patients with odontogenic fistulas were cured after regular treatments in the Department of Dentistry.
Discussion
Rhinofacial ulcers are uncommon in the clinical work of otolaryngology/head and neck surgery and dermatology. Ulcers are secondary lesions that can be caused by infections, trauma, tumors, and inflammation, therefore, clinicians need to investigate the etiology and choose the best corresponding treatment carefully and actively in order to achieve good clinical outcomes.5 Histopathological examination is an effective means of determining the etiology of rhinofacial ulcers. Combined with immunohistochemistry and other techniques, it can definitely diagnose skin tumors, such as basal-cell carcinoma, squamous-cell carcinoma, and melanoma. Bacterial and fungal cultures and drug susceptibility tests are of great value for identifying the pathogenic microorganisms in infectious ulcers and selecting therapeutic drugs.
Basal-cell carcinoma is the most common rhinofacial neoplastic ulcer in the elderly population. Basal-cell carcinoma accounts for approximately 75.0% of malignant epidermal tumors and is more common in sunlight-exposed sites, eg, the external nose, periorbital region, and cheek.6 This disease grows slowly but is an invasive tumor with single-focal continuous growth. Distant metastasis is rare, but if not treated timely, invasive lesions can cause serious damage to the surrounding tissues.7 In clinical practice, the skin lesions of basal-cell carcinoma have certain characteristic features. When the edge of the skin ulcers is in the shape of pearl string-like or tension ridges, it is necessary to be highly vigilant about the possibility of basal-cell carcinoma.8 Dermoscopy is highly sensitive for screening basal-cell carcinoma.9 Melanoma in Asians mostly occurs on the extremities, but it is also common on the face. In this study, 14 patients (66.7%) with melanoma did not have a history of pigmented nevi, which is consistent with the theory that melanoma can directly originate from melanocytes. The dark patch of melanoma progressing to ulcers often indicates that the tumor has infiltrated below the middle dermis. Melanoma is associated with a poor prognosis.10 Therefore, at this time, sentinel lymph node biopsy and local lymph node dissection are required, and visceral metastases should be carefully investigated.
The treatment of rhinofacial tumor ulcers should be individualized, and the patient’s function and aesthetics should be considered while curing the disease. Extensive resection based on the Breslow thickness of the tumor is the recommended protocol for the diagnosis and treatment of melanoma in various countries.11 Mohs micrographic surgery is recommended by the National Comprehensive Cancer Network guidelines and consensus for various skin malignancies, including basal-cell carcinoma and squamous-cell carcinoma.12 According to previous literature,13 the 5-year cure rate of traditional surgery for primary basal-cell carcinoma is only 90–93%, while that of Mohs micrographic surgery can reach 98–99%; for recurrent basal-cell carcinoma, the 5-year cure rate of traditional surgery is only 80.1%, while that of Mohs micrographic surgery can reach 94.4%. The basic principle of this procedure is to use the elasticity of fresh tissue to remove the sidewall of the tumor specimen by pressing down to make it lie in the same plane as the bottom of the tumor, and then use the method of transverse horizontal frozen sectioning and intraoperative tumor localization to perform comprehensive microscopic tracing examination, directional staining, and directional marking of all the resection margins and tumor base tissues. Then microscopic tracing is performed, and the undissected tumor pseudopodia are resected. Mohs micrographic surgery has two major advantages over traditional extended tumor resection. First, it can accurately control the surgical resection range and preserve the normal skin tissue to the maximum extent, which is particularly important for areas with skin tissue shortages such as the face. Second, repeated intraoperative inspection of the resection margin can ensure complete tumor removal, in order to significantly reduce the postoperative recurrence rate.14 For the ala nasi, periorbital, eyelid margin, and medial canthus areas, especially when there are recurrent facial tumors with unclear clinical boundaries or tumors with an invasive growth pattern on histopathology (eg, morphea-like basal-cell carcinoma), Mohs micrographic surgery has obvious advantages. However, this surgery also has its shortcomings. It requires a high degree of cooperation among surgeons, pathologists, and pathological technicians. The surgery is time-consuming, labor-intensive, and expensive. It also involves a series of special preparations and doctor-patient communication efforts in terms of the surgical environment, patient status, and doctor skills. Therefore, the patients with cancer in this study received different surgical plans according to their specific conditions. In addition to surgical treatment, recent studies have confirmed that the Hedgehog signaling pathway plays an important role in the pathogenesis of basal-cell carcinoma.15 Sonidegib phosphate, a Hedgehog pathway inhibitor, has been approved for the treatment of locally advanced basal-cell carcinoma.
Pathogenic microbial infections are another major cause of rhinofacial ulcers. Herein, approximately 10% of the ulcers were caused by fungal infections. Sporotrichosis was the most common subcutaneous mycosis in this study, which is caused by Sporothrix infection (eg, Sporothrix schenkii, Sporothrix brasiliensis, Sporothrix globosa, and Sporothrix Mexicana). Patients often have a clear history of stabbing or puncture wounds from reeds, straws, or firewood, with papules and nodules at the trauma site, which may be accompanied by ulceration and scabs, and the disease can spread through the lymphatic vessels.16 Mucormycosis, formerly known as zygomycosis, is a kind of mycosis caused by Rhizopus, Mucor, Rhizomucor and Lichtheimia infections. It often manifests as necrotizing ecthyma-like skin lesions with severe oedema, necrosis, and ulcers.17 Among the three patients with mucormycosis in this study, two had primary skin mucormycosis caused by direct skin inoculation, and one had nasal sinus mucormycosis that had spread to the skin as a secondary skin mucormycosis. The risk factors for mucormycosis mainly include diabetes with poor blood glucose control and various immunosuppressants or deficiencies, which are consistent with the characteristics of the three patients in our study. For infectious ulcers, cultures of pus, secretions, and tissue masses and drug susceptibility tests are helpful in the diagnosis and selection of therapeutic drugs. With advances in biotechnology, high-throughput sequencing technology has entered clinical practice, which can more effectively identify the pathogenic microorganisms that cause ulcers. Besides fungi, atypical mycobacterial infections such as Mycobacterium marinum infection and Mycobacterium chelonae infection can also cause facial ulcers, as well as parasitic diseases, such as, kala-azar,18 to which clinicians should pay attention.
The clinical applications of monoclonal antibodies and small-molecule targeted drugs for the treatment of malignant tumors have a short history, and some adverse reactions are still not well known by clinicians. As the main immune checkpoint inhibitors, PD-1 monoclonal antibodies have definite efficacy for various of solid tumors, but sometimes induce adverse skin reactions.19 A study that included 2016 cases of camrelizumab (a PD-1 monoclonal antibody) monotherapy or combination therapy for advanced cancer showed that 834 of 1059 patients (78.8%) receiving camrelizumab monotherapy developed reactive cutaneous angiogenesis,20 with an extremely high incidence. Recently, with the popularity of biologics and small-molecule drugs for the treatment of malignant tumors, reactive hyperplasia of the capillary endothelium has become more common, attracting the attention of otolaryngologists and dermatologists. However, the mechanism of reactive capillary hyperplasia remains unclear. Some studies have suggested that camrelizumab abnormally regulates the highly selective and low-affinity vascular endothelial growth factor receptor 2 (VEGFR2), resulting in reactive hyperplasia of vascular endothelial cells.21 This type of reactive cutaneous vascular hyperplasia can develop within a few days to several weeks of the first administration of anti-PD-1. It often manifests as multiple red papules which may disappear or disappear after drug withdrawal. The eight patients with reactive cutaneous angioplasia included in this study all had malignant tumors, eg, lung cancer and melanoma. Hemangioma-like papules, which were as large as a soybean to a pea grain, occurred after the administration of PD-1 monoclonal antibody, with the earliest ones appearing 12 days and the latest ones appearing 2 months after the administration of the drug. In such cases, ulcers are usually caused by scratching or friction.
Conclusions
In summary, rhinofacial ulcers are relatively rare in clinical practice, and their causes are extremely diverse and complex. They can be easily misdiagnosed and mistreated. Correct treatment can only be performed by actively searching for the causes of the disease and making a correct diagnosis.
Abbreviations
NK, natural killer; PD-1, programmed death-1.
Ethics Approval and Informed Consent
This study was approved by the Ethics Committee of the Affiliated Hospital of Weifang Medical University and was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all the patients before the commencement of the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Traditional Chinese Medicine Science and Technology Project of Shandong Province (number [no.]: 2021Q093) and Doctoral Startup Fund of the Affiliated Hospital of Weifang Medical University (no.: 2021BKQ02).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hoffman MD. Inflammatory ulcers. Clin Dermatol. 2007;25(1):131–138. doi:10.1016/j.clindermatol.2006.09.010
2. Bernstein SC, Lim KK, Brodland DG, Heidelberg KA. The many faces of squamous cell carcinoma. Dermatol Surg. 1996;22(3):243–254. doi:10.1111/j.1524-4725.1996.tb00315.x
3. Yang L, Tang X, Peng X, Qian D, Guo Q, Guo H. Clinical characteristics of primary intestinal NK/T cell lymphoma, nasal type: case series and review of the literature. Pathol Res Pract. 2018;214(8):1081–1086. doi:10.1016/j.prp.2018.05.013
4. Skiada A, Lass-Floerl C, Klimko N, Ibrahim A, Roilides E, Petrikkos G. Challenges in the diagnosis and treatment of mucormycosis. Med Mycol. 2018;56(suppl_1):93–101. doi:10.1093/mmy/myx101
5. Castro MCR, Ramos ESM. The rash with mucosal ulceration. Clin Dermatol. 2020;38(1):35–41. doi:10.1016/j.clindermatol.2019.10.019
6. Rubin AI, Chen EH, Ratner D. Basal-cell carcinoma. N Engl J Med. 2005;353(21):2262–2269. doi:10.1056/NEJMra044151
7. Basset-Seguin N, Herms F. Update in the management of basal cell carcinoma. Acta Derm Venereol. 2020;100(11):adv00140. doi:10.2340/00015555-3495
8. Tanese K. Diagnosis and management of basal cell carcinoma. Curr Treat Options Oncol. 2019;20(2):13. doi:10.1007/s11864-019-0610-0
9. Reiter O, Mimouni I, Gdalevich M, et al. The diagnostic accuracy of dermoscopy for basal cell carcinoma: a systematic review and meta-analysis. J Am Acad Dermatol. 2019;80(5):1380–1388. doi:10.1016/j.jaad.2018.12.026
10. Ellison PM, Zitelli JA, Brodland DG. Mohs micrographic surgery for melanoma: a prospective multicenter study. J Am Acad Dermatol. 2019;81(3):767–774. doi:10.1016/j.jaad.2019.05.057
11. Demer AM, Hanson JL, Maher IA, Liszewski W. Association of Mohs micrographic surgery vs wide local excision with overall survival outcomes for patients with melanoma of the trunk and extremities. JAMA Dermatol. 2021;157(1):84–89. doi:10.1001/jamadermatol.2020.3950
12. Lawrence L. Mohs’ micrographic surgery for basal cell carcinoma. Clin Exp Dermatol. 1999;24(2):130–133. doi:10.1046/j.1365-2230.1999.00433.x
13. Rowe DE, Carroll RJ, Day CL Jr. Long-term recurrence rates in previously untreated (primary) basal cell carcinoma: implications for patient follow-up. J Dermatol Surg Oncol. 1989;15(3):315–328. doi:10.1111/j.1524-4725.1989.tb03166.x
14. Castanheira A, Boaventura P, Soares P, Vieira F, Lopes JM, Mota A. MOHS micrographic surgery for head and neck nonmelanoma skin cancer: An approach for ENT surgeons. Dermatol Ther. 2021 Jan;34(1):e14661. doi:10.1111/dth.14661
15. Gutzmer R, Solomon JA. Hedgehog pathway inhibition for the treatment of basal cell carcinoma. Target Oncol. 2019;14(3):253–267. doi:10.1007/s11523-019-00648-2
16. Chakrabarti A, Bonifaz A, Gutierrez-Galhardo MC, Mochizuki T, Li S. Global epidemiology of sporotrichosis. Med Mycol. 2015;53(1):3–14. doi:10.1093/mmy/myu062
17. Cornely OA, Alastruey-Izquierdo A, Arenz D, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019;19(12):e405–e421. doi:10.1016/S1473-3099(19)30312-3
18. Masood S, Naveed S, Alvi RU. Infiltrated leishmaniasis recidivans cutis on the face: a rare clinical presentation. Trop Doct. 2012;42(2):120–121. doi:10.1258/td.2011.110396
19. Simonsen AB, Kaae J, Ellebaek E, Svane IM, Zachariae C. Cutaneous adverse reactions to anti-PD-1 treatment-A systematic review. J Am Acad Dermatol. 2020;83(5):1415–1424. doi:10.1016/j.jaad.2020.04.058
20. Thompson G, McLean-Tooke A, Lucas M. Cross with caution: antibiotic cross-reactivity and co-reactivity patterns in severe cutaneous adverse reactions. Front Immunol. 2021;12(12):601954. doi:10.3389/fimmu.2021.601954
21. Li Q, Wang Y, Jia W, et al. Low-dose anti-angiogenic therapy sensitizes breast cancer to PD-1 blockade. Clin Cancer Res. 2020;26(7):1712–1724. doi:10.1158/1078-0432.CCR-19-2179
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

