Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 14
Clinical Profiles and the Outcomes of Burn Patients Admitted to the Burn Unit of Jimma Medical Center
Authors Mulugeta T , Alemayehu H, Gerema U
Received 29 May 2021
Accepted for publication 2 July 2021
Published 12 July 2021 Volume 2021:14 Pages 859—866
DOI https://doi.org/10.2147/CCID.S322486
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Temesgen Mulugeta,1 Henock Alemayehu,1 Urge Gerema2
1Jimma University, Institute of Health, School of Pharmacy, Department of Clinical Pharmacy, Jimma, Oromia, Ethiopia; 2Jimma University, Institute of Health, School of Biomedical Sciences, Anatomy Course Unit, Jimma, Oromia, Ethiopia
Correspondence: Temesgen Mulugeta
Jimma University, Institute of Health, School of Pharmacy, Department of Clinical Pharmacy, Jimma, Oromia, Ethiopia
Email [email protected]
Background: Burn is a serious public health problem and a leading cause of disability and disfigurement. However, there was no published study from our Hospital Burn Unit that assessed the clinical profiles and the outcomes of burn patients.
Objective: This study was aimed to assess the clinical profiles and the outcomes of patients admitted with burn injuries.
Methods: Hospital-based retrospective cross-sectional study was conducted at the Burn Unit of JMC. Systematic random sampling was used to include the burn patients. Data were analyzed using SPSS version 25. Descriptive statistics, chi-square (χ2), and student-t-test were performed to describe and assess the relationships between the variables. Multivariate logistic regression was performed to determine the factors affecting the length of hospital stays.
Results: One hundred twenty-four burn patients (51.6% female) were included. The majority (79.84%) of the patients were in the age category of less than 29 years. Scalds (47.6%) were the most common cause of burns with three times in females. The extremities (93.5%) were the most frequently affected areas. Patients with second-degree superficial burns accounted for 61.3% of all patients. In 95.88% of the patients, the total body surface area burn (TBSA) was below 20%. Lactated ringers (69.4%) and tramadol (71.0%) were the most frequently used IV fluid for resuscitation and analgesic agent for pain, respectively. Patients who undergo any of the surgical procedures stayed in the hospital for greater than 30 days more than 4 times likely (OR = 4.8, 95% CI 2.08– 11.2, P < 0.001).
Conclusion: Scalds are the most common cause of burn injury, particularly in patients aged less than 14 years. Educating the community about the risk groups, household safety precautions, and early seeking medical care may reduce the incidence and morbidity of burn injuries.
Keywords: burn, clinical profiles, outcomes, Jimma Medical Center
Introduction
World Health Organization (2018) estimated 180,000 deaths every year are caused by burns – the vast majority (over 95%) occur in low and middle-income countries.1 In the United States of America (USA), the two most common etiologies of burn injuries were fire/flame and scalds, accounting for 76% of cases reported. Scald injuries were most prevalent in children under 5, while fire/flame injuries dominated the remaining age categories. The adult age group (20 to 59 years) makes up 55% of burns. More than 67% of the reported total burn sizes were less than 10% TBSA. Seventy-four percent of the burn injuries have occurred in the home.2
A review from sub-Saharan Africa showed the average age of burn patients was 15.3 years. Scalds were the commonest cause of thermal injuries, accounting for 59% of all burns.3 Home, particularly the kitchen, was the most common location of sustaining burn injuries.4 A study by Dongo et al reported over 40% of injuries occurred between November and January.5 From the number of risk factors for burn, underlying medical conditions; epilepsy, peripheral neuropathy, physical and cognitive disabilities, alcohol abuse, and smoking are common.1 A study reported Epileptic patients accounted for 1.38% of total burn admission.6 A study from Malawi should 31% of patients were presented to the hospital after 48 hours.7 The first 24 hours after burn injury require aggressive medical management to assure the survival and minimize complications.8 Fluid resuscitation after burn injury is a cornerstone of burn care. Fluid resuscitation must be aimed at maintaining tissue perfusion and organ function while avoiding the complications of inadequate or excessive fluid therapy.9 A study identified the most commonly used resuscitation fluid was Ringer’s lactate solution (46.9%).10 Burn injury is widely considered one of the most painful injuries that a person can sustain.11 A secondary analysis of the 1992 to 1999 data of patients with burns showed opioids were the most commonly used analgesics for all years studied.12 Tyson et al reported the commonest operative procedures done were skin grafting and debridement, accounting for 46.7% and 42.8% of all operative cases, respectively.7 The burn mortality averaged 17% or the death of one of every five burn victims.3
In Ethiopia, some of the available studies were done in the country’s capital and the northern part.13–15 An early study reported burn cases accounted for 1.73% of all hospital admissions.16 About 9.0% of the traumatic injuries were caused by burns.17 A study from the Mekelle reported, the most frequent cause of burns in children was scald (69.4%). Most (86.6%) of the patients had partial-thickness or second-degree burns. About 41.0% of the burn patients were presented lately after 24 hours of burn.18 A study reported 10% of epileptic patients sustained burns as a result of seizures.19 A study by Mengistu et al reported among patients who felt severe pain (87.1%), most of them (48.4%) took paracetamol, 30.6% took tramadol, and the remaining 8.1% took nonsteroidal anti-inflammatory drugs (diclofenac).13 Another study reported fluid resuscitation was given for 52.6% of the burn patients and the lack of fluid resuscitation within 24 hours was reported to be associated with the discharge complications (ie contracture, disfigurement, amputation, a scar of skin graft, and death).18 A study from Addis Ababa reported, 52.7% of burn patients underwent operative treatment, with the most frequent operation being skin grafting.15 Alemayehu et al reported the mean length of hospital stay of burn patients was 17.34 days (SD: 25.334; range: 1–290 days).18 However, Mulat and Salemark reported the overall median hospital stay was 44 days.14 Mehta et al reported the mortality rate among burn patients was 13.3%.15
Like other injury mechanisms, the prevention of burns requires adequate knowledge of the epidemiological characteristics and associated risk factors, it is hence important to define clearly the factors which contribute to burn causation. While much has been accomplished in the areas of primary and secondary prevention of fires and burns in many developed or high-income countries (HICs), the same cannot be done for many low and middle-income countries (LMICs).20 In particular, there was no published study from our Hospital Burn Unit that assessed the clinical profiles and the outcomes of burn patients. Therefore, this study was aimed to assess the clinical profiles and the outcomes of burn patients admitted to the burn unit of Jimma Medical Center (JMC).
Methods and Materials
Study Area and Period
This study was conducted in the Burn Unit of JMC. Jimma Medical Center is one of the teaching and the referral hospital found in Jimma town, Oromia Region, Ethiopia. It is found 350 km away from the capital city of the country, Addis Ababa in the Southwest direction. The data was collected between November 2020 and January 2021.
Study Design
Hospital-based retrospective cross-sectional study.
Study Population
The study population for this study was all burn patients who admitted to the Burn Unit of JMC between September 2018 and 2020 and received medical/surgical care. Patients’ medical records with illegible handwriting and incomplete data excluded.
Sample Size and Sampling Technique
Sample Size Determination
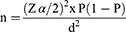
Due to the time and economic feasibility, sample size calculation was considered. The sample size was calculated by using single population proportion formula by considering the following assumptions: p = 8.9%; prevalence of burn injury among traumatic injuries in Dilchora Hospital, Dire Dawa, Eastern Ethiopia.17
Where; n = the minimum sample size required, d = Margin of error = 5%, Zα/2 = Standard normal value at (1- α) =1.96
The number of burn patients admitted in the year, 2018 to 2020 was 205. Since the total number of burn patients was small, the minimum sample size (124) was used for the final sample size.
Sampling Technique
Systematic random sampling with every other patient’s card was selected until the minimum sample size was reached.
Data Collection Instrument and Quality Assurance
Data were collected from patient’s medical records by using a data collection checklist developed after reviewing different burn guidelines and related studies. Before data collection was started, a pretest was done on 5% of the burn patients of medical records. The content of the questioner has then modified accordingly. Data collectors were trained on the content of the questionnaire. Data was collected by a principal investigator and two trained Clinical nurses.
Data Processing and Analysis
The collected data were checked, cleaned, and analyzed using SPSS version 25. Descriptive statistics were performed and presented using frequency, percentages, mean (SD), median (IQR) based on the scales of the variables. Chi-Square (χ2) for categorical variables and student-t-test for continuous variables were used to assess the relationships between the variables of interest. Bivariate and multivariate logistic regression was performed to identify factors associated with length of hospital stay for greater than 30 days. Odds ratio (OR) with 95% confidence interval (CI) and the respective P-value of less than 0.05 was used to declare the statistical significance.
Ethical Consideration
Ethical clearance was obtained from Jimma University Institutional Review Board (IRB). The study was conducted in accordance with the Declaration of Helsinki. Since it is retrospective data, the patient informed consent to review their medical records was waived by the ethics committee. Before the actual data collection, the confidentiality of the study subjects was taken into account by avoiding the names and any other personal identification information.
Operational Definition Terms
Injury: Any instance of physical damage to the body or body part.
Flame burn: injury due to overheated visible, gaseous part of a fire
Scald burn: injury due to contact with hot liquids or steam
Contact burn: injury due to contact with hot or cold solids
Chemical burn: injury due to contact with harmful chemicals
Electricity burn: an injury occurred when electric currents pass through the body
Result
Sociodemographic of the Participants and the Place of Burn Occurrence
A total of 124 patients were included. Females accounted for 51.6%. The median (IQR) age of the patients was 17.0 (4.25, 25.0) years. The majority (79.84%) of the patients were in the age category of less than 29 years. Only 7.3% of the patients were older than 45 years old. Two-third (67.7%) of the patients came from rural areas. Regarding the place of occurrence of burn injury, most (62.1%) of the burn injury occurred at home, particularly in the kitchen (Table 1).
 |
Table 1 Sociodemographic, Place of Burn of Occurrence, Predisposing Conditions, and Season of Admission of the Participants |
Time to Seeking Medical Care
Time to admission to the health facility was reported in 92 patients. The median (IQR) time to seeking medical care after sustaining burns was 6.0 (2.25, 9.75) hours. The majority (62.9%) of the patients were presented to health facilities within 12 hours of sustaining a burn injury.
Etiology of Burn
Overall, the scald (47.6%) was the most common cause of burn followed by flame (29.8%). The chemical burn was the least common (3.2%). From the scald and contact burn cases, 64.4% and 71.4% of the patients were aged below 14 years, respectively. While, from the flame and chemical burn cases, 54.1% and 75.0% of the patients were between 15 and 29 years, respectively. As the age of the patients increased to 30–45 years, gasoline (66.7%) was the frequent cause of the burn. Electricity, gasoline, and chemical burns are only reported in male patients. However, scald burn is more relatively reported in females patients compared to males (ratio 3.11: 1) (Table 2).
 |
Table 2 Etiology Distribution by Gender and Age |
Predisposing Conditions and Season of the Admission
Epilepsy (17.7%) was the most common predisposing condition for the burn. Intentional burn due to quarrels within the families causes self-burn in four patients. The winter (December to February) (33.1%) is the most common season when most patients admitted to our hospital (Table 3).
 |
Table 3 Burn Predisposing Conditions and Season of the Occurrence |
Burn Sites
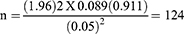
Extremities (93.5%) are the most commonly burned anatomic sites, of which the upper extremities accounted for 67.7%. The posterior trunk was the least burned site, which accounted for 14.50% of the anatomic sites burned. There are no significant differences in terms of burn sites and the sex of the patients (P>0.05). Head, face, and neck burns are proportionally higher in patients age greater than 10 years (82.1% vs 17.9%, P = 0.027) (Figure 1).
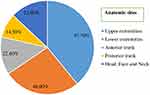 |
Figure 1 Anatomic sites of burn among patients. |
Burn Depth and Severity
Regarding the extent of the burn, 61.3% of the patients were assessed with the second degree/partial thickness burn, followed by third-degree/full-thickness burn (31.5%). Six (4.8%) of the patients had a first-degree/superficial burn. Scald and contact burn were the two causes of the superficial burn. The majority of the superficial burn is caused by scald (66.7%). Most of the full-thickness burn is caused by flame burn (64.1%). The total body surface area burn (TBSA) was estimated in 97 patients. The median (IQR) of TBSA was 16.0% (9.0, 18.5). Most (55.67%) of the patients had a TBSA burn between 10% and 20%. Four (4.12%) of the patients had TBSA burn greater than 20%. Patients with gasoline burns had higher mean TBSA burn compared to patients with contact burns (mean difference = −7.26, P = 0.004) and scald burns (mean difference= −5.18, P=0.029) (Table 4).
 |
Table 4 Etiology Against the TBSA Burn |
Medical Care
IV fluids were given for 86.3% of the burn patients. The most frequently used fluid was lactated ringer (69.4%) followed by normal saline (64.5%). Fifty-eight (46.8%) of the patients had received the combinations of lactated ringers and normal saline. For burn pain management, analgesics were prescribed to 97.6% of the patients. The most frequently prescribed agent was tramadol (71.0%) followed by diclofenac (43.5%). Forty-eight (38.7%) of the patients have prescribed the combination of tramadol with diclofenac. Tetanus anti-toxoid for the prevention of tetanus was given for 5.6% of the patients (Table 5).
 |
Table 5 Patterns of IV Fluids Used, Tetanus Anti-Toxoid, and Analgesics Prescription Among Burn Patients |
Surgical Procedures
Surgical procedures were done for 35.5% of burn patients. Debridement followed by skin grafting was done for 21.0% and 11.3% of patients, respectively (Figure 2).
 |
Figure 2 Proportion of the surgical procedures done for the burn patients. |
Length of Hospital Stay and Death
The median (IQR) length of hospital stay for all patients was 30.0 (21.25, 36) days. Half of the patients stayed in the hospital for greater than 30 days. In multivariate logistic regression, only patients who undergo any of the surgical procedures were more than 4 times likely to stay (OR = 4.8, 95% CI 2.08–11.2, P < 0.001) in the hospital for greater than 30 days. Four (3.2%) patients died. The TBSA/etiology burn for patients who died was (1) 16% flame burn, (2) 18% gasoline burn, (3) 20% electrical burn, and (4) 25% scald burn. From the death summary notes, the cause of death was cardiac arrest in the two patients, multi-organ failure, and internal bleeding in each of the remaining patients.
Discussion
Burn injuries are the most common, devastating trauma and major public health problems that result in short-and long-term squeals. Especially in the pediatric population, it has major psychosocial, emotional, functional, and cosmetic consequences. Therefore, the present study aimed to assess clinical profiles and the outcomes of burn patients admitted to the burn unit of JMC. Knowing clinical profile and the outcome of burn injuries are very important for implementing effective preventive methods, early diagnosis, and treatment of burn patients. In the current study, the majority of the burn injuries (79.8%) were occurring in children. This finding was similar to studies done in Asmara, Eritrea (75%),21 Yekatit 12 Hospital, Addis Ababa (76%),13 western Kenya (82%).22 The reason might be due to children being unaware of the surrounding environment, lack of instinct to understand the danger of different objects, high physical activity, especially during the children developing locomotor. Adults have awareness, understand objects due to increased motor skills.
In the present study, two-thirds (62.1%) of the burn injuries occurred at home, particularly in the kitchen. This finding consistent with studies done in the USA,2 Cameroon,23 Kenya,22 China.24 This could probably be due to children staying home, especially in the kitchen with their mothers while mothers preparing meals. In our study, Epilepsy (17.7%) was the most common predisposing condition for burn injuries. This study, in line with studies done in India,25 Indore,26 and Melbourne.27 This could be explained by the fact that an attack during epilepsy starts with a fall, unconsciousness, and followed by convulsion. When epileptic fall on burn agents, they experience 2 to 5-minute period and exposed to prolonged heat and result in severe and deep-degree burn.25 There is also limited awareness among the population about the epileptic risk of burn injuries. The current study showed that most burn injuries occurred in the study setting during the winter (dry) season. This finding is consistent with a study from Eritrea21 and a review done in Nigeria.28 However, it is in contrast to a study done in Iraq, where burns are more frequent during autumn.29 This is cloud be explained by the geographic variation weather.
The current study revealed the scald (47.6%) was the common cause of burn injuries followed by flame (29.8%). This finding is in line with studies done in different countries; USA,2 Iran,30 Italy,31 China.32 In our study setting, scald burn was occurred in the home, mostly caused by hot water, boiling water, hot tea in the kitchen during meal preparation. According to the current study, extremities are the most commonly burned anatomic sites, particularly upper extremities. The head, face, and neck burn injuries were the least anatomic sites. This study is similar to other previous studies.13,31,33–36 This can be explained by the mechanism of injury: when someone contacts with hot or boiling water, hot tea, chemical, electrical, and radiation, patients may present with different burned anatomic sites, in which extremities are common due to manipulation of different objects.
In our study, the second-degree/partial thickness burn was common, followed by the third-degree/full-thickness burn. This finding is consistent with the other previous studies.13,21,22,30,32,34,37 This might be explained by the common cause of burn injuries in this study was scald burn, which affected the outer layers of skin (epidermis) and part of the second layers of skin (dermis) exposed the body to infection. In this study, the median (IQR) of TBSA was less than 20%. This finding is similar to other previous studies.21,24,34–36 This might be due to similarity in sample size, admission criteria of burn injuries, causative agent and early diagnosis of burn injuries before organism invade and body loss surface epithelial that increase TBSA of burn patients.
In our study, IV fluid resuscitation was given for the majority of burn patients. The most frequently used fluid was lactated ringer, followed by normal saline and the combinations of lactated ringers and normal saline. This finding is similar to other previous studies.18,32 This can be explained by burn patient needs fluid resuscitation to maintain tissue perfusion and to halt the hypervolemia that can occur due to body response to burn injuries.
In this study, analgesics were prescribed for almost all burn patients for pain management. The most frequently prescribed agent was tramadol, followed by diclofenac and a combination of tramadol with diclofenac. This study consistent with other studies.13,25 This could be described by the burn injuries are painful and pharmacological and non-pharmacological treatment is needed to manage patients with a burn. In our study, surgical procedures were done for two-thirds of burn patients. Debridement is the common surgical procedure done followed by skin grafting and contractual release. This finding in line with other studies.18,38 This could be explained by, in order to facilitate the healing process of burn injuries in burn patients, the necrotic tissue should be removed and to preserve viable dermis in the wound bed.
Our finding indicated patients who undergo any of the surgical procedures were more than 4 times likely to stay in the hospital for greater than 30 days. A similar finding was reported from a study in Lebanon, where the length of hospital stay (LOS) was positively and significantly associated with having undergone an operation, as well as the number of operations.39 In this study, about 3.2% of burn patients died. This finding was lower compared to a review done in sub-Saharan countries3 and a study done in Yekatit 12 of Addis Ababa.15 The number of burn patients included in our study was relatively lower.
Limitations
The main strength of this study was, it was the first detailed report of burn patients from our Burn Unit. However, due to the time and financial feasibility, the sample size was relatively small and it was from a single institution. Thus, the generalization of the findings to other settings should be considered with caution.
Conclusions and Recommendations
Burn is a big public health problem, especially in the pediatric population. To halt the global problem occurs due to the burn trauma in developing countries, extensive preventive measure and early diagnosis and treatment of burn injuries should be implemented. Providing health education to health professionals, health extension, and the public on the appropriate handling of fire within the surrounding environment for children and other vulnerable during meal preparation and to visit health facilities as soon as burn injuries occur. Therefore, awareness creation through campaigns in the community and local media are essential to prevent burn. It is valuable if further research will be conducted on complications and the healing process of the burn.
Abbreviations
TBSA, total body surface area; JMC, Jimma Medical Center; IV, intravenous; OR, odds ratio; SD, standard deviation; IQR, interquartile range.
Data Sharing Statement
The data of this study are available from the corresponding author on reasonable request.
Ethics and Consent Statement
Ethical clearance was obtained from Jimma University Institutional Review Board (IRB). The ethics approval was given in accordance with the Declaration of Helsinki. The patient informed consent to review their medical records was waived by the ethics committee. Before the actual data collection, the confidentiality of the study subjects was taken into account by avoiding the names and any other personal identification information.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest for this work.
References
1. World Health Organization. Burns [factsheet]. World Health Organization. 2018;. Available from: https://www.who.int/news-room/fact-sheets/detail/burns.
2. American Burn Association. National Burn Repository. 2017 Update. American Burn Association; 2017. Available from: https://cdn.ymaws.com/ameriburn.site-ym.com/resource/collection/4C72F10C-24FD-401C-8608-417BFAB10138/2017_ABA_NBR_Annual_Report.pdf.
3. Nthumba PM. Burns in sub-Saharan Africa: a review. Burns. 2016;42(2):258–266. doi:10.1016/j.burns.2015.04.006
4. Rybarczyk MM, Schafer JM, Elm CM, et al. Revue systématique des cas de blessures par brûlure dans les pays à revenu faible et intermédiaire: épidémiologie dans la région africaine de l’OMS. African J Emerg Med. 2017;7(1):30–37. doi:10.1016/j.afjem.2017.01.006
5. Dongo AE, Irekpita EE, Oseghale LO, Ogbebor CE, Iyamu CE, Onuminya JE. A five-year review of burn injuries in Irrua. BMC Health Serv Res. 2007;7:1–5. doi:10.1186/1472-6963-7-171
6. Nguyen Nhu L, Ngo Minh Duc LN, Nam L. Epilepsy related burn injuries in developing country: an experience in National Burn Hospital. Burn Open. 2019;3(3):99–102. doi:10.1016/j.burnso.2019.05.003
7. Tyson AF, Boschini LP, Kiser MM, et al. Survival after burn in a sub-Saharan burn unit: challenges and opportunities. Bone. 2013.
8. Faldmo L, Kravitz M. Management of acute burns and burn shock resuscitation. AACN Adv Crit Care. 1993;4(2):351–366. doi:10.4037/15597768-1993-2013
9. American Burn Association. Advanced burn life support course; 2018. Available from: http://ameriburn.org/wp-content/uploads/2019/08/2018-abls-providermanual.pdf.
10. Al-Benna S. Fluid resuscitation protocols for burn patients at intensive care units of the United Kingdom and Ireland. GMS Ger Med Sci. 2011;9:1–7.
11. Romanowski KS, Carson J, Pape K, et al. American Burn Association Guidelines on the management of acute pain in the adult burn patient: a review of the literature, a compilation of expert opinion and next steps. J Burn Care Res. 2020;41(6):1152–1164. doi:10.1093/jbcr/iraa120
12. Singer AJ, Thode HC. National analgesia prescribing patterns in emergency department patients with burns. J Burn Care Rehabil. 2002;23(6):361–365. doi:10.1097/00004630-200211000-00001
13. Mengistu ND, Obsa MS, Gemeda LA. Burn pain management at burn unit of Yekatit 12 Hospitals, Addis Ababa. Pain Res Treat. 2018;2018. doi:10.1155/2018/1092650
14. Mulat T, Salemark LO. Description of patients admitted to a burn unit of Yekatit 12 Hosptial, Addis Ababa, Ethiopia. Ethiop Med J. 2006;44(4):369–375.
15. Mehta AK. Epidemiology of burns treated by Yekatit 12 burn unit in 2016. 2016. 7090.
16. Daniel E, Yoo MC. Survey of burn admissions to the Ethio-Swedish Children’s Hospital. Ethiop Med J. 1990;28(4):163–168.
17. Bulto LN, Dessie Y, Geda B. Magnitude, causes and characteristics of trauma victims visiting emergency and surgical units of Dilchora Hospital, Eastern Ethiopia. Pan Afr Med J. 2018;30:1–7. doi:10.11604/pamj.2018.30.177.10969
18. Alemayehu S, Afera B, Kidanu K, Belete T. Management outcome of burn injury and associated factors among hospitalized children at Ayder Referral Hospital. Int J Pediatr. 2020;2020.
19. Mamo Y, Alemu S, Seid E, Tiley C, Prevett M. The problem of epilepsy and its care in rural Ethiopia. Ethiop Med J. 2008;46(3):267–272.
20. Atiyeh BS, Costagliola M, Hayek SN. Burn prevention mechanisms and outcomes: pitfalls, failures and successes. Burns. 2009;35(2):181–193. doi:10.1016/j.burns.2008.06.002
21. Mohammed M, Mekonen Y, Berhe H. Clinical profile of pediatric burn patients in burn care unit of Halibet Hospital in 2018: Asmara, Eritrea. Pediatr Heal Med Ther. 2021;12:13–21.
22. Negesa R, Shitsinzi R, Emarah A. Heliyon clinical patterns and early outcomes of burn injuries in patients admitted at the Moi Teaching and Referral Hospital in Eldoret, Western Kenya. Heliyon. 2020;6(3):e03629. doi:10.1016/j.heliyon.2020.e03629
23. Forbinake NA, Dongmo G, Ohandza CS, Chichom-Mefire A, Fokam P, Beyiha G. Epidemiologic and clinical profile of burns in a tertiary hospital in Sub-Saharan Africa. Burn Open. 2020;4(1):22–27. doi:10.1016/j.burnso.2019.10.001
24. Tian H, Wang L, Xie W, et al. Epidemiologic and clinical characteristics of severe burn patients: results of a retrospective multicenter study in China, 2011–2015. Burn Trauma. 2018;6:1–11. doi:10.1186/s41038-018-0118-z
25. Akhtar MS, Ahmad I, Khan AH, Fahud Khurram M, Haq A. Burn injury in epileptic patients: an experience in a tertiary institute. Ann Burns Fire Disasters. 2014;27(3):126–129.
26. Verma A, Verma S, Moses S, et al. Burn injury in epileptic patients- a retrospective-descriptive study in a tertiary burn care unit. J Evol Med Dent Sci. 2017;6(94):6808–6811. doi:10.14260/jemds/2017/1474
27. Ansari Z, Brown K, Carson N, Ackland M. Association of epilepsy and burns: a case control study. Aust Fam Physician. 2008;37(7):584–589.
28. Oladele AO, Olabanji JK. Burns in Nigeria: a review. Ann Burns Fire Disasters. 2010;23(3):120–127.
29. Al-Shamsi M, Othman N. The epidemiology of burns in Basra, Iraq. Ann Burns Fire Disasters. 2017;30(3):167–171.
30. Aghakhani N, Nia HS, Soleimani MA, et al. Prevalence burn injuries and risk factors in persons older the 15 years in Urmia burn center in Iran. Casp J Intern Med. 2011;2(2):240–244.
31. Pavoni V, Gianesello L, Paparella L, Buoninsegni LT, Barboni E. Outcome predictors and quality of life of severe burn patients admitted to intensive care unit. Scand J Trauma Resusc Emerg Med. 2010;18(1):24. doi:10.1186/1757-7241-18-24
32. Wang S, Li D, Shen C, et al. Epidemiology of burns in pediatric patients of Beijing City. BMC Pediatr. 2016;16(1):1–7. doi:10.1186/s12887-016-0686-7
33. Babakir-Mina M. Characteristics of burn injury and factors in relation to infection among pediatric patients. MOJ Gerontol Geriatr. 2017;1(3):57–66. doi:10.15406/mojgg.2017.01.00013
34. Li H, Yao Z, Tan J, et al. Epidemiology and outcome analysis of 6325 burn patients: a five-year retrospective study in a major burn center in Southwest China. Sci Rep. 2017;7(1):1–9. doi:10.1038/s41598-016-0028-x
35. Brusselaers N, Monstrey S, Vogelaers D, Hoste E, Blot S. Severe burn injury in Europe: a systematic review of the incidence, etiology, morbidity, and mortality. Crit Care. 2010;14(5):1–12. doi:10.1186/cc9300
36. Garcia-Espinoza JA, Aguilar-Aragon VB, Ortiz-Villalobos EH, Burns AB. Definition, classification, pathophysiology and initial approach. Gen Med. 2017;5(5).
37. Chakraborty S, Bisoi S, Chattopadhyay D, Mishra R, Bhattacharya N, Biswas B. A study on demographic and clinical profile of burn patients in an Apex Institute of West Bengal. Indian J Public Health. 2010;54(1):27–29. doi:10.4103/0019-557X.70545
38. McGill V, Kowal-Vern A, Gamelli RL. Outcome for older burn patients. Arch Surg. 2000;135(3):320–325. doi:10.1001/archsurg.135.3.320
39. Bourgi J, Yaacoob E, Berberi M, et al. Factors affecting length of stay among pediatric and adult patients admitted to the lebanese burn centre: a retrospective study. Ann Burns Fire Disasters. 2019;32(3):216–221.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.