Back to Journals » International Journal of Nephrology and Renovascular Disease » Volume 14
Clinical Profile and Short-Term Outcomes of Acute Kidney Injury in Patients Admitted to a Teaching Hospital in Ethiopia: A Prospective Study
Authors Abebe A , Kebede B , Wobie Y
Received 4 May 2021
Accepted for publication 22 June 2021
Published 2 July 2021 Volume 2021:14 Pages 201—209
DOI https://doi.org/10.2147/IJNRD.S318037
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Pravin Singhal
Abinet Abebe, Bezie Kebede, Yohannes Wobie
Clinical Pharmacy, School of Pharmacy, College of Health and Medical Sciences, Mizan Tepi University, Mizan, Ethiopia
Correspondence: Abinet Abebe Email [email protected]
Background: Acute kidney injury (AKI) is a common complication in hospitalized patients and a marker for poor patient outcomes. It is associated with a high risk of mortality and other short- and long-term adverse outcomes. We aim to assess the clinical profile and short-term outcomes of acute kidney injury in adult patients admitted to the medical ward.
Methods: A hospital-based prospective observational study was conducted from October 2019 to January 2020. All adult patients diagnosed as AKI using kidney disease improving global outcomes (KIDGO) criteria were included in the study and prospectively followed to document the short-term outcomes. Outcomes and their predictors were determined using multivariate logistic regression. P-value less than 0.05 was taken as statistically significant.
Results: A total of 160 patients were included in the study. Out of this, 96 (60%) were males, 118 (74%) had community-acquired AKI, and 51 (32%) had stage 3 AKI. Common causes of AKI were hypovolemia 62 (39%) and sepsis 35 (22%). Hypertension 69 (43%) and heart failure 50 (31%) were common underlying comorbidities. Fifty-six (35%) patients developed systemic complications, 98 (61.2%) had persistent AKI, 136 (85%) had prolonged length of hospital stay, and 18 (11%) were readmitted to the hospital. The presence of AKI-related complication (AOR=2.7, 95% CI: 1.14– 6.58, p=0.024), and duration of AKI (AOR=9.7, 95% CI: 2.56– 36.98, p=0.001) were factors associated with prolonged length of hospital stay. Preexisting CKD (AOR=3.6, 95% CI: 1.02– 13.14, p=0.035) and stage 3 AKI (AOR=2.1, 95% CI: 1.6– 3.57, p=0.04) were factors associated with 30-day hospital readmission.
Conclusion: Hypovolemia and infections were the primary causes of AKI. Complications, prolonged length of hospital stay, persistent AKI, and rehospitalization were poor short-term outcomes of AKI. Early diagnosis and timely management of AKI particularly in high-risk hospitalized patients, and post-AKI care including management of comorbidities for AKI survivors should improve these poor short-term outcomes.
Keywords: acute kidney injury, short-term outcomes, Ethiopia
Key Summary Points
Why Was the Study Done?
- Relatively little is known about the prevalence of acute kidney injury and its short- and long-term adverse outcomes in low- to middle-income countries. Despite advances in renal replacement therapy and supportive measures, patients with AKI are at an increased risk of mortality, over both the short and long term, complications, progression to chronic kidney disease (CKD), ESRD, cardiovascular events, and reduced quality of life.
- This study aimed to assess the clinical profile and short-term outcomes among patients with acute kidney injury admitted to the renal units of the medical ward.
What Was Learned from the Study?
- Eighty-five percent of patients had prolonged length of hospital stay. One-third of patients develop AKI-related systemic complications, two-third of patients had a long duration of AKI, and around eleven percent of patients readmitted to the hospital during the study period. AKI-related complications and long duration of AKI were independently associated with prolonged length of hospital stay. Severe stage of AKI and preexisting CKD were predictors of thirty-day readmission.
- Early identification and timely management of AKI, particularly in high-risk patients, and post-AKI care for survivors of an AKI episode may improve these worse short-term outcomes of AKI.
Background
Acute kidney injury (AKI) is a clinical syndrome with multiple etiologies. It is a common complication in hospitalized patients, and is associated with several short- and long-term adverse outcomes.1,2 Developing AKI is a marker for poor outcomes. The mortality rate is 20% during hospital admission and rises above 35% in patients with stage 3 AKI.3
Survivors of an AKI episode are shown to be at an increased risk of long-term adverse outcomes including, mortality, chronic kidney disease, end-stage renal disease, cardiovascular events, and reduced quality of life. AKI has been reported to be associated with a 58% increased risk of heart failure, 40% increased risk of acute myocardial infarction, and 15% of stroke.4–7 The association of AKI with short-term adverse outcomes is well recognized, and causes major patient and public health burden in terms of complications, need for renal replacement therapy, increased length of hospital stays, hospital readmission, and costs of treatment. Moreover, AKI-related complications are associated with an increased risk of in-hospital mortality, especially in severe AKI.8–10
In low- and middle-income countries, AKI imposes difficult challenges due to the lack of data on the epidemiology and causes of AKI, the limited health care resources to diagnose and treat AKI, and the poor awareness of the outcomes of AKI.11 Therefore, this study aimed to assess the clinical profile and short-term outcomes of acute kidney injury in single-center hospitalized patients.
Materials and Methods
Study Design and Population
This is a single center prospective observational study involving all adult patients with the diagnosis of acute kidney injury from October 2019 to January 2020 at Jimma Medical Center (JMC), southwest Ethiopia. JMC is the only teaching and referral hospital in the southwestern part of Ethiopia. The hospital has two renal units and a dialysis center. The sample size was determined by using single population proportion formula. Patients with age above 18 years and willing to sign written informed consent were included in the study. Patients hospitalized for less than 48 hours and patients with known ESRD or who were on dialysis for AKI at study enrollment were excluded from the study.
Definitions
AKI was defined according to the KDIGO 2012 AKI criteria: (i) an increase in Scr by ≥0.3 mg/dl within 48 hours, OR (ii) an increase in Scr to ≥1.5 times baseline within the prior 7 days, and (iii) Urine volume < 0.5 mL/kg/h for 6 hours. The baseline serum creatinine used for hospital-acquired AKI was the first documented serum creatinine on admission.2 For community-acquired AKI, (i) Prehospital record of creatinine within seven days to three months of hospital admission, whichever available, or (ii) The minimum and/or most recent value of admission serum creatinine was used as baseline.12–14 Duration of AKI was defined as the number of consecutive days from the first day the patient met the AKI criteria until they no longer did. Persistent and transient AKI were defined according to the Acute Disease Quality Initiative (ADQI) definitions.15 Patients were classified into three groups based on the duration of AKI: (i) short duration of AKI (1–2 days), (ii) medium duration of AKI (3–7 days), and (iii) persistent AKI (AKI lasted greater than 7 days). This is based on a review of previous studies chosen for comparison.16,17 Prolonged length of hospital stay was defined as hospital stays greater than seven days.18 Renal recovery was defined as a return to premorbid or baseline kidney function at hospital discharge.
Statistical Analysis
Epi data version 4.4.2 was used to enter and export data. All of the analyses were performed using SPSS version 26.0. The data were presented as means ± standard deviation (SD) for continuous variables and as frequency and proportions for categorical variables. The Chi-square test was used for the comparison of proportions of categorical variables. The logistic regression model was used to determine factors associated with prolonged length of hospital stay and 30-day hospital readmissions. Odds Ratios (OR), P-values, and 95% confidence intervals were used to describe associations. Variables with a P value of less than 0.25 from the univariate analysis were included. Statistical significance was considered at the p-value of less than 0.05 on multivariate logistic regression.
Outcome Measures
The primary outcome variables were duration of AKI, length of hospital stay, and complications. The secondary outcome variable was 30-day readmission. Patients were followed prospectively from the diagnosis of AKI to discharge from the hospital.
Results
Sociodemographic and Clinical Characteristics of Patients
A total of 164 patients were included in the study from October 2019 to January 2020. Four patients who were not willing to participate in the study were excluded. Of the 160 patients, 96 (60%) were males, and 124 (77.5%) were rural dwellers. The median age was 46 years, and the mean age was 47.51±14.52 years, while the minimum and maximum ages of patients were 18 and 76 years respectively. Thirty-three (21%) patients had a history of alcohol consumption, and 12 (7.5%) patients had a history of smoking. Out of 160 patients, 118 (74%) had community-acquired AKI and the remaining 42 (26%) had hospital-acquired AKI. Using the KIDGO criteria, 51 patients (32%) were classified as stage 3 AKI, 73 (45.5%) as stage 2 AKI, and 36 (22.5%) as stage 1 AKI. Based on urine output status, 84 patients (53%) were non-oliguric, 63 (39%) oliguric, and 13 (8%) anuric. Anemia, edema and uremic syndrome (pericarditis, encephalopathy, gastropathy, bleeding diathesis) were common presenting features for patients with the severe stage of the disease. The presence of anuria and oliguria were other clinical manifestations at hospital admission (Table 1).
 |
Table 1 Sociodemographic and Clinical Characteristics of Patients |
Causes and Comorbidities of AKI
The most common causes of AKI were hypovolemia 62 (39%), sepsis 35 (22%), and pyelonephritis 18 (11%). Thirty (19%) patients had unspecified causes of AKI. One-third of patients (33%) had infectious causes of AKI. Common underlying comorbidities identified were hypertension 69 (43%) followed by heart failure 50 (31%) and diabetes 23 (14%). The remaining 28 (17.5%) patients had preexisting CKD (Table 1).
Laboratory Values
At admission, serum creatinine of patients ranged from 1.59 to 18.4mg/dl, with a mean of 4.17 ± 3.43 mg/dl. At discharge, the mean level of serum creatinine was 3.34±2.88mg/dl. The results for selected laboratory values are summarized in Table 2.
 |
Table 2 Selected Laboratory Values at JMC, Southwest Ethiopia |
Short-Term Outcomes of AKI
Complications
Overall, 56 (35%) patients develop systemic complications. Out of 118 (74%) community-acquired AKI patients, 39 (33%) develop complications on admission. Of the 42 (26%) patients with hospital-acquired AKI, 17 (40.5%) develop complications during their hospital stay. The lists of systemic complications of AKI are outlined in Table 1.
Duration of AKI
Of the 160 patients, 15 (9.4%) had short-duration AKI (1–2 days), 47 (29.4%) had a medium-duration AKI (3–7 days), and 98 (61.2%) had persistent AKI (>7 days). The average duration of AKI was 6.5 days. The median AKI duration was 6 days. Those patients with persistent AKI were patients with age ≥60 years, preexisting CKD, hypertension, and heart failure comorbidities and had a higher maximum AKI stage compared to patients with medium- and short-duration AKI (Table 3).
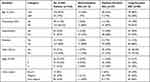 |
Table 3 Baseline and Clinical Characteristics of Patients Stratified by AKI Duration |
Length of Hospital Stay
Out of the study patients (n=160), 136 (85%) had prolonged length of hospital stay (length of hospital stay greater than seven days). The length of hospital for the patients ranges from 3 to 19 days with an average of 10.7 days. Patients who experienced prolonged length of hospital stay were patients with community-acquired AKI 98 (83%), stage 3 AKI 46 (90%), AKI on CKD 25 (89%), CHF 43 (86%), hypertension 61 (88%), diabetes 17 (74%), and systemic complications 47 (84%) than patients with a short length of hospital stay. The presence of AKI related complications (AOR 2.7, 95% CI: 1.14–6.58, p=0.024) and persistent AKI (AOR 9.7, 95% CI: 2.56–36.98, p=0.001) were factors associated with prolonged length of hospital stay (Table 4).
 |
Table 4 Factors Associated with Prolonged Length of Hospital Stay (n=136) |
30-Day Readmission
Eighteen (11%) patients were readmitted to the hospital during the study. Of the readmitted patients (n=18), 8 (44.4%), 4 (22.3%), and 6 (33.3%) patients had AKI on CKD, rapidly progressive glomerulonephritis (RPGN), and history of systemic complications, respectively, during the previous hospital stay. The most common causes of readmission were hypertension (n=4) and heart failure (n=5) and CKD (n=0.9). On multivariate logistic regression, stage 3 AKI (AOR 2.1, CI: 1.6–3.57, p=0.04) and preexisting CKD (AOR 3.6, CI: 1.02–13.14, p=0.035) were factors significantly associated with 30-day readmission (Table 5).
 |
Table 5 Factors Associated with 30-Day Readmission (n=18) |
Other Outcomes
A total of 11 (7%) patients needed renal replacement therapy. Of those patients who required renal replacement therapy, 7 (4%) patients had preexisting CKD. The main indications of the need for renal replacement therapy were severe hyperkalemia (42%), uremic syndrome (29%), refractory edema (17%), and metabolic acidosis (12%). The overall in-hospital mortality rate was 6% (n=9). Some evidence of renal recovery was observed in 75% of patients at hospital discharge.
Discussion
AKI is shown to be associated with increased length of hospital stay, complications, progression to CKD and ESRD, mortality, and increased costs of treatment.3,9,10 As the first prospective study on adult medical ward admissions, the study provides information on clinical profile and short-term outcomes of acute kidney injury in the area. Knowing the clinical profile and short-term prognosis of acute kidney injury is important for the institution of appropriate preventive and management strategies.
According to this study, the most commonly affected populations were males, and those aged less than 60 years. This is consistent with other studies in developing countries, where most patients affected are males, healthier, and middle-aged, respectively.11,19 The reason might be due to the presence of infectious causes of AKI in the younger population which is evident in our study, where around one-third of patients (33%) have infectious causes of AKI. Some of the epidemiologic features of AKI in this study are similar with that of developed countries. There is relatively higher percentage of elderly population (19%) and high prevalence of comorbidities (hypertension, heart failure, diabetes, preexisting CKD) in our study compared with a previous study done in Addis Ababa, Ethiopia.20 The high prevalence of AKI in the elderly in our study might be due to the presence of these comorbidities that accumulate with age.
The etiological pattern of AKI is shown to be different between developing and developed countries. In developed countries, AKI is reported to be hospital-acquired, occurs in critically ill patients, and usually elderly.11 In this study, we found that 74% of patients had community-acquired AKI, and the common causes of AKI were hypovolemia, sepsis, pyelonephritis, and glomerulonephritis. This is consistent with studies done in developing countries where AKI is shown to be community-acquired21,22 and usually caused by hypovolemia, infections, and AGN.19,20,23
More than half (56%) of patients develop systemic complications. Patients with AKI-related complications (severe hyperkalemia, refractory edema, and metabolic acidosis) usually require treatment with renal replacement therapy (RRT), which is costly and unaffordable for most patients especially in resource-limited settings.19,20 The main indications for renal replacement therapy in this study were hyperkalemia, uremic syndrome, refractory edema, and metabolic acidosis. The presence of any systemic complication was associated with an increased length of hospital stay (p<0.05).
We found that 61.2% of patients had persistent AKI. This is higher than a report from a previous study where most patients have resolving AKI.16 The difference might be due to the presence of higher maximum AKI stage and underlying comorbidities in patients with persistent AKI in our study. Previous studies showed that persistent AKI is associated with a higher risk of long-term mortality, cardiovascular events, increased length of hospital stay, and progression to CKD.16,24 Therefore, early identification of patients with persistent AKI is important to initiate management and preventive strategies to avoid further kidney damage and progression to CKD, and increased risk of mortality.
Many studies have demonstrated an association between AKI and increased length of hospital stay.9,18,25 Our study showed that 85% of patients have prolonged lengths of hospital stay. The presence of systemic complications and persistent acute kidney injury were associated with prolonged length of stay (p<0.05). The increased length of hospital stay in our study might be due to the need for management of patients with complications associated with acute kidney injury especially in severe cases. Other studies also demonstrated that complications associated with acute kidney injury and persistent AKI can have worse outcomes in terms of mortality, length of stay, need for renal replacement therapy, and costs of treatment.10,20,24,26,27 Therefore, clinicians should focus on the prevention and management of these complications in addition to the general management of AKI, to prevent these poor outcomes.
Previous studies showed that AKI is a frequent and independent risk factor for unplanned hospital readmissions. Compared with patients without AKI, survivors of AKI experience more than a 50% increased risk of hospital readmission.8,28 In the present study, 11% of patients were readmitted to the hospital during the study period. This is lower than a result reported by previous studies, where AKI is associated with 18% thirty-day and 39.9% five-year readmissions.29 The difference with these studies might be due to differences in sample size and duration of the study. In our study, severe stage of AKI and preexisting CKD were factors associated with 30-day hospital readmission. Similarly, report from a previous study showed that the severity of AKI is associated with increased rate of readmissions.29 The reasons for rehospitalization in our study might be due to lack of follow-up programs and post-discharge management strategies for AKI survivors in the community. Post discharge care should be implemented for AKI survivors, including management of their comorbidities.
Our study has some limitations. Outcome assessment was not performed beyond the period of hospitalization. Therefore, the incidence of CKD and ESRD after AKI, mortality rate, and other non-renal outcomes are not known.
Conclusion
In conclusion, the pattern of AKI in our study showed overlapped features of both developed and developing countries. The majority of patients had community-acquired AKI. Hypovolemia and sepsis were the dominant etiological profiles of AKI. Hypertension and heart failure were common underlying comorbidities. Anemia, edema, uremic syndrome, anuria, and oliguria were common presenting features at hospital admission. We found that increased length of hospital stay, complications, persistent AKI, and thirty-day readmissions were poor short-term outcomes associated with AKI. Presence of AKI-related complications and persistent AKI was independently associated with increased length of hospital stay. Preexisting CKD and severe stage of AKI were associated with thirty-day readmissions. Early diagnosis and timely management of AKI, particularly in high-risk hospitalized patients, and post-AKI care for AKI survivors should improve these poor short-term outcomes of AKI.
Abbreviations
ADQI, Acute Disease Quality Initiative; AGN, acute glomerulonephritis; AKI, acute kidney injury; CHF, congestive heart failure; CKD, chronic kidney disease; KIDGO, kidney disease improving global outcomes; ESRD, end-stage renal disease; JMC, Jimma Medical Center; UTI, urinary tract infections.
Data Sharing Statement
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval and Consent to Participate
The study was approved by the institutional review board (IRB) of the Institute of Health, Jimma University research ethics unit with reference number IHRPGA/574/2019. A letter of permission was forwarded to the administration of Jimma Medical Center. Informed consent was secured from all participants, and collected data were kept confidential. The study was conducted in accordance with the Helsinki Declaration. The study meets the ethical and scientific standards outlined in national and international guidelines.
Author Contributions
All authors made a significant contribution in the conception, study design, execution, acquisition of data, analysis and interpretation of the study reported, drafting, and editing of the final manuscript. All authors read and approved the final manuscript, and have agreed on the journal to which the article will be submitted. All authors agree to take responsibility and be accountable for the contents of the article.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Ostermann M, Joannidis M. Acute kidney injury 2016: diagnosis and diagnostic workup. Crit Care. 2016;20(1):1–13. doi:10.1186/s13054-016-1478-z
2. KIDGO. Clinical practice guideline for acute kidney injury. Off J Int Soc Nephrol. 2012;2(1).
3. Selby NM, Kolhe NV, Mcintyre CW, Monaghan J, Lawson N. Defining the cause of death in hospitalised patients with acute kidney injury. PLoS One. 2012;7(11):11. doi:10.1371/journal.pone.0048580
4. Lewington. AJP, Cerdá J, Mehta RL Raising awareness of acute kidney injury: a global perspective of a silent killer. Kidney Int. 2013;1–11.
5. Chang C-H, Fan P-C, Chang M-Y, et al. Acute kidney injury enhances outcome prediction ability of sequential organ failure assessment score in critically ill patients. PLoS One. 2014;9(10).
6. Linder A, Fjell C, Levin A, Walley KR, Russell JA, Boyd JH. Long-term survival after critical illness with acute kidney injury. Am J Respir Crit Care Med. 2014;189(9):1075–1081. doi:10.1164/rccm.201311-2097OC
7. Odutayo A, Wong CX, Farkouh M, et al. AKI and long-term risk for cardiovascular events and mortality. J Am Soc Nephrol. 2017;28(1):377–387. doi:10.1681/ASN.2016010105
8. Silver SA, Harel Z, McArthur E, et al. 30-day readmissions after an acute kidney injury hospitalization. Am J Med. 2017;130(2). doi:10.1016/j.amjmed.2016.09.016
9. Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol. 2005;16(11):3365–3370. doi:10.1681/ASN.2004090740
10. Libório AB, Leite TT, Neves FMDO, Teles F, Bezerra CTDM. AKI complications in critically ill patients: association with mortality rates and RRT. Clin J Am Soc Nephrol. 2015;10(1):21–28. doi:10.2215/CJN.04750514
11. Ponce D, Balbi A. Acute kidney injury: risk factors and management challenges in developing countries. Dove press International. J Nephrol Renov Dis. 2016;9:193–200. doi:10.2147/IJNRD.S104209
12. Siew ED, Ikizler TA, Matheny ME. Estimating baseline kidney function in hospitalized patients with impaired kidney function. Clin J Am Soc Nephrol. 2012;7(5):712–719. doi:10.2215/CJN.10821011
13. Thongprayoon C, Cheungpasitporn W, Kittanamongkolchai W, et al. Optimum methodology for estimating baseline serum creatinine for the acute kidney injury classification. Asian Pacific Soc Nephrol. 2015;20:881–886.
14. Siew ED, Matheny ME. Choice of reference serum creatinine in defining acute kidney injury. Nephron Clin Pract. 2015;131:107–112.
15. Chawla LS, Bellomo R, Bihorac A, et al. Acute kidney disease and renal recovery: consensus report of the Acute Disease Quality Initiative (ADQI) 16 Workgroup. Nat Rev. 2017. doi:10.1038/nrneph.2017.2
16. Federspiel CK, Itenov TS, Mehta K, et al. Duration of acute kidney injury in critically ill patients. Ann Intensive Care. 2018;8(30):1–9. doi:10.1186/s13613-018-0374-x
17. Bellomo R, Ronco C, Mehta RL, et al. Acute kidney injury in the ICU: from injury to recovery: reports from the 5th Paris International Conference. Ann Intensive Care. 2017;7(49):1–40. doi:10.1186/s13613-016-0221-x
18. Amrish S, Prasad R, Verma K, et al. Factors predicting length of hospital stay in acute kidney injury patients admitted in a rural tertiary care hospital. Acta Sci Med Sci. 2017;1(2):19–23.
19. Oluseyi A, Ayodeji A, Ayodeji F. Aetiologies and short-term outcomes of acute kidney injury in a tertiary centre in Southwest Nigeria. Ethiop J Heal Sci. 2016;26(1):37. doi:10.4314/ejhs.v26i1.8
20. Ibrahim A, Ahmed MM, Kedir S, et al. Clinical profile and outcome of patients with acute kidney injury requiring dialysis — an experience from a hemodialysis unit in a developing country. BMC Nephrol. 2016;17(91):1–5. doi:10.1186/s12882-016-0313-8
21. Evans RD, Hemmilä U, Craik A, et al. Incidence, aetiology and outcome of community-acquired acute kidney injury in medical admissions in Malawi. BMC Nephrol. 2017;18(21):1–9.
22. Dlamini TAL, Heering PJ. A prospective study of the demographics, management, and outcome of patients with acute kidney injury in Cape Town, South Africa. PLoS One. 2017;145:1–12.
23. Krishnamurthy S, Narayanan P, Prabha S, et al. Clinical profile of acute kidney injury in a pediatric intensive care unit from Southern India. Indian J Crit Care Med. 2013;17(4):207–213. doi:10.4103/0972-5229.118412
24. Mehta S, Chauhan K, Patel A, et al. The prognostic importance of duration of AKI: a systematic review and meta-analysis. BMC Nephrol. 2018;19(91):1–10. doi:10.1186/s12882-017-0808-y
25. Fuhrman DY, Kane-Gill S, Goldstein SL, et al. Acute kidney injury epidemiology, risk factors, and outcomes in critically ill patients 16 – 25 years of age treated in an adult intensive care unit. Ann Intensive Care. 2018;8(26):1–11. doi:10.1186/s13613-018-0373-y
26. Ostermann M. Core concepts in acute kidney injury; 2018:1–373. doi:10.1007/978-1-4939-8628-6
27. Murugan R, Kellum JA. Acute kidney injury: what’s the prognosis? Nat Rev Nephrol. 2013;7(4):209–217. doi:10.1038/nrneph.2011.13
28. Sawhney S, Marks A, Fluck N, et al. Acute kidney injury as an independent risk factor for unplanned 90-day hospital readmissions. BMC Nephrol. 2017;18(9):1–13. doi:10.1186/s12882-016-0417-1
29. Brown JR, Hisey WM, Marshall EJ. Acute kidney injury severity and long-term readmission and mortality following cardiac surgery. Ann Thorac Surg. 2016;102(5):1482–1489. doi:10.1016/j.athoracsur.2016.04.020
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
