Back to Journals » Open Access Emergency Medicine » Volume 14
Clinical Prediction Score for Early Diagnosis of Acute Pancreatitis in Emergency Departments
Authors Liengswangwong W, Preechakul P, Yuksen C , Jenpanitpong C , Tienpratarn W , Watcharakitpaisan S
Received 29 April 2022
Accepted for publication 16 July 2022
Published 26 July 2022 Volume 2022:14 Pages 355—366
DOI https://doi.org/10.2147/OAEM.S371237
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Wijittra Liengswangwong, Pacharaporn Preechakul, Chaiyaporn Yuksen, Chetsadakon Jenpanitpong, Welawat Tienpratarn, Sorawich Watcharakitpaisan
Department of Emergency Medicine, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
Correspondence: Chaiyaporn Yuksen, Department of Emergency Medicine, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, 10400, Thailand, Email [email protected]
Background: In Thailand, most primary care hospitals cannot measure serum lipase and amylase; no 24 hours computed tomography and magnetic resonance imaging available, and no on-call gastroenterologists. Thus, acute pancreatitis cannot be diagnosed based on the established diagnostic criteria that require this information. The resultant delayed management increases morbidity and mortality. This study was performed to create a clinical prediction score for early diagnosis of acute pancreatitis in emergency departments without requiring a computed tomography scan or laboratory measurement to assist in the initial diagnosis, treatment, or referral.
Methods: Patients with suspected acute pancreatitis who had available data regarding lipase and amylase measurements and visited the emergency department from June 2019 to August 2020 were retrospectively analyzed. The baseline predictive factors were compared between patients with and without acute pancreatitis according to the 2012 revised Atlanta classification. Multivariable logistic regression was used to explore potential predictive factors and develop a clinical prediction score for the diagnosis of acute pancreatitis.
Results: A total of 506 eligible patients, 84 (16%) had acute pancreatitis. The PRE-PAN score [area under the receiver operating characteristics curve, 0.88; 95% confidence interval (CI), 0.84– 0.93] included six factors: alcohol drinking, epigastric pain, pain radiating to the back, persistent pain, nausea or vomiting, and the pain score. A score of > 7.5 points suggested a high probability of acute pancreatitis [positive likelihood ratio, 6.80 (95% CI, 4.75– 9.34; p < 0.001); sensitivity, 66.7% (95% CI, 54.6– 77.3); specificity, 90.2% (95% CI, 86.6– 93.1); positive predictive value, 58.5% (95% CI, 47.1– 69.3);, 92.9% (95% CI, 89.6– 95.4)].
Conclusion: A PRE-PAN risk score is a screening tool for predicting acute pancreatitis without using the lipase concentration or radiological findings. A high predictive score, especially > 7.5, suggests a high probability of acute pancreatitis.
Keywords: prediction score, prediction model, clinical diagnostic score, acute pancreatitis
Background
Acute pancreatitis is an inflammatory process of the pancreas characterized by severe acute epigastric or left upper quadrant abdominal pain. Two-thirds of patients with acute pancreatitis also have severe abdominal pain radiating to the back,1 which is the third most common cause of hospitalization,3 and the prevalence is 13 to 45 per 100,000 population per year.4,5 The incidence has been rising worldwide due to the increase in obesity and gallstone disease.2,5 In most cases, the severity of acute pancreatitis is mild; however, about 15% to 20% of cases are severe. Although the overall mortality is about 5%, the mortality and morbidity of severe acute pancreatitis are as high as 15% to 20%.1,7,8
About 20% to 30% of patients have recurrent acute pancreatitis. Of these patients, about 10% develop chronic pancreatitis, and some develop pancreatic cancer.5 Reports from both Thailand and Western countries have produced similar results. Gallstones (40–45%) and chronic alcohol intake (15–25%) are the two most common causes of acute pancreatitis, whereas 15% to 20% of cases are idiopathic.6
A diagnosis of acute pancreatitis must meet two of the three diagnostic criteria.10,11 These criteria are characteristic signs and symptoms (acute abdominal pain or severe epigastric pain radiating to the back), abnormal laboratory test results (serum lipase or serum amylase concentration greater than or equivalent to three times the usual maximum), and abnormal radiological findings on contrast-enhanced computed tomography (CT) or magnetic resonance imaging (MRI).
The primary care hospitals in Thailand cannot measure serum lipase and amylase, no diagnostic radiology equipment (CT/MRI), and no on-call gastroenterologist. Moreover, without a diagnosis of acute pancreatitis, risk stratification is delayed, and without risk stratification, the resource allocation is not optimal, and this can potentially compromise clinical outcomes.11,12
Literature reviews in Thailand, Japan, and Western countries have shown that acute pancreatitis is higher among men aged 45 to 74 years.1,4,5 Risk factors for acute pancreatitis include a history of chronic alcohol intake, smoking, acute alcohol drinking,5,13 diabetes,14,15 high triglycerides,16 and gallstones.5
Recent studies have focused on establishing prediction scores for the diagnosis of acute pancreatitis by using clinical and serum lipase17 or abdominal CT findings as diagnostic criteria. However, no such studies have been performed in Thailand. Thus, no published studies contain data that can be used in rural primary care hospitals where serum lipase measurement or radiologic diagnostic imaging by CT/MRI is unavailable.
Therefore, the present study focused on establishing a prediction score for early diagnosis of acute pancreatitis without using the serum lipase or amylase concentration or diagnostic radiology (CT/MRI). Using clinical signs and symptoms and laboratory indices such as an alanine aminotransferase concentration of >150 IU/L can help clinicians anticipate the development of biliary tract problems.8 This study was performed to create a clinical prediction score for early diagnosis of acute pancreatitis in emergency departments (ED) without depending on a CT scan or serum lipase measurement to assist in the initial diagnosis, treatment, or referral.
Methods
Study Design
This retrospective cohort study was designed to establish a diagnostic prediction model conducted at the ED of Ramathibodi Hospital, a university-affiliated super-specialty tertiary care hospital in Bangkok, Thailand. Using the Ramathibodi Hospital database, we identified all patients who visited the ED from 1 June 2019 to 31 August 2020 according to the laboratory codes 200,017 (amylase) and 200,108 (lipase). None of the data used in this study revealed the patients’ identities. We replaced the patients’ names with their hospital numbers.
Sample Size
To calculate the sample size, we did the pilot study. We searched the Ramathibodi Hospital database to obtain the lipase and amylase data of the patients who had visited the ED of Ramathibodi Hospital with suspected acute pancreatitis from 1 November 2019 to 29 February 2020. We used the hospital’s emergency medical record (EMR) and radiologic diagnostic data (CT, MRI, and ultrasound findings). In total, 8 (23%) patients had acute pancreatitis, and 27 (77%) did not. The ratio of patients with acute pancreatitis to those without was 1:3.
Our pilot study used Stata version 16.0 analysis software (StataCorp, College Station, TX, USA) to calculate the sample size by employing a two-sample comparison of the populations of patients with and without acute pancreatitis. The assumptions were as follows: alpha = 0.05 (two-sided test), power of sample size = 0.8, and ratio of sample size = 1:3. The sample size of the population with acute pancreatitis was 120, and the sample size of the population without acute pancreatitis was 400.
Participants
All patients with suspected acute pancreatitis included in this study were required to have visited the ED of Ramathibodi Hospital from 1 June 2019 to 31 August 2020 and have data on their lipase and amylase levels. We excluded those with no radiologic diagnostic test data (CT/MRI/ultrasound), had missing data, had repeated data, were <18 years old, had trauma, and had a history of peritoneal metastasis. The patients were divided into two groups: those diagnosed with acute pancreatitis according to the 2012 revised Atlanta classification and those who did not meet the diagnostic criteria. The study protocol is shown in Figure 1.
 |
Figure 1 Study flow diagram of participants. |
Data Collection and Study Variables
The baseline predictive factors were sex, age, height, weight, body mass index, vital signs (temperature, heart rate, blood pressure, and respiratory rate), comorbidities, alcohol intake history, and smoking history. We also collected data on the patients’ abdominal pain characteristics (region, onset, and duration), pain score measured at the triage area in ED, gastrointestinal symptoms, laboratory findings (lipase, amylase, aspartate aminotransferase, alanine aminotransferase, total bilirubin, direct bilirubin, white blood cell count, blood urea nitrogen, and creatinine), and radiologic diagnostic findings (CT/MRI).
Statistical Analysis
Stata version 14 (StataCorp) was used to perform all statistical analyses. The baseline predictive factors were compiled in a table using descriptive statistics. Categorical data are presented as frequency and percentage, and continuous data are presented as mean and standard deviation. The potential predictors were compared between patients with and without acute pancreatitis (mean and Student’s t-test were used for continuous data, and proportion and exact probability test were used for categorical data), and a measure of the power of discrimination between two groups with the area under the receiver operating characteristics curve (AUROC) from all analyzed variables. We selected a suitable potential predictor and included it in the equation. Next, a ROC curve was created to determine how the calculated risk score can discriminate by predicting events in the logistic model. We also examined how the calculated risk score can discriminate by predicting events with a risk score in the logistic model. The Hosmer–Lemeshow goodness-of-fit test was then used to assess the predictions’ accuracy and present the actual occurrences.
Finally, the events predicted by the risk score were compared with the actual events. The proportion and percentage of patients with and without acute pancreatitis received a risk score, expressed as a positive likelihood ratio with 95% CI and p-value.
Results
Among 1,116 patients who visited the ED of Ramathibodi Hospital and underwent lipase and amylase measurement from March 2020 to September 2021, 506 were eligible for participation in this study. According to the 2012 revised Atlanta classification, 84 patients were diagnosed with acute pancreatitis. Among the 422 patients without acute pancreatitis, the most common diagnoses were cholangitis (n = 89, 21%), cholecystitis (n = 72, 17%), dyspepsia (n = 33, 8%), bowel obstruction (n = 32, 8%), symptomatic gallstones (n = 30, 7%), enteritis (n = 15, 4%), and hepatitis (n = 13, 3%). A flow diagram of the study is presented in Figure 1.
The variables were identified and categorized into 4 groups: (1) demographic variables, (2) medical comorbidities and history, (3) symptoms and signs, and (4) laboratory studies. Seven factors had high discriminative performance (AUROC curve) and were significantly associated with a diagnosis of acute pancreatitis: alcohol drinking, epigastric pain, pain radiating to the back, persistent pain, nausea or vomiting, and pain score. (Table 1).
 |
Table 1 Clinical Characteristics of Patients with Abdominal Pain Categorized by Presence and Absence of Acute Pancreatitis |
Multivariable analysis confirmed that each factor was predictive of acute pancreatitis with scores ranging from 0 to 11 by regression coefficients for each level of each clinical predictor were divided by the smallest coefficient of the model and rounded to the nearest 0 or 0.5. The multivariable analysis showed item score including pain score (score = 0, 1.5, 2.5), radiating to back (score = 0, 1), epigastrium pain (score = 0, 2), persistent pain (score = 0, 2.5), alcohol drinking (score = 0, 1.5) and nausea or vomiting (score = 0, 1.5). (Table 2).
 |
Table 2 Predictors of Acute Pancreatitis and Assigned Item Score in Patients with Suspected Acute Pancreatitis |
The AUROC of the clinical risk score showed 88% (95% CI, 0.84–0.93) power for predicting acute pancreatitis (Figure 2). The measures of calibration presented in Figure 3 show the observed risk (circle) and score-predicted risk (solid line) for acute pancreatitis. The score-predicted risk increased in close association with the observed risk. Finally, the risk scores were categorized into three groups: low risk (score of <5.0), intermediate-risk (score of 5.0–7.5), and high risk (score of >7.5) (Table 3). The positive likelihood ratio of acute pancreatitis in the high-risk group was 6.80. The risk score was termed the PRE-PAN risk score. (PRE-Pan score consists of pain-radiate- epigastrium-persistent-alcohol drinking-nausea).
 |
Table 3 Probability Categories of Acute Pancreatitis Risk Score, Likelihood Ratio of Positive (LHR+) and 95% Confidence Interval (CI) |
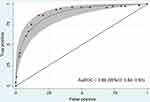 |
Figure 2 Area under the receiver operating characteristic curve (AUROC) and 95% confidence interval (CI) of the predictive power of the PRE-PAN score in patients with suspected acute pancreatitis. |
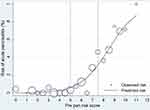 |
Figure 3 Measures of Hosmer–Lemeshow goodness-of fit test with PRE-PAN score [observed risk (circles) vs score-predicted risk (solid line) of acute pancreatitis]. |
The diagnostic performance of the PRE-PAN risk score is presented in Table 4. A PRE-PAN risk score of >5 showed a sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of 94.4% (95% CI, 86.4–98.5), 65.7% (95% CI, 60.4–70.7), 36.4% (95% CI, 29.5–43.7), and 98.3% (95% CI, 95.6–99.5), respectively. At our cut-off point of 7.5, the sensitivity, specificity, PPV, and NPV were 66.7% (95% CI 54.6–77.3), 90.2% (95% CI, 86.6–93.1), 58.5% (47.1–69.3), and 92.9% (89.6–95.4), respectively. The AuROC and 95% CI of the predictive power of PRE-PAN score compared with lipase in suspected acute pancreatitis patients are presented in Figure 4.
 |
Table 4 Prediction Score Performance Probabilities of Acute Pancreatitis at Different Cut-off Points |
Discussion
The present study evaluated the PRE-PAN score to diagnose acute pancreatitis. This score is user-friendly and accurate, allowing for rapid diagnosis of acute pancreatitis with excellent discriminatory accuracy (AUROC, 0.88; 95% CI, 0.84–0.93) (Figure 2) and high sensitivity according to the Hosmer-Lemeshow test (Figure 3). Notably, it requires only history and clinical information; no laboratory tests or radiological findings are needed. The score was generated using several predictors, including alcohol drinking, epigastric pain, pain radiating to the back, persistent pain, nausea or vomiting, and the pain score, all of which were identified using a multivariable logistic regression model (Table 2).
Acute pancreatitis should be highly suspected if the PRE-PAN score is >7.5 points (positive likelihood ratio, 6.8; 95% CI, 4.75–9.34; p < 0.001) (Table 3). Medical treatment, including intravenous hydration and enteral nutrition, and treating the underlying cause and complications should be initiated in such patients. The patient should be referred for definitive diagnosis, appropriate management, or specialty consultation.
Some studies of prediction scores for diagnosing acute pancreatitis have been published.9 However, they all use clinical presentation and serum lipase or abdominal CT findings as diagnostic criteria. Diagnosis of acute pancreatitis is challenging without serum lipase, radiologic diagnostic imaging (CT/MRI), and an on-call gastroenterologist. As a result, clinicians in this situation may hesitate to administer initial medical therapy to patients with suspected acute pancreatitis. This delay in management can increase morbidity and mortality.
Our study revealed significant diagnostic predictors of acute pancreatitis along with previous research, which identified the following predictors: pain characteristics (epigastric pain, upper abdominal pain, pain radiating to back, severe pain, pain score of 7–10, and persistent pain), nausea, prior acute pancreatitis, history of cholelithiasis, and serum lipase concentration. The predictive risk score for acute pancreatitis that included the lipase concentration identified in previous research had an estimated risk of at least 99% and at more than 8 points, and the specificity and PPV were both 100%. However, our PRE-PAN score had a specificity of 90.2% and PPV of 58.5%. The marked difference between our PRE-PAN score and the previous research score is caused by excluding the lipase concentration from the PRE-PAN score.
There is some prediction score for acute pancreatitis. The Ranson score is used to predict the severity of acute pancreatitis; the Bedside Index for Severity in Acute Pancreatitis (BISAP) score has been developed to predict at high risk for mortality and severity of acute pancreatitis patients, while the PRE-PAN score has been developed to early diagnosis of acute abdominal pain patients in ED. Pancreatitis diagnosis is not about lipase alone, and a PRE-PAN score can be helpful in early diagnosis.
Limitations
This study has some limitations. First, this study was retrospective in design. Many data were missing. The study was conducted in a single super-specialty tertiary care hospital and medical school; therefore, the characteristics of the patients differed from those of patients in rural primary care hospitals. Many patients with advanced-stage cancer were included, but we did not perform a subgroup analysis. The PRE-PAN risk score should be validated externally in primary care hospitals to establish its value and accuracy before clinical use.
Furthermore, about 50% of patients with suspected pancreatitis have no imaging available and were thus excluded from the study (the incidence of pancreatitis in this group of patients was unknown). Last, sometimes it is difficult to differentiate acute pancreatitis from biliary colic, acute cholecystitis, and choledocholithiasis/cholangitis. It depends on the onset/duration of symptoms. The final diagnosis was sometimes made during cholecystectomy; sometimes, the histopathological examination does not provide a definitive answer.
Conclusion
The PRE-PAN risk score is a screening tool for predicting acute pancreatitis. It includes seven parameters and does not require the use of the lipase concentration or radiological findings. A high predictive score, especially a score of >7.5, suggests a high probability of acute pancreatitis. However, we recommend prospective validation of the PRE-PAN risk score in primary care hospitals to establish the actual value and accuracy of the score before clinical use.
Abbreviations
CT, computed tomography; MRI, magnetic resonance imaging; ED, emergency departments; CI, confidence interval.
Data Sharing Statement
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was approved by the Faculty of Medicine, Committee on Human Rights Related to Research Involving Human Subjects, of Mahidol University’s Ramathibodi Hospital (COA. NO. MURA2020/466). The ethics committee did not require consent for this research because reviewing the medical record is the reason for the waiver and a statement covering patient data confidentiality and compliance with the Declaration of Helsinki.
Acknowledgments
We thank Angela Morben, DVM, ELS, from Edanz Group (www.edanzediting.com/ac), for editing a draft of this manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. Pongprasobchai S, Vibhatavata P, Apisarnthanarak P. Severity, treatment, and outcome of acute pancreatitis in Thailand: the first comprehensive review using revised Atlanta classification. Gastroenterol Res Pract. 2017;2017:3525349. doi:10.1155/2017/3525349
2. Iannuzzi JP, King JA, Leong JH, et al. Global incidence of acute pancreatitis is increasing over time: a systematic review and meta-analysis. Gastroenterology. 2022;162(1):122–134. doi:10.1053/j.gastro.2021.09.043
3. Forsmark CE, Vege SS, Wilcox CM. Acute pancreatitis. N Engl J Med. 2016;375:1972–1981. doi:10.1056/NEJMra1505202
4. Satoh K, Shimosegawa T, Masamune A, et al. Nationwide epidemiological survey of acute pancreatitis in Japan. Pancreas. 2011;40:503–507. doi:10.1097/MPA.0b013e318214812b
5. Yadav D, Lowenfels AB. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology. 2013;144:1252–1261. doi:10.1053/j.gastro.2013.01.068
6. Zilio MB, Eyff TF, Azeredo-Da-Silva AL, Bersch VP, Osvaldt AB. A systematic review and meta-analysis of the aetiology of acute pancreatitis. Hpb. 2019;21(3):259–267. doi:10.1016/j.hpb.2018.08.003
7. Teng TZJ, Tan JKT, Baey S, et al. Sequential organ failure assessment score is superior to other prognostic indices in acute pancreatitis. World J Crit Care Med. 2021;10(6):355–368. doi:10.5492/wjccm.v10.i6.355
8. Shah AP, Mourad MM, Bramhall SR. Acute pancreatitis: current perspectives on diagnosis and management. J Inflamm Res. 2018;11:77–85. doi:10.2147/JIR.S135751
9. Lankisch PG, Apte M, Banks PA. Acute pancreatitis. Lancet. 2015;386:85–96. doi:10.1016/S0140-6736(14)60649-8
10. Banks PA, Bollen TL, Dervenis C, et al. Classification of acute pancreatitis–2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102–111. doi:10.1136/gutjnl-2012-302779
11. Tenner S, Baillie J, DeWitt J, et al. American College of Gastroenterology. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013;108:1400–1415. doi:10.1038/ajg.2013.218
12. Vege SS, DiMagno MJ, Forsmark CE, Martel M, Barkun AN. Initial medical treatment of acute pancreatitis: American Gastroenterological Association Institute technical review. Gastroenterology. 2018;154(4):1103–1139. doi:10.1053/j.gastro.2018.01.031
13. Cote GA, Yadav D, Slivka A, et al. Alcohol and smoking as risk factors in an epidemiology study of patients with chronic pancreatitis. Clin Gastroenterol Hepatol. 2011;9(3):266–273. doi:10.1016/j.cgh.2010.10.015
14. Girman CJ, Kou TD, Cai B, et al. Patients with type 2 diabetes mellitus have higher risk for acute pancreatitis compared with those without diabetes. Diabetes Obes Metab. 2010;12(9):766–771. doi:10.1111/j.1463-1326.2010.01231.x
15. Noel RA, Braun DK, Patterson RE, et al. Increased risk of acute pancreatitis and biliary disease observed in patients with type 2 diabetes: a retrospective cohort study. Diabetes Care. 2009;32(5):834–838. doi:10.2337/dc08-1755
16. Lindkvist B, Appelros S, Regner S, et al. A prospective cohort study on risk of acute pancreatitis related to serum triglycerides, cholesterol and fasting glucose. Pancreatology. 2012;12(4):317–324. doi:10.1016/j.pan.2012.05.002
17. Jin DX, Lacson R, Cochon LR, et al. A clinical model for the early diagnosis of acute pancreatitis in the emergency department. Pancreas. 2018;47(7):871–879. doi:10.1097/MPA.0000000000001102
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

