Back to Journals » Therapeutics and Clinical Risk Management » Volume 10
Clinical management and therapeutic outcome of infertile couples in southeast Nigeria
Authors Menuba I, Ugwu E , Obi S, Lawani L, Onwuka C
Received 2 June 2014
Accepted for publication 29 July 2014
Published 1 October 2014 Volume 2014:10 Pages 763—768
DOI https://doi.org/10.2147/TCRM.S68726
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Garry Walsh
Ifeanyi E Menuba,1 Emmanuel O Ugwu,1 Samuel N Obi,1 Lucky O Lawani,2 Chidinma I Onwuka1
1Department of Obstetrics and Gynaecology, University of Nigeria Teaching Hospital, Ituku Ozalla Enugu, Enugu State, Nigeria; 2School of Postgraduate Studies, Department of Community Medicine, University of Nigeria, Enugu Campus, Enugu, Enugu State, Nigeria
Background: Infertility is highly prevalent in Nigeria and most infertile couples in southeast Nigeria are offered conventional forms of treatment, which consist mainly of ovulation induction and tubal surgery, due to limited availability and high cost of endoscopic and assisted reproductive technologies like laparoscopy and in vitro fertilization. The aim of this study was to determine the prevalence of infertility, outcome of infertility investigation, and the treatment outcome of infertile couples following therapeutic interventions in southeast Nigeria over a 12-month period.
Methods: This was a prospective cross-sectional study of 218 consecutive infertile couples presenting for infertility management at the infertility clinics of two tertiary health institutions in Enugu, southeast Nigeria. Infertility investigations were carried out on these couples using the available conventional diagnostic facilities. Following the results of the investigations/diagnosis, conventional treatment was offered to the couples as appropriate. Data analysis was both descriptive and inferential at 95% confidence level.
Results: The mean age of the women was 33.5±4.62 (range: 15–49) years. Most (58.3% [n=127]) were nulliparous. The prevalence of infertility was 12.1%. Infertility was primary in 28.4% (n=62) and secondary in 71.6% (n=156). Female etiologic factors were responsible in 32.1% (n=70), male factors in 26.1% (n=57), and a combination of male/female factors in 29.4% (n=64). The etiology was unknown in 12.4% (n=27). Tubal factors 23.8 % (n=52) and ovulation failures 26.1% (n=57) are common female factors implicated. Pregnancy rate following treatment was 16.7% (n=28). Multivariate regression analysis indicates that younger age of ≤30 years, duration of infertility ≤5 years, and female factor infertility were associated with higher pregnancy outcome following treatment.
Conclusion: The prevalence of infertility is high and pregnancy rate following conventional treatment is poor. There is a need to improve facilities for managing infertility as well as making artificial reproductive techniques readily available, accessible, and affordable.
Keywords: infertility, assisted conception, treatment, IVF, pregnancy, reproduction
Background
Successful reproduction is one of the greatest desires of couples in developing countries. Available evidence indicates that infertility is a major problem associated with reproductive health in sub-Saharan Africa.1 The exact prevalence of infertility in developing countries is unknown, due to poor documentation and lack of well-designed studies.2 However, a study in sub-Saharan Africa showed that infertility is highly prevalent, affecting about 10%–30% of couples.3 Several reports indicate that infertility is the most frequent reason for gynecological consultation in Nigeria.4,5 Worldwide, an estimated 580 million couples (approximately 5%–8% of couples) experience infertility at some point in their reproductive lives.6 The consequences of infertility in sub-Saharan Africa are enormous and include marital problems, divorce, depression, stigmatization, isolation, economic hardship, and physical violence, among others.7–9 Despite this large burden, very few infertility-management programs exist.5 Only very few resources presently exist for the treatment of infertile couples. The conventional methods of infertility treatment are poorly developed in many African countries and little is known about pregnancy outcome after those treatments or about pregnancies which occur spontaneously. In Ghana, a cumulative spontaneous pregnancy rate of 12% was reported among 1,000 infertile patients followed-up for 18 months.10 Infertility treatment by assisted reproductive technology (ART) is expensive and the availability of such services is limited even in developed countries.11–14 In southeast Nigeria, no public health facility currently offers ART services for infertility. Thus, all infertile couples seeking treatment have limited treatment options, many of which are outdated with poor therapeutic outcome and high rate of loss to follow-up. The paucity of reliable data on the clinical management and therapeutic outcome of infertility in southeast Nigeria necessitate this study to address this problem.
Materials and methods
This was a prospective cross-sectional study of 218 consecutive infertile couples who presented to the infertility clinics of the University of Nigeria Teaching Hospital and Enugu State University Teaching Hospital, Enugu State, southeast Nigeria between June 1, 2012 and May 31, 2013. The two facilities provide specialized gynecological services to women in the state and also receive referrals from the other neighboring southeast Nigerian states. Ethical clearance was obtained from the Research and Ethical committee of the hospitals. Written signed consent was obtained from the participants. All the female participants received a clinical gynecological examination and all the men received genital examinations by the investigator in conjunction with the urologist. The female participants were investigated accordingly with the available facilities in the University of Nigeria Teaching Hospital and Enugu State University Teaching Hospital. The specific investigations included transabdominal or transvaginal ultrasonography as applicable, hormonal assay, and hysterosalpingography (HSG). All the male partners were referred for semen analysis after 3–5 days of abstinence and results were interpreted according to the new World Health Organization reference value.15 Following investigations, treatment was offered based on the results of investigation/diagnosis. Thereafter, each participant (woman) was followed-up for 6 months for therapeutic outcome (pregnancy). Data were collected using a prepared structured case record form (data entry pro forma). The data entry pro forma contained the sociodemographic characteristics of the patients, duration of infertility, type of infertility, investigation done/results, duration since completion of investigations, treatment offered, and outcome in terms of pregnancy. Data collected from the study were keyed into the Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, USA) computer software version 17.0 for windows. Statistical analysis was both descriptive and inferential (odds ratio [OR]) at 95% confidence level (CI). Continuous variables were analyzed using the mean and standard deviation. Discrete variables were analyzed using proportions, Pearson’s chi-squared, and multivariate logistic regression as applicable. P-value of <0.05 was considered to be statistically significant.
Results
A total of 1,983 new patients attended the gynecology clinics of the study facilities during the study period, out of which 240 were diagnosed with infertility, giving a prevalence rate of 12.1%. Of the total of 240 infertile couples enrolled in the study, only 218 completed their investigations, giving a completion rate of 90.8%. The mean age of the women was 33.5±4.62 (range: 15–49) years and a majority of the women (63.3% [n=138]) were in the 30–39 years age group. Also in the majority were those who were nulliparous (58.3% [n=127]) and those who had tertiary level of education (41.3% [90/218]). Details of the sociodemographic characteristics of the women are as shown in Table 1.
  | Table 1 Sociodemographic characteristics of the female and male participants |
One hundred and fifty-six (71.6%) couples had secondary infertility and 62 (28.4%) had primary infertility. The duration of infertility was less than 5 years in 137 (62.8%) couples, and was 5 years or more in 81 (32.7%) couples.
Table 2 shows the results of investigations in the women and their male partners. HSG was performed in 211 women. The commonest finding on HSG was tubal blockage (24.6% [52/211]); specifically, 2.8% (6/211) had bilateral tubal blockage, 15.6% (34/211) had unilateral blockage, 1.8% (4/211) had unilateral hydrosalpinx, and 3.8% (8/211) had bilateral hydrosalpinx. Uterine synechia was diagnosed in 7.8% (17/211) of the participants.
  | Table 2 Outcome of infertility investigations and diagnosis |
Pelvic ultrasound (abdominal or transvaginal) was performed on all 218 women. The result was normal in 167 women (76.6%). The commonest abnormalities found on ultrasound were uterine fibroid (15.6%) and polycystic ovaries (10.1%). Hormonal assay findings showed that 26.1% of women had anovulatory infertility. Specifically, hyperprolactinemia was seen in 13.8% of patients and premature ovarian failure in 2.3%. Seminal fluid analysis (SFA) was performed on all 218 men. The result showed normal parameters in 51.8%. Twenty-one (9.6%) had oligozoospermia, three (1.4%) had azoospermia, 18 (8.3%) had asthenozoospermia, seven (3.2%) had teratozoospermia, nine (4.1%) had oligoasthenozoospermia, five (2.3%) had oligoteratozoospermia, four (1.8%) had asthenoteratozoospermia, and 31 (14.2%) showed evidence of infection (Table 2). Overall, infertility was found to be due to female factors in 32.1% of couples, male factors in 26.1% of couples, and a combination of male and female factors in 29.4% of couples. The cause of infertility could not be determined in 12.4% of couples.
Table 3 shows the treatment options offered to the couples; these included ovulation induction with clomiphene citrate, bromocriptine, antibiotics, and surgeries including adhesiolysis, myomectomy, and salpingostomy. Fourteen women with severe tubal-factor infertility (bilateral tubal blockage or hydrosalpinx), five women with premature ovarian failure, and 28 women whose husbands had severe abnormal SFA result were counseled on adoption or ART. None of these women referred for ART underwent the procedure because of the prohibitive cost. Also, none of these women undertook the option of adoption. Fifteen men were referred to the urologist for further evaluation of their abnormal SFA result shown in Table 2, while Table 4 shows the treatment received.
  | Table 3 Treatment options offered to the women after infertility investigation/diagnosis |
  | Table 4 Treatment options offered to male partners (n=168) of women managed for infertility |
Of the 218 women and 168 (77.1%) male partners who were followed-up to 6 months (50 [22.9%] male partners defaulted), 28 (16.6%) women reported pregnancy symptoms and these were confirmed with a positive pregnancy test and ultrasound scan. Younger women aged ≤30 years were significantly more likely to achieve pregnancy following conventional infertility treatment than older women aged >30 years (23.2% [13/56] versus 9.3% [15/162]; OR =2.96; 95% CI =1.31–6.71; P=0.01). Similarly, couples whose duration of infertility was ≤5 years were significantly more likely to achieve pregnancy following conventional infertility treatment than couples whose duration of infertility was >5 years (16.8% [23/137] versus 6.2% [5/81]; OR =3.07; 95% CI =1.12–8.42; P=0.03). Furthermore, couples with female-factor infertility were significantly more likely to achieve pregnancy following conventional infertility treatment than couples with male-factor or combined male- and female-factors infertility (22.9% [16/70] versus 9.9% [12/121]; OR =2.69; 95% CI =1.19–6.09; P=0.02). Couples with primary infertility were more likely to achieve pregnancy following conventional infertility treatment than couples with secondary infertility; however, the observed difference was not statistically significant (14.5% [9/62] versus 12.2% [19/156]; OR =1.22; 95% CI =0.52–2.88; P=0.64). Further details are shown in Table 5.
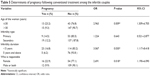  | Table 5 Determinants of pregnancy following conventional treatment among the infertile couples |
Discussion
The prevalence of infertility (12.1%) in the study population is high but comparable to reports from some related studies from southeast Nigeria.16,17 The figure is however higher than the 5.5% prevalence obtained in a previous retrospective study from the same study area.18 The higher incidence may be explained by the improved health-seeking behavior of the populace in addition to increasing awareness that infertility is a gynecological condition that is treatable and not “a punishment by the ancestral gods” as previously held. Further studies however may be necessary to confirm these assumptions. The peak age incidence of infertility in this study was in women aged 30–39 years (63.3%) and men also aged 30–39 years (69.7%). Higher rates of infertility in older women is attributable primarily to decline in fertility rate with advancing age.4 This finding is similar to the incidence reported in a previous study from the present study area18 and among infertile couples in a southwest Nigerian community,12 but is at variance with the report from Calabar, Nigeria.19 The majority of the women in this present study were civil servants (career women) who might have postponed marriage and child birth in pursuit of their career.
The predominance of secondary infertility (71.6%) in this study is similar to findings obtained in previous studies in our environment;18–20 this is however contrary to reports from developed countries where primary infertility is more prevalent, accounting for 61%–71% of cases, and secondary infertility is responsible for 29%–33% of cases.21 This high rate of secondary female infertility obtained in this study suggests that the outcome of the last pregnancy may play an important role in the etiology of infertility. The sequela of tubal damage caused by pelvic infection resulting from ascending infection during childbirth has been amply documented by other workers.22–24 Infections and their sequela no doubt played an important role in the etiology of infertility in both males and females. In this study, they accounted for about 14.2% of all causes of infertility in men. Oligospermia, teratozoospermia, azoospermia, asthenozoospermia, and a combination of oligoasthenozoospermia, oligoteratozoospermia, and asthenoteratozoospermia were the various semen parameter abnormalities observed in the study. The rate of asthenozoospermia (17.4%) as observed in the male partners in this study is similar to reports from previous studies.25,26
This study showed a greater contribution of female factor (32.1%) in the etiology of infertility as opposed to male factor (26.1%) and this is similar to the findings from previous studies from Nigeria.20–21 Tubal factor was identified in the majority of cases with identifiable causes and this is no doubt a common cause of infertility seen in many gynecology clinics in Nigeria.12–13 Early presentation of infertile couples for assessment and treatment was common in this study as 62.8% of patients presented within 5 years of infertility. This could be attributed to the fact that most of the women were well educated; evidenced by 41.2% having tertiary education. It could also be explained by the high premium placed on childbirth among the Igbo in Nigeria.18 The low pregnancy rate of 16.7% obtained in the present study is similar to the 17.0% obtained in a previous retrospective design from the same study area. This figure is however lower than the 22.4% reported by Giwa-Osagie et al from Lagos14 and the 24.0% reported by Ekwere et al from Calabar.19 Nevertheless, the short follow-up period of 6 months in this study may contribute to the lower pregnancy rate compared to the other two older studies as pregnancy may not occur for over 6 months after commencement of some infertility treatments.27 The low pregnancy rate recorded in this study reaffirms the notion that conventional treatment for infertility is not enough and that only few infertile couples can be treated effectively without ART as the majority will need in vitro fertilization and embryo transfer/intracytoplasmic sperm injection.13 The current cost of ART prohibits its wide-spread use in resource-poor countries where the burden of infertility is high. This is evidenced in this study by the fact that none of the couples referred for ART had been able to undertake the procedure because of the exorbitant cost. This study therefore reemphasizes the need for the implementation of ART in low-income countries including Nigeria.
Strength and limitation of the study
The lack of a functional laparoscope and hysteroscope in the study centers at the time of this study might have limited the scope of diagnosis made among infertile couples. The limited duration of follow-up of the women after commencement of treatment may have affected the pregnancy rate obtained in this report since some other women may achieve pregnancy following longer follow-up. The strength of this study however is in its prospective design with relatively reduced default rates/losses to follow-up which were major limitations of most previous designs on infertility management and outcome in our environment.
Conclusion
The prevalence of infertility is high and secondary infertility is more common. There is a high rate of unexplained infertility. Tubal factors and ovulation failures are commonly implicated in cases with identifiable female factors. The pregnancy rate following conventional treatment was poor. Younger age, shorter duration of infertility, and female-factor infertility were associated with better therapeutic outcome (pregnancy) following conventional infertility treatment. There is need to improve facilities for managing infertility as well as provide updated facilities for fertility-related endoscopic procedures and artificial reproductive techniques at affordable cost.
Acknowledgments
The authors extend their gratitude to all participants in this study. They are also indebted to the staff of the gynecology departments for their excellent cooperation and support in data collection during the study period.
Author contributions
The work presented here was carried out in collaboration between all authors (IEM, EOU, SNO, LOL, CIO). All authors defined the research theme, co-designed the methods, conducted the data analysis, and worked together on associated data collection and its interpretation. All the authors were involved in drafting the article and revising it critically for important intellectual content, and approved the final manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Okonfua FE, Obi H. Specialized versus conventional treatment of infertility in Africa; time for a pragmatic approach. Afr J Reprod Health. 2009;13(1):9–15. | ||
Ombelet W, Cooke I, Dyer S, Serour G, Devroey P. Infertility and the provision of infertility medical services in developing countries. Hum Reprod Update. 2008;14(6):605–621. | ||
Larsen U. Primary and secondary infertility in sub-saharan Africa. Int J Epidemiol. 2000;29:285–291. | ||
Okohue JE, Onuh SO, Ikimalo JI. Comparison of IVF/ICSI outcome in patients with polycystic ovarian syndrome or tubal factor infertility. Niger J Clin Pract. 2013;16(2):207–210. | ||
Omoaregba JO, James BO, Lawani AO, Morakinya O, Olotu OS. Psychosocial characteristics of female infertility in a tertiary health institution in Nigeria. Ann Afr Med. 2011;10(1):19–24. | ||
Okonufua FE. Infertility in sub-saharan Africa. In: Okonufua FE, Odunsi OA, editors. Contemporary Obstettrics and Gynaecology for Developing Countries. Benin City: Women’s Health Action Research center; 2003:128–156. | ||
van Balen F, Bos HM. The social and cultural consequences of being childless in poor-resource countries. F, V and V in ObGyn. 2009;1:106–121. | ||
Daar AS, Merali Z. Infertility and social suffering: the case of ART in developing countries. In: Vayena E, Rowe PJ, Griffin PD, editors. Current Practices and controversies in Assisted Reproduction: Report of a meeting on “Medical, Ethical and Social Aspects of Assisted Reproduction” held at WHO headquarters in Geneva, Switzerland 17–21 September 2001. Geneva: World Health Organization; 2002:15–21. | ||
Dyer SJ, Abrahams N, Mokoena NE, Lamard CJ, van der Spuy ZM. Psychological distress among women suffering from couple infertility in South Africa: a quantitative assessment. Hum Reprod. 2005;20:1938–1943. | ||
Fiander A. Causes of infertility among 1000 patients in Ghana. Trop Doct. 1990;20:137–138. | ||
Sharma S, Mittal S, Aggarwal P. Management of infertility in low resources countries. BJOG. 2009;116 Suppl 1:77–83. | ||
Sule JO, Erigbali P, Eruom L. Prevalence of Infertility in women in a Southwestern Nigerian Community. African Journal of Biomedical Research. 2008;11:225–227. | ||
Ombelet W, Campo R. Affordable IVF for developing countries. Reprod Biomed Online. 2007;15:257–265. | ||
Giwa-Osagie OF, Ogunyomi D, Emuveyan EE, Akinla OA. Etiologic classification and sociomedical characteristics of infertility in 250 couples. Int J Fertil. 1984;29:104–108. | ||
Cooper TG, Noonan E, von Eckardstein S, et al. World Health Organization reference values for human semen characteristics. Hum Repod Update. 2010;16:231–245. | ||
Ugwu EO, Onwuka CI, Okezie OA. Pattern and outcome of infertility in Enugu: the need to improve diagnostic facilities and approaches to management. Niger J Med. 2012;21(2):180–184. | ||
Obuna JA, Ndukwe HA, Ugboma A, Ejikeme BN, Ugboma EW. Clinical presentation of infertility in an outpatient clinic of a resource poor setting South-East Nigeria. Int J Trop Dis Health. 2012;2(2):123–131. | ||
Umeora OU, Ejikeme BN, Sunday-Adeoyo I, Umeora MC. Sociocultural impediments to male factor infertility evaluation in rural South-east Nigeria. J Obstet Gynaecol. 2008;28:323–326. | ||
Ekwere PD, Archibong EI, Bassey EE, Ekabua JE, Ekanem EI, Feyi-waboso P. Infertility among Nigerian couples as seen in Calabar. Port Harcourt Medical Journal. 2007;2:35–40. | ||
Adu BM, Massa AA, Bukar M. Clinical Presentation of Infertility in Gombe, North-Eastern Nigeria. Trop J Obstet Gynaecol. 2003;20:93–96. | ||
Templeton A, Fraser C, Thompson B. Infertility-epidemiology and referral practice. Hum Reprod. 1991;6(10):1391–1394. | ||
Pellati D, Mylonakis I, Bertoloni G, et al. Genital tract infections and infertility. Eur J Obstet Gynecol Reprod Biol. 2008;140(1):3–11. | ||
Claire B, David G, Hossein S. Sexually Transmitted Infections and sexual function in relation to male infertility. Korean J Urol. 2013;54(3):149–156. | ||
Blanchardd AC, Pastorek JG 2nd, Week T. Pelvic inflammatory disease during pregnancy. South Med J. 1987;80:1363–1365. | ||
Nwajiaku LA, Mbachu II, Ikeako L. Prevalence, clinical pattern and major causes of male infertility in Nnewi, South East Nigeria: A five year review. Afrimedic Journal. 2012;3(2):16–19. | ||
Kamath MS, Bhattacharya S. Demographics of infertility and management of unexplained infertility. Best Pract Res Clin Obstet Gynaecol. 2012;26(6):729–738. | ||
Cecil A, Klufio. Hyperprolactinaemia and prolactinoma. In: Emuveyan EE, Kwawukume EU, editors. Comprehensive Gynaecology in the Tropics. 1st ed. Graphic Packaging Ltd, Accra; 2005:300–317. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
