Back to Journals » Clinical Ophthalmology » Volume 14
Clinical Features of Vitreomacular Traction Syndrome with Peripheral Vitreoretinal Adhesion
Authors Fukumoto M, Sato T, Oosuka S, Kida T, Oku H, Ikeda T
Received 22 October 2019
Accepted for publication 14 January 2020
Published 28 January 2020 Volume 2020:14 Pages 281—286
DOI https://doi.org/10.2147/OPTH.S235670
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Masanori Fukumoto, Takaki Sato, Shou Oosuka, Teruyo Kida, Hidehiro Oku, Tsunehiko Ikeda
Department of Ophthalmology, Osaka Medical College, Takatsuki-City, Osaka, Japan
Correspondence: Tsunehiko Ikeda
Department of Ophthalmology, Osaka Medical College, 2-7 Daigaku-Machi, Takatsuki-City, Osaka 569-8686, Japan
Tel +81-72-684-6434
Fax +81-72-682-0995
Email [email protected]
Purpose: To retrospectively review and analyze the clinical and imaging data of patients with vitreomacular traction syndrome (VMTS) with strong peripheral vitreoretinal adhesion.
Subjects and Methods: This retrospective case-series study involved 4 eyes of 4 VMTS patients with vitreoretinal adhesion in both the macular region and the periphery who underwent vitreous surgery. In all 4 cases, preoperative refraction, fundoscopic findings, optical coherence tomography (OCT) findings, and intraoperative findings were evaluated.
Results: The preoperative fundoscopy and OCT findings revealed fibrous membranes around the optic nerve head in 3 eyes. Thickened posterior vitreous membranes extending from the posterior pole to the periphery were observed in all eyes. Apparent VMTS or epimacular membrane was also found in the fellow eyes of 2 patients. The preoperative refractive errors ranged from +0.5 diopters (D) to +2.75 D (mean, +1.13 D). Intraoperatively, a thickened posterior vitreous membrane was found strongly adhered to the retina in the macula regions, optic nerve head, and periphery. In 2 eyes, when artificial posterior vitreous detachment (PVD) was created, an iatrogenic tear developed in the periphery.
Conclusion: The features of VMTS that cause strong peripheral vitreoretinal adhesion include the preoperative presence of a thickened posterior vitreous membrane over a wide area, hypermetropia, and a short axial length.
Keywords: hypermetropic, iatrogenic tear, peripheral vitreoretinal adhesion, posterior vitreous detachment, vitreomacular traction syndrome, vitreous surgery
Introduction
Vitreomacular traction syndrome (VMTS) is a disorder that causes foveal depression via anterior traction of the foveal retina when posterior vitreous detachment (PVD) occurs.1–4 Optical coherence tomography (OCT) is very useful for not only diagnosing VMTS but also for determining the extent of vitreoretinal adhesion and detecting retinoschisis, retinal detachment, and cyst-like changes in the retina. In general, vitreoretinal adhesion is localized to the macular region and rarely observed in the peripheral area.
Here, we report 4 cases of VMTS with extremely strong vitreoretinal adhesion not only in the macular area but also around the optic nerve head (ONH) and in the periphery, and the clinical features of those 4 cases.
Subjects and Methods
This retrospective case study involved 4 eyes of 4 VMTS patients (3 females, 1 male; mean age: 75 years; range: 60–86 years) who presented with strong vitreoretinal adhesion in both the macular region and the peripheral area and who subsequently underwent vitreous surgery at the Department of Ophthalmology, Osaka Medical College, Takatsuki City, Osaka, Japan in 2017. In all 4 cases, the preoperative refraction, fundoscopy findings, optical coherence tomography (OCT) (SPECTRALIS®; Heidelberg Engineering GmbH, Heidelberg, Germany) findings, intraoperative findings, and postoperative treatment courses were evaluated. For OCT examinations the standard scanning protocol involved two scans, i.e., the standard macula-focused OCT, and OCT of the ONH. This protocol was attempted for both eyes of each patient.
For surgical treatment, phacoemulsification and aspiration were first performed using a 3.0 mm wide, unsutured, sclero-corneal tunnel incision at 1.0 mm post-limbus
From the 11 o’clock position. Next, intraocular lens (VA-70AD; HOYA, Corporation, Tokyo, Japan) implantation was performed using a viscoelastic substances (Opelead® HV0.85; Shiseido Co., Ltd., Tokyo, Japan) in all eyes. Vitreous surgery was then performed by resection of the cortex of the core vitreous body using 25-gauge system (CONSTELLATION® Vision System; Alcon Laboratories, Inc., Fort Worth, TX, USA). During vitreous surgery, we carefully observed the intravitreal anatomy and detected the vitreoretinal adhesions from posterior pole to peripheral area.
This case study was approved by the Ethics Committee of Osaka Medical College.
Results
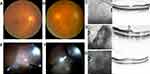
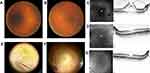
Prior to surgery, the spherical equivalent refractive errors ranged from +0.5 diopters (D) to +2.75 D (mean, +1.13D). All patients were hypermetropic, and the axial length tended to be slightly short, ranging from 22.12 to 23.51 mm (mean, 22.6 mm). The preoperative corrected visual acuity ranged from 20/200 to 20/40. In all eyes, intraocular pressure was within the normal range. The clinical findings of the 4 cases in this study are shown in Table 1. Fundoscopy examination revealed slightly glossy and thickened posterior vitreous membrane (PVM) in the macular region, yet in 3 of the 4 treated eyes, a white thickened PVM was observed in a circular fashion around the ONH. In 1 of those 4 eyes, white punctate foci were also observed on the nasal side of the ONH and appeared to represent partially fibrotic PVM. In all eyes, a thickened PVM extended from the macular region to the peripheral area. Near the equator, no findings, such as foci of retinal lattice degeneration or traction retinal detachment, were observed. Fundoscopy examination revealed almost no deviation in the retinal arcade vessels, and mild formation of a retinal fold in the macular region. OCT examination revealed findings indicative of VMTS, as well as retinoschisis-like and cyst-like findings, in all eyes. Moreover, focal traction retinal detachment was found to have occurred in the macular area of 1 eye.
 |
Table 1 The Clinical Features of the 4 Cases with VMTS |
For surgical treatment, phacoemulsification and intraocular lens implantation were first performed in all eyes, followed by resection of the cortex of the core vitreous body. In 4 eyes, the posterior vitreous body was found to have not been detached, and the thickened PVM was found to have adhered to the entire retina. With vitreous forceps, the PVM was detached from the macular region and the ONH toward the periphery to create an artificial PVD. The sites in the macular region with strong adhesion were dissected, as needed, with vitreous scissors. Next, the artificial PVD was created toward the periphery. In 1 eye with punctate white proliferative membranes at the nasal side, the sites of strong adhesion were dissected, as needed, with vitreous scissors. After being detached from the retina, the PVM was clearly visually identified as white thickened membrane-like tissue. All 4 eyes showed strong vitreoretinal adhesion in the equatorial region. Its extent was in one temporal quadrant in 1 eye, one nasal quadrant in 1 eye, two temporal-to-inferior quadrants in 1 eye, and two nasal-to-inferior quadrants in 1 eye. For the 2 eyes with two quadrants of adhesion, an iatrogenic tear was formed in the equatorial region, and peripheral vitreous shaving was also performed to reduce residual vitreous traction. Moreover, intraocular laser photocoagulation was applied around the iatrogenic tear in those 2 eyes, followed by intraocular simultaneous fluid-air exchange. Subsequently, 0.8-mL of 100% sulfur hexafluoride (SF6) gas was injected into the vitreous cavity.
After surgery, the patients were instructed to remain in the lateral position. Moreover, the postoperative courses were found to be favorable in all cases. In all eyes, the fundoscopy and OCT findings, as well as the corrected visual acuity, were improved (Figures 1–4).
Discussion
In cases of VMTS, the vitreoretinal adhesion predominantly occurs in the macular region. However, VMTS cases with peripheral adhesion are relatively rare. VMTS with a thick veil-like vitreous membrane exhibits strong adhesion in not only the macular region but also the peripheral area in some cases, as was observed in our 4 cases. In those 4 eyes, the vitreoretinal adhesion was widely extended, like a sheet, from the macular region to the periphery, and strong adhesion was also observed around the ONH.
Although the causes of the thickened vitreous membrane remain unknown, some type of vitreoretinal dystrophy might be involved. Reportedly, vitreous dystrophy with such a thickened PVM includes familial exudative vitreoretinopathy, Stickler syndrome, and Wagner disease.5–7 In 2 of the 4 eyes in this present study, the conditions were found to be unilateral, and the other 2 eyes did not show either a dragged disc or peripheral retinal abnormalities that were suggestive of such vitreous dystrophy. Moreover, in those 4 cases, there was no presence of any syndromic features and familial histories that would point towards one of the dystrophies. Although we did not perform genetic investigations for any of the dystrophies, there is little possibility of those 4 cases being any type of inherited dystrophy.
In regard to VMTS with peripheral vitreoretinal adhesion, although there have been sporadic reports of the presence of peripheral vitreoretinal adhesion, few reports have indicated an association between VMTS and a thickened PVM, as was observed in our 4 cases. Gribomont et al examined the peripheral vitreoretinal adhesion in 63 eyes with epimacular membrane (EMM) and 25 eyes with VMTS, and reported that the incidence of an intraoperative iatrogenic tear and postoperative retinal detachment was 1.5% in the EMM group, yet 8% in the VMTS group, thus significantly higher in VMTS.8 Day et al, who reportedly injected SF6 into the vitreous cavity and performed artificial PVD using SF6 gas in 9 eyes with VMTS, found that a tear was formed in the periphery of 1 eye.9 Madi et al reported 8 cases of retinal detachment that resulted from a peripheral tear that formed after artificial PVD using ocriplasmin injection for VMTS, thus indicating that the peripheral retinal conditions need to be examined prior to surgery.10 Silva et al also reported similar cases.11 Georgalas et al reported a case of VMTS with peripheral traction retinal detachment.12 As described in those reports, VMTS appears to be more frequently associated with peripheral vitreoretinal adhesion than ordinary EMM.
On the other hand, it should be noted that there have also been reported cases of VMTS with vitreoretinal adhesion around the ONH, as was observed in our 4 cases. Hixson et al described a 62-year-old woman with VMTS in whom strong adhesion of a thickened PVM was observed not only in the macular region but also around the ONH.13 In a report by Brasseur et al, the authors indicated that because the severity and the sites of vitreoretinal adhesion greatly vary among individual patients with VMTS, attention should also be paid to adhesion in areas other than the macular region when vitreous surgery is performed.14
In cases of VMTS with such a thickened PVM, vitreous surgery should be carefully performed, while considering the possible presence of vitreoretinal adhesion around the ONH and in the periphery. For this purpose, it appears important to perform a detailed ophthalmologic examination prior to surgery, including the periphery, with fundoscopy. In a previous study by Koizumi et al, the authors performed 3-dimensional (3-D) OCT to assess vitreoretinal adhesion in 48 eyes with EMM or VMTS. They found that PVD was present in 30 of 36 eyes with EMM, yet in the other 6 eyes, PVD was absent and vitreoretinal adhesion was present in the periphery.15 Thus, 3-D OCT may hold potential as a useful future tool for preoperative assessment of the eye.
Conclusion
The findings in this study showed that the features of VMTS that cause strong peripheral vitreoretinal adhesion include the preoperative presence of a thickened PVM over a wide area, hypermetropia, and a short-axial length.
Ethics Statement
This case study was approved by the Ethics Committee of Osaka Medical College.
Informed Consent
Written informed consent for publication was obtained from the patient.
Acknowledgments
The authors wish to thank John Bush for editing the manuscript.
Disclosure
The authors have no funding/conflicts of interest to disclose.
References
1. Sonmez K, Capone A
2. Jackson TL, Nicod E, Angelis A, et al. Pars plana vitrectomy for vitreomacular traction syndrome: a systematic review and metaanalysis of safety and efficacy. Retina. 2013;33(10):2012–2017. doi:10.1097/IAE.0b013e3182a6b3e2
3. Lee EK, Lee SY, Lee JY, Heo JW, Yu HG, Chung H. Anatomical configurations of vitreomacular traction syndrome: influence on clinical course and surgical outcomes. Graefes Arch Clin Exp Ophthalmol. 2019;257(8):1631–1639. doi:10.1007/s00417-019-04352-9.
4. Falcone PM. Vitreomacular traction syndrome confused with pseudophakic cystoid macular edema. Ophthalmic Surg Lasers. 1996;27(5):392–394.
5. Ikeda T, Fujikado T, Tano Y, et al. Vitrectomy for rhegmatogenous or tractional retinal detachment with familial exudative vitreoretinopathy. Ophthalmology. 1999;106(6):1081–1085. doi:10.1016/S0161-6420(99)90268-3
6. Yokoi T, Koide R, Matsuoka K, Nakagawa A, Azuma N. Analysis of the vitreous membrane in a case of type 1 Stickler syndrome. Graefes Arch Clin Exp Ophthalmol. 2009;247(5):715–718. doi:10.1007/s00417-008-1016-z.
7. Rothschild PR, Burin-des-Roziers C, Audo I, Nedelec B, Valleix S, Brézin AP. Spectral-domain optical coherence tomography in Wagner syndrome: characterization of vitreoretinal interface and foveal changes. Am J Ophthalmol. 2015;160(5):1065–1072. doi:10.1016/j.ajo.2015.08.012.
8. Gribomont AC. Surgical prognosis in idiopathic vitreomacular syndrome and epimacular membrane. J Fr Ophtalmol. 2005;28(7):739–742. doi:10.1016/S0181-5512(05)80986-6
9. Day S, Martinez JA, Nixon PA, et al. Intravitreal sulfur hexafluoride injection for the treatment of vitreomacular traction syndrome. Retina. 2016;36(4):733–737. doi:10.1097/IAE.0000000000000760.
10. Madi HA, Haynes RJ, Depla D, et al. Rhegmatogenous retinal detachment following intravitreal ocriplasmin. Graefes Arch Clin Exp Ophthalmol. 2016;254(12):2333–2338. doi:10.1007/s00417-016-3398-7
11. Silva RA, Moshfeghi DM, Leng T. Retinal breaks due to intravitreal ocriplasmin. Clin Ophthalmol. 2014;8:1591–1594. doi:10.2147/OPTH.S68037.
12. Georgalas I, Koutsandrea C, Papaconstantinou D, Karagiannis D, Ladas I. Peripheral nonrhegmatogenous retinal detachment associated with vitreomacular traction syndrome. Can J Ophthalmol. 2010;45(4):418–419. doi:10.3129/i09-257.
13. Hixson A, Reynolds S. Peripapillary vitreoretinal traction. Optometry. 2011;82(10):602–606. doi:10.1016/j.optm.2011.02.018.
14. Brasseur G. Vitreomacular traction. J Fr Ophtalmol. 2008;31(2):208–213. doi:10.1016/S0181-5512(08)70358-9
15. Koizumi H, Spaide RF, Fisher YL, Freund KB, Klancnik JM
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.