Back to Journals » International Journal of Women's Health » Volume 13
Clinical Features and Overall Survival of Females with Hepatocellular Carcinoma: A Retrospective Study and Review of the Literature in the Association of Southeast Asian Nations
Authors Ratana-Amornpin S , Vilaichone RK, Miftahussurur M, Aumpan N, Kaewkarnjanarat K, Nun-anan P, Chonprasertsuk S, Siramolpiwat S , Bhanthumkomol P, Pornthisarn B, Uchida T, Mahachai V
Received 16 March 2021
Accepted for publication 23 June 2021
Published 22 July 2021 Volume 2021:13 Pages 717—725
DOI https://doi.org/10.2147/IJWH.S311419
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Sarita Ratana-Amornpin,1 Ratha-Korn Vilaichone,1– 3 Muhammad Miftahussurur,3 Natsuda Aumpan,1 Kittipong Kaewkarnjanarat,1 Pongjarat Nun-anan,1 Soonthorn Chonprasertsuk,1 Sith Siramolpiwat,1,2 Patommatat Bhanthumkomol,1 Bubpha Pornthisarn,1 Tomohisa Uchida,4 Varocha Mahachai2,5
1Center of Excellence in Digestive Diseases and Gastroenterology Unit, Department of Medicine, Thammasat University Hospital, Pathumthani, Thailand; 2Department of Medicine, Chulabhorn International College of Medicine (CICM) at Thammasat University, Pathumthani, Thailand; 3Gastroentero-Hepatology Section, Internal Medicine Department, Universitas Airlangga, Surabaya, Indonesia; 4Department of Molecular Pathology, Oita University Faculty of Medicine, Yufu, Japan; 5Gastrointestinal and Liver Center, Bangkok Medical Center, Bangkok, Thailand
Correspondence: Ratha-Korn Vilaichone Tel +662-926-9789
Fax +662-926-9793
Email [email protected]
Introduction: Hepatocellular carcinoma (HCC) causes more than 200,000 women deaths annually. This study aimed to investigate the clinical features, provide prognostic factors for female patients with HCC, and performed a literature review on them in the Association of Southeast Asian Nations (ASEAN).
Materials and Methods: We conducted a retrospective cohort study of female patients with HCC at Thammasat University Hospital, Thailand between January 2009 and January 2019. Furthermore, important aspects of female patients with HCC in the ASEAN published in PubMed and Scopus up to October 2020 were extensively reviewed.
Results: A total of 187 female patients with HCC were included (mean age 65.7± 11.9 years). Elderly females were diagnosed with HCC at a more advanced stage than younger individuals (37.0% vs 23.2%, p=0.049, OR 1.94, 95% CI 1.00– 3.78) and the younger group had a significantly higher overall 2-year survival rate than the elderly group (65.0% vs 45.5%, p=0.03, OR 2.23, 95% CI 1.09– 4.57). Abdominal pain (HR 9.89, 95% CI 2.85– 34.38, p< 0.001), ascites at presentation (HR 2.77, 95% CI 1.11– 6.92, p=0.03), ruptured hepatoma (HR 14.68, 95% CI 12.60– 83.09, p=0.002), advanced-stage HCC (HR 9.74, 95% CI 1.89– 50.26; p=0.007), and serum hypoalbuminemia (HR 4.67, 95% CI 1.62– 13.50, p=0.004) were significantly associated with poor survival rate. From the ASEAN, a total of 543 females HCC patients from 6 studies were extensively reviewed. Chronic hepatitis B infection was among the pre-existing liver disease leading to HCC in ASEAN. HCC in females of the ASEAN occurred most often at an advanced age and had a grave prognosis.
Conclusion: HCC affects a large number of females, especially in Thailand and the ASEAN, is diagnosed at an advanced stage and had a grave prognosis. Abdominal pain, ascites, ruptured HCC, advanced-stage HCC, and serum hypoalbuminemia are associated with poor prognosis. Early detection of HCC and prompt treatment in patients at risk could result in better survival outcomes.
Keywords: clinical features, outcomes, females, hepatocellular carcinoma
Introduction
Hepatocellular carcinoma (HCC) is the sixth most common cancer and the fourth cause of cancer-related mortality worldwide with more than 800,000 new cases and almost 800,000 deaths per year. Interestingly, HCC has a particular impact on the female population with about 240,000 new cases diagnosed annually, and it is the sixth leading cause of cancer-related death in females worldwide.1 The Association of Southeast Asian Nations (ASEAN) is the subregion with the second highest incidence of HCC worldwide after East Asia.1 HCC reaches its peak incidence at the age of 70 years and is rarely seen in patients younger than 40. The prevalence of HCC is significantly higher in men than in women, and the ratio of males to females with HCC varies from 2:1 to 4:1, depending on the geographic region. A male predominance of HCC is evident in the Asia-Pacific region, an area of endemic chronic hepatitis B infection.2–4 The age-standardized incidence rate of HCC in Thailand is 22.3 per 100,000 person-years. Classified by gender, the age-standardized incidence rate is higher in men than in women (34.8 vs 11.3 per 100,000 person-years, respectively).5
Chronic hepatitis B or hepatitis C infection, alcoholic liver disease, and non-alcoholic fatty liver disease are major risk factors for the progression of cirrhosis and the development of HCC in 80–90% of HCC patients.2 Greater than 75% of all cases are related to chronic hepatitis B virus (HBV) and hepatitis C virus (HCV) infection, which have caused a 20-fold increase in the risk for development of HCC.6 In Thailand, HBV is the main etiologic risk factor for HCC, followed by alcohol consumption, chronic HCV infection and cryptogenic cirrhosis.5 However, the information about prognostic factors and survival outcomes in females with HCC is scarce due to the limited number of available studies.7–13 This study aimed to compare clinical presentation, disease etiology, treatment received, and survival rate between the elderly and younger female patients with HCC. Moreover, this study provided prognostic factors related to the survival of women with HCC.
Materials and Methods
Study Design
This was a retrospective cohort study of women diagnosed with HCC who were regularly followed up at Thammasat University Hospital, Thailand between January 2009 and January 2019. Female patients older than 18 years and diagnosed HCC were included. HCC was diagnosed by typical radiologic characteristic findings of multiphasic computed tomography (CT) scan, or dynamic contrast-enhanced magnetic resonance imaging (MRI), or confirmed by pathology. The data including demographic data, age at HCC diagnosis, underlying diseases, causes of chronic liver disease, clinical presentation, baseline laboratory values, histopathological findings, imaging findings (tumor size, portal or hepatic vessel involvement, extrahepatic metastasis, and complications), treatment, and overall survival were extensively reviewed. HCC was classified by the Barcelona Clinic Liver Cancer (BCLC) staging into early (BCLC stage 0 and A), intermediate (BCLC stage B) and advanced stages (BCLC stage C and D). Child-Turcotte-Pugh (CTP) and Model for End-Stage Liver Disease (MELD) scores were used to assess the severity of cirrhosis. p53 mutation analysis was performed from liver biopsies by immunohistochemistry staining.
Definitions
The Association of South East Asian Nations (ASEAN) is a union within the Southeast Asian region that aims for multinational-cooperation in many aspects, including public health. There are 10 member states as follows: Brunei, Cambodia, Indonesia, Laos, Malaysia, Myanmar, The Philippines, Singapore, Thailand, and Vietnam.
Elderly women are defined as those with a chronological age of 65 years old and older.
Diagnosis of HCC by imaging follows an algorithm according to the Liver Imaging Reporting and Data System (LI-RADS) system,14 which includes characteristic typical of HCC on imaging: arterial phase hyperenhancement and venous or delayed phase washout.
Hypoalbuminemia is defined as serum albumin less than 3.0 g/dL.
Treatment included surgery (liver resection), radiofrequency ablation (RFA), transarterial chemoembolization (TACE), systemic therapy, or palliative care.
Statistical Analysis
Continuous data are presented as mean and standard deviation. Nominal data were analyzed by the chi-squared test, or Fisher’s exact test, where appropriate. Univariate analysis and multivariate analysis were performed to assess the association between variables and the overall survival rate by Cox’s proportional hazards model. A p-value less than 0.05 was considered to indicate statistical significance. All statistical analyses were performed by using IBM SPSS Statistics version 26.0 (SPSS Inc., Armonk, NY, USA). The study was conducted according to the good practice guideline, as well as the Declaration of Helsinki. This study was approved by the Human Research Ethics Committee of Thammasat University, Pathumthani, Thailand. The project number for ethics approval was MTU-EC-IM-1-135/62. The committees waived informed patient consent due to the retrospective study design and allowed the authors to review their medical records for our study. Thus, it involves less than the minimal risk and no impact on the rights and well-being of the research participants. Patients’ data were kept strictly confidential.
Results
Patients
A total of 187 female patients were included, and their mean age was 65.7±11.9 years. The most common underlying diseases were essential hypertension (30.1%), diabetes mellitus (28.8%), and dyslipidemia (22.7%). Moreover, there were 3 (3.8%) and 9 (10.6%) patients with metabolic syndrome in the younger and older groups, respectively (p = 0.100). Most patients were asymptomatic (43.9%). The most common presenting symptoms were weight loss (18.5%), abdominal pain (17.2%), and fatigue (15.3%). Thirty-two (20.4%) and 31 (19.8%) patients had hepatomegaly and ascites, respectively. The leading causes of chronic liver disease in female HCC were as follows: chronic HBV infection (39.8%), nonalcoholic steatohepatitis (NASH) (27.8%), chronic HCV infection (26.7%), alcohol (5.7%), and others (1.7%). There were 65 (39.2%), 74 (44.6%), and 27 (16.3%) patients classified as Child-Pugh class A, B, and C, respectively. The mean MELD-Na score was 12.8 6.1. The baseline laboratory values, and survival rates were demonstrated in Table 1.
6.1. The baseline laboratory values, and survival rates were demonstrated in Table 1.
 |
Table 1 Demographic Data and Clinical Data of HCC Patients Classified by Age |
Difference Between the Elderly Group and the Younger Group
All 187 patients were divided into 2 groups by age. As demonstrated in Table 1, 99 (52.9%) patients were in the elderly group (≥65 years old), with a mean age of 74.9 years, whereas 88 (47.1%) patients were in the younger group (<65 years old), with a mean age of 55.3 years. The elderly group had significantly more comorbidities, which were essential hypertension (40.0% vs 19.2%, p = 0.004), diabetes mellitus (28.8% vs 18.0%, p = 0.003), and dyslipidemia (34.1% vs 10.3%, p <0.001), than the younger group. The most common cause of chronic liver disease leading to HCC was chronic HBV infection which was less commonly found in the elderly group (26.6% vs 54.9%, p < 0.001, OR 0.30, 95% CI 0.16–0.56). In contrast, nonalcoholic steatohepatitis was more commonly found as chronic liver disease in elderly patients than in younger patients with HCC (41.5% vs 12.2%, p < 0.001, OR 5.10, 95% CI 2.34–11.12). There was no significant difference in the largest size and number of HCC, portal and hepatic vessel invasion, distant metastasis, and pathology between the 2 groups (Table 2). Of 12 patients whose pathological specimens were tested for TP 53 gene mutations, and 2 (18.2%) patients were positive for the mutations.
 |
Table 2 Clinical Parameters and Management of Female HCC Patients |
BCLC Staging, Treatment Modalities and Survival Outcomes
According to BCLC staging, the elderly group presented with HCC at a more advanced stage than the younger group (37.0% vs 23.2%, p = 0.049, OR 1.94, 95% CI 1.00–3.78), but the younger group had a higher proportion in the intermediate stage (22.8% vs 36.6%, p = 0.047, OR 0.51, 95% CI 0.26–0.99). Of all patients with HCC, 7.0% had received surgical hepatic resection, while 30.0% and 35.3% underwent RFA and TACE, respectively. Advanced HCC patients who had received only supportive care had the lowest median survival time of 3.5 months as shown in Figure 1. Patients with HCC who underwent surgical hepatectomy as the primary treatment had the highest 1-year survival rate (100%) compared with RFA (87.3%, p = 0.329), TACE (75.0%, p = 0.053), and palliative care (27.0%, p <0.001). The elderly group had a lower 2-year survival rate than the younger group (45.5% vs 65.0%, p = 0.028, OR 2.23, 95% CI 1.09–4.57).
 |
Figure 1 Median survival time with each management strategy. |
Prognostic Factors Associated with the Survival Rate
Serum hypoalbuminemia was more commonly found in the advanced stage than in the intermediate or early stage (79.2% vs 56.9% vs 32.9%, p <0.001) and significantly associated with the 1-year survival rate in the early stage as shown Figure 2. Univariate and multivariate analyses were performed to determine the association between prognostic factors and overall survival. Some statistically significant variables in univariate analysis were used to perform a multivariate analysis. In multivariate Cox regression analysis, patients who had abdominal pain at presentation (hazard ratio [HR] 9.89; 95% CI 2.85–34.38; p<0.001), ascites (HR 2.77; 95% CI 1.11–6.92; p=0.029), ruptured HCC (HR 14.68; 95% CI 12.60–83.09; p=0.002), advanced BCLC staging (HR 9.74, 95% CI 1.89–50.26; p=0.007), and serum hypoalbuminemia (HR 4.67; 95% CI 1.62–13.50; p=0.004) were associated with poor prognosis.
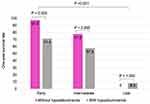 |
Figure 2 One-year survival rate related to BCLC staging and serum hypoalbuminemia. |
Female Patients with HCC in the ASEAN
There were 6 ASEAN studies reporting HCC in females. A total of 543 women female HCC patients (252 patients from Singapore; 226 patients from Thailand; 45 patients from Malaysia; and 20 patients from Vietnam) were included. Only 3 studies (2 studies from Thailand and 1 study from Vietnam) reported the data on female HCC patients, while the remaining studies reported the data on all patients, including men and women. The most common cause of chronic liver disease leading to HCC in women in the ASEAN was HBV, and the range was wide, from 39.8% to 85.7%. A large number of female patients in the ASEAN were diagnosed at a more advanced stage and had poor overall survival. The clinical characteristics and survival of female HCC patients are demonstrated in Table 3.
 |
Table 3 Clinical Characteristic and Outcomes of HCC Patients in the ASEAN |
Discussion
More men than women are typically affected by HCC. However, approximately 240,000 females are newly diagnosed with HCC annually, highlighting the importance of this cancer in the global female population.1 Liver cirrhosis is a main cause of approximately 70–90% of patients with HCC. This study disclosed that a higher proportion of HCC was present with liver cirrhosis (94.6%) in females. Chronic infections with HBV and HCV remain the major etiology of HCC development.15,16 HCC in nearly all non-cirrhotic patients was caused by chronic HBV infection. The most prevalent cause of HCC in females in this study was chronic HBV infection, whereas chronic HCV infection was the most common etiology of HCC in the USA.17 The percentage of women with HCC and NASH as the etiology of cirrhosis was slightly higher than that in a prior study conducted in the USA.18 The proportion of chronic HBV infection resulting in HCC was comparable to that in a previous study in Thailand.19 The mean age of patients with HCC caused by chronic HBV infection was 65.7 years, which was higher than that in a prior study including both genders.20 On the other hand, the prevalence of HCV infection increased with age, which was compatible with the results of earlier studies.21,22 Because of the rapidly increasing prevalence of nonalcoholic fatty liver disease (NAFLD) worldwide, it might also be a future problem and cause of HCC in the ASEAN population in the future.
HCC, which is mostly detected during surveillance with abdominal ultrasonography, is often found at an early stage with no symptoms are present. HCC surveillance by ultrasonography in patients at risk for development of HCC could be an effective tool for early detection and planning for curative treatment, leading to significant improvement of survival, especially in elderly women.23 Approximately 15% of all female HCC patients had right upper quadrant abdominal pain, which could have resulted from either hepatic capsular inflammation or tumor-related complications, such as intramural hemorrhage or necrosis.24 Therefore, abdominal pain as a presenting symptom could be associated with disease progression and poor overall survival. A minority of our patients had a family history of HCC, and the proportion was lower than that in a previous report.25 This clinical finding suggests that female patients with chronic HBV and HCV infection without a family history of HCC could perform HCC surveillance for early detection and prompt treatment. Serum hypoalbuminemia was a common condition independently associated with a poor survival rate. Serum hypoalbuminemia was found more commonly in the late stage of HCC. A low serum albumin level usually reflects impaired synthetic function of the liver and is related to poor prognosis in many cancers, including HCC, as part of an inflammatory index and aggressiveness parameters.26,27 TP53 is a tumor suppressor gene. A defect in the p53 pathway can cause proliferation of abnormal cells resulting in human cancers including HCC. Etiologies of TP 53 mutations in the molecular pathogenesis of HCC include both viruses and chemicals.28 This study demonstrated a lower proportion of p53 gene mutation positivity than the previous study.29 However, a limitation was that positive immunohistochemistry staining for p53 protein could not be considered as linked to a mutation in all HCC patients. Interestingly, our study indicated that surgical treatment in early stage of cancer could provide a longer mean survival time than RFA or TACE. This finding was correlated with the prior study of chronic HBV infection with HCC in Thailand.30 Moreover, the elderly female HCC patients receiving surgical treatment had a 100% of 1- year survival rate. Therefore, surgical resection should be considered as primary treatment in the early stage of HCC in female patients, especially in the elderly, to improve treatment outcomes and achieve a higher overall survival rate.
Conclusion
HCC notably affected a larger number of female patients in the populations. Elderly female patients had a lower 2-year survival rate and were diagnosed at a more advanced stage than the younger group. Early detection of HCC in patients at risk could result in better survival outcomes. Serum hypoalbuminemia was independently associated with overall survival and might be used as an effective prognostic predictor in female HCC patients.
Acknowledgments
This study was also supported by a grant from the Faculty of Medicine, Thammasat University, Bualuang ASEAN Chair Professorship at Thammasat University, and Center of Excellence in Digestive Diseases (CoE DD), Thammasat University, Thailand.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi:10.3322/caac.21492
2. Villanueva A, Longo DL. Hepatocellular carcinoma. N Engl J Med. 2019;380(15):1450–1462. doi:10.1056/NEJMra1713263
3. Jack Wands MD. Hepatocellular carcinoma and sex. N Engl J Med. 2007;357:1974–1976. doi:10.1056/NEJMcibr075652
4. El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132(7):2557–2576. doi:10.1053/j.gastro.2007.04.061
5. Chonprasertsuk S, Vilaichone RK. Epidemiology and treatment of hepatocellular carcinoma in Thailand. Jpn J Clin Oncol. 2017;47(4):294–297. doi:10.1093/jjco/hyw197
6. Schutte K, Bornschein J, Malfertheiner P. Hepatocellular carcinoma--epidemiological trends and risk factors. Dig Dis. 2009;27(2):80–92. doi:10.1159/000218339
7. Ladenheim MR, Kim NG, Nguyen P, et al. Sex differences in disease presentation, treatment and clinical outcomes of patients with hepatocellular carcinoma: a single-centre cohort study. BMJ Open Gastroenterol. 2016;3(1):e000107. doi:10.1136/bmjgast-2016-000107
8. Farinati F, Sergio A, Giacomin A, et al. Is female sex a significant favorable prognostic factor in hepatocellular carcinoma? Eur J Gastroenterol Hepatol. 2009;21(10):1212–1218. doi:10.1097/MEG.0b013e32831a86f8
9. Kazufumi Dohmen HS, Irie K, Shibashi H, Ishibashi H. Longer survival in female than male with hepatocellular carcinoma. J Gastroenterol Hepatol. 2003;18:267–272. doi:10.1046/j.1440-1746.2003.02936.x
10. Guo H, Wu T, Lu Q, et al. Hepatocellular carcinoma in elderly: clinical characteristics, treatments and outcomes compared with younger adults. PLoS One. 2017;12(9):e0184160. doi:10.1371/journal.pone.0184160
11. Borzio M, Dionigi E, Vitale A, et al. Management and prognosis of hepatocellular carcinoma in the elderly: results of an in-field multicenter cohort study. Liver Int. 2017;37(8):1184–1192. doi:10.1111/liv.13392
12. Tangkijvanich P, Mahachai V, Suwangool P, Poovorawan Y. Gender difference in clinicopathologic features and survival of patients with hepatocellular carcinoma. World J Gastroenterol. 2004;10(11):1547–1550. doi:10.3748/wjg.v10.i11.1547
13. Tsukioka G, Kakizaki S, Sohara N, et al. Hepatocellular carcinoma in extremely elderly patients: an analysis of clinical characteristics, prognosis and patient survival. World J Gastroenterol. 2006;12(1):48–53. doi:10.3748/wjg.v12.i1.48
14. Marrero JA, Kulik LM, Sirlin CB, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2018;68(2):723–750. doi:10.1002/hep.29913
15. Fattovich G, Stroffolini T, Zagni I, Donato F. Hepatocellular carcinoma in cirrhosis: incidence and risk factors. Gastroenterology. 2004;127(5 Suppl 1):S35–50. doi:10.1053/j.gastro.2004.09.014
16. Zhu RX, Seto WK, Lai CL, Yuen MF. Epidemiology of hepatocellular carcinoma in the Asia-Pacific region. Gut Liver. 2016;10(3):332–339. doi:10.5009/gnl15257
17. de Martel C, Maucort-Boulch D, Plummer M, Franceschi S. World-wide relative contribution of hepatitis B and C viruses in hepatocellular carcinoma. Hepatology. 2015;62(4):1190–1200. doi:10.1002/hep.27969
18. Phipps M, Livanos A, Guo A, et al. Gender matters: characteristics of hepatocellular carcinoma in women from a large, multicenter study in the United States. Am J Gastroenterol. 2020;115:1486–1495. doi:10.14309/ajg.0000000000000643
19. Somboon K, Siramolpiwat S, Vilaichone RK. Epidemiology and survival of hepatocellular carcinoma in the central region of Thailand. Asian Pac J Cancer Prev. 2014;15(8):3567–3570. doi:10.7314/apjcp.2014.15.8.3567
20. Chitapanarux T, Phornphutkul K. Risk factors for the development of hepatocellular carcinoma in Thailand. J Clin Transl Hepatol. 2015;3(3):182–188. doi:10.14218/JCTH.2015.00025
21. Garcia Comas L, Ordobas Gavin M, Sanz Moreno JC, et al. Prevalence of hepatitis C antibodies in the population aged 16–80 years in the community of Madrid 2008–2009. J Med Virol. 2015;87(10):1697–1701. doi:10.1002/jmv.24219
22. Wasitthankasem R, Posuwan N, Vichaiwattana P, et al. Decreasing hepatitis C virus infection in Thailand in the past decade: evidence from the 2014 National Survey. PLoS One. 2016;11(2):e0149362. doi:10.1371/journal.pone.0149362
23. Singal AG, Pillai A, Tiro J, Klenerman P. Early detection, curative treatment, and survival rates for hepatocellular carcinoma surveillance in patients with cirrhosis: a meta-analysis. PLoS Med. 2014;11(4):e1001624. doi:10.1371/journal.pmed.1001624
24. Bialecki ESBA, Di Bisceglie AM. Clinical presentation and natural course of hepatocellular carcinoma. Eur J Gastroenterol Hepatol. 2005;17:485–489. doi:10.1097/00042737-200505000-00003
25. Hassan MM, Spitz MR, Thomas MB, et al. The association of family history of liver cancer with hepatocellular carcinoma: a case-control study in the United States. J Hepatol. 2009;50(2):334–341. doi:10.1016/j.jhep.2008.08.016
26. Carr BI, Guerra V. Serum albumin levels in relation to tumor parameters in hepatocellular carcinoma patients. Int J Biol Markers. 2017;32(4):e391–e396. doi:10.5301/ijbm.5000300
27. Li MX, Bi XY, Li ZY, et al. Prognostic role of Glasgow Prognostic Score in patients with hepatocellular carcinoma: a systematic review and meta-analysis. Medicine (Baltimore). 2015;94(49):e2133. doi:10.1097/MD.0000000000002133
28. Hussain SP, Schwank J, Staib F, Wang XW, Harris CC. TP53 mutations and hepatocellular carcinoma: insights into the etiology and pathogenesis of liver cancer. Oncogene. 2007;26(15):2166–2176. doi:10.1038/sj.onc.1210279
29. Zhan P, Ji YN, Yu LK. TP53 mutation is associated with a poor outcome for patients with hepatocellular carcinoma: evidence from a meta-analysis. Hepatobiliary Surg Nutr. 2013;2(5):260–265. doi:10.3978/j.issn.2304-3881.2013.07.06
30. Wanich N, Vilaichone RK, Chotivitayatarakorn P, Siramolpiwat S. High prevalence of hepatocellular carcinoma in patients with chronic hepatitis B infection in Thailand. Asian Pac J Cancer Prev. 2016;17(6):2857–2860.
31. Le VQ, Nguyen VH, Nguyen VH, et al. Epidemiological characteristics of advanced hepatocellular carcinoma in the northern region of Vietnam. Cancer Control. 2019;26(1):1073274819862793. doi:10.1177/1073274819862793
32. Goh GB, Li JW, Chang PE, Chow KY, Tan CK. Deciphering the epidemiology of hepatocellular carcinoma through the passage of time: a study of 1401 patients across 3 decades. Hepatol Commun. 2017;1(6):564–571. doi:10.1002/hep4.1059
33. Norsa’adah B, Nurhazalini-Zayani CG. Epidemiology and survival of hepatocellular carcinoma in north-east Peninsular Malaysia. Asian Pac J Cancer Prev. 2013;14(11):6955–6959. doi:10.7314/apjcp.2013.14.11.6955
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
