Back to Journals » Vascular Health and Risk Management » Volume 16
Clinical Features and Factors Affecting Postoperative Mortality for Obstructive Acute Mesenteric Ischemia in China: A Hospital- Based Survey
Received 22 May 2020
Accepted for publication 9 November 2020
Published 25 November 2020 Volume 2020:16 Pages 479—487
DOI https://doi.org/10.2147/VHRM.S261167
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Konstantinos Tziomalos
Wenhan Wu, Lie Yang, Zongguang Zhou
Institute of Digestive Surgery of Sichuan University and Department of Gastrointestinal Surgery, West China Hospital, West China School of Medicine, Sichuan University, Chengdu, Sichuan, 610041, People’s Republic of China
Correspondence: Zongguang Zhou
Institute of Digestive Surgery of Sichuan University and Department of Gastrointestinal Surgery, West China Hospital, West China School of Medicine, Sichuan University, Chengdu, Sichuan, 610041, People’s Republic of China
Tel 86-18980601007
Email [email protected]
Purpose: The study aimed to report the clinical manifestation and identify the risk factors for postoperative mortality in patients who were diagnosed with obstructive acute mesenteric ischemia (AMI) based on a survey of a hospital in western China.
Patients and Methods: We reviewed clinical data of 108 patients with obstructive AMI at West China Hospital, Sichuan University, from 2011 to 2017. Clinical characteristic was described and compared. Factors affecting postoperative survival were analyzed.
Results: A total of 108 obstructive AMI cases were included in this study, with an overall average age of 57.1 years, including 58 arterial occlusive mesenteric ischemia (AOMI) and 50 mesenteric venous thrombosis (MVT). AOMI patients were older and had a significantly higher frequency of these comorbidities, including heart disease, hypertension, and diabetes. In comparison, MVT had a significantly higher proportion of male patients and a higher frequency of liver disease. A total of 77 patients underwent laparotomy, and the 30-day postoperative mortality rate was 29.9%. Multivariate logistic regression analysis showed that the time interval from admission to surgery (adjust OR 1.19; 95% CI [1.07– 1.34], P = 0.005), platelet count (adjust OR = 0.98; 95% CI [0.97– 0.99], P = 0.008) and AOMI (adjust OR = 5.55; 95% CI [1.36– 22.55], P = 0.017) were independent predictors of 30-day mortality after exploratory laparotomy for obstructive AMI. Further analysis of the 45 AOMI showed that the time interval from admission to surgery (adjustOR 1.22; 95% CI [1.01– 1.47], P = 0.036) and platelet count (adjustOR = 0.98; 95% CI [0.97– 0.99], P = 0.020) were independent risk factors for 30-day postoperative mortality of AOMI.
Conclusion: Early identification of AOMI, improving the efficiency of enhanced CT examination, strengthening doctor–patient communication, active laparotomy, and optimize platelet management may also help reduce the overall short-term mortality of obstructive AMI. Building the multidisciplinary team model of diagnostic imaging, vascular intervention, and surgical treatment to manage obstructive AMI may be urgently needed in western China.
Keywords: obstructive acute mesenteric ischemia, risk factors, laparotomy, outcome
Introduction
Acute mesenteric ischemia (AMI) can generally be defined as a type of disease, usually a sudden insufficient supply of blood in the intestine, including arterial occlusive mesenteric ischemia (AOMI, 65–75%), mesenteric venous thrombosis (MVT, 5–15%) and nonocclusive mesenteric ischemia (NOMI, 10–30%).1 The first two types of acute mesenteric ischemia can be summarized as obstructive AMI. Thrombosis and embolism are usually located in the superior mesenteric artery (SMA) or superior mesenteric vein (SMV) in obstructive AMI. Although AMI is an uncommon surgical emergency, the annual incidence rate is 0.09% to 0.2%, which often brings catastrophic troubles for patients with a mortality rate of 40% - 100%.1,2 A high index of suspicion of this disease and a positive diagnostic method are conducive to distinguish from other benign abdominal pain diseases, thus contributing to early intervention and improving the prognosis.3 Most studies on obstructive AMI have been reported abroad, which are still scarce in china, and the samples are small (usually less than 30 cases), clinical characteristics, comorbidities, and management practice are poorly depicted.4,5
Regardless of the cause, obstructive AMI is a surgical emergency that requires systemic support and surgical treatment. Because of the non-specific symptoms and possible delay in diagnosis, a large portion of patients with obstructive AMI had intestinal necrosis and secondary peritonitis on admission. For these patients, laparotomy, removal of the necrotic intestine, and restoration of blood supply to the remaining intestine are usually a definite method of surgical treatment, unfortunately, carries significant morbidities and mortalities.6 Identifying the factors affecting postoperative mortality for these patients will help provide appropriate risk stratification during preoperative preparation and further optimize the management of obstructive AMI.
This study aims at presenting the clinical characteristics of obstructive AMI based on a survey of a hospital in western China. It also investigates the prognostic factors that can be used to determine therapeutic options and facilitate optimal decision-making of obstructive AMI during daily clinical practice.
Materials and Methods
Patient Data
We conducted a retrospective, single-center study of patients confirmed obstructive AMI at West China Hospital of Sichuan University from January 2011 to December 2017. A total of 108 cases were included. The diagnosis of obstructive AMI was based on clinical symptoms, imaging characteristics, and pathological reports after surgery. The following data were collected: age, gender, current medical history, comorbidities, routine admission laboratory tests (such as blood test, coagulation test, biochemical test), medical imaging examination, and postoperative pathology report of surgical patients. Decisions to withhold and withdraw for each patient were based on their clinical evaluation and hospital course. Hospital records and phone calls with family members were used to get 30-day mortality of all patients. This study was conducted in accordance with the Declaration of Helsinki and was performed with approval from the Institutional Review Board of West China Hospital, Sichuan University, Chengdu, Sichuan, China. The present study did not affect the management of medical care and used anonymous methods to collect data, so it was exempt from the patients’ informed consent.
Statistical Analysis
Patient demographics, clinical symptoms, concomitant diseases, physical examination, blood test results, and the data regarding the type of occlusive cause were analyzed. The study group was divided into subgroups based on the cause of ischemia and survival for statistical analyses.
Data are expressed as proportions for dichotomous variables and as mean ± standard deviation or median with interquartile range (25th–75th percentiles) for continuous variables. Comparisons of independent two groups were chosen by using the Student’s t-test where numerical variables were normally distributed or using the Mann Whitney U-test when they were not normally distributed. The Chi-squared test was used to compare nominal data, and the Fisher exact test was used if necessary. More than two-group comparisons of independent numerical variables were performed by using the One Way ANOVA test when variables were normally distributed or the Kruskal Wallis test when they were not normally distributed. Risk factors affecting postoperative mortality were analyzed by univariate analysis. Factors with P < 0.05 at univariate analysis were included in a final forward logistic regression multivariate model. The odds ratio (OR) with a 95% confidence interval (CI) was calculated as an estimate of relative risk.
All the tests were two-tailed. All statistical analyses were performed using the R software for windows (version 3.5.3). P < 0.05 was considered statistically significant.
Results
Patient Information and Clinical Presentation
A total of 108 patients (71 males and 37 males; mean age 57.1) with obstructive AMI were included in this study. All patients were divided into two types according to the location of thrombus or embolism, AOMI for 53.7% (n = 58), and MVT for 46.3% (n = 50). The most common comorbidities were previous abdominal surgery (n = 39; 36.1%), followed by hypertension (n = 28; 25.9%), cardiac disease (coronary artery disease, atrial fibrillation, or heart valve disease; n = 26; 24.1%), liver disease (chronic hepatitis or cirrhosis; n = 14; 13.0%), diabetes (n = 11; 10.2%), peripheral vascular disease (n = 9, 8.3%).
AOMI patients were older (64.1 vs 49.1 years; P < 0.001) with a lower proportion of male (55.2% vs 78.0%; P = 0.013) compared to MVT patients. Moreever, AOMI patients experienced cardiac disease (37.9% vs 8.0%; P < 0.001), hypertension (34.5% vs 16.0%; P = 0.029), and diabetes (15.5% vs 4.0%; P = 0.048) more often. While MVT patients had a higher proportion of liver disease (22.0% vs 5.2%; P = 0.009). Table 1 presents a comparsion of demographic characteristics and major comorbidities observed in patients with a different type of obstructive AMI.
 |
Table 1 Demographic Characteristics and Major Comorbidities for Different Types of Obstructive AMI |
With regard to initial clinical symptoms, the following initial symptoms were common, including abdominal pain (n = 102; 94.4%), abdominal distension (n = 35; 32.4%), vomiting (n = 16; 14.8%), blood stool (n = 15; 13.9%) and diarrhea (n = 8; 7.4%). About physical findings, abdominal tenderness (n = 80; 74.1%) was the most common presenting sign, other signs included rebounding pain (n = 69; 63.9%) and muscle guarding (n = 62; 57.4%). Besides, the clinical symptoms and physical findings among different types of obstructive AMI were not statistically different. Table 2 presents a comparison of the initial clinical symptoms and physical findings observed in patients with a different type of obstructive AMI.
 |
Table 2 Initial Clinical Symptoms and Physical Findings for Different Types of Obstructive AMI |
Imaging and Laboratory Evaluation
A total of 100 patients underwent contrast-enhanced computed tomography (CT) examination, thrombosis or embolism were found in 72 (72%) patients. Abnormalities related to AMI were found in 82 cases (82%), including the thickening intestinal wall, pneumatosis intestinalis, and free peritoneal fluid. In this study, the sensitivity of the diagnosis of obstructive AMI based on contrast-enhanced CT was 82%.
Leukocytosis, with a mean value of 1.7 × 104/mm3, was the most easily observed abnormal laboratory result. Compared to MVT patients, AOMI patients tended to have higher high-density lipoprotein (HDL; 1.3±0.6 mmol/L vs 0.9±0.4 mmol/L, P = 0.001) and fibrinogen (Fb; 4.5±1.9g/L vs 3.6±1.5g/L, P = 0.011). There were no statistically significant differences in the other blood tests, biochemical tests, and coagulation tests. Table 3 presents a comparison of laboratory results observed in patients with a different type of obstructive AMI.
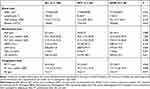 |
Table 3 Laboratory Results for Different Types of Obstructive Acute Mesenteric Ischemia |
Treatment and Outcome
Of all 108 patients, the primary therapy for 17 patients was systemic anticoagulation with intravenous heparin, and a total of 14 patients chose to withdraw from treatment after admission. Exploratory laparotomy was performed in 77 patients due to peritoneal signs or deteriorating clinical symptoms, including the triad of severe abdominal pain, gastrointestinal dysfunction, and systemic hemodynamic abnormalities. Significant necrosis of the intestine was found in 75 (97.4%) patients, with the surgically removed intestine ranging from 5 cm to 240 cm, and none of the patients had undergone intravascular manipulation or treatment. In our research, the overall 30-day mortality of obstructive AMI was 37.0% (AOMI 26, MVT 14).
Factors Affecting Postoperative Mortality of Obstructive AMI
Of the 77 obstructive AMI patients who underwent exploratory laparotomy, 23 deaths (29.9%) occurred within 30 days after surgery. Univariate analysis of the factors such as demographic characteristics, major comorbidities, clinical symptoms, physical findings, laboratory results, disease subtype was performed to investigate the potential risk factors associated with 30-day postoperative mortality. As shown in Table 4, elder age (≥60 years old; 65.2% vs.40.7%, P = 0.049), female (52.2% vs 25.9%, P = 0.026), AOMI (78.3% vs 50.5%, P = 0.021) were associated with higher mortality. Besides, non-survivors had a higher high-density lipoprotein (HDL, 1.3±0.7mmol/L vs 1.0±0.5mmol/L, P = 0.048), a lower platelet count ((144±50)*109/L vs (210±98) *109/L, P = 0.003), and a longer time interval from admission to surgery (12.5±6.3 hours vs 8.1±4.0 hours, P = 0.001).
 |
Table 4 Factors Effecting 30-Day Postoperative Mortality in the Patients with Obstructive AMI |
Potential factors associated with survival of patients with obstructive AMI were used to create a logistic regression model to determine independent risk factors for postoperative mortality. Time interval from admission to surgery (OR 1.19; 95% CI [1.07–1.34], P = 0.005), platelet count (OR = 0.98; 95% CI [0.97–0.99], P = 0.008) and AOMI (OR = 5.55; 95% CI [1.36–22.55], P = 0.017) were identified as independent predictors of 30-day postoperative mortality for obstructive AMI (Table 5).
 |
Table 5 Independent Risk Factors of 30-Day Postoperative Mortality in the Patients with Obstructive AMI |
Factors Affecting Postoperative Mortality of AOMI
The 77 obstructive AMI patients underwent laparotomy included 45 AOMI and 32 MVT. There were 18 deaths (40.0%) within 30 days of surgery for AOMI and five deaths (15.6%) within 30 days of surgery for MVT. Therefore, further exploration of 30-day postoperative mortality risk factors for AOMI was performed. The univariate analysis presented non-survivors had a lower platelet count ((144±44)*109/L vs (206±76)*109/L, P = 0.003), a higher fibrinogen (5.1±2.0g/L vs 3.6±1.6g/L, P = 0.006), and a longer time interval from admission to surgery (12.1±6.9 hours vs 7.4±3.8 hours, P = 0.006) (Table 6).
 |
Table 6 Factors Effecting 30-Day Postoperative Mortality in the Patients with AOMI |
The above potential risk factors were further analyzed by multivariate logistic regression analysis, the time interval from admission to surgery (OR 1.22; 95% CI [1.01–1.47], P = 0.036) and platelet count (OR = 0.98; 95% CI [0.97–0.99], P = 0.020) were independent risk factors for 30-day postoperative mortality of AOMI (Table 7).
 |
Table 7 Independent Risk Factors of 30-Day Postoperative Mortality in Patients with AOMI |
Discussion
Obstructive AMI is a surgical emergency with high mortality, and we should distinguish it from other benign abdominal diseases. In this study, we divided all 108 patients into two categories based on the location of thrombus or embolism, including AOMI and MVT. Because the incidence of obstructive AMI is relatively low, and multiple causes may induce obstructive AMI, randomized controlled studies of obstructive AMI are not common, so this study is also a retrospective design.
Understanding the clinical manifestations and comorbidities of obstructive AMI helps the early diagnosis and differentiation of its subtypes. Previous studies have reported that AOMI patients experienced cardiac disease more often, while MVT patients were often related to the hypercoagulable state.7,8 This difference was also confirmed in our research. As far as the subtypes of obstructive AMI are concerned, some studies have reported that the primary type of obstructive AMI was the arterial origin, while the venous origin AMI was relatively rare.3,9 However, in this study, 54% of obstructive AMI were AOMI, and the remaining patients were MVT. In developed countries, the reason why AOMI was more prevalent than MVT might be related to the aging population and the prevalence of cardiovascular diseases. While the Chinese populations are still relatively young, and the burden of liver cirrhosis is heavy (prevalence 0.5%). This may be an essential reason for the many MVT patients in this study. Therefore, when implementing preventive strategies for obstructive AMI, we should consider the differences in population structure and disease susceptibility factors in different regions.
Men appear to be more susceptible than women to obstructive AMI in this study, but the majority of obstructive AMI patients in previous reports were female,9–11 which may be related to the fact that there are more MVT patients among the 108 patients, and the proportion of male in MVT patients is 78.4%, which is consistent with the previous reports.7,12 A large number of MVT patients included in this study also caused the average age of patients with obstructive AMI (57 years) to be younger than previous reports (70 years).9–11 Compared with MVT, AOMI has higher plasma fibrinogen. The high level of plasma fibrinogen may play a pathogenic role in the occurrence of AOMI. The mechanism may be through the bridging of its glycoprotein IIb-IIIa receptors to strengthen platelets and act as the direct substrate of blood clots, thereby forming arterial thrombosis, and the shedding of arterial thrombosis can induce new embolism.13 Another reason may be that the average age of AOMI patients is older, and high fibrinogen is a sign of the chronic inflammatory state of aging. Besides, AOMI patients had higher high-density lipoproteins, which may be related to more patients with a history of heart disease. There is no statistical difference in the high-density lipoprotein between AOMI patients without heart disease and MVT. AOMI with a history of heart disease may use statins and fibrates for a long time, and statins or fibrates can directly or indirectly induce high-density lipoprotein increases.14,15 In short, clinicians need to understand these clinical characteristics of each subtype of obstructive AMI, especially for emergency doctors and gastrointestinal surgeons, to better distinguish between AOMI and MVT early.
Abdominal contrast-enhanced CT is a fast, non-invasive, and highly accurate method that is recommended for patients with high clinical suspicion of intestinal ischemia and can also be used to distinguish from other abdominal abnormalities.16 However, the accuracy of ordinary CT is not high for the diagnosis of any kind of AMI. In our study, the contrast-enhanced CT and a high index of suspicion of ischemia made the diagnosis of AMI clearly after admission.
The diagnosis and treatment of obstructive AMI should start from the early diagnosis, followed by basic life support, antibacterial therapy, and the rational use of anticoagulation therapy according to the patient’s etiology.3,17 For patients with high suspicion of intestinal necrosis, exploratory laparotomy is a definite treatment.6 In our study, 77 patients with surgical indicators or whose condition gradually got worse underwent laparotomy. Among them, 75 patients showed obvious necrosis of the intestine. Not all patients had used second-look surgery. Only when the intestinal vitality cannot be assessed, we will perform a second-look surgery. This treatment strategy was similar to previous reports.18–20 No patients received endovascular treatment because many patients in this study showed signs of peritonitis. From the AMI patients who underwent laparotomy, almost all patients had some degree of intestinal necrosis, while endovascular techniques are often more suitable for AMI patients who have not experienced intestinal necrosis.20 However, recent studies showed that for arterial-derived AMI, whether the disease was at an early stage or there was already intestinal necrosis, we should consider vascular reconstruction, endovascular techniques, and open surgery during treatment.21 Therefore, the combined treatment of gastrointestinal surgery and vascular surgery may improve the overall management of obstructive AMI.
For patients who urgently need exploratory laparotomy, the knowledge of the risk factors of postoperative death can help physicians to optimize the management and take personalized interventions to reduce postoperative mortality. Advanced age has been considered a risk factor related to death in previous studies of AMI.2,3 However, in this study, the advanced age did not appear in the results of the multivariate analysis. So the simply advanced age should not consider as a contraindication for laparotomy. Previous studies showed the postoperative mortality risk of AOMI was higher than that of MVT.22,23 Our study also showed that AOMI was an independent risk factor for 30-day postoperative mortality of obstructive AMI. And multivariate logistic regression also showed that lower platelet count at admission was also an independent risk factor, which was similar to previous researches.24,25 However, whether the mortality of obstructive AMI is directly related to the lower platelet count or is related to the disease behind the low platelet is worthy of further exploration.
The time interval from admission to surgery was also strongly proved to be related to 30-day postoperative mortality of obstructive AMI. The delay of surgery in some patients in this study might be related to waiting for emergency contrast-enhanced CT results to form the treatment decisions. Although this study was conducted in a large tertiary hospital in western China, it might still take more than three hours to complete the emergency contrast-enhanced CT and obtain the results. Previous studies have shown that if AMI does not receive active intervention within 24 hours of acute symptoms, the mortality rate will increase significantly.22 Therefore, for those patients who were highly suspected of obstructive AMI, improving the efficiency of CT examination, strengthening doctor–patient communication, and active laparotomy may also help to reduce the scope of intestinal necrosis and further reduce the overall short-term mortality of obstructive AMI.
This study further analyzed the postoperative mortality risk factors of AOMI. Logistic multivariate regression analysis showed that low platelet count at admission and a long time interval between admission and surgery were associated with higher mortality. Compared with overall obstructive AMI, the time interval from hospital admission to surgery was more important for AOMI. Given that waiting for contrast-enhanced CT results may cause delays in surgery, the different clinical characteristics between AOMI and MVT may help clinicians to achieve a preliminary distinction and then take more active interventions.
The main limitations of our study are the lack of randomness, retrospectiveness, and the fact that specific patient groups in a single center. From another perspective, these were rather advantages that postoperative mortality risk factors of obstructive AMI among different institutions might be heterogeneity. Therefore, our research may provide unique and specific insights into the optimization of obstructive AMI in western China.
Conclusion
Early identification of AOMI, improving the efficiency of enhanced CT examination, strengthening doctor–patient communication, active laparotomy, and optimize platelet management may also help reduce the overall short-term mortality of obstructive AMI. Building the multidisciplinary team model of diagnostic imaging, vascular intervention, and surgical treatment to manage obstructive AMI may be urgently needed in western China.
Acknowledgments
This study was supported by Sichuan University West China Hospital Disciplinary Excellence Development 1.3.5 Project (ZY2016105).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Clair DG, Beach JM. Mesenteric ischemia. New England J Med. 2016;374(10):959–968. doi:10.1056/NEJMra1503884
2. Crawford RS, Harris DG, Klyushnenkova EN, et al. A statewide analysis of the incidence and outcomes of acute mesenteric ischemia in Maryland from 2009 to 2013. Frontierssurgery. 2016;3:22. doi:10.3389/fsurg.2016.00022
3. Park WM, Gloviczki P, Cherry KJ
4. LI X, GU Y, YU H, et al. Diagnosis and treatment of acute mesenteric venous thrombosis. Chinese J General Surgery. 2009;6.
5. Zhong-Zhen T. Analysis of 30 patients with mesenteric ischemia disease [J]. China J Modern Med. 2006;11.
6. Acosta S. Surgical management of peritonitis secondary to acute superior mesenteric artery occlusion. World J Gastroenterol. 2014;20(29):9936. doi:10.3748/wjg.v20.i29.9936
7. Eslami MH, Rybin D, Doros G, McPhee JT, Farber A. Mortality of acute mesenteric ischemia remains unchanged despite significant increase in utilization of endovascular techniques. Vascular. 2016;24(1):44–52. doi:10.1177/1708538115577730
8. Acosta-Merida MA, Marchena-Gomez J, Hemmersbach-Miller M, Roque-Castellano C, Hernandez-Romero JM. Identification of risk factors for perioperative mortality in acute mesenteric ischemia. World J Surg. 2006;30(8):1579–1585. doi:10.1007/s00268-005-0560-5
9. Oldenburg WA, Lau LL, Rodenberg TJ, Edmonds HJ, Burger CD. Acute mesenteric ischemia: a clinical review. Arch Intern Med. 2004;164(10):1054–1062. doi:10.1001/archinte.164.10.1054
10. Stoney RJ, Cunningham CG. Acute mesenteric ischemia. Surgery. 1993;114(3):489–490.
11. Alhan E, Usta A, Cekic A, Saglam K, Turkyilmaz S, Cinel A. A study on 107 patients with acute mesenteric ischemia over 30 years. Int J Surgery. 2012;10(9):510–513. doi:10.1016/j.ijsu.2012.07.011
12. Karkkainen JM. Acute mesenteric ischemia in elderly patients. Expert Rev Gastroenterol Hepatol. 2016;10(9):985–988. doi:10.1080/17474124.2016.1212657
13. Tracy RP. Hemostatic and inflammatory markers as risk factors for coronary disease in the elderly. Am J Geriatr Cardiol. 2002;11(2):93–101. doi:10.1111/j.1076-7460.2002.00997.x
14. Chapman M. Are the effects of statins on HDL-cholesterol clinically relevant? European Heart J Supplements. 2004;6(suppl_C):C58–C63. doi:10.1016/j.ehjsup.2004.04.002
15. Rubins HB, Robins SJ, Collins D, et al. Gemfibrozil for the secondary prevention of coronary heart disease in men with low levels of high-density lipoprotein cholesterol. New England J Med. 1999;341(6):410–418. doi:10.1056/NEJM199908053410604
16. Menke J. Diagnostic accuracy of multidetector CT in acute mesenteric ischemia: systematic review and meta-analysis. Radiology. 2010;256(1):93–101. doi:10.1148/radiol.10091938
17. Harward TR, Green D, Bergan JJ, Rizzo RJ, Yao JS. Mesenteric venous thrombosis. J Vasc Surg. 1989;9(2):328–333. doi:10.1016/0741-5214(89)90053-0
18. Hedayati N, Riha GM, Kougias P, et al. Prognostic factors and treatment outcome in mesenteric vein thrombosis. Vasc Endovascular Surg. 2008;42(3):217–224. doi:10.1177/1538574407312653
19. Levy P, Krausz M, Manny J. The role of second-look procedure in improving survival time for patients with mesenteric venous thrombosis. Surg Gynecol Obstet. 1990;170(4):287–291.
20. Blauw JT, Bulut T, Oderich GS, Geelkerken BR. Mesenteric vascular treatment 2016: from open surgical repair to endovascular revascularization. Best Pract Res Clin Gastroenterol. 2017;31(1):75–84. doi:10.1016/j.bpg.2017.01.002
21. Nuzzo A, Maggiori L, Ronot M, et al. Predictive factors of intestinal necrosis in acute mesenteric ischemia: prospective study from an intestinal stroke center. Am J Gastroenterol. 2017;112(4):597–605. doi:10.1038/ajg.2017.38
22. Schoots I, Koffeman G, Legemate D, Levi M, Van Gulik T. Systematic review of survival after acute mesenteric ischaemia according to disease aetiology. British J Surgery. 2004;91(1):17–27. doi:10.1002/bjs.4459
23. Adaba F, Askari A, Dastur J, et al. Mortality after acute primary mesenteric infarction: a systematic review and meta‐analysis of observational studies. Colorectal Disease. 2015;17(7):566–577. doi:10.1111/codi.12938
24. Merle C, Lepouse C, De Garine A, et al. Surgery for mesenteric infarction: prognostic factors associated with early death within 72 hours. J Cardiothorac Vasc Anesth. 2004;18(6):734–741. doi:10.1053/j.jvca.2004.08.011
25. Groteluschen R, Bergmann W, Welte MN, Reeh M, Izbicki JR, Bachmann K. What predicts the outcome in patients with intestinal ischemia? A single center experience. J Visc Surg. 2019;156(5):405–411. doi:10.1016/j.jviscsurg.2019.01.007
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
