Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 15
Clinical Features and C-Reactive Protein as Predictors of Bacterial Exacerbations of COPD
Authors Francis NA , Gillespie D , Wootton M, White P , Bates J, Richards J, Melbye H , Hood K , Butler CC
Received 6 June 2020
Accepted for publication 23 September 2020
Published 1 December 2020 Volume 2020:15 Pages 3147—3158
DOI https://doi.org/10.2147/COPD.S265674
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Richard Russell
Nick A Francis,1 David Gillespie,2 Mandy Wootton,3 Patrick White,4 Janine Bates,2 Jennifer Richards,3 Hasse Melbye,5 Kerenza Hood,2 Christopher C Butler6
1Primary Care, Population Sciences and Medical Education, University of Southampton, Southampton, England, UK; 2Centre for Trials Research, Cardiff University, Cardiff, Wales, UK; 3Specialist Antimicrobial Chemotherapy Unit, Microbiology Cardiff, Public Health Wales, Cardiff, Wales, UK; 4School of Population Health and Environmental Sciences, King’s College London, London, England, UK; 5Department of Community Medicine, UIT the Arctic University of Norway, Tromsø, Norway; 6Nuffield Department of Primary Care Health Sciences, University of Oxford, Oxford, England, UK
Correspondence: Nick A Francis
Primary Care, Population Sciences and Medical Education, University of Southampton, Aldermoor Health Centre, Southampton SO16 5ST, UK
Email [email protected]
Introduction: Identifying predictors of bacterial and viral pathogens in sputum from patients with acute exacerbations of chronic obstructive pulmonary disease (COPD) may help direct management.
Methods: We used data from a trial evaluating a C-reactive protein (CRP) point of care guided approach to managing COPD exacerbations in primary care. We used regression analyses to identify baseline clinical features, including CRP value in those randomized to testing, associated with bacterial, viral or mixed infections, defined by the presence of bacterial and viral pathogens in sputum, detected by culture or polymerase chain reaction (PCR), respectively.
Results: Of 386 participants with baseline sputum samples, 79 (20.5%), 123 (31.9%), and 91 (23.6%) had bacterial, viral/atypical, and mixed bacterial/viral/atypical pathogens identified, respectively. Increasing sputum purulence assessed by color chart was associated with increased odds of finding bacterial and mixed (bacterial and viral/atypical) pathogens in sputum (area under the ROC curve (AUROC) for bacterial pathogens =0.739 (95% CI: 0.670, 0.808)). Elevated CRP was associated with increased odds of finding bacterial pathogens and mixed pathogens but did not significantly increase the AUROC for predicting bacterial pathogens over sputum color alone (AUROC for combination of sputum color and CRP = 0.776 (95% CI: 0.708, 0.843), p for comparison of models = 0.053). We found no association between the presence of sputum pathogens and other clinical or demographic features.
Conclusion: Sputum purulence was the best predictor of sputum bacterial pathogens and mixed bacterial viral/atypical pathogens in patients with COPD exacerbations in our study. Elevated CRP was associated with bacterial pathogens but did not add to the predictive value of sputum purulence.
Keywords: COPD, exacerbation, infection, bacteria, sputum, primary care
Plain Language Summary
People with chronic obstructive pulmonary disease (COPD) can experience flare-ups with cough, shortness of breath and producing more phlegm. These flare-ups can be caused by viral infections, bacterial infections, or other causes such as pollution or changes in the weather. It can be difficult for doctors, nurses and patients to know what is causing a flare-up. This is important because antibiotics will only help if bacteria are causing the flare-up, and antibiotics are often overused, leading to antibiotic resistance.
In this study, we used data from a randomized trial of patients presenting in primary care with a COPD flare-up. Participants were asked to provide a sample of sputum (phlegm), which was tested for bacteria and viruses that commonly cause infections. We then did statistical tests to see what factors were associated with having bacteria in the sputum.
Less than half of the patients had harmful bacteria in their sputum. Having sputum that was more green (purulent) was associated with having bacteria, and using a color chart resulted in better prediction than just asking the patient if their sputum had become more green. More green sputum was associated with bacteria whether or not viruses were present. Higher levels of the blood marker C-reactive protein (CRP) was also associated with bacteria but did not improve how well sputum color predicted bacteria.
In this study, sputum becoming more green, assessed using a color chart, was the best predictor of finding harmful bacteria in people with a COPD flare-up.
Introduction
Acute exacerbations of chronic obstructive pulmonary disease (AECOPD) are associated with deleterious effects on morbidity, mortality, and healthcare utilization.1 Potentially pathogenic bacteria can be identified in the sputum of just over half of all community-based patients with AECOPD.2,3 However, AECOPD can also be associated with viral infections, mixed bacterial-viral infections, cold air,4 air pollution,5 or unknown factors.6 Around three-quarters of patients consulting in primary care for AECOPD are prescribed an antibiotic, and experts have estimated that this should be reduced to around 54%.7 With around 95% of all healthcare contacts for COPD taking place in primary care,8 there is considerable potential for more personalized prescribing decisions to improve the targeting of antibiotics to those most likely to benefit, and enhance the focus on non-antibiotic interventions for those who are unlikely to benefit from antibiotics. Enhancing personalized decision making can be done through better clinical prediction models. In addition, point of care testing could add further diagnostic value, but this has not been adequately assessed in patients consulting in primary care with AECOPD. Overuse of antibiotics wastes resources, promotes the development of resistant organisms, and causes harm through side effects and distracting from other potentially more beneficial treatments. Antimicrobial resistance is a major threat to public health,9 and increasing resistant bacteria in patients living with COPD may make subsequent AECOPDs harder to treat.10
Antibiotic treatment confers only modest benefits for outpatients with AECOPD,11 and guidance on how to identify patients more likely to benefit from antibiotic treatment is vague. Three features identified by Anthonisen (increased sputum volume, increased sputum purulence and increased breathlessness)12 have been used for years as a guide to antibiotic treatment. However, a more recent study found that only sputum purulence and C-reactive protein (CRP) level predicted benefit from antibiotic treatment.13
We recently conducted a randomized-controlled trial of using a CRP point of care test to guide antibiotic prescribing decisions in primary care for patients presenting with AECOPD, and demonstrated a 20% reduction in use of antibiotics.14 However, it is still not clear whether bacterial exacerbations can be identified by clinical features, and whether CRP measurement adds diagnostic value to clinical assessment alone.
We therefore set out to determine the clinical features associated with detecting bacterial pathogens in the sputum of people experiencing AECOPD in primary care, and the added diagnostic value of CRP measured at the point of care.
Materials and Methods
This is a secondary analysis of data from the PACE trial.14,15 The PACE trial randomized 653 patients presenting in primary care with AECOPD to care as usual or use of a C-reactive protein point of care test (CRP POCT) to guide antibiotic therapy. The PACE study was approved by the Research Ethics Committee (REC) for Wales recognized by the United Kingdom Ethics Committee Authority (REC reference: 14/WA/1106), and all participants provided informed consent.
Participating primary care clinicians recruited sequential eligible participants and collected information about duration of illness, symptoms, comorbid illness (coronary heart disease, chronic heart failure, hypertension, diabetes, chronic kidney disease, other chronic disease), and clinical findings (pulse, temperature, oxygen saturation, chest findings). They also asked the participant to provide a sputum sample, which was assessed by the recruiting clinician for purulence by grading the color from 1 to 5 by using the Bronkotest [now called the Birmingham Sputum Colour Chart, Stockley, Birmingham, UK], with a higher grade indicative of a greater degree of purulence, and then sent to the study laboratory by first class post using compliant packaging. Participants who could not produce a sputum sample during the consultation were asked to grade the color of their sputum using the same 1 to 5 scale. Patients randomized to the CRP arm of the trial had a CRP measurement taken by the participating clinician using an Afinion desktop point of care device (Alere, now Abbott).
All sputum samples were processed in the Specialist Antimicrobial Chemotherapy Unit Laboratory for Public Health Wales using the laboratory’s standard operating procedures. Potential pathogenic bacteria (including Streptococcus pneumoniae, Haemophilus influenzae/parainfluenzae, Moraxella catarrhalis, Pseudomonas species, Enterobacterales and Staphylococcus aureus) were identified from sputum samples using standard culture techniques and Matrix-Assisted Laser Desorption Ionizing Time of Flight Mass Spectrometry (MALDI-ToF-MS), and semi-quantitatification was performed using chromogenic agar and a spiral plater. Nucleic acid was extracted from sputum samples using the EasyMag system then analyzed with the Luminex NxTAG Respiratory Pathogens Panel PCR system for a variety of viral and atypical bacterial pathogens. PCR was not used for detecting conventional bacterial pathogens.
Using data from the MALDI-ToF-MS baseline sputum samples were classified as containing: a) one or more bacterial pathogens, or b) no bacterial pathogens. Using data from the MALDI-ToF-MS and Luminex NxTAG analyses samples were further classified as containing, a) only bacterial pathogens, b) bacterial and viral pathogens, c) only viral pathogens, or d) no respiratory pathogens isolated.
We fitted mixed effects (participants within practices) binary logistic regression models to identify predictors of isolating a bacterial pathogen (yes/no) from sputum. We also fitted multinomial logistic regression models using the four pathogen categories described previously (no respiratory pathogen as the reference), inflating standard errors for the clustering of participants within practices using a clustered sandwich estimator. Predictors included in the model were: age, gender, smoking status, the presence of comorbid illness (heart failure, coronary heart disease, diabetes mellitus, chronic kidney disease, hypertension, ‘other chronic illness’), GOLD stage (using most recent recorded FEV1), duration of symptoms (in days), the presence or absence of the following features as measured at baseline (tachypnoea, crackles, wheeze, diminished vesicular breathing, evidence of consolidation, temperature (<36, 36–37.9, ≥38 °C), sputum color (1–5 using the Bronkotest (with 1–2 being non-purulent and 3–5 being purulent)) and CRP category. In the PACE study, we gave clinicians advice based on using the CRP categories <20 mg/L, 20–40 mg/L and >40 mg/L. However, we found that more than 70% of participants had CRP measurements <20 mg/L. Furthermore, CRP < 5mg/L is the lower limit of detection for the device we used. Therefore, for this analysis, we used the categories <5 mg/L, 5–19, 20–39, ≥40mg/L. CRP values were only available for those allocated to the CRP arm in the trial. We also included the Anthonisen criteria (increased breathlessness, increased sputum production and increased sputum purulence). For the binary logistic regression, candidate predictors which were statistically significant at p<0.05 in univariable analyses were included in a multivariable model. Sputum color and CRP categories were fitted as both categorical and continuous variables, with the latter fit used to explore any linear relationship between increasing purulence/CRP and pathogen detection. The area under the receiver operating characteristic (AUROC) was estimated to examine the performance of graded sputum color with and without the addition of CRP category in predicting sputum samples containing potentially pathogenic bacteria. For the four-category outcome (a) only bacterial pathogens, b) bacterial and viral pathogens, c) only viral pathogens, or d) no respiratory pathogens isolated) we fitted multiple univariable models but did not fit a multivariable model because the numbers in each category were too small. We also explored the association between sputum color and number of bacterial pathogens (0, 1, 2+) using a Chi-squared test.
Findings of the binary and multinomial logistic regression models are presented as odds ratios and relative risk ratios respectively, with associated 95% confidence intervals and p-values. Analyses were conducted using Stata version 16.0.
Results
Baseline sputum pathogen data were available for 386/653 (59.1%) participants. One hundred and seventy (44.0%) participants had one or more bacterial pathogens isolated and 216 (56.0%) did not have any bacterial pathogens. Seventy-nine (20.5%) had one or more bacterial pathogens with no viral/atypical pathogens isolated, 91 (23.6%) had both bacterial and viral/atypical pathogens isolated, 123 (31.9%) had one or more viral/atypical pathogens and no bacterial pathogens isolated, and 93 (24.1%) had no bacterial or viral/atypical pathogens isolated. The most common bacterial pathogens isolated were H. influenza, M. catarrhalis, S. pneumoniae and P. aeruginosa (Figure 1A), and most participants had relatively low growths of these organisms (Table 1). The most common viral/atypical pathogens isolated were Rhinovirus/Enterovirus, Human metapneumovirus, Coronavirus and Influenza (Figure 1B).
 |
Table 1 Growth of the Most Common Bacterial Pathogens* |
 |
Figure 1 Bacterial (A) and viral/atypical (B) pathogens isolated from baseline sputum samples. |
Older age; comorbid diabetes mellitus, chronic kidney disease and hypertension; patient reported increase in sputum purulence; graded sputum purulence (using the Bronkotest color chart) and CRP; were all associated with finding a bacterial pathogen in the sputum in univariable analyses (Table 2). Sputum purulence using the color chart was the only factor that remained statistically significant in multivariable analysis. A CRP of 5–19 mg/mL was found to be significantly associated with bacterial pathogens when compared to a CRP of 0–4 mg/mL, but none of the other categories of elevated CRP reading were statistically significant, and a test for trend was not significant (p=0.214). We found a significant linear association between sputum purulence and bacterial pathogens (p=0.005), and those with the most purulent sputum had almost 25 times the odds of finding a bacterial pathogen in the sputum compared with those with the least purulent sputum (AOR 24.8 (95% CI: 3.2 to 194.1)). Sputum purulence increased with increasing numbers of bacterial pathogens (Figure 2) and to a lesser extent increasing numbers of viral pathogens (supplementary Figures 1 and 2) isolated in the sputum (p< 0.001). As sputum colour increased, the distribution of CRP categories changed, with higher CRP values typically observed for higher sputum colours (supplementary Figure 3). Sputum purulence gave an area under the ROC curve (AUROC) of 0.739 (95% CI: 0.670, 0.808). Adding CRP category negligibly increased this (AUROC for combination of sputum color and CRP = 0.771 (95% CI: 0.703, 0.839), p for comparison of models = 0.062).
 |
Table 2 Association Between Demographic and Clinical Features, and Finding a Bacterial Pathogen in Sputum* |
 |
Figure 2 Association between sputum color and number of bacterial pathogens isolated. |
There was no evidence to suggest an association between sociodemographic or most clinical features and identifying bacterial pathogens alone, viral pathogens alone, or both bacterial and viral pathogens. Increased sputum volume was associated with an increased risk of viral/atypical pathogens alone and mixed bacterial and viral/atypical pathogens. Increased sputum purulence was associated with an increased risk of bacterial pathogens alone, viral/atypical pathogens alone, and mixed bacterial and viral/atypical pathogens (all compared with no pathogens). An increase in graded sputum color was associated with an increased risk of bacterial pathogens alone, viral/atypical pathogens alone, and mixed bacterial and viral/atypical pathogens (p-values for linear trend <0.001, 0.021, and <0.001, respectively). CRP levels greater than 0–4 were associated with increased odds of detecting bacterial pathogens and mixed bacterial and viral/atypical pathogens (compared with no pathogens)(p-values for linear trend =0.008 and 0.008, respectively). There was insufficient evidence to suggest that a raised CRP was associated with the detection of viral/atypical pathogens alone, compared with no pathogens (p-value for linear trend =0.103)(Figure 3). We found no evidence to suggest that increased breathlessness was associated with identifying bacterial or viral pathogens (Table 3).
 |
Table 3 Univariable Associations Between Demographic and Clinical Predictors and Bacterial, Viral/Atypical, or Both Bacterial and Viral/Atypical Pathogens in Sputum* |
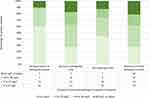 |
Figure 3 CRP Category by type (bacterial, viral, mixed or none) of pathogen isolated. |
Discussion
In this secondary analysis of data from a randomized controlled trial of CRP point of care testing to guide antibiotic use in primary care, we found that sputum purulence was the best predictor of identifying bacterial pathogens in sputum in patients with acute exacerbation of COPD. Assessing sputum purulence using a color chart (Bronkotest) was the only predictor that was significantly associated with bacterial pathogens in our multivariable model. However, sputum purulence was not specific to bacterial pathogens, with increased purulence being associated with both bacterial and viral pathogens alone and in combination. We found an association between an increase in CRP values and the presence of bacterial pathogens (both alone and mixed with viral/atypical pathogens) compared with no pathogens. We did not find evidence that using CRP category improves the predictive properties of sputum color in detecting bacterial pathogens in sputum.
This unique primary care study collected sputum samples and potential predictors, including sputum color using a standardized chart, for over 380 participants. We used comprehensive culture and molecular techniques to identify both bacterial and viral/atypical pathogens, and had data on sociodemographic, comorbid, and clinical predictors. However, this was a secondary analysis of trial data and our study was likely underpowered for some potential predictors, especially CRP for which we only had data from half the participants (those randomized to have a CRP test) and there were very few participants with results in the higher categories. Sputum color was assessed using a color chart that has been shown to be of value in detecting bacterial pathogens.16 Although use of a color chart is likely to improve the objectivity of sputum color assessment there will still be a degree of subjectivity in the assessment and we have not been able to identify any published data on the inter- or intra-rater reliability of this tool. Assessment is also likely to be affected by lighting conditions and ambient light, but this reflects real-life use of a tool like this. Despite this variability, clinician-assessed sputum color was associated with bacterial pathogens when other clinician-assessed characteristics were not, therefore suggesting that use of a color chart to assess sputum has some value in this setting.
It is important to highlight that although microbial pathogens are an essential component of infection, detecting pathogens is not the same as having an infection. This is particularly true for sputum samples, which may contain commensal (or pathogenic) organisms from the upper respiratory tract. Most of the pathogens we detected were found to have low growth. This was particularly true for the more fastidious organisms such as S. pneumoniae and H. influenzae, which may have died during transport to the lab, but could also be consistent with detection of commensal organisms as opposed to organisms causing infections. However, these were patients who were experiencing a clear exacerbation, as demonstrated by their recovery over the four weeks following recruitment.14 Viral pathogens are less likely to be simply commensals, but may not be the main cause of symptoms in an individual in whom they have been isolated. Samples were collected in participating general practices and transported to the study laboratory. They were refrigerated if stored overnight before transport, but transported at room temperature. Nevertheless, we were able to culture pneumococci, an organism known to be fastidious and prone to dying during transportation, in a significant proportion of participants.
We detected bacterial pathogens in just under half (44%) of patients, which is similar to the 35%-55% seen in other primary and secondary care studies using culture.17–20 Sputum purulence has previously been shown to be a predictor of bacterial pathogens in patients with AECOPD or chronic bronchitis in hospital settings.16,17,19,20 Our findings are consistent with these reports but also demonstrate that purulence is associated with bacterial pathogens in patients with AECOPD in the primary care setting, and that it is common with finding a mixed bacterial and viral/atypical picture. We found a stronger association between the presence of bacterial pathogens and sputum purulence measured using a color chart rather than a binary question about patient reported increase in sputum purulence. A previous study also found that sputum purulence measured objectively with a color chart is a better predictor of bacterial pathogens than patient reported purulence.21 Although sputum color was associated with both bacterial and viral infections, the association with purely viral infections was much weaker than was found for purely bacterial or mixed bacterial/viral exacerbations. Previous studies have shown an association between finding bacterial pathogens in the sputum of patients with acute exacerbation of COPD and increased dyspnea,19,20 male gender,19 FEV1,17 BMI,17 Albumin,20 and absence of fever/lower body temperature.19,20 We did not find an association with gender, FEV1, or increase in dyspnea, did not have data on BMI or albumin, and had so few patients with abnormal body temperature we were unable to include it in the model. Our findings suggest that patients with a COPD exacerbation in whom both bacterial and viral pathogens (and a combination of the two) can be isolated are more likely to have elevated CRP levels (≥5 mg/L) compared to patients in whom no pathogens are isolated. However, although we were able to demonstrate a significant trend between CRP categories and finding bacterial and mixed bacterial and viral/atypical pathogens, this was not the case for just viral pathogens. We only had CRP measurements for half our participants, and these analyses are exploratory and underpowered. A previous study in hospitalized patients with AECOPD found a strong association between CRP level and both viral and mixed bacterial/viral detection, but not detection of bacterial pathogens alone.22 Other reported predictors of viral infections are sputum eosinophils and higher temperature.18,22
Two further points warrant discussion. The first is that microbiology tests are measuring the presence of respiratory pathogens in sputum which may or may not be causing an infection, whereas CRP is measuring something very different - the body’s inflammatory response (potentially from an infection). Therefore, it may be that these two measurements are complementary, with microbiology testing indicating whether a potential pathogen is present or not, and CRP measuring the body’s response to the challenge. Those who mount a limited inflammatory response may be experiencing an infection with a lower bacterial load or with less virulent organisms, and may be less likely to benefit from antibiotics even when bacterial pathogens are present. This hypothesis is supported by a secondary analysis of a trial of antibiotics for patients with COPD exacerbations which found that purulence and CRP both predicted benefit from antibiotics.13 The second point to make is that not all patients are able to produce a sputum sample for assessment of purulence (only 59% of participants in the PACE study were able to produce a baseline sputum sample for analysis), and it is possible that CRP may have a role in predicting bacterial infection in those unable to produce a sputum sample.
Conclusions
Sputum purulence assessed using a color chart was the best predictor of bacterial pathogens in the sputum of primary care patients presenting with AECOPD, but it is not specific to bacterial pathogens, with increased purulence being associated with viral and mixed infections as well. Elevation of CRP shows some evidence of being independently predictive of bacterial and viral pathogens, but we were not able to demonstrate that it added to the predictive value of sputum purulence in this study. Clinicians should consider using color charts, in addition to CRP measurement, to identify those more likely to benefit from antibiotics. We found no evidence to support using the Anthonisen features of patient reported increased sputum increased sputum volume or increased breathlessness, or any other features on history or examination, to predict the presence of respiratory pathogens in AECOPD.
Data Sharing Statement
Anonymised data from the PACE trial are available upon request.
Ethics
Ethics approval for the PACE trial was given on 15 September 2014 by the Research Ethics Committee (REC) for Wales (Wales REC 6), recognised by the United Kingdom Ethics Committee Authority (REC reference 14/WA/1106). This was a secondary analysis conducted by the original investigators, who had freely available access to the data, and the aims of this paper fell within the remit of the original ethics application.
Acknowledgments
We would like to acknowledge Rachel Lowe, Emma Thomas-Jones, Nigel Kirby, Micaela Gal (all from Cardiff University); Evgina Riga (University of Oxford); Ann Cochrane (King’s College London); Carl Llor (University Institute in Primary Care Research Jordi Gol, Barcelona); and Jochen Cals (Maastricht University), who helped lead and manage the data collection for the trial. We would also like to thank the study participants, participating practices, and primary care networks for their contribution to this research.
Funding
This study is a secondary analysis of data collected by a project funded by the NIHR Health Technology Assessment Program (project number 12/33/12). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. The work was undertaken with the support of: 1) The UK Clinical Research Collaboration (UKCRC) registered Clinical Trials Unit, the Centre for Trials Research, and funding from Health and Care Research Wales and Cancer Research UK, under the auspices of the UKCRC collaboration, is gratefully acknowledged, and; 2) The UK Clinical Research Collaboration (UKCRC) registered University of Oxford Primary Care and Vaccines Clinical Trials Collaborative.
Disclosure
Nick A Francis reports grants from NIHR HTA, during the conduct of the study. David Gillespie reports grants from the National Institute for Health Research, during the conduct of the study. Janine Bates reports grants from NIHR HTA, during the conduct of the study. Kerenza Hood report grants from NIHR HTA, during the conduct of the study; and I am a member of three NIHR funding committees: HTA General Committee, HTA Funding Committee Policy Group and the Research Professors panel. Christopher C Butler reports grants from the National Institute for Health Research Health Technology Assessment Programme, during the conduct of the study. The authors report no other potential conflicts of interest for this work.
References
1. Anzueto A. Impact of exacerbations on COPD. Eur Respir Rev. 2010;19(116):113–118. doi:10.1183/09059180.00002610
2. Bafadhel M, McKenna S, Terry S, et al. Acute Exacerbations of Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2011;184(6):662–671. doi:10.1164/rccm.201104-0597OC
3. Wilkinson TMA, Aris E, Bourne S, et al. A prospective, observational cohort study of the seasonal dynamics of airway pathogens in the aetiology of exacerbations in COPD. Thorax. 2017;72(10):919–927. doi:10.1136/thoraxjnl-2016-209023
4. Donaldson GC, Seemungal T, Jeffries DJ, Wedzicha JA. Effect of temperature on lung function and symptoms in chronic obstructive pulmonary disease. Eur Respir J. 1999;13(4):844–849. doi:10.1034/j.1399-3003.1999.13d25.x
5. Anderson HR, Spix C, Medina S, et al. Air pollution and daily admissions for chronic obstructive pulmonary disease in 6 European cities: results from the APHEA project. Eur Respir J. 1997;10(5):1064–1071. doi:10.1183/09031936.97.10051064
6. Miravitlles M. Exacerbations of chronic obstructive pulmonary disease: when are bacteria important? Eur Respir J. 2002;20(Supplement 36):9s–19s. doi:10.1183/09031936.02.00400302
7. Pouwels KB, Dolk FCK, Smith DRM, Robotham JV, Smieszek T. Actual versus ‘ideal’ antibiotic prescribing for common conditions in English primary care. J Antimicrob Chemother. 2018;73(suppl_2):19–26. doi:10.1093/jac/dkx502
8. Punekar YS, Shukla A, Müllerova H. COPD management costs according to the frequency of COPD exacerbations in UK primary care. Int J Chron Obstruct Pulmon Dis. 2014;9:65–73. doi:10.2147/COPD.S54417
9. O’Neill J. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations. 2016. HM Gov Welcome Trust UK; 2018.
10. Wilson R, Anzueto A, Miravitlles M, et al. Prognostic factors for clinical failure of exacerbations in elderly outpatients with moderate-to-severe COPD. Int J Chron Obstruct Pulmon Dis. 2015;10:985–993. doi:10.2147/COPD.S80926
11. Vollenweider D, Frei A, Steurer‐Stey C, Garcia‐Aymerich J, Puhan M. Antibiotics for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2018;10. doi:10.1002/14651858.CD010257.pub2
12. Anthonisen N. Antibiotic Therapy in Exacerbations of Chronic Obstructive Pulmonary Disease. Ann Intern Med. 1987;106(2):196–204. doi:10.7326/0003-4819-106-2-196
13. Miravitlles M, Moragas A, Hernández S, Bayona C, Llor C. Is it possible to identify exacerbations of mild to moderate COPD that do not require antibiotic treatment? Chest. 2013;144(5):1571–1577. doi:10.1378/chest.13-0518
14. Butler CC, Gillespie D, White P, et al. C-Reactive Protein Testing to Guide Antibiotic Prescribing for COPD Exacerbations. N Engl J Med. 2019;381(2):111–120. doi:10.1056/NEJMoa1803185
15. Bates J, Francis NA, White P, et al. General practitioner use of a C-reactive protein point-of-care test to help target antibiotic prescribing in patients with acute exacerbations of chronic obstructive pulmonary disease (the PACE study): study protocol for a randomised controlled trial. Trials. 2017;18(1):442. doi:10.1186/s13063-017-2144-8
16. Stockley RA, O’Brien C, Pye A, Hill SL. Relationship of Sputum Color to Nature and Outpatient Management of Acute Exacerbations of COPD. Chest. 2000;117(6):1638–1645. doi:10.1378/chest.117.6.1638
17. Tsimogianni AM, Papiris SA, Kanavaki S, et al. Predictors of positive sputum cultures in exacerbations of chronic obstructive pulmonary disease. Respirology. 2009;14(8):1114–1120. doi:10.1111/j.1440-1843.2009.01615.x
18. Papi A, Bellettato CM, Braccioni F, et al. Infections and Airway Inflammation in Chronic Obstructive Pulmonary Disease Severe Exacerbations. Am J Respir Crit Care Med. 2006;173(10):1114–1121. doi:10.1164/rccm.200506-859OC
19. Miravitlles M, Kruesmann F, Haverstock D, Perroncel R, Choudhri SH, Arvis P. Sputum colour and bacteria in chronic bronchitis exacerbations: a pooled analysis. Eur Respir J. 2012;39(6):1354–1360. doi:10.1183/09031936.00042111
20. Ra SW, Kwon YS, Yoon SH, et al. Sputum bacteriology and clinical response to antibiotics in moderate exacerbation of chronic obstructive pulmonary disease. Clin Respir J. 2018;12(4):1424–1432. doi:10.1111/crj.12671
21. Daniels JMA, de Graaff CS, Vlaspolder F, Snijders D, Jansen HM, Boersma WG. Sputum colour reported by patients is not a reliable marker of the presence of bacteria in acute exacerbations of chronic obstructive pulmonary disease. Clin Microbiol Infect off Publ Eur Soc Clin Microbiol Infect Dis. 2010;16(6):583–588. doi:10.1111/j.1469-0691.2009.02892.x
22. Clark TW, Medina M, Batham S, Curran MD, Parmar S, Nicholson KG. C-reactive protein level and microbial aetiology in patients hospitalised with acute exacerbation of COPD. Eur Respir J off J Eur Soc Clin Respir Physiol. 2015;45(1):76–86. doi:10.1183/09031936.00092214
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
