Back to Journals » International Journal of Nephrology and Renovascular Disease » Volume 15
Clinical Evaluation of Dapagliflozin in the Management of CKD: Focus on Patient Selection and Clinical Perspectives
Received 23 May 2022
Accepted for publication 12 October 2022
Published 1 November 2022 Volume 2022:15 Pages 289—308
DOI https://doi.org/10.2147/IJNRD.S234282
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Pravin Singhal
Khaled Nashar, Patricia Khalil
Department of Medicine, Allegheny Health Network, Pittsburgh, PA, USA
Correspondence: Khaled Nashar; Patricia Khalil, Email [email protected]; [email protected]
Abstract: Dapagliflozin is a selective sodium–glucose cotransporter 2 (SGLT2) inhibitor that was recently approved in the USA and the EU for the treatment of adults with chronic kidney disease (CKD) with or without diabetes mellitus (DM). The DAPA-CKD trial showed a 39% decline in the risk of worsening kidney function, onset of end-stage kidney disease, or kidney failure-related death. Patients with lower levels of eGFR and higher levels of albuminuria are among those who stand to gain the greatest absolute benefits. These benefits were similar in both patients with or without diabetes, thus undermining the hypothesis that these drugs mitigate glycemia-related nephrotoxicity. Suggested mechanisms for renal protection include hemodynamic effects; BP reduction and improving salt sensitivities and metabolic effects; and glucose, uric acid and triglycerides (TG)-lowering effects. There have been already many excellent reviews on dapagliflozin and CKD management. Most of them cover both efficacy and safety. This review will focus on clinical perspectives and patient selection for the practicing clinician.
Keywords: dapagliflozin, SGLT 2inhibitors, CKD, proteinuria
Introduction
Chronic Kidney Disease Management and the Evolution of SGLT-s Inhibitors
The Kidney Disease: Improving Global Outcomes (KDIGO) working group defines Chronic Kidney Disease (CKD) as abnormalities of kidney structure or function present for >3 months, with implications for health. The KDIGO CKD risk score is classified based on estimated glomerular filtration rate (eGFR) and albuminuria (Figure 1).1 Diabetes and hypertension remain the leading causes of CKD in the United States and worldwide.1
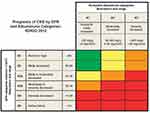 |
Figure 1 KDIGO CKD staging by GFR and albuminuria categories. Notes: Reprinted from Kidney Int Suppl, 3(1), Levin A, Stevens PE, Bilous RW, et al. Kidney Disease: Improving Global Outcomes CKD Working Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease, 1–150, Copyright (2013), with permission from Elsevier.1 |
CKD affects 12% of the global population and is a major cause of morbidity and mortality consuming a significant proportion of the health-care resources.2,3 According to the United States Center for Disease Control and Prevention (CDC), 1 in 7 (15%) US adults or a total of 37 million people are estimated to have CKD. Globally, the prevalence of CKD is estimated at 9.1% (697.5 million cases)4 CKD increases the risk for all-cause mortality, cardiovascular mortality, kidney failure, and other adverse outcomes. In 2018, treating Medicare beneficiaries with CKD cost over $81.8 billion, and treating people with end-stage kidney disease (ESKD) cost and additional $36.6 billion.3
Often times, CKD is referred to as the “silent killer” considering that as many as 9 in 10 adults with CKD do not know they have CKD. Global estimates indicate that 1.2 million deaths were attributable to chronic kidney disease in 2017. Additionally, about 2 in 5 adults with severe CKD do not know they have the disease, leading to delayed diagnosis and delivery of care.3,5
There is no cure for CKD and for decades, management has been focused on delaying its progression and preventing cardiovascular complications. Treatment options have been limited to blood pressure control, reduction of albuminuria and optimization of glycemic control. Clinicians have a few tools to achieve these treatment targets. Guidelines recommend reducing blood pressure to a target of 130/80 mm Hg in most CKD patients. Screening for proteinuria is recommended at the time of diagnosis and at least once a year thereafter. Random measurement of urinary albumin and urinary creatinine is the method of choice.1
For almost 20 years, angiotensin-converting enzyme inhibitors and angiotensin receptor blockers were the cornerstone of CKD progression retardation strategies. However, neither class reduced the risk of all-cause mortality in patients with CKD and evidence for their use in patients with CKD without T2D is relatively limited. Results from two landmark clinical trials: Reduction of Endpoints in NIDDM with the Angiotensin II Antagonist Losartan Study (RENAAL) and Irbesartan Diabetic Nephropathy Trial (IDNT), have shown a reduction in CKD progression in diabetic patients by 16–20% compared to placebo and calcium channel blockers.6,7 Although renin angiotensin aldosterone blocking drugs reduce the risk of adverse renal outcomes in patients with diabetes, the risk remains high and there is a large need for new treatments that lower the risk of kidney failure and improve cardiovascular risks independent of BP control.8 Furthermore, despite the above evidence of the benefits of renin aldosterone angiotensin system (RAAS) blockade, a large proportion of patients who meet the criteria for this treatment do not initiate it within 1 year of CKD diagnosis, highlighting a need for new therapies that can slow the progression of CKD.9
The Advent of SGLT-2 Inhibitors
Many years of research dedicated to understanding the role the kidneys play in handling glucose have led to the discovery of sodium-glucose co-transporters (SGLT). Currently, six different isoforms of SGLT cotransporters have been identified. However, SGLT-1 and 2 have been studied the most due to their role in glucose and sodium transport across the brush border of intestines and kidney cells.10 SGLT2 is a transport protein responsible for the reabsorption of approximately 90% of filtered glucose, with the remainder being absorbed by another transporter protein, sodium-glucose co-transporter 1 (SGLT1). The development of inhibitors targeting SGLT began with experiments around the compound phlorizin, first isolated over 150 years ago by French chemists from the root bark and the apple tree.11 In 1975, DeFronzo et al showed that phlorizin infusion in dogs increased fractional excretion of glucose by 60%, improving blood glucose levels without affecting the glomerular filtration rate and renal plasma flow. Despite these encouraging results, the use of phlorizins in the treatment of diabetes mellitus was not pursued due to their poor bioavailability and their interference with glucose transport in other parts of the body.12 It was not until 1995, when researchers found that phlorizin inhibited both SGLT1 and SGLT2 that revealed the phlorizin’s side effects as SGLT1 is found in many tissues and plays a key role in absorbing glucose in the intestine. Subsequent research focused on phlorizins more selective to SGLT2 led to their approval for the treatment of diabetes mellitus type 2 by the European Medicines Agency in 2012. In the US, the first SGLT2 inhibitor to be FDA-approved was canagliflozin (marketed as Invokana®) in March 2013, followed by the approval of dapagliflozin (marketed as Farxiga®) in January 2014 and empagliflozin (marketed as Jardiance®) in August 2014. Ertugliflozin (Steglatro®) was approved in 2017. A fifth SGLT2i, sotagliflozin (Zynquista) is being developed.13
SGLT2 inhibitors have a unique mechanism of action independent of insulin or insulin sensitivity resulting from inhibition of SGLT2 in the proximal tubule of the kidney and allowing for their use in combination with other hypoglycemic agents including insulin. Inhibition of SGLT2 results in decreased renal glucose reabsorption by approximately 50% and therefore modestly lower elevated blood glucose levels and glycated hemoglobin (HbA1c) levels in patients with type 2 diabetes. Along, they do not usually cause hypoglycemia. SGLT2 inhibitors also have a modest natriuretic effect that may lower blood pressure; however, this effect is typically transient due to other compensatory mechanisms. The blood pressure-lowering effect of SGLT2 inhibitors is likely influenced by several other effects of SGLT2 inhibition, including weight loss and diuresis.14
In 2008, the FDA antidiabetic drug guidance required cardiovascular outcome trials (CVOTs) for novel anti-diabetic medications to ensure that they do not increase the risk of myocardial infarction, stroke or cardiac death. Three SGLT2is (canagliflozin, empagliflozin, dapagliflozin) have been studied in cardiovascular outcomes trials; canagliflozin has also been studied in an additional randomized clinical trial involving patients with diabetic kidney disease. These studies revealed improved cardiovascular and renal outcomes which sparked interest in studying the cardio-renal protective effects of these agents.15
Table 1 summarizes the safety studies for the approved SGLT2 inhibitors available in the US.
 |
Table 1 Summary of Trials on SGLT2 Inhibitors with Kidney Outcomes |
Mechanisms of Action
SGLT2 inhibitors inhibit sodium and glucose reabsorption in the proximal tubule, leading to increased sodium and chloride delivery to the macula densa. This results in vasoconstriction in the afferent arteriolar secondary to adenosine-mediated myogenic activation which leads to a reduction in the intra-glomerular pressure and glomerular filtration rate.
Based upon this physiologic action on the kidney, many pathways which lead to the cardiovascular and renal protective effects of SGLT-2 inhibition are triggered and these include natriuresis, reduced intra-glomerular pressure, tubule-glomerular feedback, blood pressure lowering, and reduced oxidative stress and fibrosis.16
Figure 2 outlines the systemic effects and mechanisms of action for SGLT2 inhibitors.
 |
Figure 2 Mechanisms of action of SGLT2 inhibitors. |
Dapagliflozin in Diabetes Mellitus
Dapagliflozin is a potent and specific SGLT-2 inhibitor and hence it increases the amount of glucose excreted in the urine and improves both fasting and post-prandial plasma glucose levels in patients with T2D.17 The glucosuric effect of dapagliflozin results in caloric loss and a modest reduction in bodyweight, as well as mild osmotic diuresis and transient natriuresis.18 These benefits have been demonstrated by multiple randomized controlled trials.19
The glucose-lowering effect of dapagliflozin was similar in patients with or without cardiovascular disease and hypertension.20,21 In a pooled analysis of five, Phase 2–3 clinical trials of ≤52 weeks’ duration, patients with T2D and a history of heart failure saw an improvement in glycated hemoglobin from baseline (placebo-adjusted mean change −0.55%; baseline 8.2%), bodyweight (−2.7 kg; baseline ≈97 kg) and systolic blood pressure (−2.1 mmHg; baseline ≈134 mmHg) with dapagliflozin 10 mg monotherapy or add-on therapy to other glycemic agents (n = 171) relative to placebo/active comparator (n = 149).22
Effect on Blood Pressure
Dapagliflozin achieves modest decrease in blood pressure. This effect may be explained by the diuretic and natriuretic properties of the drug which cause a decrease in circulating volume.23 That being said, in two mechanistic studies, DAPASALT and DIAMOND, designed to study the effect of dapagliflozin in patients with CKD without T2D, it was demonstrated that during strictly controlled sodium intake, dapagliflozin increased glucosuria but not natriuresis or diuresis. This is probably related to compensatory mechanisms in the kidney that are activated during SGLT2 inhibition which may attenuate the natriuretic/osmotic-induced diuresis.24 This brings up the question, how can we still have blood pressure reduction if there is no increase in natriuresis? Experts explain this by the positive effects of SGLT-2 inhibition on endothelial function, arterial stiffness and pulse wave velocity.25
In two Phase 3 studies, 10 mg once daily of dapagliflozin reduced SBP and improved glycemic control in patients with inadequately controlled type 2 diabetes and hypertension despite their receiving antihypertensive therapy (angiotensin-converting enzyme inhibitor (ACEi)/angiotensin receptor blocker (ARB) therapy alone or in combination with one other antihypertensive.24,25 SBP reduction was greater when dapagliflozin was added to a β blocker or a calcium-channel blocker when compared to a thiazide diuretic.27
Dapagliflozin in Heart Failure
The cardiovascular (CV) benefits of dapagliflozin were first observed in the DECLARE-TIMI 58 trial, in which dapagliflozin 10 mg/day significantly reduced the risk of CV death or HF hospitalization in patients with T2D who had or were at risk for atherosclerotic CV disease.26 In the subsequent DAPA-HF trial, dapagliflozin 10 mg/day in addition to standard of care was associated with a significantly lower risk of worsening HF or CV death compared with placebo in patients with established heart failure, regardless of the presence or absence of T2DM. The benefits of Dapagliflozin also remained consistent regardless of background HF therapies.29
Dapagliflozin and Kidney Disease
We will review here the three major studies that examined dapagliflozin use in patients with chronic kidney disease. Inclusion criteria and patient characteristics in these trials are summarized in Table 2.
 |
Table 2 Patients Characteristics in Dapagliflozin Studies |
The DERIVE study (Efficacy and safety of dapagliflozin in patients with type 2 diabetes and moderate renal impairment (chronic kidney disease stage 3A), was a double-blind, multinational, phase 3 that evaluated the efficacy and safety of dapagliflozin in patients with type 2 diabetes and chronic kidney disease stage 3A. Patients with T2D and glycated hemoglobin of 7–11% and a BMI of 18–45 kg/m2 were receiving other glucose-lowering regimens and had CKD stage 3A were randomized to receive 24 weeks of dapagliflozin 10 mg once daily (n = 159) or placebo (n = 161). At week 24, dapagliflozin significantly (p = 0.05) lowered HbA1c (primary endpoint; placebo-adjusted mean change −0.34; baseline ≈8.2%), fasting blood glucose (−0.9 mmol/L; baseline ≈10 mmol/L), bodyweight (−1.3 kg; baseline ≈90 kg) and SBP (−3.1 mmHg; baseline ≈135 mmHg) relative to placebo.30
The DECLARE-TIMI 58 trial, a randomized, double-blind phase 3 study, was designed to assess the effects of dapagliflozin on CV and renal outcomes. This study initially excluded patients with CKD, however results from the 2015 EMPA-REG OUTCOME study began to show decreased risk of incident or worsening kidney disease, progression to macroalbuminuria, and doubling of serum creatinine in patients treated with empagliflozin. Similarly, the 2019 CREDENCE trial found that canagliflozin reduced the risk of several cardiovascular and renal outcomes. The DECLARE-TIMI trial subsequently began to include patients with CKD. The study’s two pre-specified secondary endpoints were renal composite outcome and death from any cause. At baseline, patients (n = 17,160 randomized) had a mean age of 64 years and 41% had established ASCVD, including coronary artery disease (33% of the patients) and heart failure (HF; 10%).25 The mean duration of diabetes was ≈11 years, mean HbA1c was 8.3% and the mean estimated glomerular filtration rate (eGFR) was 85 mL/min/1.73 m2 (45% and 7% of the patients had an eGFR of 60–90 and <60 mL/min/1.73 m2, respectively). Patients were randomized to receive dapagliflozin 10 mg once daily or placebo in addition to other glucose-lowering agents at the discretion of the treating physician. The median follow-up duration was 4.2 years (69,547 patient-years). dapagliflozin significantly lowered the rate of CV death/HHF versus placebo, but there was no significant between-group difference in the rate of major adverse cardiovascular events. Secondary analysis results suggested that dapagliflozin decreases the likelihood of progression of renal disease compared with placebo. The reduction in sustained decline in eGFR was ≥40% to <60 mL/min per 1.73 m2 [hazard ratio (HR) 0.54; 95% CI 0.43–0.67; p < 0.0001), end-stage kidney disease (ESKD; HR 0.31; 95% CI 0.13–0.79; p = 0.013), and renal death or ESKD (HR 0.41; 95% CI 0.20–0.82; p = 0.012). The mean decrease from baseline in eGFR was significantly (p < 0.0001) greater with dapagliflozin than placebo at 6 months, but had equalized with placebo by 2 years, and was significantly (p < 0.0001) less than placebo by 3 and 4 years after randomization.28,31
The DECLARE-TIMI 58, EMPA-REG OUTCOME and CREDENCE only included patients with diabetes, and whether this benefit would extend to for adults without T2DM was unclear at that point. This formed the question of whether dapagliflozin would affect the progression of chronic kidney disease and cardiovascular death in patients with or without type 2 diabetes and chronic kidney disease characterized by eGFR reduction and microalbuminuria. The Dapagliflozin And Prevention of Adverse Outcomes in Chronic Kidney Disease (DAPA-CKD) study, a multicenter, double-blind, randomized, placebo controlled study, was designed to answer this question. The study included 4304 participants with CKD (defined by eGFR of 25–75 mL/min/1.73 m2 and albuminuria with albumin-to-creatinine ratio (ACR) of 200–5000 mg/g) with and without T2DM and compared the effect of dapagliflozin to placebo. At least a third of patients without diabetes saw changes associated with ischemic and hypertensive nephropathy, and had chronic glomerulonephritis (especially IgA nephropathy). The study was stopped early after an interim safety analysis found conclusive evidence of the benefit of Dapagliflozin, which demonstrated to reduce the composite endpoint of decline of ≥50% in eGFR, new ESKD, renal mortality, or CVD mortality (9.2% vs 14.5%; HR 0.61; 95% CI 0.51–0.72; NNT=19). Remarkably, this benefit was similar regardless of T2D status. The medication was also associated with reduction in other endpoints, including all-cause mortality (4.7% vs 6.8%; 0.69; 0.53–0.88; NNT=48). There was a slightly higher risk of major hypoglycemia (0.7% vs 1.3%; P=0.04; NNH=166) with dapagliflozin use.
The study concludes that among patients with chronic kidney disease stages 2 through 4 and elevated levels of albuminuria, regardless of the presence or absence of diabetes, the risk of a sustained decline in eGFR of at least 50%, end-stage kidney disease, or death from renal or cardiovascular causes was significantly lowered (39%) when dapagliflozin is used in combination with standard of care treatment with RAAS blockade compared to placebo. The absolute risk reduction was 5.3% over a median time of 2.4 years, dapagliflozin also reduced the relative risk of death from any cause by 31% compared to placebo.32 The trial was unique in that one-third of patients did not have diabetes, and yet these benefits were the same regardless of diabetes status. This finding contradicts the hypothesis that such drugs mitigate glycemia-related nephrotoxicity.
The findings in the DAPA-CKD trial led the US Food and Drug Administration in April 2021 to approve dapagliflozin as the first drug that reduces the risk of kidney function decline, kidney failure, cardiovascular death and hospitalization for heart failure in adults with chronic kidney disease who are at risk of disease progression regardless of diabetes status.33
The DAPA-CKD results were followed by two sub-analyses. The first aimed to answer the question: is dapagliflozin safe in CKD stage 4 patients? Glenn M. Chertow et al analyzed data of 624 of 4304 (14%) patients in the DAPA-CKD study who had stage 4 CKD (estimated glomerular filtration rate [eGFR] <30 mL/min/1.73 m2). Compared with placebo, dapagliflozin was associated with a significant 27% improvement in the primary composite endpoint time of 50% or more decline in eGFR as well as end-stage kidney disease, or kidney or cardiovascular death in patients with advanced CKD. Furthermore, dapagliflozin significantly lowered both the risks for the kidney and cardiovascular endpoints by 29% and 17%, respectively, and the risk for all-cause mortality by 32%. Compared to placebo, dapagliflozin was superior at preservation of kidney function, with eGFR decreasing by 2.15 vs 3.38 mL/min/1.73 m2 per year. Rates of serious adverse events including major hypoglycemia, bone fractures, kidney-related events, and amputation were similar between the two groups. It was concluded that the effects of dapagliflozin among patients with stage 4 CKD are similar to those patients with mild-to-moderate CKD.34 It should be noted that the lower number of participants with eGFR <30 mL/min/1.73 m2 and the different underlying diseases may have caused a certain bias.
Another pre-specified subgroup analysis was performed to determine whether these outcomes were influenced by the presence or absence of cardiovascular disease. Of the total study population, 37.4% were secondary prevention patients, this group was predominantly males and likely to have diabetes. Additionally, the secondary prevention group had a higher BMI and blood pressure versus other participants. The primary and secondary prevention groups had similar eGFR and median urinary albumin-to-creatinine ratio. Rate of kidney failure was similar between the two groups, but the secondary prevention group had higher rates of adverse cardiovascular outcomes. The primary composite outcome (which included a sustained decline in eGFR of 50% or lower, end-stage kidney disease, and kidney or cardiovascular death) was significantly reduced by dapagliflozin treatment in both the primary and secondary prevention groups. Additionally, dapagliflozin treatment yielded similar reductions in terms of composite outcome of heart failure hospitalization, cardiovascular death, and all-cause mortality. No differences in rates of adverse events were detected between the groups. Based on these data, it was concluded that benefits from dapagliflozin are present in patients with and without cardiovascular disease.35
Another interesting sub-analysis examined the efficacy and safety of dapagliflozin in patients with immunoglobulin A nephropathy (IgAN). Of 270 participants with IgAN (254 [94%] confirmed by previous kidney biopsy), 137 were randomized to dapagliflozin and 133 to placebo. Mean age was 51.2 years; mean eGFR, 43.8 mL/min/1.73 m2; and median urinary albumin-to-creatinine ratio, 900 mg/g. Median follow-up was 2.1 years. The primary outcome occurred in six (4%) participants on dapagliflozin and 20 (15%) on placebo (hazard ratio, 0.29; 95% confidence interval, 0.12, 0.73). Mean rates of eGFR decline with dapagliflozin and placebo were −3.5 and −4.7 mL/min/1.73 m2/year, respectively. Dapagliflozin reduced the urinary albumin-to-creatinine ratio by 26% relative to placebo. Adverse events leading to study drug discontinuation were similar with dapagliflozin and placebo. There were fewer adverse events with dapagliflozin, and no new safety findings in this population. The analysis concluded that dapagliflozin reduces the risk of chronic kidney disease progression in participants with IgAN and has a favorable safety profile.36
Given the diversity of CKD etiologies in this study’s patients population, the results can be generalized to a wide spectrum of patients with CKD in clinical practice. Dual renin-angiotensin/SGLT2 inhibition may become the new standard. The same rule applies for patients with podocytopathy-related focal segmental glomerulosclerosis lesions. Experts believe that from now on, IgAN and podocytopathy trials without SGLT2 inhibition as background therapy and without glomerular filtration rate decline as a primary outcome criterion will be of limited value.37
It should be noted, however, that patients with type 1 diabetes, polycystic kidney disease, and recent immune disorders were not included in this trial. Furthermore, African American patients were poorly represented in most of the SGLT2 inhibitor studies including DAPA-CKD (4.4%), while 34% of the participants in the DAPA-CKD trial were Asian.38
Another limitation of the DAPA-CKD is that CKD patients without proteinuria (albuminuria <200 mg/g) were excluded; therefore, benefits in this patients’ group remain unknown.39
Dapagliflozin versus Other SGLT2 Inhibitors
Data from many large cardiovascular outcome trials in patients with diabetes (EMPA-REG, CANVAS, DECLARE-TIMI 58, and VERTIS CV) as well as heart failure (DAPA-HF1 and EMPEROR-Reduced2) have demonstrated consistent renal benefits from SGLT2 inhibitors including preservation of estimated glomerular filtration rate (eGFR) and reduced rates of renal outcomes. The CREDENCE trial (Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation), published in 2019, showed that in patients with T2D and urine albumin-to-creatinine ratio (UACR) of 300–5000 mg/g and eGFR of 30–90 mL/min/1.73 m2 100 mg/day, 100 mg/day of canagliflozin reduces the risk of the composite endpoint of end-stage kidney disease, doubling of serum creatinine from baseline, and death from renal or cardiovascular disease when compared to placebo (HR 0.70; 95% CI 0.59–0.82; p = 0.00001). Results from CREDENCE promoted a new KDIGO guideline of a class 1a recommendation that patients with type 2 diabetes and CKD with eGFR >30 mL/min/1.73 m2 be treated with an SGLT2 inhibitor.40
Similar changes in sCr and GFR were observed in both DAPA-CKD and CREDENCE compared to placebo. In the DAPA-CKD trial, dapagliflozin reduced the primary endpoint by 39%, resulting in a number needed to treat of 19. In CREDENCE, primary composite endpoints were reduced by 30%. However, DAPA-CKD cohort included patients with CKD without diabetes (32% of patients) and with more advanced kidney disease and less cardiac disease than the one enrolled in CREDENCE. The rate of heart failure was 10.9% and the rate of CVD was 37% at baseline in DAPA-CKD compared with 14.9% and 50.5% in CREDENCE.13,40
The EMPA-KIDNEY trial included patients with or without diabetes with eGFR 20–45 mL/min/1.73 m2 regardless of albuminuria or eGFR 45–90 mL/min per 1.73 m2 with UACR ≥200 mg/g on maximally tolerated RAAS blockade. A total of 6609 patients with a mean eGFR of 37.5 mL/min per 1.73 m2 were enrolled in this study. 48% of the participants had a UACR <300 mg/g. The primary outcome of this trial was a sustained ≥40% decline in eGFR, ESKD, or death from renal or cardiovascular causes. The EMPA-KIDNEY trial was stopped early in March 2022 for efficacy suggesting that CKD patients without albuminuria also benefit from SGLT2 inhibitors. The results are not published at the time of writing this manuscript.41
The choice of SGLT-2 inhibitor should be based upon the current FDA indication, the patient’s kidney function at time of initiation as well as affordability.
Table 3 compares different SGLT-2 inhibitors by indication.
 |
Table 3 SGLT-s Inhibitors Dosing and Indications |
Pharmacology/Pharmacodynamics Properties of Dapagliflozin
Dapagliflozin is rapidly absorbed following oral administration, with peak plasma concentrations usually achieved at 2 hours. Dapagliflozin pharmacokinetics are not affected by food. After a 10 mg dose, the absolute oral bioavailability of dapagliflozin is 78%. The mean steady-state volume of distribution of dapagliflozin is 118 L and it is ≈91% protein bound. The mean half-life is 12.9 hrs. Dapagliflozin is largely metabolized in the liver via CYP to an inactive metabolite (dapagliflozin 3-O-glucuronide). The drug and its metabolites are mainly excreted in the urine, with 75% of a dose recovered in the urine and 21% in the feces.39
Table 4 summarizes the drug characteristics.
 |
Table 4 Dapagliflozin Drug Characteristics |
Adverse Effects
Genital Infections
Genital contamination leading to vulvovaginitis and balanitis is considered the most common adverse reaction to dapagliflozin. In clinical trials of SGLT-2 inhibitors, there was a two- to fourfold increase (10–15% of women) in the incidence of vulvovaginal candidiasis. Results from twelve studies which included patients treated with dapagliflozin at a dose of 5mg, 10 mg and placebo, showed an infection rate of 5.7%, 4.8% and 0.9%, respectively.42,43 Patients should be cautioned when prescribing dapagliflozin regarding the possibility of genital infections. Dapagliflozin should be stopped in the case of recurrent or relapsing infections.
Urinary Tract Infections
In clinical trials, SGLT2 inhibitors increased the rate of urinary tract infections (8.8 versus 6.1%) There was a higher risk of emergent infections in those having previous history. Patients administered with dapagliflozin of 5mg, 10mg and placebo developed infection at rates of 5.7%, 4.3% and 3.7%, respectively. There are also reports of severe urosepsis and pyelonephritis with SGLT-s inhibitors’ use.14,44
A report in the annals of medicine outlined 55 unique case reports to the FDA of Fournier’s gangrene (FG) in patients receiving SGLT2 inhibitors between March 2013 and January 2019. The patients ranged in age from 33 to 87 years; 39 were men, and 16 were women. Time to onset after initiation of SGLT2-inhibitor therapy ranged from 5 days to 49 months. All patients had surgical debridement and were severely ill. Reported complications included diabetic ketoacidosis (n = 8), sepsis or septic shock (n = 9), and acute kidney injury (n = 4). Eight patients had fecal diversion surgery, 2 patients developed necrotizing fasciitis of a lower extremity that required amputation, and 1 patient required a lower-extremity bypass procedure because of gangrenous toes. Three patients died. For comparison, the FDA identified 19 FG cases associated with other antidiabetic agents between 1984 and 2019: metformin (n = 8), insulin glargine (n = 6), short-acting insulin (n = 2), sitagliptin plus metformin (n = 2), and dulaglutide (n = 1). These patients ranged in age from 42 to 79 years; 12 were men, and 7 were women. Two patients died.45,46
Four cases of FG attributed to the use of dapagliflozin specifically were published recently. Obesity and elevated levels of hemoglobin A1C were common patient characteristics in these cases. All patients were required to stay in the intensive care unit and underwent surgical intervention. The underlying mechanism is unclear; however, elevated blood glucose levels coupled with glucosuria caused by SGLT2 in patients with impaired microvascular supply and decreased immune response provide a favorable setup for urinary infections.
Further studies are needed to determine risk factors and to generate evidence for a causal connection between dapagliflozin and FG. In the meantime, it is advised to counsel patients about the low risk of FG though not a negligible one especially in patients who are obese and have poorly controlled diabetes mellitus.47
While history of UTIs does not preclude the use of dapagliflozin, patients should be forewarned about the increased risk, and the drug should be stopped in the case of recurrent or relapsing infections.
Bladder Cancer
In dapagliflozin clinical trials, there were 10 cases of bladder cancers. Five patients were diagnosed in the first 6 months of its use, a time period which is too limited to reliably indicate whether dapagliflozin is carcinogenic, but this finding certainly signals a risk. The FDA recommended post-marketing surveillance studies.48
A pooled analysis of 21 clinical trials has suggested that dapagliflozin is not linked to increased risk for bladder cancer. A total of 9/5936 dapagliflozin-treated patients versus 1/3403 otherwise-treated patients developed bladder cancer. All bladder cancer patients had clinical risk factors for the disease (>60 years of age, male patients, tobacco use and microscopic hematuria).49
A study is ongoing to compare the incidence of bladder and breast cancer among male and female patients with type 2 diabetes who are new users of dapagliflozin compared with those who are new users of antidiabetic agents in classes other than SGLT2 inhibitors, insulin monotherapy, metformin monotherapy, or sulfonylurea monotherapy.50 Till the results become available, it is recommended to avoid dapagliflozin in patients at increased risk of bladder cancer or with a prior history of bladder cancer.
Hypoglycemia
Dapagliflozin is not linked with hypoglycemia. When dapagliflozin is added to other hypoglycemic agents such as insulin and sulfonylurea, the combination increases the risk for hypoglycemia. It is recommended that at the initiation of therapy, hypoglycemic risks can be minimized by reducing the dose of other agents.51
Hypotension
By inducing glucosuria, SGLT2 inhibitors can cause osmotic diuresis and intravascular volume contraction. This may be especially be important in older patients, or those taking diuretics, or RAAS blocking agents.52
Using data from the DAPA-HF trial, researchers examined the effects of baseline systolic blood pressure on 1205 patients with heart failure and reduced ejection fraction who were randomized to either treatment with dapagliflozin or placebo. The dapagliflozin group experienced superior outcomes versus the placebo group across the range of SBP in adjusted and unadjusted analyses. dapagliflozin was well-tolerated and associated with better outcomes compared with placebo in patients with HFrEF across the range of SBP. Only a small proportion of patients experienced a decline in SBP to below 90 mmHg and this proportion was similar in each treatment group (6.3% with dapagliflozin and 5.6% with placebo); the equivalent proportion with a SBP decreasing to <85 mmHg was even smaller and balanced between treatment groups (2.9% and 2.7%, respectively).53
Dehydration
Dapagliflozin-based therapy is not associated with severe dehydration, considered to be an uncommon effect.54
Acute Kidney Injury (AKI)
Based on post-marketing Food and Drug Administration Adverse Events Reporting System (FAERS) reports, in June 2016, the US Food and Drug Administration (FDA) issued a warning that SGLT2is (especially canagliflozin and dapagliflozin) might cause AKI.55,56
There have been 101 cases of possible SGLT2-associated acute kidney injury reported to the FDA. Some of these post-marketing reports were in patients taking dapagliflozin. Some of which required hospitalizations and dialysis. Approximately half of these cases occurred within 1 month of initiating the drug, and most patients improved after discontinuation. It is not known how many patients had an underlying chronic kidney disease. Some patients may have been volume depleted, hypotensive, or taking other medications that could affect the kidneys. In one case report, a biopsy was done that revealed acute tubular necrosis. The patient recovered after 4 weeks on hemodialysis.57
In a systematic review and meta-analysis of the effect of SGLT2is on renal adverse events (AEs) in randomized controlled trials and controlled observational studies, 30 trials identified 410 serious AEs due to AKI. SGLT2is reduced the odds of developing AKI by 36% (odds ratio [OR] 0.64 [95% confidence interval (CI) 0.53–0.78], p < 0.001). A total of 1089 AKI events of any severity (AEs and serious AEs [SAEs]) were published in 41 trials (OR 0.75 [95% CI 0.66–0.84], p < 0.001). This sweeping review concluded that SGLT2i reduced the odds of suffering AKI with and without hospitalization in randomized trials and the real-world setting, despite the fact that more AEs related to hypovolemia have been reported.58
It is important to note that SGLT2 inhibitors induce an acute, reversible reduction in GFR, which is often referred to as the GFR “dip.” This response pattern suggests that these agents reduce glomerular hypertension, similar to what is seen with ACE inhibitors/ARBs’ use. The clinical implications of an acute eGFR dip were previously unknown and led to concerns around the risk of AKI with these therapies. However, data from three recent analyses— Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients (EMPA-REG OUTCOME), Evaluation of Ertugliflozin Efficacy and Safety Cardiovascular Outcomes Trial (VERTIS-CV), and canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) are reassuring and confirm the dip in eGFR is not associated with progressive long-term kidney function loss or AKI.59
A few recent case reports of biopsy-proven osmotic nephropathy with SGLT2-inhibitors have been published. These five patients ranged in age from 41 to 66 years, and all had DM/hypertension and CKD with eGFR ranging from 27 to 79 mL/min/176 m2. Three patients were on Dapagliflozin, 1 on canagliflozin and 1 patient on empagliflozin. Serum creatinine on presentation ranged from 1.1mg/dL to 10.7mg/dL (mean 4.6mg/dL). Kidney biopsy in all patients revealed findings consistent with osmotic nephropathy with vacuolization and cell swelling limited to the proximal tubules. With supportive care and SGLT2-inhibitor discontinuation, four patients recovered kidney function back to baseline and one patient left with higher stage CKD. Interestingly, osmotic nephropathy caused by phlorizin was described in 1935 by Homer Smith. The exact etiology of osmotic nephropathy caused by SGLT inhibitors is not entirely clear; however, a kidney biopsy may be warranted in patients with SGLT2 inhibitor–associated acute kidney injury that does not recover to baseline within 5–7 days.60
In the DAPA-CKD trial, the incidence of renal related adverse events (defined as doubling of serum Creatinine) between two subsequent study visits was 63 (2.9%) in the treatment group and 91 (4.2%) in the placebo group (hazard ratio 0.68 [95% confidence interval 0.49, 0.94]). Acute kidney injury–related serious adverse events were not significantly different between groups and occurred in 52 (2.5%) and 69 (3.2%) participants in the dapagliflozin and placebo groups, respectively (0.77 [0.54, 1.10]). This analysis suggests that dapagliflozin reduced the risk of abrupt declines in kidney function in patients with CKD and albuminuria.61
Nevertheless, renal function should be assessed prior to initiation of dapagliflozin and monitored during treatment. The drug should be used with caution in patients with comorbidities that might predispose to acute kidney injury (eg, heart failure, hypovolemia) and in conjunction with other medications that predispose to AKI (nonsteroidal anti-inflammatory drugs [NSAIDs], ACE inhibitors/ARBs, diuretics). Dose adjustments and more frequent monitoring are required in patients with moderate chronic kidney disease.
Diabetic Ketoacidosis (DKA) and Euglycemic DKA
SGLT2 inhibitors are thought to increase the risk of DKA. In a population-based cohort study from Canada and the United Kingdom, SGLT2 inhibitors (empagliflozin, dapagliflozin, canagliflozin) compared with dipeptidyl peptidase 4 (DPP-4) inhibitors were associated with an increased risk of DKA (incidence 2.03 versus 0.75 per 1000 person-years [HR 2.85, 95% CI 1.99–4.08]). Among the three SGLT2 inhibitors, canagliflozin was associated with the highest risk.62
In several studies, “euglycemic” DKA (Eu-DKA) has been reported in patients with type 2 diabetes taking dapagliflozin. Eu-DKA is an uncommon form of DKA that is characterized by metabolic acidosis (pH <7.3), a decreased level of serum bicarbonate (<18 mEq/L), and a relatively low blood glucose level (<200 mg/dL).63 In these individuals, the absence of substantial hyperglycemia delays recognition of the problem and makes diagnosis challenging.64,65
In one report, 33 articles on SGLT2 inhibitors-induced ketoacidosis in the context of surgical treatment were identified. According to this literature research, risk factors for the development are infection, perioperative fasting, surgical stress, and insulin dose reduction. This emphasizes the need to withhold treatment with SGLT-2 inhibitors for at least 24–48 h prior to surger.y66 Similarly, patients should hold the drug for illness or excessive exercise or alcohol intake and seek medical help early.
In DAPA-CKD, 0/2149 receiving dapagliflozin developed DKA compared to 2/2149 (<0.1) in the placebo group.32
The proposed mechanisms of eu-DKA induced by SGLT-2 inhibitors are as follows: SGLT-2 inhibitors reduce blood glucose levels, thereby decreasing the secretion of endogenous insulin by pancreatic β-cells. This in turn stimulates pancreatic α-cells, leading to increased glucagon secretion. SGLT-2 inhibitors also directly stimulate α-cells, thereby increasing plasma glucagon concentration and promoting hepatic ketogenesis.67
The risk of SGLT2 inhibitors with regard to DKA has been demonstrated in placebo-controlled trials in type 1 diabetes. An increased risk for DKA was seen in these studies even though participants at high risk for DKA were excluded at baseline and substantial efforts to mitigate this risk were undertaken. SGLT2 inhibitors are not indicated in type 1 diabetes mellitus and off-label use in type 1 diabetes is discouraged.67
In practice, patients should be instructed to avoid ketogenic diet “carbohydrate-free” diet. We also recommend checking serum ketones in any patient with nausea, vomiting, or malaise while taking SGLT2 inhibitors, and SGLT2 inhibitors should be discontinued if acidosis is confirmed. In addition, clinicians should be mindful that acute illnesses such as diffuse paralytic ileus and urinary tract infection, as well as dietary restrictions or fasting in patients with DM, can all be considered potential predisposing factors for SGLT-2 inhibitor-associated eu-DKA. Therefore, we recommend withholding SGLT2 inhibitors in this setting.
Amputations
Compared with other oral and injectable diabetes agents, SGLT2 inhibitors, particularly canagliflozin, are associated with an increased risk of amputation.68,69
In two randomized trials evaluating canagliflozin versus placebo in patients with type 2 diabetes and established CVD, there was an approximately two-fold increased risk of lower limb amputations (mostly toe and midfoot) in patients taking canagliflozin. Patients with a history of prior amputation, peripheral vascular disease, and neuropathy were at highest risk for amputation.70
In another study of over eight million case safety reports, 79 lower-limb amputations associated with the use of SGLT2 inhibitors were reported since 2013. An increased risk of lower-limb amputations was reported with canagliflozin, empagliflozin, and dapagliflozin (PRRs 8.91, 6.86, and 2.62, respectively).71
The incidence of amputations (defined as cases of surgical amputation or spontaneous or nonsurgical amputation, excluding amputation due to trauma) was 35/2149 (1.6%) in the dapagliflozin group versus 39/2149 (1.8%) in the placebo group.32
In clinical practice, SGLT2 inhibitors should be avoided in patients at risk for foot amputation, including neuropathy, foot deformity, vascular disease, and history of previous foot ulceration. Patients taking SGLT2 inhibitors should be monitored for signs and symptoms of foot ulceration.
Bone Fracture
Some studies have shown an increase in the incidence of fractures in patients taking canagliflozin. These low trauma fractures were reported within 12 weeks following initiation of the drug. Orthostatic hypotension was thought to be the underlying cause of these incidents.
A meta-analysis of trials evaluating safety outcomes did not show an increased risk of fracture with dapagliflozin or empagliflozin. The increase in fracture with canagliflozin was not significant (odds ratio [OR] 1.15, 95% CI 0.71–1.88).72 In addition, a total of 85/2149 (4.0) of patients treated with dapagliflozin in the DAPA-CKD study had fractures compared to 69/2149 (3.2) in those who received placebo.32
Patient Selection and Clinical Perspectives
Renal Indications
As stated above, several clinical trials provided clear and consistent data that SGLT2 inhibitors have marked renal benefits, with preservation of estimated glomerular filtration rate (eGFR) and reduced rates of renal outcomes observed with SGLT2 inhibitors compared with placebo in each of these trials. DAPA-CKD in particular created a paradigm shift in the management of chronic kidney disease (CKD). Current indications for dapagliflozin include chronic kidney disease stages 1–4 (eGFR>25 mL/min/1.73 m2) with proteinuria (>200 mg/g): To reduce the risk of sustained eGFR decline, end-stage kidney disease, cardiovascular death, and hospitalization for heart failure in adults with chronic kidney disease at risk of progression.32 The 2020 Kidney Disease Improving Global Outcomes (KDIGO) clinical practice guideline for management of diabetes and CKD aims to address this issue by providing new clinical recommendations and practical points for clinicians.2 The guideline recommends treatment with SGLT2i for patients with type 2 diabetes, CKD, and eGFR >30 mL/min per 1.73 m2 at any level of current glycemic control.73
Limitations of use: Dapagliflozin is not recommended in patients with type I diabetes, polycystic kidney disease, or in those who currently require or have a recent history of immunosuppressive therapy for kidney disease.
Figure 3 outlines the current approach to CKD with proteinuria and where dapagliflozin is indicated.
 |
Figure 3 Management of CKD with proteinuria. |
Contraindications
- Diabetes mellitus type 1
- Advanced CKD with eGFR <25 mL/min/1.73m2 (patients may continue 10 mg orally once daily to reduce the risk of eGFR decline, ESKD, CV death and HF)
- Prior diabetic ketoacidosis (DKA)
Precautions
- Frequent bacterial urinary tract infections or genitourinary yeast infections.
- In conjunction with NSAIDs, RAAS inhibitors, and diuretics.
- Peripheral vascular disease, foot ulceration, and neuropathy.
- Patients at high risk for Diabetic Ketoacidosis (DKA).
- Low bone mineral density and high risk for falls and fractures.
- Conditions that predispose to AKI, eg, liver disease and hypovolemia.
- Known history of bladder cancer or at risk of bladder cancer.
- Risk of hypovolemia, eg, ileostomy.
- SGLT-2 inhibitors should be withheld at least 24–48 hours prior to elective surgery, planned invasive procedures, or anticipated severe stressful physical activity and restarted only in stable clinical conditions.
- Patients with severe hepatic impairment were excluded from clinical trials and therefore we recommend avoiding using the drug in this population.
Prior to Initiating Dapagliflozin, Clinician Should
- Obtain a baseline kidney function (sCr, albuminuria/proteinuria) and liver function tests.
- Assess and correct hypovolemia as it is optimal to start therapy when the patient is euvolemic. Consider reducing the dose of diuretic therapy by 25–50% at the initiation of dapagliflozin.
- Decrease the dose of insulin and oral hypoglycemic agents to reduce the risk of hypoglycemia.
Dosing
Dose of 10 mg once daily can be taken any time of day with or without food.
For patients with reduced liver function, a starting dose of 5 mg is recommended.
In impaired renal function: if eGFR ≥45 mL/minute/1.73 m2, no dosage adjustment is necessary.
In patients with eGFR 25 to <45 mL/minute/1.73 m2, no dosage adjustment is necessary, but caution should be used.
In patients with eGFR <25 mL/minute/1.73 m2, dapagliflozin should not be initiated; however, patients previously established on dapagliflozin may continue 10 mg once daily. This is consistent with the DAPA-CKD trials enrollment.74
Monitoring During Treatment
Clinicians should monitor the following during treatment with dapagliflozin:
- Fasting blood sugar and glycated hemoglobin
- Renal function (BUN and sCr)
- Volume status and blood pressure
Even though most clinicians argue for the need to monitor renal function in all patients following the initiation of SGLT2 inhibitors, a recent report published in the Clinical Journal of American Society of Nephrology (CJASN) indicates that there is no need to have a routine monitoring strategy to check kidney function or electrolytes, unless there is a clinical concern about volume depletion in specific individuals, such as in patients with BP <120/70 mm Hg, sign/symptoms of volume depletion (eg, orthostatic symptoms), a regimen of high-dose diuretics, and perhaps among elderly patients. This recommendation is predicated on the concept that the risk of AKI is not increased, eGFR dipping is not associated with kidney injury, and that ultimately dipping should not affect management or continuation of therapy. Furthermore, unlike RAAS inhibitors, SGLT2 inhibitors do not cause hyperkalemia after initiation. Therefore, patients can safely undergo blood work at a subsequent follow-up appointment to avoid additional cost and unnecessary anxiety around an eGFR dip. The authors hope that this strategy will decrease the barriers to initiating guidelines-recommended therapy, particularly in the primary care setting.75 Monitoring renal function 4 weeks after initiating SGLT2 inhibitors is recommended for high-risk patients (prior episodes of kidney injury, advanced CKD and patients at risk of volume depletion). If serum creatinine rose >30% of baseline value, clinicians need to reassess blood pressure and volume status with consideration to reduce/hold diuretics, liberalize fluid intake or holding SGLT-2 inhibitors.
Clinicians should ask patients who are taking insulin or insulin secretagogues to monitor fasting and pre-meal glucose levels for the first few weeks following initiation or dose escalation of dapagliflozin.
Insulin dosing should be decreased by 10% to 20% and insulin secretagogue dosing by 50% if blood glucose fall <80 mg/dL.
Use of Dapagliflozin in Special Situations
Use in the Elderly
Special consideration should be given when prescribing dapagliflozin to elderly patients as they are predisposed to intravascular volume depletion. Clinicians should monitor for symptoms such as hypotension, orthostatic hypotension, dizziness, syncope, and dehydration before prescribing dapagliflozin.
The cardiovascular and renal benefits of dapagliflozin in elderly patients were evaluated in a sub-analysis of DECLARE-TIMI 58 trial, which included a large cohort of elderly and very elderly patients (65–75 and >75 years old). Similar results were noted across all age groups indicating that the overall efficacy and safety of dapagliflozin were consistent regardless of age.76
Dapagliflozin and Pregnancy
(SGLT2) inhibitors are not recommended for patients with type 2 diabetes mellitus planning to become pregnant. This is based on adverse effects on renal development observed in animal studies. Similarly due to the potential for serious adverse reactions in the breastfeeding infant, breastfeeding is not recommended by the manufacturer.74 Patients of child-bearing age should use effective contraception during therapy. Transition to a preferred therapy should be initiated prior to conception and contraception should be continued until glycemic control is achieved.
Dapagliflozin in Patients Who Received Kidney Transplant
Little is known about the safety and efficacy of SGLT2i in the kidney transplant setting. Concerns regarding increased risk of urinary tract infections, diabetic ketoacidosis and acute kidney injury limit their use in this patient population. In a single center, retrospective analysis of 50 adult kidney transplant recipients who were followed for a period of 6 months, improvement in weight (−2.95 kg [SD 3.54, P = <0.0001 (CI: 3.53, 1.50)]), hypomagnesemia (0.13 [SD 1.73, P = 0.0004 (CI: 0.06, 0.20)]) and insulin usage (−3.7 units [SD 22.8, P = 0.17]) was observed. Similar rate of UTIs was observed in patients receiving treatment compared to a control group. No incidence of DKA or amputations was observed. While conclusions cannot be accurately drawn from a single-center retrospective studies like this one and while randomized research is needed to further validate these results, this data serves as a hypothesis for future studies. In the meantime, the use of dapagliflozin should be avoided in the first-year post kidney transplant.77
Dapagliflozin: Current State and Future Directions
Real-world effectiveness studies have confirmed that the benefits of SGLT-2 inhibitors observed in clinical trials. CVD-REAL 3, a multinational observational cohort study, assessed kidney outcomes in 35,561 patients initiating SGLT2 inhibitors propensity matched to other glucose-lowering agents and found that SGLT2 inhibitors reduced eGFR decline by 1.53 mL/min per 1.73 m2 per year (95% CI 1.34–1.72).78 The efficacy and safety of dapagliflozin in patients with CKD was studied across 4 broad global regions: Asia, Europe, Latin America, and North America with no apparent effect modification by geographic region. Similar to randomized controlled trials, the composite outcome of 50% decline in eGFR, progression to ESKD or death from kidney or cardiovascular cause was lower with dapagliflozin.79 The effect of dapagliflozin on new-onset type 2 diabetes mellitus was assessed in a pooled analysis or patient-level data from the DAPA-CKD and the DAPA-HF trials with evidence of reduction of new-onset diabetes mellitus in participants with chronic kidney disease and heart failure.80
According to clinicaltrials.gov, there are 183 studies in progress using dapagliflozin in different disease states. A total of 23 of these studies are specific to kidney disease. Notable among them are a study exploring dapagliflozin outcomes in advanced kidney disease stages 4 and 5, vascular impact, as well as a study looking at pharmacokinetics and dialyzability of dapagliflozin in dialysis patients. Finally, a separate study is evaluating dapagliflozin in the transplant population, IgA nephropathy patients and those with FSCG.50
Acknowledgment
The authors would like to thank Caitlin Rossi for reviewing and editing the manuscript.
Disclosure
Dr Khaled Nashar is on the speaker bureau for Kerendia for Bayer Pharmaceutical and on the speaker bureau for Veltassa for Vifor Pharma, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Kidney Disease: Improving Global Outcomes CKD Working Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3(1):1–150.
2. Mills KT, Xu Y, Zhang W, et al. A systematic analysis of worldwide population-based data on the global burden of chronic kidney disease in 2010. Kidney Int. 2015;88:950–957. doi:10.1038/ki.2015.230
3. Bikbov B, Purcell CA, Levey AS; GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395:709–733. doi:10.1016/S0140-6736(20)30045-3
4. Centers for Disease Control and Prevention. Chronic Kidney Disease in the United States, 2021. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2021.
5. Rothberg MB, Kehoe ED, Courtemanche AL, et al. Recognition and management of chronic kidney disease in an elderly ambulatory population. J Gen Intern Med. 2008;23(8):1125–1130. doi:10.1007/s11606-008-0607-z
6. Brenner BM, Cooper ME, de Zeeuw D, et al.; RENAAL Study Investigators. Effects of losartan on renal and cardiovascular outcomes in patient with type 2 diabetes and nephropathy. N Engl J Med. 2001;345(12):861–869. doi:10.1056/NEJMoa011161
7. Lewis EJ, Hunsicker LG, Clarke WR, et al.; Collaborative Study Group. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes s. N Engl J Med. 2001;345(12):851–860. doi:10.1056/NEJMoa011303
8. Bavishi C, Bangalore S, Messerli FH. Renin angiotensin aldosterone system inhibitors in hypertension: is there evidence for benefit independent of blood pressure reduction? Prog Cardiovasc Dis. 2016;59(3):253–261. doi:10.1016/j.pcad.2016.10.002
9. Fried LF, Petruski-Ivleva N, Folkerts K, Schmedt N, Velentgas P, Kovesdy CP. ACE inhibitor or ARB treatment among patients with diabetes and chronic kidney disease. Am J Manag Care. 2021;27:S360–S368. doi:10.37765/ajmc.2021.88806
10. Wright EM, Loo DD, Panayotova-Heiermann M, et al. “Active” sugar transport in eukaryotes. J Exp Biol. 1994;196:197–212. doi:10.1242/jeb.196.1.197
11. Petersen C. Analyse des phloridzins. Ann Acad Sci. 1835;15:178.
12. Ehrenkranz JR, Lewis NG, Kahn CR, Roth J. Phlorizin: a review. Diabetes Metab Res Rev. 2005;21(1):31–38. doi:10.1002/dmrr.532
13. Nelinson DS, Sosa JM, Chilton RJ. SGLT2 inhibitors: a narrative review of efficacy and safety. J Osteopathic Med. 2021;121(2):229–239. doi:10.1515/jom-2020-0153
14. Clar C, Gill JA, Court R, Waugh N. Systematic review of SGLT2 receptor inhibitors in dual or triple therapy in type 2 diabetes. BMJ Open. 2012;2(5):e001007. doi:10.1136/bmjopen-2012-001007
15. Kluger AY, Tecson KM, Lee AY. Class effects of SGLT2 inhibitors on cardiorenal outcomes. Cardiovasc Diabetol. 2019;18:99. doi:10.1186/s12933-019-0903-4
16. Kidokoro K, Cherney DZI, Bozovic A, et al. Evaluation of glomerular hemodynamic function by empagliflozin in diabetic mice using in vivo imaging. Circulation. 2019;140:303–315. doi:10.1161/CIRCULATIONAHA.118.037418
17. Hsia DS, Grove O, Cefalu WT. An update on sodium-glucose co-transporter-2 inhibitors for the treatment of diabetes mellitus. Curr Opin Endocrinol Diabetes Obes. 2017;24(1):73–79. doi:10.1097/MED.0000000000000311
18. Bailey CJ, Gross JL, Pieters A, et al. Effect of dapagliflozin in patients with type 2 diabetes who have inadequate glycaemic control with metformin: a randomised, double-blind, placebo-controlled trial. Lancet. 2010;375(9733):2223–2233. doi:10.1016/S0140-6736(10)60407-2
19. Bolinder J, Ljunggren O, Kullberg J, et al. Effects of dapagliflozin on body weight, total fat mass, and regional adipose tissue distribution in patients with type 2 diabetes mellitus with inadequate glycemic control on metformin. J Clin Endocrinol Metab. 2012;97(3):1020–1031. doi:10.1210/jc.2011-2260
20. Leiter LA, Cefalu WT, de Bruin TW, et al. Dapagliflozin added to usual care in individuals with type 2 diabetes mellitus with preexisting cardiovascular disease: a 24-week, multicenter, randomized, double-blind, placebo-controlled study with a 28-week extension. J Am Geriatr Soc. 2014;62(7):1252–1262. doi:10.1111/jgs.12881
21. Cefalu WT, Leiter LA, de Bruin TWA, et al. Dapagliflozin’s effects on glycemia and cardiovascular risk factors in high-risk patients with type 2 diabetes: a 24-week, multicenter, randomized, double-blind, placebo-controlled study with a 28-week extension. Diabetes Care. 2015;38(7):1218–1227. doi:10.2337/dc14-0315
22. Dhillon S. Dapagliflozin: a review in type 2 diabetes. Drugs. 2019;79:1135–1146. doi:10.1007/s40265-019-01148-3
23. Heerspink HJL, Kurlyandskaya R, Xu J, et al. Differential effects of dapagliflozin on cardiovascular risk factors at varying degrees of renal function. Diabetes. 2016;65(Suppl 1):A286.
24. Sen T, Scholtes R, Greasley PJ, et al. Effects of dapagliflozin on volume status and systemic haemodynamics in patients with chronic kidney disease without diabetes: results from DAPASALT and DIAMOND. Diabetes Obes Metab. 2022;24(8):1578–1587. doi:10.1111/dom.14729x
25. Solini A, Giannini L, Seghieri M, et al. Dapagliflozin acutely improves endothelial dysfunction, reduces aortic stiffness and renal resistive index in type 2 diabetic patients: a pilot study. Cardiovasc Diabetol. 2017;16(1):138. doi:10.1186/s12933-017-0621-8
26. Weber MA, Mansfield TA, Alessi F, et al. Effects of dapagliflozin on blood pressure in hypertensive diabetic patients on renin-angiotensin system blockade. Blood Press. 2016;25(2):93–103. doi:10.3109/08037051.2015.1116258
27. Weber MA, Mansfield TA, Cain VA, et al. Blood pressure and glycaemic effects of dapagliflozin versus placebo in patients with type 2 diabetes on combination antihypertensive therapy: a randomised, double-blind, placebo-controlled, phase 3 study. Lancet Diabetes Endocrinol. 2016;4(3):211–220. doi:10.1016/S2213-8587(15)00417-9
28. Wiviott SD, Raz I, Bonaca MP, et al.; DECLARE–TIMI 58 Investigators. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380(4):347–357. doi:10.1056/NEJMoa1812389
29. McMurray JJV, Solomon SD, Inzucchi SE, et al.; DAPA-HF Trial Committees and Investigators. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381(21):1995–2008. doi:10.1056/NEJMoa1911303
30. Fioretto P, Del Prato S, Buse JB, et al. Efficacy and safety of dapagliflozin in patients with type 2 diabetes and moderate renal impairment (chronic kidney disease stage 3A): the DERIVE study. Diabetes Obes Metab. 2018;20(11):2532–2540. doi:10.1111/dom.13413
31. Mosenzon O, Wiviott SD, Cahn A, et al. Effects of dapagliflozin on development and progression of kidney disease in patients with type 2 diabetes: an analysis from the DECLARE–TIMI 58 randomised trial. Lancet Diabetes Endocrinol. 2019;7:606–617. doi:10.1016/S2213-8587(19)30180-9
32. Heerspink HJL, Stefánsson BV, Correa-Rotter R, et al.; DAPA-CKD Trial Committees and Investigators. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020;383(15):1436–1446. doi:10.1056/NEJMoa2024816
33. US Food & Drug Administration. FDA Approves Treatment for Chronic Kidney Disease. Available from: https://www.fda.gov/news-events/press-announcements/fda-approves-treatment-chronic-kidney-disease. US Food & Drug Administration US Food & Drug AdministrationAccessed October US Food & Drug Administration US Food & Drug Administration US Food & Drug Administration 12, 2022.
34. Chertow G, Vart P, Jongs N, et al. Effects of dapagliflozin in stage 4 chronic kidney disease. J Am Soc Nephrol. 2021;32:2352–2361. doi:10.1681/ASN.2021020167
35. McMurray JJV, Wheeler DC, Stefánsson BV, et al.; DAPA-CKD Trial Committees and Investigators. Effect of dapagliflozin on clinical outcomes in patients with chronic kidney disease, with and without cardiovascular disease. Circulation. 2021;143(5):438–448. doi:10.1161/CIRCULATIONAHA.120.051675
36. Wheeler DC, Toto RD, Stefánsson BV, et al.; DAPA-CKD Trial Committees and Investigators. A pre-specified analysis of the DAPA-CKD trial demonstrates the effects of dapagliflozin on major adverse kidney events in patients with IgA nephropathy. Kidney Int. 2021;100(1):215–224. doi:10.1016/j.kint.2021.03.033
37. Anders HJ, Peired AJ, Romagnani P. SGLT2 inhibition requires reconsideration of fundamental paradigms in chronic kidney disease, ‘diabetic nephropathy’, IgA nephropathy and podocytopathies with FSGS lesions. Nephrol Dial Transplant. 2020;gfaa329. doi:10.1093/ndt/gfaa329
38. Wheeler DC, Stefansson BV, Batiushin M, et al. The dapagliflozin and prevention of adverse outcomes in chronic kidney disease (DAPA-CKD) trial: baseline characteristics. Nephrol Dial Transplant. 2020;35(10):1700–1711. doi:10.1093/ndt/gfaa234
39. AstraZeneca. Forxiga (dapagliflozin): summary of product characteristics; 2019. Available from: https://www.ema.europa.eu/en.
40. Perkovic V, Jardine MJ, Neal B, et al.; CREDENCE Trial Investigators. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380(24):2295–2306. doi:10.1056/NEJMoa1811744
41. Herrington WG, Wanner C, Green JB; EMPA-KIDNEY Collaborative Group. Design, recruitment, and baseline characteristics of the EMPA-KIDNEY trial. Nephrol Dial Transplant. 2022;37(7):1317–1329. doi:10.1093/ndt/gfac040
42. Johnsson KM, Ptaszynska A, Schmitz B, Sugg J, Parikh SJ, List JF. Vulvovaginitis and balanitis in patients with diabetes treated with dapagliflozin. J Diabetes Complications. 2013;27:479–484. doi:10.1016/j.jdiacomp.2013.04.012
43. Bailey CJ, Gross JL, Hennicken D, Iqbal N, Mansfield TA, List JF. Dapagliflozin add-on to metformin in type 2 diabetes inadequately controlled with metformin: a randomized, double-blind, placebo-controlled 102-week trial. BMC Med. 2013;11:43. doi:10.1186/1741-7015-11-43
44. Musso G, Gambino R, Cassader M, Pagano G. A novel approach to control hyperglycemia in type 2 diabetes: sodium glucose co-transport (SGLT) inhibitors: systematic review and meta-analysis of randomized trials. Ann Med. 2012;44(4):375–393. doi:10.3109/07853890.2011.560181
45. Bersoff-Matcha SJ, Chamberlain C, Cao C, Kortepeter C, Chong WH. Fournier gangrene associated with sodium-glucose cotransporter-2 inhibitors: a review of spontaneous postmarketing cases. Ann Intern Med. 2019;170(11):764–769. doi:10.7326/M19-0085
46. Omer T, Dharan SS, Adler A. Sodium-glucose cotransporter 2 (SGLT-2) inhibitor dapagliflozin and Fournier’s gangrene: a life threatening severe adverse outcome: case report. Diabet Med. 2018;35(Suppl1):100.
47. Rodler S, Weig T, Finkenzeller C, Stief C, Staehler M. Fournier´s gangrene under sodium-glucose cotransporter 2 inhibitor therapy as a life-threatening adverse event: a case report and review of the literature. Cureus. 2019;11(9):e5778. doi:10.7759/cureus.5778
48. US Food & Drug Administration. Center for Drug Evaluation and Research. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2014/202293Orig1s000MedR.pdf.
49. Ptaszynska A, Cohen SM, Messing EM, et al. Assessing bladder cancer risk in type 2 diabetes clinical trials: the dapagliflozin drug development program as a ‘case study’. Diabetes Ther. 2015;6(3):357–375. doi:10.1007/s13300-015-0128-9
50. ClinicalTrials.gov. Cancer in Patients on Dapagliflozin and Other Antidiabetic Treatment Available from: https://www.clinicaltrials.gov/ct2/show/NCT02695121.
51. Zhang M, Zhang L, Wu B, Song H, An Z, Li S. Dapagliflozin treatment for type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Diabetes Metab Res Rev. 2014;30(3):204–221. doi:10.1002/dmrr.2479
52. Weir MR, Januszewicz A, Gilbert RE, et al. Effect of canagliflozin on blood pressure and adverse events related to osmotic diuresis and reduced intravascular volume in patients with type 2 diabetes mellitus. J Clin Hypertens. 2014;16(12):875–882. doi:10.1111/jch.12425
53. Serenelli M, Böhm M, Inzucchi SE, et al. Effect of dapagliflozin according to baseline systolic blood pressure in the Dapagliflozin and Prevention of Adverse Outcomes in Heart Failure trial (DAPA-HF). Eur Heart J. 2020;41(36):3402–3418. doi:10.1093/eurheartj/ehaa496
54. Brooks AM, Thacker SM. Dapagliflozin for the treatment of type 2 diabetes. Ann Pharmacother. 2009;43(7):1286–1293. doi:10.1345/aph.1M212
55. US Food & Drug Administration. FDA Drug Safety Communication: FDA strengthens kidney warnings for diabetes medicines canagliflozin (Invokana, Invokamet) and dapagliflozin (Farxiga, Xigduo XR) Available from: https://www.fda.gov/Drugs/DrugSafety/ucm505860.htm.
56. Perlman A, Heyman SN, Matok I, Stokar J, Muszkat M, Szalat A. Acute renal failure with sodium-glucose-cotransporter-2 inhibitors: analysis of the FDA adverse event report system database. Nutr Metab Cardiovasc Dis. 2017;27(12):1108–1113. doi:10.1016/j.numecd.2017.10.011
57. Pleros C, Stamataki E, Papadaki A, et al. Dapagliflozin as a cause of acute tubular necrosis with heavy consequences: a case report. CEN Case Rep. 2018;7(1):17–20. doi:10.1007/s13730-017-0283-0
58. Jan MenneI D, Eva DumannI D, Hermann Haller BM, Schmidt W. Acute kidney injury and adverse renal events in patients receiving SGLT2-inhibitors: a systematic review and meta-analysis. PLoS Med. 2019. doi:10.1371/journal.pmed.1002983
59. Hiddo JL, Heerspink DZI. Cherney clinical implications of an acute dip in eGFR after SGLT2 inhibitor initiation. CJASN. 2021;16(8):1278–1280. doi:10.2215/CJN.02480221
60. Perazella MA, Juncos LA. Drug-induced osmotic nephropathy: add SGLT2-inhibitors to the list? Kidney. 2022;3(3):550–553. doi:10.34067/KID.0007882021
61. Heerspink HJL, Cherney D, Postmus D, et al.; DAPA-CKD Trial Committees and Investigators. A pre-specified analysis of the Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease (DAPA-CKD) randomized controlled trial on the incidence of abrupt declines in kidney function. Kidney Int. 2022;101(1):174–184. doi:10.1016/j.kint.2021.09.005
62. Douros A, Lix LM, Fralick M, et al. Sodium-glucose cotransporter-2 inhibitors and the risk for diabetic ketoacidosis: a multicenter cohort study. Ann Intern Med. 2020;173(6):417. doi:10.7326/M20-0289
63. Lee IH, Ahn DJ. MDb dapagliflozin-associated euglycemic diabetic ketoacidosis in a patient with type 2 diabetes mellitus. Medicine. 2020;99(21):e20228. doi:10.1097/MD.0000000000020228
64. Fralick M, Schneeweiss S, Patorno E. Risk of diabetic ketoacidosis after initiation of an SGLT2 inhibitor. N Engl J Med. 2017;376(23):2300. doi:10.1056/NEJMc1701990
65. US Food & Drug Administration. FDA revises labels of SGLT2 inhibitors for diabetes to include warnings about too much acid in the blood and serious urinary tract infections Available from: https://www.fda.gov/drugs/drug-safety-and-availability/fda-revises-labels-sglt2-inhibitors-diabetes-include-warnings-about-too-much-acid-blood-and-serious#:~:text=FDA%20has%20added%20warnings%20about%20ketoacidosis%20and%20serious%20urinary%20tract,Inhibitors%20for%20Type%202%20Diabetes.
66. Kietaibl AT, Fasching P, Glaser K, Petter-Puchner AH. New diabetic medication sodium-glucose cotransporter-2 inhibitors can induce euglycemic ketoacidosis and mimic surgical diseases: a case report and review of literature. Front Surg. 2022;9:828649. doi:10.3389/fsurg.2022.828649
67. Taylor SI, Blau JE, Rother KI. SGLT2 inhibitors may predispose to ketoacidosis. J Clin Endocrinol Metab. 2015;100:2849–2852. doi:10.1210/jc.2015-1884
68. Chang HY, Singh S, Mansour O, Baksh S, Alexander GC. Association between sodium-glucose cotransporter 2 inhibitors and lower extremity amputation among patients with type 2 diabetes. JAMA Intern Med. 2018;178(9):1190. doi:10.1001/jamainternmed.2018.3034
69. Fralick M, Kim SC, Schneeweiss S, Everett BM, Glynn RJ, Patorno E. Risk of amputation with canagliflozin across categories of age and cardiovascular risk in three US nationwide databases: cohort study. BMJ. 2020;370:m2812. doi:10.1136/bmj.m2812
70. Neal B, Perkovic V, Matthews DR, et al. Rationale, design and baseline characteristics of the CANagliflozin cardioVascular Assessment Study-Renal (CANVAS-R): a randomized, placebo-controlled trial. Diabetes Obes Metab. 2017;19(3):387. doi:10.1111/dom.12829
71. Khouri C, Cracowski JL, Roustit M. SGLT-2 inhibitors and the risk of lower-limb amputation: is this a class effect? Diabetes Obes Metab. 2018;20(6):1531. doi:10.1111/dom.13255
72. Tang HL, Li DD, Zhang JJ, et al. Lack of evidence for a harmful effect of sodium-glucose co-transporter 2 (SGLT2) inhibitors on fracture risk among type 2 diabetes patients: a network and cumulative meta-analysis of randomized controlled trials. Diabetes Obes Metab. 2016;18(12):1199. doi:10.1111/dom.12742
73. Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group. Diabetes in CKD. Available from: https://kdigo.org/guidelines/diabetes-ckd/.
74. FARXIGA® (dapagliflozin) [package insert]. Wilmington, DE: AstraZeneca Pharmaceuticals LP; 2021.
75. Meraz-Muñoz AY, Weinstein J, Wald R. eGFR decline after SGLT2 inhibitor initiation: the tortoise and the hare reimagined. Kidney. 2021;2(6):1042–1047. doi:10.34067/KID.0001172021
76. Cahn A, Mosenzon O, Wiviott SD, et al. Efficacy and safety of dapagliflozin in the elderly: analysis from the DECLARE-TIMI 58 study. Diabetes Care. 2020;43(2):468–475. doi:10.2337/dc19-1476
77. Song CC, Brown A, Winstead R, et al. Early initiation of sodium-glucose linked transporter inhibitors (SGLT-2i) and associated metabolic and electrolyte outcomes in diabetic kidney transplant recipients. Endocrinol Diabetes Metab. 2020;4(2):e00185. doi:10.1002/edm2.185
78. Heerspink HJL, Karasik A, Thuresson M, et al. Kidney outcomes associated with use of SGLT2 inhibitors in real-world clinical practice (CVD-REAL 3): a multinational observational cohort study. Lancet Diabetes Endocrinol. 2020;8:27–35. doi:10.1016/S2213-8587(19)30384-5
79. Vart P, Correa-Rotter R, Hou FF, et al. Efficacy and safety of dapagliflozin in patients with CKD across major geographic regions. Kidney Int Rep. 2022;7(4):699–707. doi:10.1016/j.ekir.2022.01.1060
80. Rossing P, Inzucchi SE, Vart P, et al. Dapagliflozin and new-onset type 2 diabetes in patients with chronic kidney disease or heart failure: pooled analysis of the DAPA-CKD and DAPA-HF trials. Lancet Diabetes Endocrinol. 2022;10(1):24–34. doi:10.1016/S2213-8587(21)00295-3
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
