Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 16
Clinical Characteristics, Treatment Patterns and Economic Burden of COPD in Kyrgyzstan: A FRESH AIR Study
Authors Tabyshova A , Estebesova B, Beishenbekova A, Sooronbaev T, Brakema EA , Chavannes NH , Postma MJ, van Boven JFM
Received 7 June 2021
Accepted for publication 13 September 2021
Published 11 October 2021 Volume 2021:16 Pages 2833—2843
DOI https://doi.org/10.2147/COPD.S322778
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 6
Editor who approved publication: Dr Richard Russell
Aizhamal Tabyshova,1,2 Bermet Estebesova,3,4 Alina Beishenbekova,5 Talant Sooronbaev,1 Evelyn A Brakema,6 Niels H Chavannes,6 Maarten J Postma,2,7– 9 Job FM van Boven10
1Pulmonology Department, National Center of Cardiology and Internal Medicine Named After M.M. Mirrakhimov, Bishkek, Kyrgyzstan; 2Department of Health Sciences, Unit of Global Health, University of Groningen, University Medical Center Groningen, Groningen, The Netherlands; 3Kyrgyz-Russian Slavic University (KRSU), Bishkek, Kyrgyzstan; 4Primary Care Center of the Ministry of Internal Affairs, Bishkek, Kyrgyzstan; 5International Medical University, Bishkek, Kyrgyzstan; 6Department of Public Health and Primary Care, Leiden University Medical Center, Leiden, The Netherlands; 7Department of Economics, Econometrics & Finance, University of Groningen, Faculty of Economics & Business, Groningen, The Netherlands; 8Department of Pharmacology & Therapy, Airlangga University, Surabaya, Indonesia; 9Center of Excellence in Higher Education for Pharmaceutical Care Innovation, Universitas Padjadjaran, Bandung, Indonesia; 10University of Groningen, University Medical Center Groningen, Groningen Research Institute for Asthma and COPD (GRIAC), Groningen, The Netherlands
Correspondence: Aizhamal Tabyshova
Pulmonology Department, National Center for Cardiology and Internal Medicine, Togolok Moldo st. 3, Bishkek, 720040, Kyrgyzstan
Email [email protected]
Background: COPD prevalence and mortality in Kyrgyzstan are high. Data on clinical and economic impact of COPD in Kyrgyzstan are scarce. This study was part of the FRESH AIR research project that focused on prevention, diagnosis and treatment of chronic lung diseases in low-resource settings.
Aim: We aimed to evaluate the clinical characteristics, treatment patterns and economic burden of COPD in Kyrgyzstan.
Methods: A representative sample of patients with a spirometry-confirmed diagnosis of COPD was included. All patients were registered in one of the five major hospitals in Kyrgyzstan. Patients were surveyed on COPD risk factors, health-care utilization and patient reported outcomes (CCQ, MRC). Associations with high symptom burden (MRC score ≥ 4) and cost were assessed using logistic regression analyses.
Results: A total of 306 patients were included with mean age 62.1 (SD: 11.2), 61.4% being male, mean BMI 26.9 (SD: 5.2) and mean monthly income $85.1 (SD: 75.4). Biomass was used for heating and cooking by 71.2% and 52.0%. Current and ex-smokers accounted 14.1% and 32%. Mean FEV1 was 46% (SD: 12.8), 71.9% had COPD GOLD III–IV and most frequent co-morbidities were hypertension (25.2%), diabetes (5.6%) and heart diseases (4.6%). Mean CCQ score was 2.0 (SD: 0.9) and MRC score 3.7 (SD: 0.9). Yearly mean number of hospital days due to COPD was 10.1 (SD: 3.9). Total annual per-patient costs of reimbursed health-care utilization ($107) and co-payments ($224, ie, 22% of patients’ annual income) were $331. We found that only GOLD IV and hypertension were significantly associated with high symptom burden. Exacerbations and hypertension were significantly associated with high cost.
Conclusion: The clinical and economic burden of COPD on patients and the government in Kyrgyzstan is considerable. Notably, almost half of interviewed patients were current or ex-smokers and biomass exposure was high.
Keywords: COPD, clinical characteristics, economics, healthcare utilization, Kyrgyzstan
Introduction
The Global Burden of Disease Study reported a prevalence of 251 million cases of chronic obstructive pulmonary disease (COPD) globally in 2016.1 Of those, more than 90% of COPD deaths occur in low- and middle-income countries (LMIC). The primary cause of COPD is exposure to tobacco smoke (either active smoking or secondhand smoke). Other risk factors include exposure to indoor and outdoor air pollution and occupational dusts and fumes. Exposure to air pollution can affect the unborn child and represents a risk factor for developing COPD later in life.1
COPD is currently the third leading cause of death worldwide.2 The percentage of deaths from COPD in Kyrgyzstan in 2016 was 4.1% of the total number of deaths.3 Data on COPD prevalence in Kyrgyzstan are scarce.4 There are hardly any data for Central Asia. According to data of the National Statistical Committee of the Kyrgyz Republic, 593.804 cases of respiratory diseases were registered in 2018.5 Yet, even in high-income countries, registration data of diagnoses may greatly underestimate the total burden of COPD because it is often not diagnosed until it is more advanced.6 Indeed, in a recent prevalence study in a high-altitude region of Kyrgyzstan, a prevalence of 36.7% was found.7
It is well known that COPD entails high economic costs associated to the consumption of health-care resources, as well as a significant loss of health-related quality of life.8 However, the economic burden of COPD has not been assessed in Kyrgyzstan. The economic burden includes not only direct costs associated with the consumption of health resources, but also labor productivity losses of patients related to poor health from COPD.9 The healthcare system in Kyrgyzstan is mostly financed by the government but despite this, COPD patients are forced to pay for many medicines from their own pockets.10
It is important to better understand the economic burden of COPD and its cost drivers in Kyrgyzstan. This knowledge is essential to inform policy makers regarding strategic planning, management, and allocation of resources. Estimating the health care and broader costs associated with the various components of COPD helps decision makers target necessary interventions to those areas with the potential for greatest impact on overall disease-related costs. Also, more data on COPD in low-resource settings is required to fully understand the total global burden of COPD, beyond high-resource settings only.
The aim of this paper is to characterize the clinical characteristics, treatment patterns, and economic burden of COPD in Kyrgyzstan.
Methods
Study Design
We conducted an observational, cross-sectional study in the two main regions of Kyrgyzstan (North and South) from November 6, 2017 to April 30, 2018. The study is reported according to the STROBE checklist for cross-sectional studies (see Appendix Table 1).
Every patient was acquainted with the study design and purposes, and included in the study after providing written, informed consent. The ethics committee of the National Center of Cardiology and Internal Medicine approved the study on March 1, 2016 (PROTOCOL №5). This study was part of the FRESH AIR (Free Respiratory Evaluation and Smoke-exposure reduction by primary Health cAre Integrated gRoups) implementation research project conducted from October 2015 to September 2018. This Horizon 2020 project addressed the prevention, diagnosis and treatment of chronic lung diseases in low-resource settings. The studies were conducted in four countries that were part of the International Primary Care Respiratory Group’s (IPCRG) global network: Uganda, the Kyrgyz Republic, Vietnam and Greece. We first studied the diverse local contexts, and then implemented context-driven lung health interventions, ranging from smoking cessation to pulmonary rehabilitation.11
Setting
In Kyrgyzstan, the vast majority of spirometry confirmed diagnosed COPD patients are registered in one of the five major hospitals. Three hospitals are in the North and two are in the South (see Appendix Figure 1 and Table 2). Opportunistically, patients were recruited from these five hospitals.
Participants
Eligibility criteria were patients aged ≥18 years, with a spirometry confirmed diagnosis of COPD (FEV1/FVC <0.7) according to pulmonologist records, who consented to participate. Patients who had a disability in communication (ie, those with cognitive impairment, those who cannot speak) were excluded.
Data Collection Procedure
Patients were invited to the clinics where they filled out a questionnaire (see Appendix Table 3 and 4). If they could not come to the hospital, we interviewed them by telephone using the same questionnaire. Clinical data was provided by the pulmonologist from existing medical history files in each clinic and the patient provided the remaining data through an interview performed by our team.
Data Sources/Measurement
We randomly chose every third COPD patient with a spirometry confirmed diagnosis of COPD (FEV1/FVC <0.7) (GOLD, 2011) among those included in existing patient registries of the hospitals until the calculated center sample size (306) was reached (see Appendix Table 5). Additionally, we used the EasyOneTM (Switzerland) spirometry device for patients who had spirometry of insufficient quality in their medical records.
Study Size
The total population of Kyrgyzstan is 5776 million of which 3985 million adults (≥15 years old) (Source: Republic Medical Information Center, Ministry of Health).12 Assuming a prevalence of diagnosed COPD of 0.9%, and assuming a 60% relative standard error (due to under-registration), we needed 306 patients to be representative (95% confidence level) for the country.
Outcomes
Data collected with the questionnaire included demographic characteristics (age, sex, highest education), smoking status (current/ex/non-smoker), occupational status (working, retired), occupational risk factors, health-care utilization (diagnostics, GP visits, specialist visits, hospitalization and medication, related with COPD), environmental risk factors (biomass use) and quality-of-life as measured using the Clinical COPD Questionnaire (CCQ)13 and the Medical Research Council (MRC) dyspnea scale translated in Russian (official language of Kyrgyzstan). Clinical data, obtained from patients’ medical history, or if missing, directly measured in the hospital included: body mass index (BMI), spirometry (FEV1% predicted), GOLD status based on airflow limitation (I–IV) and symptoms (ABCD) and selected comorbidities.
Healthcare Costs
The costs of all health-care utilization were calculated. In Kyrgyzstan, health-care costs are paid by the Compulsory Health Insurance Fund (CHIF). Costs paid by the CHIF and patients’ co-payments were identified separately. Comorbidity costs were not included. Hospitalization costs were calculated using the CHIF tariff at 1166 SOM (SOM: Kyrgyz national currency) ($13.8) per day, inclusive of a patient co-payment if:
- <70 years old, no disability, no insurance: 2980 SOM ($35.3)
- <70 years old, no disability, with insurance: 1160 SOM ($13.7)
- <70 years old retired, no disability, with insurance: 330 SOM ($4)
- >70 years old: free
- <4 days: 50% of this price.
Informal co-payments were taken into account when interviewing patients, yet we acknowledge that these might be underestimated because of embarrassment or fear of being accused of bribery, or patients simply did not want to offend the health-care workers. GP visits costed 60 SOM ($0.71), pulmonologist visits – 125 SOM ($1.48). Costs for diagnostics are provided in Appendix Table 6. In Kyrgyzstan, reimbursement of COPD drugs can be full or partial, at 50%. Salbutamol, ipratropium bromide and inhaled corticosteroids (ICS) are 50% reimbursed. Costs for comorbidity treatment were not included.
Statistical Methods
Demographic and clinical population characteristics were analyzed using descriptive statistics (mean, standard deviations, percentages). To investigate the relationship between clinical predictors and two important outcomes (ie, high symptom burden and high cost), we first performed a univariate logistic regression analysis, followed by multivariate logistic regression analysis. In the univariate analyses, we used a p value lower than 0.25 as a marker for potential significance in the multivariate analysis.14 In the multivariate analyses, we considered a p value lower than 0.05 as statistically significant. All analyses were performed using SPSS version 26; IBM, Armonk, NY, USA.
Results
Clinical and Demographic Characteristics
Of the 308 invited participants from the registries, we included a total of 306 participants. Two patients did report not having COPD. Mean age was 62.1 (SD=11.2), mean BMI was 26.9 (SD=5.2), and the majority was male (61.4%) (Table 1). As for risk factors, biomass (coal, wood, dung) was used by 71.2% for heating and by 52.0% for cooking. Current smokers accounted for 14.1%, ex-smokers for 32%, and the largest number were non-smokers 53.9%. Mean FEV1 was 46% (SD=12.8), the majority had COPD GOLD II or III, with 27.8% and 59.5%, respectively (Table 2, Figure 1). The highest distribution of patients according to the GOLD ABСD classification was D (70.2%), followed by B (22.2%), A (6.3%) and C (1.3%). In addition, the number of patients with an exacerbation of COPD was 95.8% (Table 2). Among the participants, 20.3% answered that they had co-morbidities, and most frequent co-morbidities were hypertension (25.2%), diabetes (5.6%) and heart diseases (4.6%), with some having multiple comorbidities (Figure 2). Regarding quality of life (Table 2), mean CCQ score was 2.0 (0.9) and mean MRC 3.7 (SD=0.9). Most participants (88.6%) had an MRC score ≥2 and almost 20% a score ≥4. As for the working status, most patients were retired (58.8%), 11.1% had no job and 30.1% worked.
 |
Table 1 Demographics of the Kyrgyz COPD Study Population (n=306) |
 |
Table 2 Clinical and Functional Characteristics of COPD Patients in Kyrgyzstan |
 |
Figure 1 FEV1% predicted in Kyrgyz COPD patients. |
 |
Figure 2 Comorbidities (%) in COPD patients in Kyrgyzstan, only co-morbidities that occurred in 10 or more patients shown. |
Pharmacotherapy
The most frequent type of therapy was monotherapy in all (A=68.4%, B=76.1%, C=75%, D=90.7%) GOLD groups. Free combinations and fixed-dose combinations of inhaled corticosteroids and long-acting b2-agonists (ICS/LABA) were equally most frequently prescribed in GOLD A (10.5%) and GOLD B (4.5%), and almost identically in GOLD D (15.3% vs 14.8%) (Figure 3).
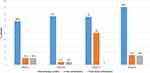 |
Figure 3 Pharmacotherapy of COPD patients by GOLD classification. |
Health Care Utilization and Costs
The yearly mean number of GP visits, pulmonologist visits and hospitalization days in the pulmonary department due to COPD were 2.9 (SD=3.6), 1.2 (SD=1.02) and 10.1 (SD=3.9), respectively (Table 3). Mean total annual per-patient costs of government reimbursed health-care utilization ($107) and patient co-payments ($224) were $331.5 (median: $103.5). Mean annual patient income was $1021.7 (SD=905.5). Notably, 71.5% of the interviewed patients had to pay their medications themselves and 64.4% paid for their diagnostics. Copayments comprised around one-fifth of Kyrgyz COPD patients’ annual income.
 |
Table 3 Healthcare Resource Use, Direct, and Indirect Costs per Kyrgyz COPD Patient per Year (n=306) |
Associations with High Symptom Burden and High Costs
Using univariable and multivariable logistic regression analyses, we explored associations of clinical variables with either high symptom burden (expressed by MRC score) (Table 4) or high costs (Table 5).
 |
Table 4 Univariate and Multivariate Associations with High MRC |
 |
Table 5 Univariate and Multivariate Associations with High Cost |
Regarding associations with the MRC score, we assessed two groups: “high MRC” (defined as MRC≥4, N=60, ie, the highest quintile) and “low MRC” (defined as MRC <4, N=246, ie, the lowest four quintiles). In the multivariate analyses, only GOLD IV (OR 3.625, 95% CI 1.417–9.271), and hypertension (OR 0.385, 95% CI 0.171–0.867) were significantly associated with high MRC. Age, BMI, unemployment, being retired, GOLD III and being exposed to occupational risks or biomass were non-significantly associated with higher symptom burden.
Regarding associations with costs, we first divided the patients into two groups based on total direct medical cost: “high cost” (N=154) and “low cost” (N=152), where the delimiter was the median cost of the total population ($103.5). In the multivariate analyses, suffering from exacerbations (OR 13.407, 95% CI 1.691–106.306) and hypertension (OR 1.736, 95% CI 1.002–3.007) were significantly associated with higher costs. Being retired (OR 1.171, 95% CI 0.636–2.154) and female sex (OR 1.357, 95% CI 0.831–2.21) were associated with higher medical costs, but these associations were not significant.
Discussion
Key results
We have evaluated the demographic and clinical characteristics and socio-economic burden of COPD patients in Kyrgyzstan. The findings demonstrated that the majority (ie, 71.9%) of the COPD patients had severe or very severe COPD. The majority were male, non-smokers and ex-smokers outnumbered the current smokers, and over two-thirds were exposed to biomass exposure due to heating and/or cooking. Almost all patients suffered from exacerbations. Almost all Kyrgyz COPD patients (99%) had an MRC score ≥2, and one in five an MRC of ≥4. Cardiovascular disease including hypertension was the most frequent comorbidity. Annual per-patient costs of reimbursed health-care utilization ($107) and co-payments ($224, ie, 22% of patients’ annual income) were $331. Concerning the economic burden, over 50% of the total direct medical costs were spent on medication, hospitalization and diagnostics. Notably, 64.4% of the patients had to pay for diagnostics and 71.5% had to pay for medication. Additionally, we have found that a low FEV1 (GOLD IV) and hypertension were significantly associated with high MRC scores. Exacerbations and hypertension were also significantly associated with high costs.
Interpretation
The results showed a high percentage of severe and very severe COPD patients, both in terms of quality of life (high CCQ and MRC scores) and spirometry (ie, high percentage of GOLD III–IV). The latter is higher than in Kyrgyz neighboring country Russia, where the proportions of GOLD III and IV were 41% and 12%, respectively.15 In a recent study in Uzbekistan, the percentages of COPD GOLD III and IV were 13.3% and 4.6%, respectively.16 The high number of severe COPD in Kyrgyzstan can be due to the fact that the number of spirometers is limited and there is low awareness and limited training of medical workers about COPD. In turn, this may result in underdiagnoses, and many patients only go to the doctor when they are already having severe COPD. Other potential reasons for the high burden of COPD include the high number of risk factors (smoking, biomass exposure) and non-adherence to treatment due to frequent co-payments, inappropriate therapy and beliefs that inhalation therapy can induce an addictiveness. This requires further in-depth studies. Of note, men were more likely to have COPD than women. Possibly, this may be because smoking rates are also higher in men.17,18 In Kyrgyzstan, this is related to the local culture, where a woman is not encouraged to smoke.19 For both men and women, the use of biomass (wood, coal and animal dung) is still high in rural areas.20 Biomass fuel is affordable, widely available, and awareness about chronic respiratory diseases and the risks of biomass fuel smoke is low.21 Exacerbations were associated with high cost. Also, previous studies have reported that the more exacerbations, the higher the annual cost per COPD patient.22,23 Cardiovascular comorbidities are often seen in COPD patients and the observed prevalence seems similar to other studies.23,24 The high burden of hypertension is possibly related to the lifestyle of the population, as they mainly eat salty, fatty, fried foods, and large portions of meat. It can also be associated with the highlands, given in Kyrgyzstan there are many settlements in areas with altitudes of over 1200 meters above sea level. Shen et al found a high prevalence of hypertension and prehypertension in the working population at high altitude in China.36 The association of hypertension with high cost may be related with its high incidence as a comorbid disease with COPD. Since the treatment of hypertension requires several medications, therefore, the costs are high, especially in combination with the treatment of COPD. Indeed, also a Spanish study demonstrated high health-care costs, mainly related to pharmacological treatment of arterial hypertension.24
In economic terms, the money spent on hospital admissions and GP visits was 32.9% and 6.6%, respectively, while in Russia, these numbers were 83.9% and 11.1%.25 The total average cost of COPD in Kyrgyzstan ($331) is almost a tenth of the mean cost per patient in high-income countries such as Italy (€2.647 per patient).26 However, in Uzbekistan, on average, a patient treated for an illness associated with tobacco use paid $137 per year for inpatient and outpatient services. Government spending on hospitalization and outpatient visits for CLD associated with tobacco smoking in Uzbekistan amounted to $1,347,686 and $7848 in 2005.27 The average cost of treatment per COPD patient in the Krasnoyarsk Kray (Russia) was 4222 rubles in 2014 ($87), which is more in line with our Kyrgyz findings.28 Differences in costs could be explained by differences in health-care systems, the ratio of the dollar to the som and medication prices.
Importantly, co-payment made up over half of the total COPD costs. Up to 71.5% of COPD patients from our study had to pay a fairly large amount of money due to the absent, non-working or outdated devices in public medical centers. Therefore, they have to turn to private diagnostic centers, which have to be paid for by patients themselves, regardless of whether they have insurance. It can be due to the lack of many diagnostic tests in primary health-care centers (PHC), and patients had to go to private diagnostic centers for a certain fee. Lastly, it should be noted that beyond direct medical costs and co-payments, also indirect costs are important. These include work productivity losses of which we previously showed that these played an important role in Kyrgyzstan.9
Strengths and Limitations
It is important to note that this is the first study conducted in Kyrgyzstan, focusing on the clinical characteristics and health-care costs of COPD. It was a national study integrated into the international FRESH AIR project. The study sample of patients with diagnosed COPD was nationally representative with patients recruited from five of the largest hospitals located in diverse regions in Kyrgyzstan. The sample size was calculated to achieve a minimum sample to answer our research question without overburdening the patients and pulmonologists. A larger sample could have however more power and would allow more subgroup analyses. Another limitation can be attributed to the fact that the study was carried out in already diagnosed patients with COPD, which could lead to an underestimation of the real total burden. On the other hand, patients were recruited from hospitals only (given spirometry was only available there), probably resulting in a more symptomatic population. Thus, the national Kyrgyz burden of COPD is likely to be even higher. Therefore, it is necessary to study the prevalence of the disease in the entire population. In future studies, better characterization of COPD, including functional tests, hyperinflation, and assessment of blood eosinophils should be considered if resources allow.
Recommendations
Kyrgyzstan faces a widescale underdiagnosis of COPD which may be attributed to poor awareness about COPD and its risk factors among communities and health-care workers, and lack of spirometers and skills to interpret spirometry in health centers. Given Kyrgyzstan is a resource-limited country, investing in better awareness and diagnoses, supported by country and context relevant guidelines29 can be cost-effective because of the considerable burden of COPD. This would also require more in-depth assessment of current access to pharmacological and non-pharmacological treatment.
During the FRESH AIR project, a lot of work has been done: we developed community awareness raising programmes on the respiratory health risks of indoor air pollution, engaged local and international stakeholders, implemented cleaner cookstoves and smoking cessation programs – ie, Very Brief Advice (VBA) by training family physicians throughout the country.30,32 After the implementation of new clean cookstoves, the number of respiratory symptoms in adults and children decreased, as well as the level of PM2.5. Also, we have implemented digital spirometry trainings to improve skills of health-care professionals, pulmonary rehabilitation (PR) on COPD, asthma and post-TB patients, that improve lung health and reduce the frequency of exacerbations. The results from the pilot study were positive, and PR is now recommended in the management of COPD and asthma patients, taking into account the patient’s condition. Here, we stress the need for appropriate and systematic implementation and scale-up of these interventions.21,31,35,37 All these implementations are likely to positively impact on the economic burden from CRDs.
Most importantly, policymakers should focus on promoting early detection of COPD and actively incorporate awareness programs to educate people on the risks of smoking and biomass exposure, and on affordable solutions (eg, clean stoves). In addition, expanded self-monitoring need to be introduced, and health-care providers need to educate patients on disease control.
Conclusion
Our findings demonstrated the clinical and economic burden of COPD on patients and the government in Kyrgyzstan. Notably, many COPD patients seem to be diagnosed in more advanced stages of the disease. As such, increasing the number of spirometry centers, improving of screening and the awareness of health-care workers on COPD, as well as education of the Kyrgyz population on the prevention of the disease, are necessary.
Funding
This study was funded by the EU Research and Innovation program Horizon 2020 (Health, Medical research and the challenge of ageing) under grant agreement no. 680997.
Disclosure
Dr Aizhamal Tabyshova and Dr Job FM van Boven report grants from European Commission H2020, during the conduct of the study. Dr Evelyn A Brakema report grants from Horizon 2020, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. World Health Organization. Chronic obstructive pulmonary disease. WHO Fact Sheets; 2017.
2. Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380(9859):2095–2128. doi:10.1016/S0140-6736(12)61728-0
3. Institute for Health Metrics and Evaluation. GBD compare data visualization. Kyrgyzstan; 2017.
4. Tabyshova A, Emilov B, Postma MJ, Chavannes NH, Sooronbaev T, van Boven JFM. Prevalence and economic burden of respiratory diseases in central Asia and Russia: a systematic review. Int J Environ Res Public Health. 2020;17(20):7483. doi:10.3390/ijerph17207483
5. National Statistical Committee of the Kyrgyz Republic. The number of diseases by major disease groups; 2018.
6. Pauwels RA, Rabe KF. Burden and clinical features of chronic obstructive pulmonary disease (COPD). Lancet. 2004;364.
7. Brakema EA, Tabyshova A, Kasteleyn MJ, et al. High COPD prevalence at high altitude: does household air pollution play a role? Eur Respir J. 2019;53(2):1801193. doi:10.1183/13993003.01193-2018
8. Miravitlles M, Murio C, Guerrero T, Gisbert R. Costs of chronic bronchitis and COPD: a 1-year follow-up study. Chest. 2003;123(3):784–791. doi:10.1378/chest.123.3.784
9. Brakema EA, Tabyshova A, van der Kleij RMJJ, et al. FRESH AIR collaborators. The socioeconomic burden of chronic lung disease in low-resource settings across the globe - an observational FRESH AIR study. Respir Res. 2019;20(21). doi:10.1186/s12931-019-1255-z
10. Ibraimova A, Akkazieva B, Ibraimob A, Manzhieva E, Rachel B. Kyrgyzstan. Health system overview. Health Syst Time Change. 2011;13(3):17.
11. Cragg L, Williams S, Chavannes NH, et al. FRESH AIR: an implementation research project funded through Horizon 2020 exploring the prevention, diagnosis and treatment of chronic respiratory diseases in low-resource settings. NPJ Primary Care Respir Med. 2016;26:1–5.
12. National Statistical Committee of the Kyrgyz Republic. Population of the Kyrgyz Republic; 2016.
13. van der Molen T, Willemse BW, Schokker S, Ten Hacken NH, Postma DS, Juniper EF. Development, validity and responsiveness of the clinical COPD questionnaire. Health Qual Life Outcomes. 2003;1:1–0.
14. Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3(17). doi:10.1186/1751-0473-3-17
15. Arkhipov V, Arkhipova D, Miravitlles M, Lazarev A, Stukalina E. Characteristics of COPD patients according to GOLD classification and clinical phenotypes in the Russian Federation: the SUPPORT trial. Int J Chron Obstruct Pulmon Dis. 2017;12:3255.
16. Tashmetova GT, Liverko IV. Chronic obstructive pulmonary disease in organized groups. Tuberculosis Lung Dis. 2020;98(6):36–39. doi:10.21292/2075-1230-2020-98-6-36-39
17. American Cancer Society, Inc. and Vital Strategies. The tobacco atlas. Tobacco Atlas; 2015.
18. Roberts B, Gilmore A, Stickley A, et al. Changes in smoking prevalence in 8 countries of the former Soviet Union between 2001 and 2010. Am J Public Health. 2012;102(7):1320–1328. doi:10.2105/AJPH.2011.300547
19. Quirmbach D, Gerry CJ. Gender, education and Russia’s tobacco epidemic: a life-course approach. Soc Sci Med. 2016;160:54–66.
20. Gordon SB, Bruce NG, Grigg J, et al. Respiratory risks from household air pollution in low and middle income countries. Lancet Respir Med. 2014;2(10):823–860.
21. Brakema EA, van Gemert FA, Williams S, et al; FRESH AIR collaborators. Implementing a context-driven awareness programme addressing household air pollution and tobacco: a FRESH AIR study. NPJ Prim Care Respir Med. 2020;30(1):1–8.
22. Dalal AA, Patel J, D’Souza A, Farrelly E, Nagar S, Shah M. Impact of COPD exacerbation frequency on costs for a managed care population. J Manag Care Spec Pharm. 2015;21(7):575–583.
23. Mannino DM, Thorn D, Swensen A, Holguin F. Prevalence and outcomes of diabetes, hypertension and cardiovascular disease in COPD. Eur Respir J. 2008;32(4):962–969. doi:10.1183/09031936.00012408
24. Sicras-Mainar ANR. Cost of arterial hypertension according to levels of morbidity in primary care setting. Med Clin (Barc). 2009;133(8):290–295. doi:10.1016/j.medcli.2009.05.017
25. Kontsevaya AV, Mukaneyeva DK, Balanova YA, Khudyakov MB, Drapkina OM. Economic burden of respiratory diseases and chronic obstructive pulmonary disease in Russian Federation, 2016. Pulmonologiya. 2019;29(2):159–166. doi:10.18093/0869-0189-2019-29-2-159-166
26. Corsico AG, Braido F, Contoli M, et al. Healthcare costs of the SATisfaction and adherence to COPD treatment (SAT) study follow-up. Respir Med. 2019;153:68–75.
27. Ministry of Health of the Republic of Uzbekistan and World Bank. Health effects of smoking population and economy of Uzbekistan; 2005.
28. Gaygol’nik TV, Demko IV, Bochanova EN, Bikulova TV, Kraposhina AY. Drug supplying management for patients with chronic obstructive pulmonary disease at Krasnoyarsk kray. Pulmonologiya. 2016;26(2):208–214.
29. Tabyshova A, Hurst JR, Soriano JB, et al. Gaps in COPD guidelines of low- and middle-income countries: a systematic scoping review. Chest. 2021;159(2):575–584. doi:10.1016/j.chest.2020.09.260
30. van Gemert F, de Jong C, Kirenga B, et al. Effects and acceptability of implementing improved cookstoves and heaters to reduce household air pollution: a FRESH AIR study. NPJ Prim Care Respir Med. 2019;29(1). doi:10.1038/s41533-019-0144-8
31. Anastasaki M, Trigoni M, Pantouvaki A, et al. Establishing a pulmonary rehabilitation programme in primary care in Greece: a FRESH AIR implementation study. Chron Respir Dis. 2019;16:156.
32. Papadakis S, Anastasaki M, Papadakaki M. ‘Very brief advice’ (VBA) on smoking in family practice: a qualitative evaluation of the tobacco user’s perspective. BMC Fam Pract. 2020;21(1). doi:10.1186/s12875-020-01195-w
33. Punekar YS, Shukla A, Müllerova H. COPD management costs according to the frequency of COPD exacerbations in UK primary care. Int J Chron Obstruct Pulmon Dis. 2014;9:65–73. doi:10.2147/COPD.S54417
34. Chen W, Thomas J, Sadatsafavi M, FitzGerald JM. Risk of cardiovascular comorbidity in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Lancet Respir Med. 2015;3(8):631–639. doi:10.1016/S2213-2600(15)00241-6
35. Philip KE, Akylbekov A, Stambaeva B, Sooronbaev T, Jones R. Music, dance, and harmonicas for people with COPD. Respir Care. 2019;64(3):359. doi:10.4187/respcare.06701
36. Shen Y, Chang C, Zhang J, Jiang Y, Ni B, Wang Y. Prevalence and risk factors associated with hypertension and prehypertension in a working population at high altitude in China: a cross-sectional study. Environ Health Prev Med. 2017;22(1):19. doi:10.1186/s12199-017-0634-7
37. Kjærgaard J, Nissen TN, Isaeva E, et al.; FRESH AIR collaborators. No time for change? Impact of contextual factors on the effect of training primary care healthcare workers in Kyrgyzstan and Vietnam on how to manage asthma in children - A FRESH AIR implementation study. BMC Health Serv Res. 2020;20(1). doi:10.1186/s12913-020-05984-y
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
