Back to Journals » Cancer Management and Research » Volume 11
Clinical characteristics of testicular seminoma in individuals in West China: a 10-year follow-up study
Authors Chen Z, Qiu S, Cao D, Guo J, Chen B, Huang Y, Lai L, Bao Y, Dong Q , Liu L, Wei Q
Received 13 May 2019
Accepted for publication 22 July 2019
Published 14 August 2019 Volume 2019:11 Pages 7639—7645
DOI https://doi.org/10.2147/CMAR.S215537
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Antonella D'Anneo
Zeyu Chen,1,2,* Shi Qiu,1,3,* Dehong Cao,1,* Jianbing Guo,1,2 Bo Chen,1,2 Yin Huang,1,2 Li Lai,1 Yige Bao,1 Qiang Dong,1 Liangren Liu,1 Qiang Wei1
1Department of Urology/Institute of Urology, West China Hospital, Sichuan University, Chengdu 610041, People’s Republic of China; 2West China School of Medicine, Sichuan University, Chengdu, People’s Republic of China; 3Center of Biomedical Big Data, West China Hospital, Sichuan University, Chengdu, Sichuan, People’s Republic of China
*These authors contributed equally to this work
Objective: To assess the clinical characteristics of testicular seminoma (TS).
Patients and methods: A testicular cancer (TC) survey was conducted by the Department of Urology, West China Hospital, between 2008 and 2018. Tumors were classified according to the NCCN criteria such as age, tumor size, tumor marker levels, histopathology, clinical stage, initial treatment, follow-up, and clinical outcomes, were obtained from the database of our center.
Results: Among 155 registered cases of TC with seminomatous element, 127 cases of pure TS were analyzed. All 127 patients with a median age of 37 years were pathologically diagnosed with orchiectomy specimens. Orchiectomy, chemotherapy, and radiotherapy were the main treatments for these patients. Patients with clinical stages I, II, and III testicular cancer of accounted for 81.1% (n=103), 15.7% (n=20), and 3.2% (n=4) of all patients, respectively. After a median follow-up time of 50 months, five patients presented with relapse during follow-up, and one among them died. Of the patients with stage I TS (T1N0M0S0 CS IA), three patients who only underwent orchiectomy relapsed. Among patients with stage II TS (T1N1M0S1 CS IIA), one patient relapsed after orchiectomy, post-surgery chemotherapy and radiotherapy. In four patients with stage III disease (T2N1M1aS1 CS IIIA), one relapsed after orchiectomy and chemotherapy, and died shortly after salvage chemotherapy and radiotherapy due to recurrence. The median overall survival time was 50 months. In all patients, the 2-year overall survival and progression-free survival probabilitis were 98.6% and 98.8%, respectively.
Conclusion: The present study shows that patients with TS have good prognosis even at an advanced stage. Surveillance after orchiectomy was important for patients with CSI seminoma, and we recommend cisplatin-based chemotherapy as salvage therapy for patients with CSI seminoma. In addition, patients with a maximal tumor diameter >4 cm should undergo post-surgery chemotherapy.
Keywords: testicular cancer, testicular seminoma, orchiectomy, post-orchiectomy therapy
Introduction
Testicular tumor is a rare disease of the urogenital system, accounting for 1% of all male neoplasms and 5% of all urological tumors. The incidence of testicular cancer (TC) is approximately one case per 100,000 person-years in China, which is lower than that seen in western countries. A slight increase in the incidence of this cancer has been observed over the past decades.1 Histologically, pure seminomas account for approximately 60% of TCs. Treatments for testicular seminoma (TS) have been continuously improving over the years due to a series of advancements in therapeutic regimens.2 Most patients with seminoma can be treated with orchiectomy and, if necessary, subsequent chemotherapy or radiotherapy can be provided.3,4 Although accurate diagnosis and advanced multimodal treatment significantly contribute to good prognosis, some controversies regarding the different side effects of post-orchiectomy therapeutic regimens for the treatment of TS still exists.2–6
This study aims to assess the clinical characteristics, treatment, and outcome of TS. We have conducted a study of TS adapted by our hospital between 2008 and 2018. Several testicular tumors comprised mixed elements. Therefore, we analyzed the clinical characteristics of pure TS.
Methods
Patients diagnosed with TS according to NCCN criteria were included in this study. Patients with seminomas with non-seminoma germ cell tumor elements were excluded. The collection and processing of all data were conducted per the Declaration of Helsinki. After obtaining written informed consent, each patient was evaluated. Furthermore, as the study include no intervention upon patients, ethical approval was not needed after consulting the the Committee of the West China Hospital, Sichuan University. All available data, including age; primary symptoms; laterality; tumor size, imaging examination results (ultrasonography, radiography, and computer tomography), tumor marker levels [serum lactate dehydrogenase (LDH), serum β-human chorionic gonadotropin (HCG), and serum alpha fetoprotein (AFP)]; tumor staging (TNM, S stage, and clinical); initial treatment; time of relapse; and outcome, were obtained from the database. The following values were used according to the criteria of our institution: normal serum LDH level, <220 IU/L; β-HCG level, <3.81 mIU/mL; and AFP level, <8 ng/mL.
Overall survival (OS) was measured from the time of diagnosis to the time of the latest follow-up or death. Progression-free survival (PFS) was measured from the time of diagnosis to the time of disease progression, disease relapse, latest follow-up, or death (Figure 1).
 |
Figure 1 Patients enrolled in every step. |
The Kaplan–Meier method was used to estimate PFS and OS. The Cox proportional hazards model was used to compare the survival times in terms of varying parameters between the patient groups.
Results
Baseline characteristics
The participants were 21–77 years old, with a mean age of 38 years. The primary symptoms were scrotal masses in 108 (85.0%), pain of testis in 20, and respiratory symptoms for lung metastasis in one patient. All patients were diagnosed based on pathological classification. A total of 125 (98.4%) lesions were unilaterally located in the body, one (0.8%) bilaterally, and one (0.8%) in the abdomen. Among patients with unilateral lesions, 58 (46.4%) presented with a mass on the left testis, whereas 67 (52.8%) had a mass on the right testis (Table 1).
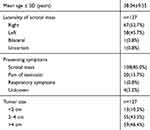 |
Table 1 Baseline characters of testicular seminoma |
As shown in Table 2, according to the NCCN staging system,4 the patients were categorized as follows: 49 (38.6%) with clinical stage IA, 15 (11.8%) with IB, 39 (30.6%) with IS, 14 (11.0%) with IIA, four (3.2%) with IIB, two (1.6%) with IIC, 3 (2.4%) with IIIA, and one (0.7%) with IIIB. The most common metastatic lesion site was the lung (n=2), and one patient presented with metastasis in the neck and mediastinum (pT2N2M1bS1 CS IIIb) (Table 2).
 |
Table 2 Tumor classification |
Tumor marker levels
The tumor marker levels were measured in all patients before the initial treatments (Table 3). AFP levels were elevated in 10 (8.5%) patients, and 1 (0.9%) had an extremely elevated AFP level (>1210 ng/mL). β-HCG levels were elevated in 66 patients and was extremely high in one patient (>1360 mIU/mL). LDH levels were elevated in 50 (44.2%) patients, and six (5.3%) patients had a 5-fold increase in LDH levels. According to the abovementioned information, we assessed the S classification of these patients. The following results were obtained: 55 (44.3%) were S0, 15 (11.8%) were Sx, 52 (41.0%) were S1; and five (3.9%) were S2 (Table 2).
 |
Table 3 Tumor markers |
Treatments
As a first-line treatment for seminoma, orchiectomy was performed in all patients. Among them, two (1.5%) underwent retroperitoneal lymph node dissection. A total of 40 (31.5%) patients received chemotherapy after orchiectomy. Eighteen (14.2%) received varied doses and cycles of radiotherapy, and four (3.1%) underwent chemotherapy and radiotherapy as post-surgical treatments. As after-orchiectomy therapy for seminoma, 30 patients with CSI, 9 with CSII, and one with CSIII received chemotherapy. In addition, 16 patients with CSI and two with CSII received radiotherapy as post-orchiectomy therapy. Two patients with CSIA, one with CSIS, and one with CSIIIA received both chemotherapy and radiotherapy as post-orchiectomy treatments. One patient with CSIIA received chemotherapy as a first-line post-surgery therapy and radiotherapy as salvage therapy after relapse (Table 4).
 |
Table 4 Post-orchiectomy treatment |
Survival data
During the median observation period of 50 (range: 4–118) months, five (3.9%) patients confirmed relapse after orchiectomy, whereas one (T2N1M1aS1 CSIIIA) died during follow-up. The 2-year OS and PFS probabilitis were 98.6% and 98.8%, respectively. According to the NCCN criteria,4 the 1- and 3-year OS probabilitis of patients with seminoma were 99.8% and 99.5%, respectively. According to our statistics, the 4-year PFS probabilitis of patients with CSIA and IIA were 91.9% and 83.3%, respectively. Further, the 4- and 8-year PFS probabilitis in all patients with CSI were 96.4% and 90%, respectively. The 4- and 8-year PFS probabilitis in all patients with seminoma were 93.6% and 85.3%, respectively (Figure 2).
 |
Figure 2 (A) and (B) 4-year and 8-year PFS probabilities of all patients. |
Discussion
This large-scale study for the first time shows the characteristics and outcome of patients with TC in China based on data from uni-institutional registry. A good prognosis was observed even in patients with advanced-stage disease. The most common symptom of seminoma, ie, a testicular mass, was found using multiple methods. All tumor samples were collected via surgery and were pathologically identified.
The first-line therapy for CSI seminoma is still orchiectomy. According to the EAU and NCCN guidelines,3,4 the actuarial relapse rate is approximately 15–20% after 5 years. Based on a surveillance performed by experienced centers, the overall cancer-specific survival probability for CSI seminoma is approximately 97–100%. Because carboplatin-based chemotherapy was introduced in the 1970s,3,4 the effect of chemotherapy had significantly improved. Two cycles of carboplatin-based chemotherapy may further reduce the relapse risk to approximately 1–3%. We found that 3 (4%) of 75 patients with CSIA who experienced relapsed had only undergone orchiectomy. However, none of the patients who had received after-surgery therapy experienced recurrence during follow-up, which shows that post-orchiectomy therapy can reduce the risk of recurrence in patients with CSI, which has been reported by other researchers also. However, recent studies have shown that the utilization of post-orchiectomy therapy after orchiectomy did not show any significant benefits in the survival of patients with CSI.7 Furthermore, because salvage chemotherapy and radiotherapy are quite effective in patients with relapse and result in a relatively good prognosis, surveillance is a better option for patients with CSI seminoma. The tumor size of these patients is large (maximal diameter >4 cm). Trevino et al8 have shown that tumor size >4 cm was a significant predictor of a higher risk of relapse for CSI seminoma. Tyrell et al9 have identified a hazard ratio (HR) of 1.219 [95% confidence interval (CI), 0.58–2.55; p=0.598] for recurrence in tumors >4 cm in size compared with those that are ≤4 cm, which was according to the data from their center. Tandstad et al10 have reported a similar result showing that a tumor diameter of >4 cm (HR, 2.7; p<0.001) was a risk factor correlated to relapse. In addition, in a systematic review by Zengerling et al,11 tumor size was found to be significantly associated with relapse in CSI patients. Furthermore, as reported in a multi-institutional study by Dieckmann et al12 on patients with tumors >5 cm, carboplatin is the primary treatment modality. According to these studies, we conclude that patients with CSI who have a tumor with a maximal diameter >4 cm should receive salvage therapy after orchiectomy.
As shown in recent studies, radiotherapy was significantly associated with severe side effects; therefore, the use of RT has been criticized.13 As shown in the study by Maroto et al,14 the risk of a second solid non-germ-cell tumor is approximately doubled after radiotherapy or chemotherapy. Groot et al5 have also conducted a large-scale multi-institutional study in 2018 and evaluated 5,848 one-year survivors treated for TC before the age of 50 years between 1976 and 2007. After a median follow-up of 14.1 years, 350 solid secondary malignant neoplasms were observed, indicating a 1.8-fold (95% CI: 1.6–2.0) increased risk compared with the risk in the general population. Moreover, this risk was dose-related. According to our latest follow-up, none of the patients with relapsed CSI from our center died after salvage therapy. According to these data, we consider active surveillance as the first option for stage I seminoma, and chemotherapy could be the salvage treatment after relapse.
Of 24 patients with metastasis (CSII and CSIII), 11 (45.8%) were followed-up. Among them, nine (81.8%) received chemotherapy or radiotherapy, seven (63.6%) received cisplatin-based chemotherapy, one (9.1%) received salvage radiotherapy after relapse, one (9.1%) received radiotherapy as post-orchiectomy treatment, and one (9.1%) (T2N1M1aS1 CSIIIa) received both chemotherapy and radiotherapy as salvage therapies. These data show that post-orchiectomy therapy is recommended in patients with metastasis and that chemotherapy may be used more frequently. As demonstrated by the NCCN and EAU guidelines,3,4 for patients with advanced-stage disease, chemotherapy and radiotherapy could be the recommended treatment options. In patients with CSIIA and IIB, varied doses of cisplatin-based chemotherapy and radiotherapy to the para-aortic and ipsilateral iliac fields are highly recommended in both guidelines. However, a recent study conducted by Glaser et al showed that patients with CSIIA who received radiotherapy had improved survival than patients who received chemotherapy. In addition, for patients with CSIIB who received radiotherapy and chemotherapy, no significant difference was observed in terms of 5-year survival.15 For advanced metastatic seminoma (CSIIC and CSIII), both guidelines have recommended different regimens of cisplatin-based chemotherapy.3,4
According to the data from our institute, the 4- and 8-year PFS probabilitis were 96.4% and 90% in all patients with CSI (Figure 3), respectively. The 2-year OS probability was 98.6% in all patients, whereas the 4-year PFS probability in patients with CSIA and IIA were 91.9% and 83.3% (Figure 4), respectively. Overall, the 2-, 4-, and 8-year PFS probabilitis in all seminoma patients were 98.8%, 93.6%, and 85.3%, respectively, suggesting that the prognosis of TS was found to be relatively good. The Japanese Urological Association conducted a similar nationwide investigation on TC by registering patients newly diagnosed with TCs in 2005 and 2008. The 1- and 3-year OS probabilitis in their study were 98.3% and 96.8%, respectively, which showed a good prognosis even at an advanced stage.16
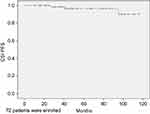 |
Figure 3 4-year and 8-year PFS probabilities in CSI patients. |
 |
Figure 4 (A) 4-year PFS probabilities in CSIA patients, (B) 4-year PFS probabilities in CSIIA patients. |
The present study has several limitations. First, not all clinical data were collected, including tumor marker levels, clinical stage, dose of chemotherapy, and radiotherapy. However, this could not be avoided due to its retrospective nature. Second, the study lasted for over a 10–year period; therefore, 44 patients were lost to follow-up due to missing contact information and other unavoidable reasons. However, we compared the baseline characters of followed and lost patients and found no significant difference (Table 5). So we consider the outcome of those lost patients is similar to our results.
 |
Table 5 Comparison of baseline characters of patients followed and lost |
Conclusion
According to our study, based on the good prognosis of patients with CSI seminoma, surveillance after orchiectomy is important for this group of patients. We recommend cisplatin-based chemotherapy as salvage therapy for patients with CSI. In addition, patients with a maximal tumor diameter >4 cm should receive post-surgery chemotherapy. In our center, most patients with metastasis received varied doses and cycles of cisplatin-based chemotherapy after orchiectomy, and a relatively good prognosis was observed.
Acknowledgment
The authors are grateful to Enago for editing the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ding Q, Wei Q, Yin C, et al. Chinese Association of Urology Guidelines on Testicular Cancer. People's Medical Publishing House; 2014.
2. Chahoud J, Zhang M, Shah A, Lin S-H, Pisters LL, Tu S-M. Managing seminomatous and nonseminomatous germ cell tumors. Curr Opin Oncol. 2018. doi:10.1097/cco.0000000000000446
3. Albers P, Albrecht W, Algaba F, et al. EAU guidelines on testicular cancer. EAU Guidelines. 2018(1).
4. Timothy G, Daniel WL, Rahul A, et al. NCCN clinical practice guidelines in oncology on testicular cancer. NCCN Guidelines. 2018;1.
5. Groot HJ, Lubberts S, de Wit R, et al. Risk of solid cancer after treatment of testicular germ cell cancer. J Clin Oncol. 2018;36:2504–2515. doi:10.1200/JCO10.1200/JCO.2017
6. Chovanec M, Hanna N, Cary KC, Einhorn L, Albany C. Management of stage I testicular germ cell tumours. Nat Rev Urol. 2016;13:663–673. doi:10.1038/nrurol.2016.164
7. Kamran SC, Seisen T, Markt SC, et al. Contemporary treatment patterns and outcomes for clinical stage IS testicular cancer. Eur Urol. 2017;73:262–270. doi:10.1016/j.eururo.2017.06.013
8. Trevino KE, Esmaeili-Shandiz A, Saeed O, Xu H, Ulbright TM, Idrees MT. Pathological risk factors for higher clinical stage in testicular seminomas. Histopathology. 2018;73:741–747. doi:10.1111/his.13667
9. Tyrrell HEJ, Church DN, Joseph J, et al. Changing practice evaluation-stage 1 seminoma: outcomes with adjuvant treatment versus surveillance: risk factors for recurrence and optimizing follow-up protocols-experience from a supraregional center. Clin Genitourin Cancer. 2018;16:240–244. doi:10.1016/j.clgc.2017.12.001
10. Tandstad T, Ståhl O, Dahl O, et al. Treatment of stage I seminoma, with one course of adjuvant carboplatin or surveillance, risk-adapted recommendations implementing patient autonomy: a report from the Swedish and Norwegian Testicular Cancer Group (SWENOTECA). Ann Oncol. 2016;27:1299–1304. doi:10.1093/annonc/mdw164
11. Zengerling F, Kunath F, Jensen K, Ruf C, Schmidt S, Spek A. Prognostic factors for tumor recurrence in patients with clinical stage I seminoma undergoing surveillance-A systematic review. Urol Oncol. 2018;36:448–458. doi:10.1016/j.urolonc.2017.06.047
12. Dieckmann KP, Dralle-Filiz I, Matthies C, et al. Testicular seminoma clinical stage 1: treatment outcome on a routine care level. J Cancer Res Clin Oncol. 2016;142:1599–1607. doi:10.1007/s00432-016-2162-z
13. Berghen C, Albersen M, Blanchard P, et al. Readressing the rationale of irradiation in stage I seminoma guidelines: a critical essay. BJU Int. 2019. doi:10.1111/bju.14686
14. Maroto P, Anguera G, Martin C. Long-term toxicity of the treatment for germ cell-cancer. A review. Crit Rev Oncol Hematol. 2018;121:62–67. doi:10.1016/j.critrevonc.2017.11.015
15. Glaser SM, Vargo JA, Balasubramani GK, Beriwal S. Stage II testicular seminoma: patterns of care and survival by treatment strategy. Clin Oncol. 2016;28:513–521. doi:10.1016/j.clon.2016.02.008
16. Miki T, Kamoi K, Fujimoto H, et al. Clinical characteristics and oncological outcomes of testicular cancer patients registered in 2005 and 2008: the first large-scale study from the Cancer Registration Committee of the Japanese Urological Association. Int J Urol. 2014;21:S1–S6. doi:10.1111/iju.12441
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
