Back to Journals » Neuropsychiatric Disease and Treatment » Volume 12
Clinical characteristics of synthetic cannabinoid-induced psychosis in relation to schizophrenia: a single-center cross-sectional analysis of concurrently hospitalized patients
Authors Altintas M, Inanc L, Akcay Oruc G, Arpacioglu S, Gulec H
Received 2 March 2016
Accepted for publication 20 June 2016
Published 2 August 2016 Volume 2016:12 Pages 1893—1900
DOI https://doi.org/10.2147/NDT.S107622
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Roger Pinder
Merih Altintas,1 Leman Inanc,2 Gamze Akcay Oruc,1 Selim Arpacioglu,1 Huseyin Gulec1
1Department of Psychiatry, Erenköy Mental and Neurological Diseases Training and Research Hospital, Istanbul, 2Department of Psychiatry, Dr Cevdet Aykan Mental Health and Diseases Hospital, Tokat, Turkey
Background: This study aimed to evaluate synthetic cannabinoid (SC)-induced psychosis in terms of patient profile and clinical characteristics with reference to concurrently hospitalized schizophrenic patients.
Methods: A total of 81 male patients diagnosed with psychotic disorder induced by the use of SCs (n=50; mean (standard deviation [SD]) age: 25.9 (5.5) years) or with schizophrenia (n=31, mean (SD) age: 42.9 (11.6) years) based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, diagnosis criteria who were concurrently hospitalized at Erenköy Mental and Neurological Diseases Training and Research Hospital were included in this cross-sectional study. Data on sociodemographic characteristics, Brief Psychiatric Rating Scale (BPRS), Positive and Negative Syndrome Scale (PANSS), Frontal Assessment Battery (FAB), Hamilton Rating Scale for Depression (HRSD), and Hamilton Anxiety Rating Scale (HAM-A) were recorded in all the patients.
Results: Mean (SD) age at disease onset in SC-induced psychosis patients was 22.3 (5.6) years; 26.0% had suicidal ideation and 58.4% were hospitalized involuntarily. Marijuana was the most common first used substance (72.0%), and solitary use of SC was noted in 38.0% of patients. SC-induced psychosis patients had similar PANSS positive, BPRS, HRSD, and FAB scores and significantly lower PANSS negative scores (18.0 [6.5] vs 22.3 [6.0], P=0.004) than patients with schizophrenia, while they had similar HAM-A scores (17.8 [10.3] vs 21.6 [5.5], P=0.085) as young schizophrenics. Age at onset for SC (r=0.364, P=0.05) or substance (r=0.395, P=0.01) use was correlated positively with total FAB scores.
Conclusion: In conclusion, our findings revealed SC-induced psychosis to influence young individuals and be associated with remarkable rates of suicidal ideation and involuntary hospitalization as well as similar clinical picture with schizophrenia in terms of PANSS positive, BPRS, HRSD, HAM-A, and FAB scores. Younger age at onset was associated with poorer frontal lobe functions overall, regardless of the type of substance, and with poorer inhibitory control and programming performance in case of SC use.
Keywords: synthetic cannabinoid, psychosis, schizophrenia, frontal lobe, cognition, psychotogenic, bonzai
Introduction
Consumption of synthetic cannabinoids (SCs), marketed under different names such as K2, Spice, Aroma, and Dream in different countries and named as Bonzai in Turkey, has been increasing worldwide.1–5 Albeit no data are available on the exact prevalence of SC use in Turkey, a rapidly growing increase in SC consumption among young population has been noted in Turkey consistent with the global increase in the prevalence of SC use among adolescents and young adults with a male predominance.5–9
Cannabidiol (CBD) and delta-9-tetrahydrocannabinol (THC) are the two principal ingredients of natural cannabis (marijuana) with counteracting functions.10 Whilst purchased and perceived as risk-free marijuana-like herbal blends,1 SCs are much more potent than natural cannabis, since they act as a more potent full agonist at the cannabinoid subtype 1 receptor than THC, and they also lack cannabinoids such as CBD that may otherwise counteract psychoactive properties of THC.1,5,11,12 Hence, SCs may induce a more severe clinical presentation than the natural plants they are supposed to mimic, including agitation, anxiety, tachycardia, hallucinations, irritability, memory and cognitive impairment, violent behavior, unresponsiveness, and psychosis.1,13,14
SCs are shown to trigger psychotic symptoms including paranoia, hallucinations, disorganized behavior, and suicidal thoughts among individuals with or without concomitant psychiatric disorders.5,7,10,13–20 SCs were also reported to be associated with a wide range of positive and negative symptoms and cognitive impairment that resemble the phenomenology of schizophrenia.21,22 However, being mainly based on case reports and laboratory studies, limited data are available on SC-induced psychosis.
The present study was therefore designed to evaluate SC-induced psychosis in terms of patient profile, clinical characteristics, and psychotogenic profile with reference to concurrently hospitalized schizophrenic patients.
Methods
Study population
A total of 81 male patients diagnosed with psychotic disorder induced by the use of SCs (n=50) or with schizophrenia according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, diagnosis criteria23 (n=31) who were concurrently hospitalized at Erenköy Mental and Neurological Diseases Training and Research Hospital, Istanbul, were included in this cross-sectional study. Age 16–60 years, being literate, use of SC for at least 4 months, and lack of previous diagnosis of any psychiatric disorder were the inclusion criteria for SC-induced psychosis group, while patients at the intoxication stage of SCs, decided based on successive analysis of laboratory and clinical findings, and patients with mental retardation or any other neurological disease and past history of head trauma were excluded. Aged 16–60 years and no personal or family history of substance use were the eligibility criteria for the patients with schizophrenia.
Written informed consent was obtained from each subject following a detailed explanation of the objectives and protocol of the study, which was conducted in accordance with the ethical principles stated in the Declaration of Helsinki and approved by the Ethics Committee of Erenköy Mental and Neurological Diseases Training and Research Hospital.
Assessments
Data on sociodemographic (age, marital status) and disease (family history, age at onset, duration of disease, hospitalizations) characteristics, urinalysis for SC metabolites, and psychometric assessments including Brief Psychiatric Rating Scale (BPRS), Positive and Negative Syndrome Scale (PANSS), Frontal Assessment Battery (FAB), Hamilton Rating Scale for Depression (HRSD), and Hamilton Anxiety Rating Scale (HAM-A) were recorded on the seventh day of hospitalization in all the patients. Detailed history of SC and substance use (type, usage pattern) was also recorded in the SC-induced psychosis group.
Urinalysis
Laboratory analysis to confirm SC use included SC screening of urine samples via enzyme immunoassay method (K2 Enzyme Immunoassay; Immunalysis, Pomona, CA, USA) with the use of a commercially available kit enabling the detection of JWH-018, JWH-073, and AM-2201 metabolites in the urine with a cutoff value of 20 ng/mL for positivity.
Brief Psychiatric Rating Scale
This scale was developed by Overall and Gorham24 to assess the severity and change of psychotic and some depressive symptoms in schizophrenia and other psychotic disorders. It consists of 18 items, each being rated for severity of symptom ranging from 1 (not present) to 7 (extremely severe). Factor analysis results signal different symptom clusters in this scale: the set of negative symptoms (emotional withdrawal, blunted affect, and motor retardation) and the set of positive symptoms (conceptual disorganization, hallucinations, and unusual though content). Scores obtained from the BPRS rating do not separate negative schizophrenia cases from positive schizophrenia cases; rather they are used to establish both negative and positive symptoms seen in a given case.24 Preliminary data for the reliability of Turkish translation of BPRS were reported in our country.25
Positive and Negative Syndrome Scale
It is a semi-structured interview form designed to assess positive and negative symptoms as well as general psychopathology and to measure the levels of these symptoms in case of schizophrenia or any other psychotic disorder.26 The scale consists of 30 items rated from 0 (absent) to 7 (extreme) that represent increasing levels of psychopathology. Seven items are related to positive syndrome subscale, seven items are related to negative syndrome subscale, and the remaining 16 items are related to general psychopathology subscale. The study of validity and reliability of this scale (in Turkish) was conducted by Kostakoglu et al.27
Frontal Assessment Battery
FAB is a short bedside cognitive and behavioral test to assess frontal lobe functions. It has six subscales, giving a total possible score of 0–18. The subscales are conceptualization, mental flexibility, programming, sensitivity to interference, inhibitory control, and environmental autonomy. Higher scores indicate better performance. This short battery was designed to assess executive functions at bedside.28,29
Hamilton Rating Scale for Depression
This scale aims to assess severity of, and change in, depressive symptoms for a given patient. It was first introduced by Hamilton and then was transformed into a structured form by Williams under the supervision of Hamilton.30 Validity and reliability of the Turkish questionnaire was conducted by Akdemir et al.31 This scale consists of 17 questions and it is not utilizable in making diagnosis, while enables assessment of existing level of, and change in, depressive symptoms with higher scores indicating more severe depression.
Hamilton Anxiety Rating Scale
This scale consists of 14 items designed to establish anxiety states and distribution of symptoms, and to measure change in severity.32 Each item is scored on a scale of 0 (not present) to 4 (severe), with a total score range of 0–56, where <17 indicates mild severity, 18–24 mild-to-moderate severity, and 25–30 moderate-to-severe. Validity and reliability study for this scale in Turkish was performed by Yazici et al.33
Statistical analysis
Statistical analysis was made using IBM SPSS Statistics (version 20.0; IBM Corporation, Armonk, NY, USA). Chi-square (χ2) test was used for the comparison of categorical data, while Student’s t-test was used for normally distributed metric data. Mann–Whitney U-test for metric data with non-normal distribution was used for the analysis of numerical data. Spearman correlation test was used for correlation analysis. Data were expressed as “mean (standard deviation [SD])”, minimum–maximum, and percent (%) where appropriate. P<0.05 was considered statistically significant.
Results
Sociodemographic and disease-related characteristics
Mean (SD) age of the SC-induced psychosis patients was 25.9 (5.5) years. Majority of patients were single and living with their family, while 36.0% had family history for substance abuse and a psychiatric disease, in the first-degree relatives in most of the cases (76.0%). Overall 26.0% of patients had suicidal ideation and 32.0% had prior suicide attempt. Overall, 58.4% of patients were hospitalized involuntarily, while the mean (SD) number of previous hospitalizations and length of hospital stay were 2.4 (2.3) times and 14.1 (6.2) days, respectively (Table 1).
Mean (SD) age of schizophrenia patients was 42.9 (11.6) years; most of them were single and living with their family; 29.0% had family history for a psychiatric disease, in first degree-relatives in most of the cases (77.8%), 3.2% had suicidal ideation, and 19.4% had prior suicide attempt. Mean (SD) age at disease onset was 27.1 (9.0) years, while the duration of disease was 178.0 (111.2) months. Overall, 51.6% of patients were hospitalized involuntarily, while the mean (SD) number of previous hospitalizations and length of hospital stay were 4.5(3.9) times and 28.6 (21.9) days, respectively (Table 1).
Data on SC and substance use
None of the urine samples were found positive for SC, consistent with the fact that despite the presence of more than 400 types of SCs, the only kit available in our hospital enables measurement of only three SC types. Hence, confirmation of SC use was based on anamnesis taken from patients and their relatives, rather than urinalysis in our study. Average age at onset was 16.4 and 22.7 years for substance and SC use with an average duration of use of 103 (53.9) and 33.1 (20.3) months, respectively. Marijuana was the most common substance first used (72.0%). SC was the first substance only in 8.0% of patients. A total of 38% of the patients were using only SC, while mixed substances (22%), cannabis (20%), and alcohol (10%) were the most common concomitantly used substances. SC was identified to be used on a daily basis in 54.2% and twice a week in 25.0% of patients (Table 2).
  | Table 2 Synthetic cannabinoid and other substance use in the SC-induced psychosis group |
PANSS, BPRS, HAM-A, HRSD, and FAB scores
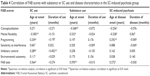
SC-induced psychosis patients had significantly lower PANSS negative scores (18.0 (6.5) vs 22.3 (6.0), P=0.004) and higher HAM-A scores (17.8 (10.3) vs 11.4 (9.4), P=0.003) than patients with schizophrenia, while the two diseases had similar PANSS positive, BPRS, HRSD, and FAB scores (Table 3).
Since patients in the schizophrenia group were significantly older than patients in SC-induced psychosis group in our cohort, PANSS negative and HAM-A scores in schizophrenia were also analyzed according to age subgroups (median split: 43.0 years). This analysis revealed a significant age effect for both scales. PANSS negative scores were still significantly higher in young schizophrenia patients than in SC-induced psychosis patients (22.9 [6.5], P=0.011), while old schizophrenia patients had significantly lower (13.3 [11.5], P=0.036) PANSS negative scores than SC-induced psychosis patients. HAM-A scores were significantly lower in old schizophrenia patients than in SC-induced psychosis patients (9.1 [5.5], P=0.003), while young schizophrenia patients had similar (21.6 [5.5], P=0.085) HAM-A scores as SC-induced psychosis patients (Table 3).
Correlation of FAB scores with substance or SC use and disease characteristics
Age at onset for SC use was correlated positively with programming (r=0.339, P=0.05), inhibitory control (r=0.289, P=0.05), and total FAB scores (r=0.364, P=0.05), while negatively with mental flexibility (r=−0.383, P=0.01) scores. Duration of SC use was negatively correlated with inhibitory control scores (r=−0.402, P=0.01) (Table 4).
Age at onset for substance use was correlated positively with mental flexibility (r=0.332, P=0.05) and total FAB scores (r=0.395, P=0.01), while negatively with conceptualization (r=−0.368, P=0.01) scores. No correlation was noted between FAB scores and duration of substance use (Table 4).
Age at disease onset was correlated positively with programming (r=0.292, P=0.01) and total FAB scores (r=0.272, P=0.05), while negatively with conceptualization (r=−0.256, P=0.05) and mental flexibility (r=−0.238, P=0.01) scores. No correlation was noted between FAB scores and duration of disease (Table 4).
Discussion
Our findings revealed that SC-induced psychosis influences young adults and is associated with remarkable rates of suicidal ideation and involuntary hospitalization alongside a psychotogenic profile comparable to schizophrenia in terms of PANSS positive, BPRS, HRSD, HAM-A, and FAB scores. Younger age at onset was associated with poorer overall frontal lobe functions regardless of the type of substance, while with poorer inhibitory control and programming performance in case of SC use.
Our findings support that clinical presentations triggered by the use of SC are frequently seen among the youth,34 emphasizing the likelihood of SC-induced psychosis to emerge in a short span of time.17
Consistent with the statement that the majority of first-time SC users are experienced marijuana smokers,1,35,36 SC was used following other transitional substances rather than as a first substance in majority of our patients, with cannabis being the most popular antecedent substance. SC was not the first substance in the majority of our patients, and preceded by use of other transitional substances, such as cannabis in most cases.7,35
SC-induced psychosis was shown to be associated with similar psychotogenic profile in terms of PANSS positive, BPRS, and HRSD scores as well as FAB scores in our cohort. Although lower PANSS negative scores and higher HAM-A scores were noted in SC-induced psychosis patients as compared with overall schizophrenia population, subgroup analysis with age-matched young schizophrenia patients revealed similar level of anxiety and still lower PANSS scores in SC-induced psychosis patients.
Paranoia, disorganized behavior, visual and auditory hallucinations, and suicidal thoughts are considered amongst the psychotic-like symptoms that can be triggered by SCs, not only in vulnerable individuals but also in subjects with no previous history of psychosis.1,16
Indeed, the rarity of negative symptoms in SC-induced psychosis has been reported; the term “spiceophrenia” is used to refer the involvement of hallucinations, delusions, and increased positive psychotic symptoms in SC-induced psychosis.34,37,38 Therefore, our findings are in line with the publications describing SC psychosis34,37 and support that SCs may trigger new-onset psychosis in otherwise healthy young men with no previous history of psychosis.1 This seems notable given that exposure to cannabis in adolescence is thought to contribute to an increased risk of psychosis later in life.11
Accordingly, data from laboratory studies indicate that SCs are likely to produce a wide range of positive, negative, and cognitive symptoms in healthy human subjects that resemble the phenomenology of schizophrenia, along with a transient exacerbation of symptoms when used by individuals with schizophrenia.21
Given that anxiety is considered amongst the acute psychoactive adverse effects associated with the consumption of SCs,1,11,38 identification of mild-to-moderate levels of anxiety similarly among SC-induced psychosis and young schizophrenia patients seems to be associated with the assessment of HAM-A scale on the seventh day of hospitalization. This also emphasizes the risk for the persistence of psychotic symptoms well beyond acute intoxication as reported in otherwise healthy young men with SC-induced new-onset psychosis.37
SC-induced psychosis is considered to be an acute onset psychosis lasting from 1–5 weeks with a need for an average 8.5 days of hospital stay in patients with severe psychotic symptoms.16,39,40 Accordingly, shorter length of hospitalization was noted in patients with SC-induced psychosis than schizophrenia in our cohort, despite similar psychotogenic profile.
Verbal learning, short-term memory and working memory, executive functions, abstract ability, decision making, and attention functions were reported to be the particularly affected cognitive domains among SC users.41 Overall frontal lobe functions were worsened with younger age at onset for SC or substance use in our cohort; while in line with the characteristic behavioral disinhibition and low impulse control resulting from reduced neural inhibition among substance users,42 inhibitory control and programming seem to be the cognitive domains specifically affected by SC.
Altered composition of SCs, with an increase of the psychoactive compound THC and a decrease of the potentially therapeutic compound CBD, is considered likely to be associated with persistent and neuroanatomic alterations in the hippocampus, prefrontal cortex, amygdala, and cerebellum.43 Association between poorer cognitive performance and younger age of onset for SC usage has also been reported.22,43
Similarity of FAB scores in terms of conceptualization, mental flexibility, programming, sensitivity to interference, inhibitory control, and environmental autonomy between the SC-induced psychosis and schizophrenia groups in our cohort supports that there is a good degree of overlap in the profile of cognitive impairments arising in response to SC use and due to schizophrenia.21,42,44
Notably, adolescent cannabinoid exposure was shown to be associated with impaired brain maturation and long-term cognitive impairment in specific components of learning and memory, alike to schizophrenia. Hence, adolescent cannabinoid exposure is considered likely to be a risk factor for developing psychosis symptoms in adulthood.45
Hence, our findings support the evidence regarding the link between cannabis use and psychosis along with similarities between SC and schizophrenia-induced cognitive impairment.22,42
Presence of suicidal ideation in one-third and involuntary hospitalizations in more than half of SC-induced psychosis patients in our cohort seems consistent with the nature of SC-induced psychosis and the fact that involuntary hospitalization is mostly caused by the circumstances where the patient has lost his/her insight and discernment, the severity of psychosis is relatively stronger, and suicidal or homicidal ideations or rejection of treatment are evident. Suicidal ideation is considered to be highly frequent among SC patients,46 and suicide-related death is considered likely to occur after severe acute psychosis or panic attack induced by SC.47
Hence, our findings emphasize the importance of observing patients with SC use referred to the hospital in terms of homicidal or suicidal behaviors and clinical picture characteristically comparable to psychosis in schizophrenia along with the likelihood of faster recovery and quicker discharge than schizophrenic patients despite an acute clinical presentation.
Certain limitations of this study should be considered. First, evaluating SC-induced psychosis seems challenging since it is relatively harder to have access to those patients who only use SC. Accordingly, in the present study, only 38% of the patients were using only SC and thus our findings may not represent clear clinical presentation specific to SC usage given the likely contribution of co-ingestion with multiple illicit drugs or alcohol to the clinical picture.
Second, since SC is composed of various additives and chemicals that may also cause a wide variety of physical signs and symptoms, it seems not possible to discriminate the exact content of SC responsible for the presenting clinical manifestations.5 Third, due to difference among SC users with respect to usage patterns and inability to reach precisely declared quantities particularly in cases with collective use with bucket or through rolling method, we failed to analyze the effects of daily dose on psychotogenic profile and cognitive impairment, which otherwise would extend the knowledge achieved in the current study. Fourth, given that urinalysis for SC screening revealed negative results for all patients consistent with the ability of the available kit to cover only three SC types, confirmation of SC use was based on anamnesis taken from patients and their relatives, rather than urinalysis in our study. Nonetheless, despite these limitations, given the paucity of the solid information regarding SC use that poses a significant risk with an ever-increasing rate notably among the youth, our findings contribute to available data on patient profile and clinical impacts of SC usage.
Conclusion
Our findings revealed that SC-induced psychosis influences young individuals and is associated with remarkable rates of suicidal ideation and involuntary hospitalization as well as similar psychotogenic profile with schizophrenia in terms of PANSS positive, BPRS, HRSD, HAM-A, and FAB scores. While younger age at onset was associated with poorer frontal lobe functions overall, inhibitory control and programming seem to be the cognitive function domains specifically affected by SC use. Hence, our findings emphasize the role of appropriate psychiatric management of SC-induced psychosis to minimize the potential risk for suicide attempt and cognitive dysfunction, given the likelihood of faster recovery despite psychotogenic profile and cognitive dysfunction comparable to schizophrenia. Further investigations are needed to have a better understanding of specific and dose-dependent long-term effects of newly emerging SCs.
Disclosure
The authors report no conflicts of interest in this work.
References
Fattore L. Synthetic cannabinoids-further evidence supporting the relationship between cannabinoids and psychosis. Biol Psychiatry. 2016;79(7):539–548. | ||
Cohen J, Morrison S, Greenberg J, Saidinejad M. Clinical presentation of intoxication due to synthetic cannabinoids. Pediatrics. 2012;129(4):e1064–e1067. | ||
Harris CR, Brown A. Synthetic cannabinoid intoxication: a case series and review. J Emerg Med. 2013;44(2):360–366. | ||
Gurdal F, Asirdizer M, Aker RG, et al. Review of detection frequency and type of synthetic cannabinoids in herbal compounds analyzed by Istanbul Narcotic Department of the Council of Forensic Medicine, Turkey. J Forensic Leg Med. 2013;20(6):667–672. | ||
Besli GE, Ikiz MA, Yildirim S, Saltik S. Synthetic cannabinoid abuse in adolescents: a case series. J Emerg Med. 2015;49(5):644–650. | ||
Coban M. The rise of synthetic marijuana in Turkey: the Bonzai phenomenon of the 2010s. Addicta Turkish J Addict. 2014;1(1):41–62. | ||
Vandrey R, Dunn KE, Fry JA, Girling ER. A survey study to characterize use of spice products (synthetic cannabinoids). Drug Alcohol Depend. 2012;120(1–3):238–241. | ||
Kucuk E, Kucuk I, Kirazaldi YY. A new threat in the emergency department: synthetic cannabinoids (Bonzai, Jamaica). Genel Tip Derg. 2015;25:18–22. | ||
Seyit M, Ozen M, Oskay A, Kadioglu E. Effectiveness of the synthetic cannabinoids seminar. Turk J Emerg Med. 2016;16(2):57–59. | ||
Every-Palmer S. Synthetic cannabinoid JWH-018 and psychosis: an explorative study. Drug Alcohol Depend. 2011;117(2–3):152–157. | ||
D’Souza DC, Spaderna M, Addy P, Ranganathan M. Spicing thing up – what can we learn from synthetic cannabinoids about the link between cannabinoids and psychosis. Schizophr Res. 2014;153(suppl 1):S32. | ||
European Monitoring Centre for Drugs and Drug Addiction (EMCDDA). Understanding the “Spice” Phenomenon. Luxembourg: Publications Office of the European Union; 2009. Available from: http://www.emcdda.europa.eu/. Accessed May 24, 2016. | ||
Seely KA, Lapoint J, Moran JH, Fattore L. Spice drugs are more than harmless herbal blends: A review of the pharmacology and toxicology of synthetic cannabinoids. Prog Neuropsychopharmacol Biol Psychiatry. 2012;39(2):234–243. | ||
Baumann MH, Solis E Jr, Watterson LR, Marusich JA, Fantegrossi WE, Wiley JL. Baths salts, spice, and related designer drugs: the science behind the headlines. J Neurosci. 2014;34(46):15150–15158. | ||
van Amsterdam J, Brunt T, van den Brink W. The adverse health effects of synthetic cannabinoids with emphasis on psychosis-like effects. J Psychopharmacol. 2015;29(3):254–263. | ||
Glue P, Al-Shaqsi S, Hancock D, Gale C, Strong B, Schep L. Hospitalization associated with use of the synthetic cannabinoid K2. N Z Med J. 2013;126(1377):18–23. | ||
Müller H, Sperling W, Köhrmann M, Huttner HB, Kornhuber J, Maler JM. The synthetic cannabinoid Spice as a trigger for an acute exacerbation of cannabis induced recurrent psychotic episodes. Schizophr Res. 2010;118(1–3):309–310. | ||
Every-Palmer S. Warning: Legal synthetic cannabinoid receptor agonists such as JWH018 may precipitate psychosis in vulnerable individuals. Addiction. 2010;105(10):1859–1860. | ||
Van der Veer N, Friday J. Persistent psychosis following the use of Spice. Schizophr Res. 2011;130(1–3):285–286. | ||
Celofiga A, Koprivsek J, Klavz J. Use of synthetic cannabinoids in patients with psychotic disorders: case series. J Dual Diagn. 2014;10(3):168–173. | ||
Sherif M, Radhakrishnan R, D’Souza DC, Ranganathan M. Human laboratory studies on cannabinoids and psychosis. Biol Psychiatry. 2016;79(7):526–538. | ||
Broyd SJ, van Hell HH, Beale C, Yücel M, Solowij N. Acute and chronic effects of cannabinoids on human cognition-a systematic review. Biol Psychiatry. 2016;79(7):557–567. | ||
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Washington, DC: American Psychiatric Publishing; 2013. | ||
Overall JE, Gorham DR. The brief psychiatric rating scale. Psychol Rep. 1962;10:799–812. | ||
Soykan C. Institutional differences and case typicality as related to diagnosis system severity, prognosis and treatment. Ankara: Master Thesis, Middle East Technical University: 1989. | ||
Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276. | ||
Kostakoglu EA, Batur S, Tiryaki A, Göğüş A. Validity and reliability of Turkish version of the Positive and Negative Syndrome Scale (PANSS). Türk Psikoloji Derg. 1999;14:23–32. | ||
Dubois B, Slachevsky A, Litvan I, Pillon B. The FAB: A Frontal Assessment Battery at bedside. Neurology. 2000;55(11):1621–1666. | ||
Güleç H, Kavakçı Ö, Güleç MY, Küçükalioğlu CI. Psychometric properties of the Turkish version of the Frontal Assessment Battery in patients with schizophrenia. J Psychiatry Neurol Sci. 2007;20(3):151–157. | ||
Williams BW. A structured interview guide for Hamilton Depression Rating Scale. Arch Gen Psychiatry. 1978;45(8):742–747. | ||
Akdemir A, Orsel S, Dag I, Türkcapar H, Iscan N, Ozbay H. The validity, reliability and clinical use of Hamilton depression rating scale. Turk J Psychiatry Psychol Psychopharmacol. 1996;4:251–259. | ||
Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32(1):50–55. | ||
Yazici MK, Demir B, Tanriverdi N, Karaagaoglu E, Yolac P. Hamilton anxiety rating scale: study of interrater reliability and validity (in Turkish). Turk J Psychiatry. 1998;9:114–117. | ||
Papanti D, Schifano F, Botteon G, et al. Spiceophrenia: a systematic overview of “spice”-related psychopathological issues and a case report. Hum Psychopharmacol. 2013;28(4):379–389. | ||
Winstock AR, Barratt MJ. Synthetic cannabis: a comparison of patterns of use and effect profile with natural cannabis in a large global sample. Drug Alcohol Depend. 2013;131(1–2):106–111. | ||
Bozkurt M, Umut G, Evren C, Karabulut V. Clinical characteristics and laboratory test results of patients admitted to outpatient clinic for synthetic cannabinoid usage. J Psychiatry Neurol Sci. 2014;27:328–334. | ||
Hurst D, Loeffler G, McLay R. Psychosis associated with synthetic cannabinoid agonists: a case series. Am J Psychiatry. 2011;168(10):1119. | ||
Morrison PD, Zois V, McKeown DA, et al. The acute effects of synthetic intravenous Delta 9-tetrahydrocannabinol on psychosis, mood and cognitive functioning. Psychol Med. 2009;39(10):1607–1610. | ||
Castellanos D, Thornton G. Synthetic cannabinoid use: recognition and management. J Psychiatry Pract. 2012;18(2):86–93. | ||
Castaneto MS, Gorelick DA, Desrosiers NA, Hartman RL, Pirard S, Huestis MA. Synthetic cannabinoids: epidemiology, pharmacodynamics, and clinical implications. Drug Alcohol Depend. 2014;144:12–41. | ||
Radhakrishnan R, Wilkinson ST, D’Souza DC. Gone to pot-a review of the association between cannabis and psychosis. Front Psychiatry. 2014;5:54. | ||
Solowij N, Michie PT. Cannabis and cognitive dysfunction: parallels with endophenotypes of schizophrenia? J Psychiatry Neurosci. 2007;32(1):30–52. | ||
Lorenzetti V, Solowij N, Yücel M. The role of cannabinoids in neuroanatomic alterations in cannabis users. Biol Psychiatry. 2016;79(7):e17–e31. | ||
Heinrichs RW, Zakzanis KK. Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology. 1998;12(3):426–445. | ||
Rubino T, Parolaro D. The impact of exposure to cannabinoids in adolescence: insights from animal models. Biol Psychiatry. 2016;79(7):578–585. | ||
Thomas S, Bliss S, Malik M. Suicidal ideation and self-harm following K2 use. J Okla State Med Assoc. 2012;105(11):430–433. | ||
Brents LK, Prather PL. The K2/Spice phenomenon: emergence, identification, legislation and metabolic characterization of synthetic cannabinoids in herbal incense products. Drug Metab Rev. 2014;46(1):72–85. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.