Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 15
Clinical Characteristics of Concomitant Diabetic Ketoacidosis in Type 2 Diabetes Patients with Acute Pancreatitis
Authors Fu Y , Liu X, Cui B, Wang C, Liu Z, Zhao B
Received 29 October 2021
Accepted for publication 14 December 2021
Published 11 January 2022 Volume 2022:15 Pages 111—119
DOI https://doi.org/10.2147/DMSO.S336619
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ming-Hui Zou
Yan Fu, Xue Liu, Beichen Cui, Cong Wang, Zhiwei Liu, Bin Zhao
Emergency Department, Beijing Jishuitan Hospital, Beijing, People’s Republic of China
Correspondence: Bin Zhao
Emergency Department, Beijing Jishuitan Hospital, No. 31, Xinjiekou East Street, Xicheng District, Beijing, 100035, People’s Republic of China
Tel +86-10-5851-6417
Email [email protected]
Objective: The objective of this retrospective study was to evaluate the clinical characteristics of diabetic ketoacidosis (DKA) in type 2 diabetes mellitus (T2DM) patients with acute pancreatitis (AP) in a cohort from China and to identify simple laboratory parameters to discriminate high-risk patients.
Methods: Patients diagnosed with AP and T2DM from January 2015 to December 2020 were retrospectively enrolled. They were divided into DKA group and non-DKA group. We calculated etiologies of AP, compared demographic and clinical features, laboratory findings on admission and clinical course. The receiver operating characteristic (ROC) curve was used to explore the ability of clinical parameters to identify high-risk patients.
Results: A total of 136 patients were enrolled, of which 19.9% (27 patients) concomitant with DKA. Compared with patients without DKA, patients with DKA were younger and more obese with higher levels of serum triglycerides (TGs), blood glucose and hemoglobin A1c (HbA1C). There was a significant difference in etiology between the two groups. Compared with the non-DKA group, the DKA group showed higher rate of HTG, lower rates of gallstones and alcohol abuse. And patients in the DKA group were more likely to be admitted to intensive care unit (ICU) and have longer hospital stays. ROC analyses showed that blood glucose concentration at a cutoff value of 21.75 mmol/L resulted in the highest Youden index with sensitivity and specificity at 81.5% and 94.5%, respectively, for identifying concomitant DKA (AUC = 0.949).
Conclusion: The prevalence of concomitant DKA in T2DM patients with AP was 19.9%, concomitant DKA patients tend to be younger, more obese and have higher blood glucose and TGs levels on admission. We found that blood glucose > 21.75mmol/L could potentially be used as a simple laboratory parameter to identify high-risk patients.
Keywords: type 2 diabetes mellitus, acute pancreatitis, diabetic ketoacidosis
Introduction
During the past decades, the prevalence of diabetes mellitus (DM) has increased significantly. DM has become a critical health problem worldwide due to its high prevalence and significant morbidity and mortality.1 A national cross-sectional study from 2015 to 2017 showed that among adults living in China, the weighted prevalence of prediabetes and total diabetes using the WHO criteria were 35.2% and 11.2%, respectively.2 T2DM is the most common form of DM, approximately 90% of all DM patients. DKA which is characterized by ketoacidosis, ketonuria and hyperglycemia is a potentially life-threatening acute metabolic complication of DM that often requires intravenous insulin therapy and fluid resuscitation in ICU. AP, a rapid onset of inflammation of the pancreas that can lead to life-threatening illness, is the first most expensive digestive disease, the second highest cause of total hospital stays, and the fifth leading cause of in-hospital mortality.3
The association among T2DM, DKA and AP has been discussed in several literatures.4–6 Previous studies demonstrated that T2DM increased the risk of AP by 1.9–2.9 times,7–9 especially in younger patients with poorly controlled DM. AP as a consequence or cause of DKA has been reported previously.4 Significant higher mortality was found in patients with AP and concomitant DKA than those with AP alone.6
Arterial blood gas (ABG) test, which is important in the diagnosis of DKA, is usually not one of the primary tests ordered when patients present to the emergency department with complaint of abdominal pain, especially when diagnosis of AP is made firstly, as a result diagnosis of DKA is often delayed. Concomitant DKA exacerbates hypovolemic shock and metabolic disorders in patients with AP, thus in most cases, these patients require more aggressive fluid resuscitation and intravenous insulin therapy than those with AP alone. Early identification of patients with AP of high-risk for concomitant DKA is crucial for reducing adverse outcomes and beneficial for therapeutic approaches. Therefore, we evaluated the clinical characteristics of concomitant DKA in T2DM patients with AP in this retrospective study. The ROC curve was used to explore the ability of clinical parameters to identify high-risk patients.
Materials and Methods
Data Collection
We retrospectively reviewed the medical records of patients who were admitted to the emergency department of Beijing Jishuitan Hospital from January 2015 to December 2020. Inclusion criteria: 1) a previous history of T2DM; 2) diagnosed with AP according to the Atlanta criterion:10 fulfilled at least two of the three following criteria: 1) abdominal pain consistent with AP; 2) serum amylase activity at least three times greater than the upper limit of normal; 3) characteristic findings of AP on computed tomography (CT). DKA diagnosis was made according to the American Diabetes Association (ADA) consensus guidelines:11 1) plasma glucose >13.9 mmol/L; 2) presence of positive serum or urine ketones; 3) arterial pH <7.3, serum bicarbonate <18mmol/L and anion gap (AG) >10mmol/L. Hypertriglyceridemia (HTG) diagnosis was made when TGs concentration ≥150 mg/dl (1.7mmol/L) according to NCEP ATP III.12 Exclusion criteria: 1) <18 years old; 2) a previous history of chronic pancreatitis or pancreatic tumor; 3) gravida; 4) without complete data profiles.
We documented demographic information (sex and age), body mass index (BMI), symptoms on admission (abdominal pain, nausea and/or vomiting), vital signs (blood pressure and mental status), etiologies of AP (gallstones, alcohol abuse and HTG), laboratory findings on admission. We also collected information on intravenous insulin therapy, ICU admission, length of hospital stays and mortality. Besides, Acute Physiology and Chronic Health Evaluation II (APACHE II), Ranson criteria, Bedside Index for Severity in Acute Pancreatitis (BISAP score), Modified Marshall score, Balthazar CT grade and Sequential Organ Failure Assessment Score (SOFA score) were calculated and documented.
This retrospective study was conducted according to guidelines laid down in the Declaration of Helsinki and all procedures were approved by the Beijing Jishuitan Hospital Institutional Review Board (IRB) (No. 202109–59). Data were obtained with permission from the medical director office of the respective center, and the data were maintained with confidentiality. The IRB waived the requirement to obtain informed consent for this study for the following reasons: 1) this study involves no more than minimal risk to the patients; 2) the waiver will not adversely affect the rights and welfare of the patients; 3) the study could not practicably be carried out without the waiver; 4) whenever appropriate, the patients will be provided with additional pertinent information after participation.
Statistical Analysis
Statistical analyses were performed using IBM SPSS Statistics for Windows, version 24.0 (IBM Corp., Armonk, NY, USA). All descriptive statistics were summarized and displayed as the mean ± standard deviation (SD) for continuous variables or the median with 25% to 75% interquartile range for categorical data. The primary analysis compared the DKA group with the non-DKA group. All the variables were tested for a normal distribution using the Kolmogorov–Smirnov test. Continuous variables and normal distribution data were compared using independent sample t tests. Categorical data were compared using the Chi-square test or Fisher's exact test. The independent predictors of DKA were identified using logistic regression and including the factors that were significant in the univariate analysis. Results were considered significant if they achieved a P-value of <0.05. The ROC curve was used to explore the ability of clinical parameters to identify high-risk patients.
Results
Comparison of Demographic and Clinical Features on Admission of DKA Group and Non-DKA Group
A total of 1176 consecutive patients were diagnosed with AP from January 2015 to December 2020, of which 155 patients with confirmed diagnosis of T2DM. Nineteen patients were excluded according to the exclusion criteria. At last, 136 patients were enrolled in our study (Table 1), 27 patients (19.9%) had DKA, including 22 males and 5 females, the mean age was 31 years, ranging from 18 to 70 years, the mean BMI was 27.7 kg/m2, whereas 12 patients (44.4%) were obese. In the non-DKA group, there were 109 patients (80.2%), including 78 males and 31 females, the mean age was 50 years, ranging from 24 to 96 years, the mean BMI was 24.8 kg/m2, whereas 16 patients (14.7%) were obese. Patients in the DKA group were younger (31 years vs 50 years, P < 0.001) and more obese with higher BMI (27.7 kg/m2 vs 24.8 kg/m2, P = 0.005) than those in the non-DKA group.
 |
Table 1 Comparison of Demographic and Clinical Features on Admission of DKA Group and Non-DKA Group |
Mental status was categorized into alert and not alert (including drowsy, stupor and coma) based on the reaction level scale. There were more patients presented to be not alert on admission in the DKA group than in the non-DKA group (18.5% vs 4.6%, P = 0.038). Nausea and/or vomiting (70.4% vs 86.2%, P = 0.049) were more likely to occur in patients with DKA. There were no significant differences in abdominal pain (85.2% vs 94.5%, P = 0.212) or BP on admission between the two groups.
Comparison of Laboratory Findings of DKA Group and Non-DKA Group (Table 2)
Patients in the DKA group had high AG metabolic acidosis with lower level of partial pressure of carbon dioxide (20.5 mmHg vs 36.3 mmHg, P < 0.001), which was supposed to be a sign of respiratory compensation. Moreover, they had lower PH (7.29 vs 7.39, P < 0.001) and lower serum bicarbonate level (11.1 mmol/L vs 23.2 mmol/L, P < 0.001), which were consistent with the diagnosis of DKA.
 |
Table 2 Comparison of Laboratory Findings of DKA Group and Non-DKA Group |
Higher levels of lactate (Lac, 1.9 mmol/L vs 1.2 mmol/L, P = 0.001), hematocrit (HCT, 46.9% vs 42.4%, P < 0.001), blood urea nitrogen (BUN, 6.6 mmol/L vs 5.0 mmol/L, P = 0.015) and serum osmolality (320.3 mOsm/kg vs 301.7 mOsm/kg, P < 0.001) were found in patients with DKA. Moreover, compared with the non-DKA group, patients in the DKA group had higher blood glucose (26.1 mmol/L vs 12.6 mmol/L, P < 0.001) and HbA1C (11.0% vs 8.0%, P < 0.001), lower levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), gamma-glutamyl transferase (GGT), total bilirubin (TBil), direct bilirubin (DBil) were found in patients with DKA. There was no significant difference in serum creatinine on admission.
No significant difference was found in serum amylase between the two groups. The overall incidence of hyperamylasemia was 69.1% (94), and 43.4% (59) patients had serum amylase levels three times greater than the upper limit of normal. In the DKA group, 63.0% (17) patients had serum amylase levels less than three times the upper limit of normal, while 40.7% (11) patients without serum amylase elevated. All 17 patients had HTG on admission, and 8 of them had severe HTG (TGs ≥ 11.3mmol/L). On the other hand, serum amylase in 60 (55.1%) patients in non-DKA group was less than three times the upper limit of normal, whereas 31 (28.4%) patients without serum amylase elevated, 47 patients had HTG, and 29 of them had severe HTG on admission.
The overall incidence of HTG was 69.1% (94), whereas severe HTG was found in 39.7% (54) patients, 59.3% (16) patients in the DKA group and 34.9% (38) patients in the non-DKA group. Patients in the DKA group had a higher incidence of HTG and higher levels of TGs (11.7 mmol/L vs 2.7 mmol/L, P = 0.002) and cholesterol (9.9 mmol/L vs 5.9 mmol/L, P < 0.001) compared with those in the non-DKA group.
Comparison of Clinical Course of DKA Group and Non-DKA Group (Table 3)
Patients in the DKA group were more likely to be admitted to ICU for close monitoring (37.0% vs 5.5%, P < 0.001), to receive intravenous insulin therapy (81.5% vs 13.8%, P < 0.001) and stay longer in hospital (15 days vs 11 days, P = 0.014). However, there were no significant differences in mortality rates between the two groups.
 |
Table 3 Comparison of the Clinical Course of DKA Group and Non-DKA Group |
Comparison of the Etiologies of AP
The etiologies of AP are shown in Table 4. The three main etiologies were HTG (48.5%), gallstones (30.9%) and alcohol abuse (19.9%). There were significant differences in etiologies between the two groups. Compared with the non-DKA group, the DKA group showed higher rate of HTG (88.9% vs 38.5%), lower rates of gallstones (3.7% vs 37.6%) and alcohol abuse (7.4% vs 22.9%).
 |
Table 4 Comparison of the Etiologies of AP |
Comparison of Risk Assessment Scores of DKA Group and Non-DKA Group
Six standardized risk assessment scores were calculated and summarized in Table 5. Patients in the DKA group had higher Ranson criteria (3 vs 2, P = 0.038). There were no significant differences between the two groups in APACHE II, BISAP score, Marshall score, Balthazar CT grade or SOFA score.
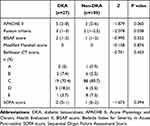 |
Table 5 Comparison of Risk Assessment Scores of DKA Group and Non-DKA Group |
ROC Curve Analysis on the Optimal Clinical Parameters in Predicting Concomitant DKA in T2DM Patients with AP
The ROC curve was performed (Figure 1, Table 6), and the surface area under the curve (AUC) for blood glucose identifying concomitant DKA was 0.949 (95% CI, 0.909–0.988). When a cut-off value of blood glucose concentration >21.75mmol/L was used for diagnosis of concomitant DKA, sensitivity was 81.5%, specificity was 94.5%, positive predictive value was 78.6%, negative predictive value was 95.4% and the accuracy was 91.9% (Table 7).
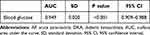 |
Table 6 AUC for Blood Glucose Identifying Concomitant DKA in T2DM Patients with AP |
 |
Table 7 Cut-off Value of Blood Glucose for Identifying Concomitant DKA in T2DM Patients with AP |
Discussion
In this single-center retrospective cohort study of 136 T2DM patients with AP, we found that 27 patients (19.9%) fulfilled the diagnostic criteria of DKA, the incidence of DKA in T2DM patients with AP was much higher than that of patients with AP alone, which was about 1.2% to 2.1% according to published literatures.5,6 Poorly controlled DM is a risk factor for both AP and DKA. However, we still need large population or epidemiologic studies to confirm the high prevalence of DKA in T2DM patients with AP.
Patients in the DKA group were younger and more obese with higher BMI than those in the non-DKA group, which was consistent with previous studies.6 This may be because alcohol-induced HTG affects young people more.13 On the other hand, young people have more family and social responsibilities but less health awareness, unhealthy lifestyles such as high energy and/or high fat diet and lack of physical activity, as well as ineffective medical treatment, leading to poorly controlled DM. HbA1C reflects average blood glucose over approximately 3 months. In our study, elevated HbA1C was found in most cases, especially in DKA patients, where the mean HbA1C was as high as 11.0%, significantly higher than the target of 7.0% for non-pregnant adults recommended in ADA 2020 Guideline.14 Elevated HbA1C indicates poor glycemic control, which may be the initial factor leading to subsequent AP and DKA.15 In our study, blood glucose concentration > 21.75mmol/L could be used to diagnose concomitant DKA with sensitivity and specificity at 81.5% and 94.5%, respectively.
The three most common symptoms of AP are fever, abdominal pain, nausea and/or vomiting, with or without DKA.10,16 In our study, patients with DKA were more likely to experience nausea and/or vomiting. However, the diagnosis of concomitant DKA is still easily delayed due to the similarity of clinical presentation with AP-only patients. The reaction level scale was used to assess a patient’s level of consciousness, and previous studies have concluded that there was a positive linear relationship between serum osmolality and change in mental status, which was a risk factor of DKA.5 In our study, more patients in the DKA group presented to be not alert on admission. They also had higher level of serum osmolality. DKA should be considered when T2DM patients with AP presented to be not alert on admission, especially in those with definite rise in serum osmolality.
Serum amylase is used to diagnose AP. Due to the etiology of AP and the timing of the test, the sensitivity of serum amylase in the diagnosis of AP ranges between 45% and 87%. On the other hand, published literatures have concluded that hyperamylasemia could occur in 16% to 25% of the cases in the presence of DKA, possibly due to severely insufficient insulin action.17,18 In our study, 94 (69.1%) patients had hyperamylasemia, while 59 (43.4%) patients had serum amylase levels three times greater than the upper limit of normal, and more than a quarter of patients had serum amylase levels within the normal range, with no significant differences found between the DKA and non-DKA groups. There are probably three reasons. Firstly, serum amylase levels rise rapidly in the setting of AP, peaking within 3–6 hours of symptoms onset, with a short half-life of 10–12 hours, and returning to normal within 3–5 days.19 Normal levels may be related to the timing of patients’ presentation to the emergency department, too early or too late presentations may result in normal level results. Secondly, previous studies have shown that HTG may occur in the presence of DKA,4,6 and severe HTG may result in lower serum amylase level due to calorimetric interference of lipemic serum.20,21 Thirdly, low serum amylase levels were associated with T2DM.22,23 After all, an initial negative result from a serum amylase test is unlikely to rule out a diagnosis of AP,20,21 especially if the patient is brought to the emergency department relatively early in the clinical course, or has DKA/HTG/T2DM.
Previous studies show that gallstones and alcohol abuse are the main etiologies of AP,24,25 and the incidence of hypertriglyceridemic pancreatitis (HTGP) is on the rise, HTG has become the third leading cause of AP, accounting for 8% to 15% of AP cases.26–28 The coexisting of DKA, AP and HTG has been discussed.4,6 Previous studies concluded that HTG played an important role in disease process,29 AP may be secondary to DKA induced HTG (DKA→HTG→AP).4 On the other hand, HTGP can result in transient insulin deficiency triggered by acute destruction of pancreatic beta cells, leading to DKA (HTG→AP→DKA), especially in patients with poorly controlled DM.30 In our study, HTG is the main cause of AP in T2DM patients, especially in those with concomitant DKA patients. The prevalence is up to 88.9%, it is much higher than previous studies. In a prospective study of 100 consecutive cases, the prevalence of the HTG in AP with concomitant DKA was 36.4%.31 Compared with the non-DKA group, the DKA group had higher levels of TGs. Severe HTG was seen in 54 patients, 20 in the DKA group and 34 in the non-DKA group. More patients in the DKA group had severe HTG (P = 0.002). However, multivariate analysis showed no significant correlation between HTG and DKA (P=0.052). In our study, the levels of ALT, AST, GGT, TBil and DBil were higher in the non-DKA group, and these changes were consistent with the higher incidence of gallstones in the non-DKA group.
Concomitant DKA could deteriorate hypovolemic shock and metabolic disorders, exacerbate the severity of AP and result in increased mortality. In our study, patients with concomitant DKA had more severe hyperglycemia, and most of them received intravenous insulin therapy. Compared with the non-DKA group, the DKA patients had higher levels of Lac, HCT, BUN and serum osmolality, all of which were associated with dehydration,32 and they all received more aggressive fluid resuscitation. At the same time, patients in the DKA group were more likely to be admitted to ICU, and stay longer in hospital. In a large cohort study which enrolled 2.8 million patients with AP, 33,356 patients had DKA.6 Compared with patients with AP alone, patients with DKA had a higher incidence of complications, such as acute kidney injury, systemic inflammatory response syndrome, shock, acute respiratory distress syndrome, sepsis, ileus and parenteral nutrition requirement, and patients with DKA had a longer hospital stay and significantly increased mortality.6 In our study, one patient in the DKA group died of multiple organ failure and intraabdominal hypertension, while no patient in the non-DKA group died. There was no significant difference between the two groups, which may be due to the small sample size. According to the Ranson criteria, we found that concomitant DKA worsened the severity of AP. However, in the setting of DKA, hyperglycemia, acidosis and dehydration induced by DKA may increase Ranson criteria score, so the differences in Ranson criteria may reflect derangement of laboratory values secondary to DKA rather than objective severity of AP.30 To our knowledge, there is not one scale more objective for prediction of severity of AP concomitant with DKA.
Limitations of the Study
Our study had some limitations. Firstly, this was a single-center retrospective cohort study, there is a potential selection bias. Secondly, a major limitation was small sample size. Only 136 patients were enrolled, of which 27 patients in the DKA group and only one in-hospital death was documented. Prospective studies with larger sample sizes are necessary to confirm our findings in the future.
Conclusion
In conclusion, our study showed that there was a high prevalence of concomitant DKA in T2DM patients with AP. Concomitant DKA patients tend to be younger, more obese and have higher levels of blood glucose and TGs on admission. We found that blood glucose concentration >21.75mmol/L could potentially be used as a simple laboratory parameter to identify high-risk patients. The physicians should consider the possibility of concomitant DKA in these patients.
Funding
This project is funded by Beijing Jishuitan Hospital Nova Program XKXX201807.
Disclosure
The authors declare no conflicts of interest.
References
1. Ogurtsova K, da Rocha Fernandes JD, Huang Y, et al. IDF diabetes atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. 2017;128:40–50. doi:10.1016/j.diabres.2017.03.024
2. Li Y, Teng D, Shi X, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ. 2020;369:m997. doi:10.1136/bmj.m997
3. Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143(5):1179–1187 e1173. doi:10.1053/j.gastro.2012.08.002
4. Singla AA, Ting F, Singla A. Acute pancreatitis secondary to diabetic ketoacidosis induced hypertriglyceridemia in a young adult with undiagnosed type 2 diabetes. JOP. 2015;16(2):201–204. doi:10.6092/1590-8577/2961
5. Yuan S, Liao J, Cai R, Xiong Y, Zhan H, Zheng Z. Acute pancreatitis concomitant with diabetic ketoacidosis: a cohort from South China. J Int Med Res. 2020;48(3):300060520912128. doi:10.1177/0300060520912128
6. Simons-Linares CR, Jang S, Sanaka M, et al. The triad of diabetes ketoacidosis, hypertriglyceridemia and acute pancreatitis. How does it affect mortality and morbidity?: a 10-year analysis of the National Inpatient Sample. Medicine. 2019;98(7):e14378. doi:10.1097/MD.0000000000014378
7. Noel RA, Braun DK, Patterson RE, Bloomgren GL. Increased risk of acute pancreatitis and biliary disease observed in patients with type 2 diabetes: a retrospective cohort study. Diabetes Care. 2009;32(5):834–838. doi:10.2337/dc08-1755
8. Gonzalez-Perez A, Schlienger RG, Rodriguez LA. Acute pancreatitis in association with type 2 diabetes and antidiabetic drugs: a population-based cohort study. Diabetes Care. 2010;33(12):2580–2585. doi:10.2337/dc10-0842
9. Girman CJ, Kou TD, Cai B, et al. Patients with type 2 diabetes mellitus have higher risk for acute pancreatitis compared with those without diabetes. Diabetes Obes Metab. 2010;12(9):766–771. doi:10.1111/j.1463-1326.2010.01231.x
10. Banks PA, Bollen TL, Dervenis C, et al. Classification of acute pancreatitis–2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62(1):102–111. doi:10.1136/gutjnl-2012-302779
11. Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. 2009;32(7):1335–1343. doi:10.2337/dc09-9032
12. Expert Panel on Detection E. Treatment of High Blood Cholesterol in A. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001;285(19):2486–2497. doi:10.1001/jama.285.19.2486
13. Bessembinders K, Wielders J, van de Wiel A. Severe hypertriglyceridemia influenced by alcohol (SHIBA). Alcohol Alcohol. 2011;46(2):113–116. doi:10.1093/alcalc/agq088
14. American Diabetes A. 6. Glycemic Targets: standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(Suppl1):S66–S76. doi:10.2337/dc20-S006
15. Kota SK, Meher LK, Jammula S, Kota SK, Modi KD. Genetics of type 2 diabetes mellitus and other specific types of diabetes; its role in treatment modalities. Diabetes Metab Syndr. 2012;6(1):54–58. doi:10.1016/j.dsx.2012.05.014
16. Kitabchi AE, Umpierrez GE, Murphy MB, Kreisberg RA. Hyperglycemic crises in adult patients with diabetes: a consensus statement from the American Diabetes Association. Diabetes Care. 2006;29(12):2739–2748. doi:10.2337/dc06-9916
17. Rizvi AA. Serum amylase and lipase in diabetic ketoacidosis. Diabetes Care. 2003;26(11):3193–3194. doi:10.2337/diacare.26.11.3193
18. Yadav D, Nair S, Norkus EP, Pitchumoni CS. Nonspecific hyperamylasemia and hyperlipasemia in diabetic ketoacidosis: incidence and correlation with biochemical abnormalities. Am J Gastroenterol. 2000;95(11):3123–3128. doi:10.1111/j.1572-0241.2000.03279.x
19. Basnayake C, Ratnam D. Blood tests for acute pancreatitis. Aust Prescr. 2015;38(4):128–130. doi:10.18773/austprescr.2015.043
20. Scherer J, Singh VP, Pitchumoni CS, Yadav D. Issues in hypertriglyceridemic pancreatitis: an update. J Clin Gastroenterol. 2014;48(3):195–203. doi:10.1097/01.mcg.0000436438.60145.5a
21. Garg R, Rustagi T. Management of hypertriglyceridemia induced acute pancreatitis. Biomed Res Int. 2018;2018:4721357. doi:10.1155/2018/4721357
22. Yadav R, Bhartiya JP, Verma SK, Nandkeoliar MK. The evaluation of serum amylase in the patients of type 2 diabetes mellitus, with a possible correlation with the pancreatic functions. J Clin Diagn Res. 2013;7(7):1291–1294. doi:10.7860/JCDR/2013/6016.3120
23. Nakajima K. Low serum amylase and obesity, diabetes and metabolic syndrome: a novel interpretation. World J Diabetes. 2016;7(6):112–121. doi:10.4239/wjd.v7.i6.112
24. Lankisch PG, Apte M, Banks PA. Acute pancreatitis. Lancet. 2015;386(9988):85–96. doi:10.1016/S0140-6736(14)60649-8
25. Forsmark CE, Vege SS, Wilcox CM. Acute pancreatitis. N Engl J Med. 2016;375(20):1972–1981. doi:10.1056/NEJMra1505202
26. Association PDGoCSoGoCM. Guideline for the diagnosis and treatment of acute pancreatitis in China (2019 Shenyang). J Chin J Pancreatol. 2019;19(5):321–331. doi:10.3760/cma.j.issn.1674-1935.2019.05.001
27. Zhu Y, Pan X, Zeng H, et al. A study on the etiology, severity, and mortality of 3260 patients with acute pancreatitis according to the Revised Atlanta Classification in Jiangxi, China over an 8-year period. Pancreas. 2017;46(4):504–509. doi:10.1097/MPA.0000000000000776
28. Parniczky A, Kui B, Szentesi A, et al. Prospective, multicentre, nationwide clinical data from 600 cases of acute pancreatitis. PLoS One. 2016;11(10):e0165309. doi:10.1371/journal.pone.0165309
29. Mosztbacher D, Hanak L, Farkas N, et al. Hypertriglyceridemia-induced acute pancreatitis: a prospective, multicenter, international cohort analysis of 716 acute pancreatitis cases. Pancreatology. 2020;20(4):608–616. doi:10.1016/j.pan.2020.03.018
30. Wang Y, Attar BM, Hinami K, et al. Concurrent diabetic ketoacidosis in hypertriglyceridemia-induced pancreatitis: how does it affect the clinical course and severity scores? Pancreas. 2017;46(10):1336–1340. doi:10.1097/MPA.0000000000000937
31. Nair S, Yadav D, Pitchumoni CS. Association of diabetic ketoacidosis and acute pancreatitis: observations in 100 consecutive episodes of DKA. Am J Gastroenterol. 2000;95(10):2795–2800. doi:10.1111/j.1572-0241.2000.03188.x
32. Marra MV, Simmons SF, Shotwell MS, et al. Elevated serum osmolality and total water deficit indicate impaired hydration status in residents of long-term care facilities regardless of low or high body mass index. J Acad Nutr Diet. 2016;116(5):828–836 e822. doi:10.1016/j.jand.2015.12.011
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

