Back to Journals » Infection and Drug Resistance » Volume 15
Clinical Characteristics in Patients with Redetected Positive RNA Test After Recovery from Foreign-Imported COVID-19 Cases in Xi’an, China
Authors Yan Y, Yang L, Li X, Hao J, Wang B, Wang D, Wang J
Received 16 April 2022
Accepted for publication 16 June 2022
Published 24 June 2022 Volume 2022:15 Pages 3295—3307
DOI https://doi.org/10.2147/IDR.S371088
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Yun Yan,1,* Lei Yang,2,* Xiaoli Li,3,* Jian Hao,4,* Bijue Wang,4 Dan Wang,5 Junning Wang3
1Department of Orthopedics and Traumatology, Honghui Hospital, Xi’an Jiaotong University, Xi’an, Shaanxi, 710054, People’s Republic of China; 2Department of Osteoporosis, Honghui Hospital, Xi’an Jiaotong University, Xi’an, Shaanxi, 710054, People’s Republic of China; 3Department of Respiratory, Honghui Hospital, Xi’an Jiaotong University, Xi’an, Shaanxi, 710054, People’s Republic of China; 4Xi’an Public Health Center, Xi’an, Shaanxi, 710200, People’s Republic of China; 5Department of Pathology, Honghui Hospital, Xi’an Jiaotong University, Xi’an, Shaanxi, 710054, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Junning Wang, Department of Respiratory, Honghui Hospital, Xi’an Jiaotong University, No. 555, Youyi East Road, Nanshaomen, Xi’an, Shaanxi, 710054, People’s Republic of China, Tel/Fax +86 02962818354, Email [email protected]
Purpose: At present, it has been found that managing patients with a redetected positive RNA test after recovery from foreign-imported coronavirus disease 2019 (COVID-19) cases in China is challenging. The purpose of the current study was to describe the clinical characteristics of these patients.
Methods: This retrospective cohort study included 137 COVID-19 patients who were discharged from the Xi’an Public Health Center from 28 July 2020 to 31 December 2021. We compared the clinical characteristics between positive retest patients and non-positive retest patients.
Results: 137 COVID-19 patients entered our study, 27 (19.7%) cases of COVID-19 with a redetected positive RNA test by the end of the follow-up period. Fever [(n = 31 (22.6%)], cough [n = 26 (18.9%)] and sore throat [n = 20 (14.5%)] were the most common initial symptoms among the foreign-imported COVID-19 patients, and there were almost no significant differences in initial symptoms between positive retest patients and non-positive retest patients. The positive retest patients had a higher lymphocyte count (p = 0.031) and lymphocyte percentage (p = 0.007) during readmission. There were generally no significant differences in other routine blood test findings, IgG and IgM antibody responses, between positive retest patients and non-positive retest patients, or in positive retest patients over time (before, during, or after positive patient detection). After readmission, positive retest patients displayed fewer symptoms or no obvious disease progression and more sustained remission by CT imaging.
Conclusion: Our findings revealed that the clinical characteristics at the time of initial diagnosis were not closely related to redetected positive RNA tests after recovery from foreign-imported COVID-19 cases. Positive retest patients had virtually no symptoms and displayed no obvious disease progression during readmission. These findings provide important information and clinical evidence for the effective management of foreign-imported COVID-19 patients during their convalescent phase.
Keywords: SARS-CoV-2, COVID-19, clinical characteristics, foreign-imported cases, redetected positive RNA test
Introduction
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). At present, COVID-19 has spread globally, which has resulted in the present worldwide pandemic.1 As of March 5, 2022, more than 450 million suffered from this disease, and deaths exceeded 6 million worldwide,2 posing huge challenges for medical institutions and public health.3 Owing to the efficient prevention and control measures carried out by the government, to some extent, the COVID-19 epidemic in mainland China has been well controlled since March 2020.4 However, COVID-19 still transmits rapidly and is much more devastating than expected, showing no signs of slowing down due to the continued uncontrolled mutations of SARS-CoV-2 and the complexity and high volume of international flights.5–7 With the surge of returnees from foreign cases, our task has become extremely arduous. At the current stage, the main task of epidemic prevention and control is to prevent and manage imported cases from abroad. Transmission from a asymptomatic carrier has been reported, and it is very important to screen and quarantine both infected patients and potential asymptomatic carriers,8 which challenges symptom-based screening that may potentially miss travellers concealing symptoms or travellers with asymptomatic viral carriers during travel and contribute to foreign-imported COVID-19 cases. Currently, real-time (RT)-PCR for the detection of SARS-CoV-2 RNA in nasal swab and pharyngeal swab samples is a reliable test for detecting both symptomatic and asymptomatic COVID-19.8,9 When we treated patients with COVID-19 in Xi’an Public Health Center, we found an increasing number of patients with redetected positive RNA tests after recovery being discharged from the hospital. This is in line with the results reported by Lan.10 The redetected positive RNA test aroused our interest. The management of repositive patients is challenging because of the mechanism of repositive SARS-CoV-2, and its infectivity is still unclear, but this condition results in a longer hospitalization and isolation time. Meanwhile, patients with positive retest SARS-CoV-2 account for approximately 11.0%–20.4% of infectious patients, bringing mounting pressure to the medical and health organization and patients’ psychological condition.11–13 An et al14 indicated that the recurrent positive patients were characterized by a younger age and milder symptoms during hospitalization. However, the former reported focus on positive retest patients domestically, and there have been few reports of positive retest patients from abroad.
We conducted a retrospective study of 137 overseas-imported COVID-19 cases that recovered from COVID-19. Among these patients, 27 recurrent positive cases were identified, and 3 cases were multiple recurrent positions. Compared with the nonrecurrent positive patients, we detailed the clinical characteristics of positive retest patients, clarifying the characteristics of positive retest patients is urgent for appropriately managing these patients. To provide empirical information and evidence-based support for the management of cases with a redetectable positive RNA test after recovery.
Materials and Methods
Patients
For this retrospective analysis, clinical data records were collected from the Xi’an Public Health Center, which was the officially designated hospital to quarantine and treat foreign-imported COVID-19 cases in Shaanxi Province. The patient had a history of travel or residence in a foreign country or region within 14 days before the onset of the disease were defined as foreign-imported cases. All COVID-19 patients were selected as the study population in Xi’an Public Health Centre, and their clinical data were extracted from 28 July 2020 to 31 December 2021. All COVID-19 case diagnoses, clinical classifications, treatment and discharge criteria were determined by the Diagnosis and Treatment Protocol of Coronavirus Diseases 2019,15 National Health Commission (NHC) of the People’s Republic of China. The confirmed cases were admitted to the COVID-19 confirmed ward for further treatment. The COVID-19 patient’s discharge criteria were to meet the following 4 conditions at the same time: (1) normal temperature for ≥3 days, (2) significant improvement in respiratory symptoms, (3) significant absorption of acute lesions in chest CT images, and (4) negative results for SARS CoV-2 RNA from two consecutive respiratory sample swabs obtained at least 24 h apart. All discharged patients continued to be quarantined and were observed for 14 days in centralized facilities. At the end of the quarantine period, both nasopharyngeal and oropharyngeal swabs were collected from each patient for SARS-CoV-2 RNA detection by RT-PCR. In addition, each patient underwent physical examination, routine laboratory tests and chest CT examination at this time. The flowchart of management for foreign-imported COVID-19 patients is shown in Figure 1.
 |
Figure 1 A flow chart of management for foreign-imported COVID-19 patients. |
Data Collection
General information, including demographic data [ie, sex, age, body mass index (BMI), country of departure], medical comorbidities, clinical symptoms, clinical severity information, laboratory results and chest computed tomography imaging (CT) features as well as treatment details and clinical endpoints, especially the RNA test of SARS-CoV-2, was obtained using a standardized data collection form from electronic hospital medical records and attending doctors. Clinical severity on first admission was classified as asymptomatic, mild, moderate, or critical based on Chinese Guidelines for Diagnosis and Treatment for Novel Coronavirus Pneumonia.15 The countries in which imported cases had a history of travel or residence in a foreign country or region within 14 days before the onset of the disease were defined as the source of their infection. The date of onset of the disease was defined as the first RT–PCR positive result for the virus for asymptomatic patients or the date of the onset of symptoms for symptomatic patients. The protocol of this study was approved by the Ethics Committee of Honghui Hospital, Xi’an Jiaotong University (approval number: 202203017). Written patient consent was waived by the Ethics Commission because the study was a retrospective analysis and only involved the extraction of medical records. The information from the patients we studied was anonymized. All methods were carried out in accordance with relevant guidelines and regulations of declaration of Helsinki.
Strategy for Nucleic Acid Tests
The open reading frame 1ab (ORF1ab) and nucleocapsid protein (N) were the two target genes of SARS-CoV-2 using a 2019-nCoV nucleic acid detection reagent and a commercial kit (Bio-germ, Shanghai, China) recommend by the Chinese Center for Disease Control and Prevention (CCDC). In this study, although both the ORF1b gene and N gene of SARS-CoV-2 were detected in specimens with cycle threshold (Ct) values of ≤40 for both tested genes that were considered positive, single-gene-positive specimens were retested old specimen to perform extraction again to perform RT-PCR and considered positive if the Ct values from the repeat tests were ≤40.
Statistical Analysis
Continuous variables are expressed as the means ± standard deviations (SDs) for data with a normal distribution. Otherwise, they are expressed as medians with interquartile ranges (25% and 75%), and comparisons between groups were analysed with Student’s t test or the Mann-Whitney U-test. Categorical variables are described as counts with percentages (%), and differences between groups were analysed with the χ2 test or Fisher’s exact test. All statistical analyses were performed using SPSS software (version 19.0; SPSS Inc., Chicago, IL, USA) in this study. P < 0.05 denoted statistical significance for all two-tailed tests.
Results
Demographic and Clinical Characteristics of All Included Patients
A total of 213 COVID-19 patients were selected as the initial study population from 28 July 2020 to 31 December 2021 in the Xi’an Public Health Centre. Six patients who lacked complete data were excluded. Seventy patients who had a history of COVID-19 infection were excluded. Finally, 137 patients entered our study. Twenty-seven cases of COVID-19 were redetected with positive SARS-CoV-2 RNA as a positive retest group, including 3 patients with twice recurrent-positive results post discharge, and 110 patients who did not show positive RT–PCR results again by the end of the follow-up period were included as a nonpositive retest group. The 137 foreign-imported patients were from 22 countries, one-fifth of them were from Uzbekistan. Majority of the patients (89.8%) were male while over half of the patients (68.6%) were aged 25–49 years. All of the patients recovered and discharged. The demographic characteristics of the patients are shown in Table 1.
 |
Table 1 Demographic Characteristics of the Imported COVID-19 Cases |
Clinical Characteristics on the First Admission
A total of 89.8% of patients were male, and 10.2% of patients were female, but no significant difference in sex was found between positive retest patients and non-positive retest patients. There were also no significant differences in BMI or sex distribution between positive retest patients and non-positive retest patients. Hypertension [n = 10 (7.3%)] and hepatic adipose infiltration (n = 4 (2.9%)] were the most common comorbidities among the COVID-19 patients. Additionally, a few patients had diabetes mellitus, respiratory system diseases, and coronary heart disease, but there were no significant differences between the 2 groups. Asymptomatic [n=67 (48.9%)] was the most common disease severity classification among the COVID-19 patients. Mild and moderate cases accounted for 23.3% (n=32) and 27.0% (n=37), respectively, in this study population. There was only 1 severe case in this study cohort, and there were no critically ill patients. However, there were no significant differences in distribution between the 2 groups. Fever [n = 31 (22.6%)], cough [(n = 26 (18.9%)] and sore throat [n = 20 (14.5%)] were the most common initial symptoms among the COVID-19 patients. Additionally, a few patients had diarrhoea, stuffy nose, shortness of breath, rhinorrhea, fatigue, chest pain, headache, mental disorder, and muscle ache. Notably, the incidence rate of rhinorrhoea [2 (7.4%) vs 1 (0.9%); p = 0.039] as part of the initial symptoms was higher in positive retest patients than in non-positive retest patients. However, other symptoms were not significantly different between the two groups. The days from the onset of symptoms to admission were also not significantly different between the two groups. During the diagnostic procedure, 18 patients (13.1%) tested positive for the first nucleic acid test, 75 patients (54.78%) tested positive for the second nucleic acid test, and 44 patients (32.1%) tested positive for the third or above nucleic acid test, but there were no significant differences between positive retest patients and non-positive retest patients. Of the imported cases, 93 (67.8%) cases were diagnosed within 3 days, and another 44 (32.2%) were diagnosed 3 days later. Notably, the incidence of diagnosis within 3 days [23 (85.1%) vs 70 (63.6%); p=0.032] was higher in positive retest patients than in non-positive retest patients. In the treatment of patients, 81 patients (59.1%) received antiviral treatment, and 106 patients (77.4%) were taking Chinese medicine treatments. Moreover, no significant difference was observed between positive retest patients and non-positive retest patients in terms of treatment status or hospital stay during their first hospitalization. A comparison of clinical characteristics on the first admission between the COVID-19 patients who were virus non-positive and positive after discharge is shown in Table 2.
 |
Table 2 Comparison of Clinical Characteristics on the First Admission Between COVID-19 Patients with Non-Positive and Positive Retest Results After Discharge |
Laboratory and Chest CT Findings on the First Admission
Among laboratory indicators tested at admission, data revealed that positive retest patients had significantly lower percentages of neutrophils (54.1±5.6% vs 59.1±10.3%; p = 0.018), with significantly higher percentages of lymphocytes (34.25% ± 5.36% vs 30.2% ± 9.72%; p = 0.039) than non-positive retest patients. However, the neutrophil count (3.5×109/L ± 0.93 ×109/L vs 4.1×109/L ± 1.4×109/L; p = 0.06) and lymphocyte count (2.16×109/L ± 0.45 ×109/L vs 2.18×109/L ± 1.79×109/L; p = 0.963) were not significantly different between the 2 groups. Notably, other routine blood test findings were not significantly different between the two groups. Furthermore, no significant difference was observed for IgG and IgM antibody response in COVID-19 on the day of admission between the two groups. Initial lesion analysis of the chest by CT scan showed no difference in the extent of lesions between positive retest patients and non-positive retest patients. However, notably, the incidence of pure ground-glass opacities (GGOs) [5 (18.5%) vs 7 (6.3%); p = 0.045] was higher in positive retest patients than in non-positive retest patients. However, the incidence of GGOs with reticular and/or interlobular septal thickening and GGOs with consolidation or consolidation was not significantly different between the two groups. (Table 3).
 |
Table 3 Comparison of Laboratory Findings and Chest CT Findings on the First Admission Between the COVID-19 Patients with Non-Positive and Positive Retest Results After Discharge |
COVID-19 patients who met all of the hospital discharge criteria were recommended to stay in a medical centre with strict medical isolation for an additional 14 days. At the end of the quarantine, all patients were reviewed for routine blood test, IgG and IgM antibody responses in COVID-19, and chest CT. Notably, various indicators in routine blood test findings were not significantly different between positive retest patients and non-positive retest patients. Furthermore, no significant difference was observed for IgG and IgM antibody response in COVID-19 on the day of end of the quarantine between the two groups. There was also no significant difference in the changes in chest CT between the two groups. (Table 4).
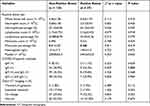 |
Table 4 Comparison of Laboratory Data and Chest CT Findings Between Non-Positive and Positive Retest COVID-19 Patients When Quarantine Ended |
Laboratory Findings of Positive Retest Patients at First Hospitalization and Readmission
To describe the clinical laboratory findings of positive retest cases at different stages, we analysed the routine blood, IgG and IgM antibody responses in positive retest COVID-19 patients. On the day of readmission, data revealed that readmission COVID-19 patients with SARS-CoV-2 repositivity had significantly lower percentages of neutrophils (54.1±5.6% vs 59.9±9.2%; p = 0.008) on readmission than on first hospitalization. However, neutrophil count (3.51×109/L ±0.94 ×109/L vs 4.08×109/L ±1.58×109/L; p = 0.109) was not significantly different between the 2 groups. Positive retest patients had significantly higher percentages of lymphocytes (34.25% ±5.36% vs 29.31% ±7.32%; p = 0.007) and higher lymphocyte counts (2.17×109/L ± 0.453 ×109/L vs 1.88×109/L ± 0.49×109/L; p = 0.031) on readmission than they had on first hospitalization. Notably, other routine blood test findings were not significantly different between the first hospitalization and readmission. Furthermore, no significant difference was observed for IgG and IgM antibody response in COVID-19 between the first hospitalization and readmission. (Table 5).
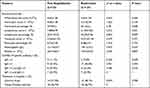 |
Table 5 Baseline Characteristics of Positive Retest Patients at First Hospitalization and Readmission |
Clinical Characteristics of Positive Retest Patients Upon Readmission
Considering the potential infectious risks of positive retest patients, all 27 positive retest patients were readmitted to the hospital for observation and treatment. Two patients (7.4%) complained of sore throat, and one patient complained (3.7%) of chest tightness. Another patient (3.7%) reported a slight stuffy nose on the second admission, which was previously observed and did not increase in severity. Twelve (44.5%) patients had asymptomatic infections. Two radiologists independently assessed the chest CT images of the positive retest patients. The images taken at readmission were compared to those taken at the first admission. Fourteen patients showed normal lung images with no signs of inflammation, 9 (33.3%) patients had no obvious changes in the lungs, 2 (7.2%) had sustained remission, and 2 (7.4%) patients had transient progression. No patient showed aggravated lung images. The clinical characteristics of positive retest patients upon readmission are shown in Table 6.
 |
Table 6 Clinical Characteristics of Positive Retest Patients on Readmission |
Discussion
This retrospective cohort study identified the clinical characteristics of positive retest COVID-19 patients in Xi’an Public Health Center Hospital. By systematically analysing the 137 foreign imported patients during hospitalization, quarantine and follow-up, we noticed that positive retest SARS-CoV-2 RNA detection accounted for 19.7% of recovered patients, which is close to most previous reports (15%–21%).16,17 Zou et al18 demonstrated that 20.6% of 257 individuals suffered from positive retest SARS-CoV-2 RNA detection after two consecutive negative RNA tests, and 5.4% of patients were identified after three negative detections. This is similar to recent studies on positive SARS-CoV-2 RNA detection.
In this study, we determined that the 137 imported COVID-19 patients were generally young, asymptomatic, and had no disease progression. We found that on the first admission, there was no significant difference in age, disease severity classification or initial symptoms (such as fever, cough and sore throat) between the repositive patients and the non-repositive patients. A recent study by Hong et al19 showed that the rate of rhinorrhoea was not significantly different between the positive retest and non-positive retest groups. Another study by Yi et al20 reported that there were only 2 COVID-19 patients with rhinorrhoea among the 184 patients, which was close to our study. In this study, although the rate of rhinorrhoea was higher in positive retest patients than in non-positive retest patients [2 (7.4%) vs 1 (0.9%); p = 0.039], few enrolled patients suffered from this initial symptom. Moreover, the study by Wong et al21 showed that patients who were positive for SARS-CoV-2 RNA did not show COVID-19 symptoms after discharge from the hospital. Meanwhile, in another study involving 123 patients who were positive again for SARS-CoV-2 RNA, there were virtually no related clinical symptoms after recovery, which may be related to the higher proportion of mild symptoms or asymptomatic patients at the initial episode.22 Consistent with previous findings, we also comprehensively characterized the clinical symptoms of redetectable positive RNA test patients when they were readmitted to the hospital. None of the positive patients had cough or fever on readmission. Only two patients complained of sore throat, and one patient complained of chest tightness. Another patient reported a slight stuffy nose on readmission, which was observed and did not increase in severity. These data indicated that although there was positive RNA detection for SARS-CoV-2, there was no obvious disease progression during readmission. In our study, continuous observations over time (before, during, or after positive retest patient detection) revealed improvements in imaging features in all positive patients and non-positive patients. The lung imaging reports for positive retest and non-positive retest patients showed no significant differences, which showed that sustained remission or no lesions in the lungs occurred between positive and non-positive retest patients. In addition, studies have also shown that upon readmission, positive retest patients’ chest CT findings showed no signs of deterioration compared with the previous scans.23 This indicates no obvious disease progression during readmission.
COVID‐19 is a systemic infection with the characteristics of haematopoietic system changes, and the laboratory data of imported patients were retrospectively analysed in our study. Lymphocytes are thought to be associated with viral infection. Previous studies suggested that decreased lymphocyte count was one of the most common laboratory abnormalities in COVID-19, and it was a predictive factor of severity and mortality.24–27 We found that there were significant differences in the neutrophil percentage and lymphocyte percentage between the positive retest patients and the non-positive retest patients on the first admission. Meanwhile, at the first hospitalization, the lymphocyte count and lymphocyte percentage of the positive retest patients were lower than those at readmission. We inferred that the difference in lymphocyte count between the first hospitalization and readmission may predict the decrease in severity among positive retest patients who recovered from COVID-19. However, our study differs from a previous study of 7 positive retest patients, which Yang et al28 revealed that there was no difference in lymphocyte count between the first hospitalization and readmission. Changes in the lymphocyte count are mainly observed in patients with virus infection, haemopathy and glucocorticoid therapy, and lymphocyte count is easily affected by factors such as the temperature of the environment and detection instrument. The limited sample size suggests that further validation is needed.
COVID-19 patients have comorbidities, including hypertension, diabetes, and cardiovascular disease, and are more likely to be transferred to the ICU.29 In our research, a majority of COVID-19 patients had hypertension and hepatic adipose infiltration, and a small proportion had diabetes mellitus, respiratory system diseases, and coronary heart disease. However, there was no significant difference in patients with regard to comorbidity between positive retest patients and non-positive retest patients. This result suggests that comorbidities such as hypertension, hepatic adipose infiltration, and diabetes may be related to the patient’s disease severity or prognosis but have little to do with the positive retest for SARS-CoV-2. In another study,30 it was also found no significant differences between positive retest patients and non-positive retest patients with regard to comorbidities, including hypertension, diabetes, and cardiovascular disease.
Although positive retest patients have been noticed and reported by multiple independent researchers10,31 and government authorities, including the Korean Centers for Disease Control and Prevention (CDC),32 there is a large controversy regarding the cause of returning positive episodes and the infectivity of positive retest patients. Because the positive retest patients were strictly quarantined at the medical centre in our study before readmission, we excluded positive retest patients reinfected with SARS-CoV-2. Therefore, we suspect that there are other reasons for the positive retest results. To the best of our knowledge, an accurate explanation for positive retests is lacking. In Singapore, the median duration of the loss of SARS-CoV-2 from nasopharyngeal aspirates was 24 days (median duration 12 days; range from 1 day to 24 days) after symptom onset, which may be related to the intermittent release of the virus from the respiratory tract leading to intermittently detected positive nucleic acid detection results.33 SARS-CoV-2 clearance characteristics in the bodies of patients are still not fully understood. There are several possible mechanisms, such as intermittent loss of SARS-CoV-2, viral distribution, intermittent dormancy period, residual viral presence, and false negatives during the initial discharge, to explain the existence of positive retest patients.31,33–35 However, in a study conducted in Hong Kong, researchers could not amplify active SARS-CoV-2 from samples of positive retest patients.36 Thus, it is also possible that the presence of positive retest cases was caused by broken SARS-CoV-2 fragments or dead SARS-CoV-2 particles that were not completely cleared in the body. Another study found that an intermittent, nonstable excretion of low-level viral RNA may result in positive retest occurrence rather than reinfection.31 A study in South Korea states that a repositive RNA test result for SARS-CoV-2 can only indicate that viral nucleic acid has been detected again but not that SARS-CoV-2 has caused reinfection or is reactivated.37 At the same time, some researchers believe that the low efficiency of throat swab and nasopharyngeal swab detection might result in the appearance of retest positivity.38 Positive retest results may be due to false-negative SARS-CoV-2 RNA test results at discharge.
Our study has some limitations. First, this study was a single-centre medical retrospective study based on a rather small cohort. The bias of the trial cannot be completely controlled, due to differences in SARS-CoV-2 RNA testing methods and the discharge criteria among different counties and cities. Larger samples and multicentre studies are necessary to further verify the findings in the present study. Second, respiratory specimens were collected from the patients in this study for nucleic acid detection according to the time period. The nucleic acid collection time points were the end of hospitalization, the end of isolation, and the end of follow-up. Nucleic acid was not collected every day. It is impossible to determine the specific viral shedding time and virus detection recovery time. The dynamics of SARS-CoV-2 RNA in COVID-19 patients need to be monitored and evaluated for positive retest. Last but not least, because our research is retrospective, we have not been able to detect the complete information of the virus whole genome sequencing and virus culture to verify the presence/absence of live virus and clarify the viral genome characteristics of positive retest patients. When the nucleic acid test is positive, it is impossible to determine whether there is an active virus in the respiratory tract and is unable to judge the infectivity of repositive patients. In future studies, we can use viral culture and rapid antigen test to assess the infectivity. Finally, due to the strict management of recovered patients after discharge, most recovered patients were identified as positive again during quarantine; consequently, they had few close contacts. Epidemiologic studies are needed to further confirm the transmission risk posed by positive retest patients.
Conclusions
In this study, it was found that demographic characteristics, medical comorbidities, initial symptoms, laboratory results, chest CT images and severity of the disease of patients at the time of initial diagnosis were not closely related to redetected positive RNA tests after recovery from foreign-imported COVID-19 cases. Positive retest patients had virtually no symptoms and displayed no obvious disease progression during readmission. These findings provide important information and clinical evidence for the effective management of foreign-imported COVID-19 patients during their convalescent phase.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi:10.1056/NEJMoa2001017
2. World Health Organization. WHO coronavirus (COVID-19) dashboard. Available from: https://covid19.who.int.
3. Parra LM, Cantero M, Morras I, et al. Hospital readmissions of discharged patients with COVID-19. Int J Gen Med. 2020;13:1359–1366. doi:10.2147/IJGM.S275775
4. Liu XH, Lu SH, Chen J, et al. Clinical characteristics of foreign-imported COVID-19 cases in Shanghai, China. Emerg Microbes Infect. 2020;9(1):1230–1232. doi:10.1080/22221751.2020.1766383
5. Leung K, Shum MH, Leung GM, Lam TT, Wu JT. Early transmissibility assessment of the N501Y mutant strains of SARS-CoV-2 in the United Kingdom, October to November 2020. Euro Surveill. 2021;26(1):2002106.
6. Tegally H, Wilkinson E, Giovanetti M, et al. Detection of a SARS-CoV-2 variant of concern in South Africa. Nature. 2021;592(7854):438–443. doi:10.1038/s41586-021-03402-9
7. Wells CR, Sah P, Moghadas SM, et al. Impact of international travel and border control measures on the global spread of the novel 2019 coronavirus outbreak. Proc Natl Acad Sci USA. 2020;117(13):7504–7509. doi:10.1073/pnas.2002616117
8. Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382(10):970–971. doi:10.1056/NEJMc2001468
9. Hoehl S, Rabenau H, Berger A, et al. Evidence of SARS-CoV-2 infection in returning travelers from Wuhan, China. N Engl J Med. 2020;382(13):1278–1280. doi:10.1056/NEJMc2001899
10. Lan L, Xu D, Ye G, et al. Positive RT-PCR test results in patients recovered from COVID-19. JAMA. 2020;323(15):1502–1503. doi:10.1001/jama.2020.2783
11. Yuan B, Liu HQ, Yang ZR, et al. Recurrence of positive SARS-CoV-2 viral RNA in recovered COVID-19 patients during medical isolation observation. Sci Rep. 2020;10(1):11887. doi:10.1038/s41598-020-68782-w
12. Huang K, Liu W, Zhou J, et al. Repositive RT-PCR test in discharged COVID-19 patients during medical isolation observation. Int J Med Sci. 2021;18(12):2545–2550. doi:10.7150/ijms.58766
13. Gao C, Zhu L, Jin CC, Tong YX, Xiao AT, Zhang S. Prevalence and impact factors of recurrent positive SARS-CoV-2 detection in 599 hospitalized COVID-19 patients. Clin Microbiol Infect. 2021;27(5):
14. An J, Liao X, Xiao T, et al. Clinical characteristics of recovered COVID-19 patients with re-detectable positive RNA test. Ann Transl Med. 2020;8(17):1084. doi:10.21037/atm-20-5602
15. Wei PF; National Health Commission & State Administration of Traditional Chinese Medicine. Diagnosis and treatment protocol for novel coronavirus pneumonia (8th ed). Chin Med J. 2021;133(9):1087–1095.
16. Xiao AT, Tong YX, Zhang S. False negative of RT-PCR and prolonged nucleic acid conversion in COVID-19: rather than recurrence. J Med Virol. 2020;92(10):1755–1756. doi:10.1002/jmv.25855
17. Xu K, Chen Y, Yuan J, et al. Factors associated with prolonged viral RNA shedding in patients with coronavirus disease 2019 (COVID-19). Clin Infect Dis. 2020;71(15):799–806. doi:10.1093/cid/ciaa351
18. Zou Y, Wang BR, Sun L, et al. The issue of recurrently positive patients who recovered from COVID-19 according to the current discharge criteria: investigation of patients from multiple medical institutions in Wuhan, China. J Infect Dis. 2020;222(11):1784–1788. doi:10.1093/infdis/jiaa301
19. Hong LX, Liu L, Lin A, Yan WH. Risk factors for SARS-CoV-2 re-positivity in COVID-19 patients after discharge. Int Immunopharmacol. 2021;95:107579. doi:10.1016/j.intimp.2021.107579
20. Yi W, Long X, Liu J, et al. Risk factors for recurrent positive results of the nucleic acid amplification test for COVID-19 patients: a retrospective study. Hum Cell. 2021;34(6):1744–1754. doi:10.1007/s13577-021-00618-9
21. Wong CL, Lei SK, Lei CI, Lo IL, Lam C, Leong IH. Re-positive of SARS-CoV-2 test is common in COVID-19 patients after hospital discharge. Data from high standard post-discharge quarantined patients in Macao SAR, China. PeerJ. 2021;9:e11170. doi:10.7717/peerj.11170
22. Váncsa S, Dembrovszky F, Farkas N, et al. Repeated SARS-CoV-2 positivity: analysis of 123 cases. Viruses. 2021;13(3):512. doi:10.3390/v13030512
23. Zhou J, Zhang J, Zhou J, et al. Clinical characteristics of re-positive COVID-19 patients in Huangshi, China: a retrospective cohort study. PLoS One. 2020;15(11):e0241896. doi:10.1371/journal.pone.0241896
24. Fu L, Wang B, Yuan T, et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: a systematic review and meta-analysis. J Infect. 2020;80(6):656–665. doi:10.1016/j.jinf.2020.03.041
25. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi:10.1016/S0140-6736(20)30183-5
26. Ziadi A, Hachimi A, Admou B, et al. Lymphopenia in critically ill COVID-19 patients: a predictor factor of severity and mortality. Int J Lab Hematol. 2021;43(1):e38–e40. doi:10.1111/ijlh.13351
27. Terpos E, Ntanasis-Stathopoulos I, Elalamy I, et al. Hematological findings and complications of COVID-19. Am J Hematol. 2020;95(7):834–847. doi:10.1002/ajh.25829
28. Yang Z, Chen X, Huang R, et al. Atypical presentations of coronavirus disease 2019 (COVID-19) from onset to readmission. BMC Infect Dis. 2021;21(1):127. doi:10.1186/s12879-020-05751-8
29. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi:10.1001/jama.2020.1585
30. Shi D, Wu W, Wang Q, et al. Clinical characteristics and factors associated with long-term viral excretion in patients with severe acute respiratory syndrome coronavirus 2 infection: a single-center 28-day study. J Infect Dis. 2020;222(6):910–918. doi:10.1093/infdis/jiaa388
31. Yang C, Jiang M, Wang X, et al. Viral RNA level, serum antibody responses, and transmission risk in recovered COVID-19 patients with recurrent positive SARS-CoV-2 RNA test results: a population-based observational cohort study. Emerg Microbes Infect. 2020;9(1):2368–2378. doi:10.1080/22221751.2020.1837018
32. Findings from investigation and analysis of re-positive cases. Available from: https://www.cdc.go.kr/board/boardes?mid=a30402000000&bid=0030.
33. Young BE, Ong SWX, Kalimuddin S, et al. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA. 2020;323(15):1488–1494. doi:10.1001/jama.2020.3204
34. Li D, Wang D, Dong J, et al. False-negative results of real-time reverse-transcriptase polymerase chain reaction for severe acute respiratory syndrome coronavirus 2: role of deep-learning-based CT diagnosis and insights from two cases. Korean J Radiol. 2020;21(4):505–508. doi:10.3348/kjr.2020.0146
35. Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. 2020;92(6):589–594. doi:10.1002/jmv.25725
36. Kang H, Wang Y, Tong Z, Liu X. Retest positive for SARS-CoV-2 RNA of “recovered” patients with COVID-19: persistence, sampling issues, or re-infection? J Med Virol. 2020;92(11):2263–2265. doi:10.1002/jmv.26114
37. Kang YJ. South Korea’s COVID-19 infection status: from the perspective of re-positive test results after viral clearance evidenced by negative test results. Disaster Med Public Health Prep. 2020;14(6):762–764. doi:10.1017/dmp.2020.168
38. Wang W, Xu Y, Gao R, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020;323(18):1843–1844. doi:10.1001/jama.2020.3786
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
