Back to Journals » Clinical Audit » Volume 7
Clinical audit of breast cancer care at the Benavides Cancer Institute, University of Santo Tomas Manila, Philippines: Part 1, methods and tools
Authors Sy Ortin T, Mejia M, Dizon J, Grimmer K, Gonzalez-Suarez C, Bacorro W, Co J, Caguioa P, Calma C, Regala E, Baldivia K, Yolo R, Morales K, Sanchez J, Malilay R, Tabangay-Lim IM, Que J, Bautista MJ
Received 29 November 2013
Accepted for publication 11 June 2014
Published 5 January 2015 Volume 2015:7 Pages 1—12
DOI https://doi.org/10.2147/CA.S58482
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Teresa T Sy-Ortin,1 Michael Benedict A Mejia,1 Janine Margarita Dizon,1–3 Karen Grimmer,2 Consuelo Gonzalez-Suarez,2,3 Warren Bacorro,1 Jayson Co,1 Priscilla Caguioa,4 Clevelinda Calma,4 Eugenio Regala,4 Kathleen Baldivia,1 Rowen Yolo,5 Karl Morales,6 Josefino Sanchez,6 Ray Malilay,6 Ida Marie Tabangay-Lim,6 Jocelyn C Que,7,8 Mary Jocylyn Bautista7
1Department of Radiation Oncology, Benavides Cancer Institute, University of Santo Tomas Hospital, Espana, Manila, Philippines; 2International Centre for Allied Health Evidence, University of South Australia, Adelaide, SA, Australia; 3Centre for Health Research and Movement Science, University of Santo Tomas, Espana, Manila, Philippines; 4Section of Medical Oncology, Department of Medicine, University of Santo Tomas Hospital, Espana, Manila, Philippines; 5Department of Pathology, University of Santo Tomas Hospital, Espana, Manila, Philippines; 6Department of Surgery, University of Santo Tomas Hospital, Espana, Manila, Philippines; 7Pain Management and Palliative Care Unit, Benavides Cancer Institute, University of Santo Tomas Hospital, Espana, Manila, Philippines; 8Center for Pain Medicine, Faculty of Medicine and Surgery, University of Santo Tomas, Espana, Manila, Philippines
On behalf of the Benavides Cancer Institute Breast Cancer Working Group (BCIBC-WG)
Background: The prevalence and incidence of breast cancer has been increasing worldwide. It has been reported that the Philippines has the highest number of cases in Asia, and breast cancer is now the leading cause of death in the country. This study protocol presents the methodological plan for a quality improvement study that will assess the current practice of breast cancer examination, diagnosis, and management at one of the leading cancer institutions in the Philippines, the University of Santo Tomas Hospital-Benavides Cancer Institute (USTH-BCI); and map with standards of care, in order to identify areas that would need improvement to facilitate best practice care for breast cancer patients.
Methods: This study has been approved by the Institutional Review Board of the University of Santo Tomas Hospital. A breast cancer working group has been established (Benavides Cancer Institute Breast Cancer Working Group [BCIBC-WG]) during a 1 day meeting of cancer specialists at USTH-BCI. The meeting was facilitated by both international and local methodologists in the field of evidence-based practice and quality improvement. A quality improvement plan and a clinical audit protocol for assessing current practice were drafted during this meeting. The clinical audit of current breast cancer care will be undertaken at USTH-BCI using medical records review. Clinical indicators of outcomes were identified and typical patient journeys were mapped to develop the data collection/extraction form. The data collection forms were sent to experts for face and content validation, to ensure a valid and comprehensive collection of the data. The form was revised as needed. Three hundred and eighteen (318) breast cancer cases were seen at USTH-BCI in the year 2012, and all 318 records will be reviewed as decided by the group. A reliability procedure will be undertaken among data collectors of the study and pilot testing procedure will be undertaken to test the feasibility of the data collection methods. Data will be analyzed and reported using means and percentages as appropriate. Missing data will also be reported in order to identify strategies to ensure completeness of medical records in the future.
Keywords: breast cancer, audit, quality improvement, developing countries, protocol
Background
The increasing prevalence and incidence of cancer worldwide is alarming. In the United States alone, the prevalence of cancer in 2011 was 12,549,000.1 In less developed countries, the incidence of cancer is projected to increase from 56% of world cases in 2008 to greater than 60% by 2030. Cancer is also the leading cause of death globally. The World Health Organization reports that the number of deaths due to cancer is projected to increase by 45% from 2007 to 2030 (from 7.9 million to 11.5 million deaths).2
With the alarming increase in the prevalence and incidence of cancer and the rate of mortality due to cancer worldwide, much research has been done on identification of risk factors, prevention and management. Such that, with advancements in medical science research, one third of cases can now be prevented, one third can be diagnosed early and thus managed early, and one third can be treated.3 However, this is only possible if management and treatment provided are consistent with evidence-based standards of cancer care.3
In the Philippines, cancer was one of the leading causes of morbidity and mortality in 2002: the leading cancer types are lung, breast, cervix, liver and colon.4 More recently, the Philippines’ Department of Health and the Philippine Cancer Society have reported that breast cancer is now the leading cancer type in the country and accounts for the highest incidence rate in Asia.5 Thus, the Philippines’ Department of Health, in partnership with the Philippine Cancer Society has developed programs in relation to screening, prevention, and management of cancer.6 Programs such as free screening, medicines for poor women diagnosed early with breast cancer, and the “Z Benefit Package of PhilHealth” were developed and implemented to address the alarming increase in breast cancer morbidity and mortality.6
The University of Santo Tomas Hospital (USTH), one of the leading private health institutions in the Philippines, established the Benavides Cancer Institute (BCI) in 2006. The mission of the USTH-BCI is to strengthen the national cancer care program and provide comprehensive and multidisciplinary cancer care for diagnosis, treatment and prevention.7 Consistent with its mission, the USTH-BCI is continuously planning and strategizing ways to identify and deliver the best cancer care in the Philippines.
As medical science research has reported that cancer can be prevented, diagnosed early, and treated if care management and treatment programs are consistent with evidence-based guidelines, the USTH-BCI developed a research project that will assess current practice and then map current practice with existing evidence-based guidelines for breast cancer care such as the National Comprehensive Cancer Network (NCCN) Guidelines for breast cancer.8 USTH-BCI agreed to use the NCCN guidelines,3 as standard of care to underpin health care provided to patients. However, it is not known whether the standards of care are being adhered to or complied with by all health professionals involved in the care of breast cancer patients. There is much discussion in the literature regarding the availability of evidence-based standards of care and the existing gap in compliance with the standards.9–11 For instance, whilst guideline adherence was associated with improved survival, one study reports that guideline adherence was low for patients with triple negative breast cancer.9 Another one reports less than half of women with breast cancer completed the recommended therapy.12 Thus, it is very important to assess whether existing practice follows the recommended standards, and then later, plan for strategies that would address the gaps and plan for sustainable efforts in the long term to improve clinical outcomes of care.
This may be an ambitious project but it could be a milestone in clinical practice and health care as this is the first attempt to evaluate current practices in breast cancer care in the Philippines. This is valuable because identifying current practices allows: 1) identification of relevant data items to be used as basis for assessing breast cancer care delivery; 2) identification of gaps which are useful in identifying areas which need improvement; 3) opportunities for better patient outcomes and better utilization of resources, especially in developing countries, such as the Philippines, with limited resources and lastly; 4) change and improve health policies in order to standardize health services and improve the health system, thus, championing best breast cancer care in the Philippines.13,14
Objectives
This study protocol presents the methods for undertaking a quality improvement project that will describe the current practice of breast cancer examination, diagnosis, and management at the USTH-BCI, and map whether current practice is consistent with evidence based standard of care.
Methods
Ethics
Ethical approval was obtained from the Institutional Review Board of the USTH, Manila, Philippines.
Study design and setting
A clinical audit study using medical record review will be undertaken to address the study objectives. The clinical audit will be undertaken at the USTH-BCI.
Reference population
Patients with breast cancer seen at USTH-BCI can come from any of the following:
- Patients in the clinical division of the USTH and referred to BCI for screening/evaluation, diagnosis/staging and treatment and management
- Patients seen by a medical doctor within USTH and referred to BCI for diagnosis/staging and then for treatment and management
- Patients diagnosed elsewhere in the Philippines and referred for breast cancer treatment and management from other institutions in the Philippines.
Sampling method and sample size
A total of 318 patients with breast cancer were seen at BCI for the year 2012. As 318 is a manageable number of breast cancer patient cases, the group decided to consider all these cases for inclusion in the audit, thus using census sampling. This will allow 100% statistical power and accuracy in describing the current practice in different categories of breast cancer care provided by BCI.15
Working group
The clinical audit proposal was formulated by the BCI Breast Cancer Working Group (BCIBC-WG) consisting of key health care personnel involved in breast cancer care at USTH-BCI (Teresa SyOrtin, MD, chair of BCI; Priscilla B Caguioa, MD; Clevelinda Calma, MD; Eugene Regala, MD; Kathleen Baldivia, MD; Rowen Yolo, MD; Michael A Mejia, MD; Karl Morales, MD; Josefino Sanchez, MD; Ray Malilay, MD; Ida Marie Tabangay-Lim, MD; Jocelyn Que, MD; Joycylyn Bautista, MD; Warren Bacorro, MD; and Jayson L Co, MD; and methodologists in the area of quality improvement and evidence based practice, (JRD, the project leader; KG, an external collaborator; and CGS, a local evidence based practice [EBP] champion). The BCIBC-WG held a 1 day meeting on quality improvements and audits, role of clinical guidelines in improving quality of health care services, and planning the quality improvement proposal of BCI.
Identification of patient journeys
In order to identify the current practices in breast cancer care at BCI a typical patient journey was identified by the BCIBC-WG. Patient journeys are visualizations of the usual flow of relevant processes a patient undergoes when seen in the facility.16 A copy of the patient journey was then sent to other health care personnel involved in breast cancer care for validation of the processes. Thus, the patient journey presented in Figure 1 has been validated by all involved in breast cancer care at BCI and will be the basis of this clinical audit.
Audit data items
The BCIBC-WG has identified an agreed list of items to be included in the clinical audit to obtain a comprehensive profile of breast cancer care at BCI (Tables 1–3).
Data collection methods
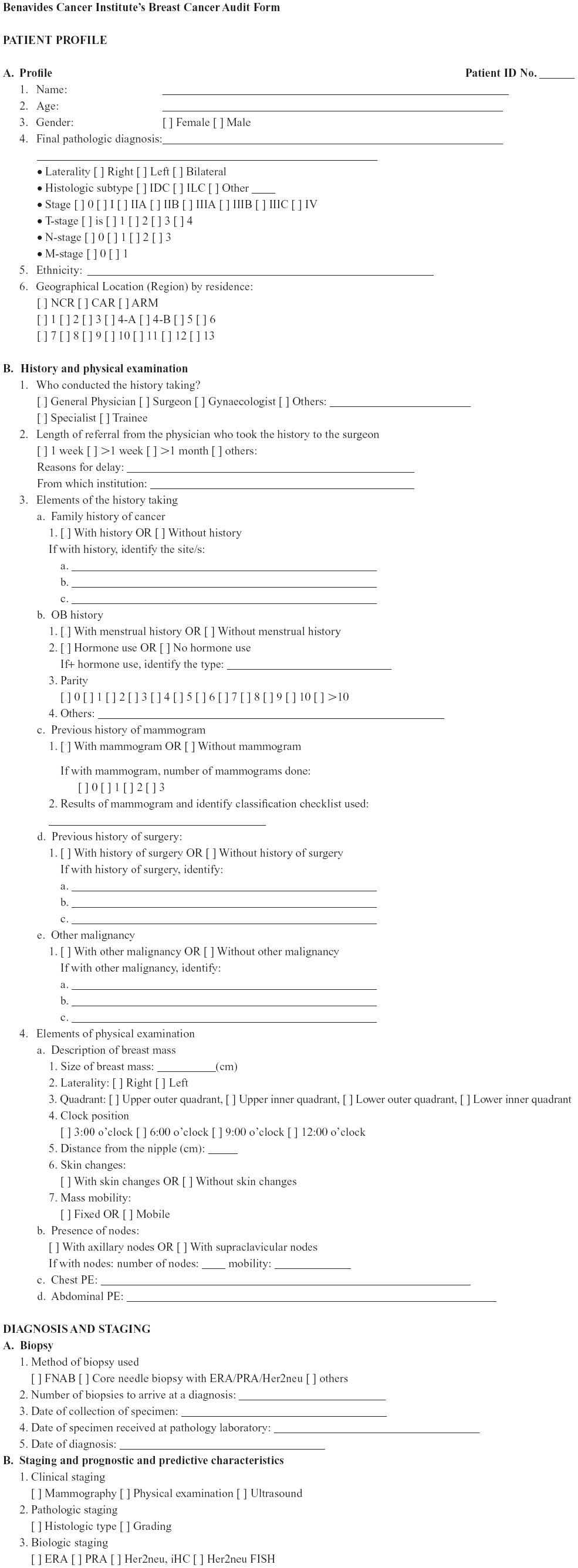
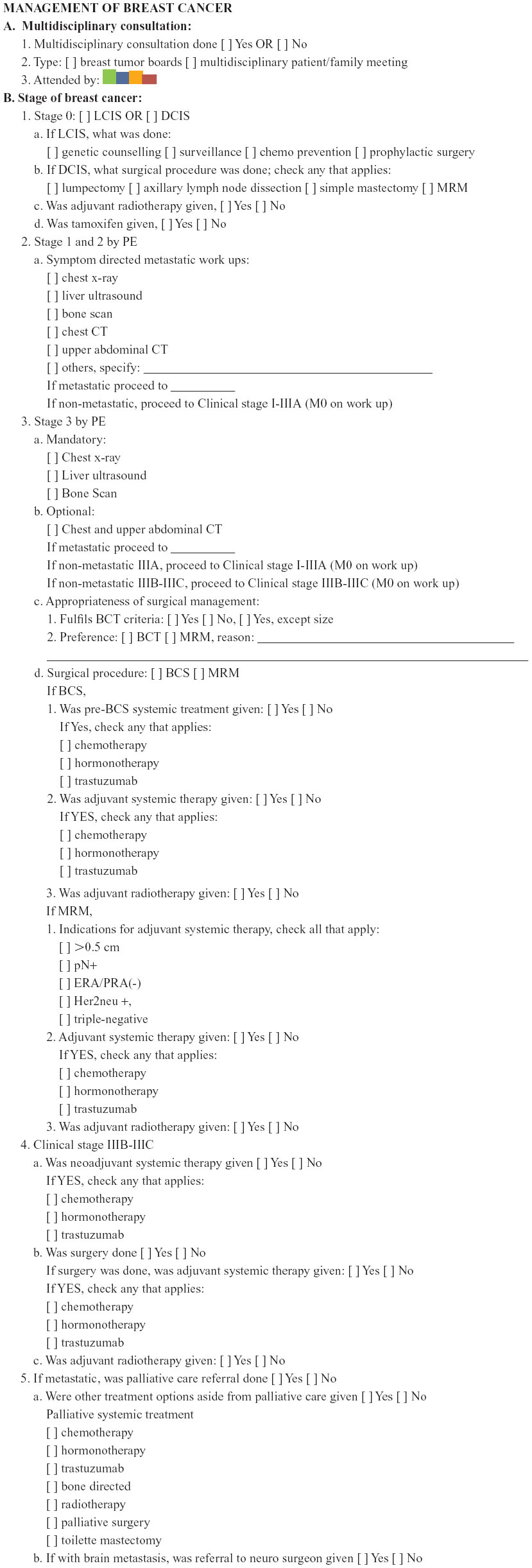
Data collection tool
A standard data collection form (Supplementary materials) will be used to retrieve the relevant audit items from the patients’ medical records. This form includes information from patient demographics, history and physical examination, diagnosis/stages of breast cancer and management for breast cancer patients. Consent from the attending physicians will be obtained.
Validity of the data collection tool
The data collection form was sent to experts (surgeon, a medical oncologist and a pathologist) and comments were discussed in a meeting for face and content validation. This was to ensure that the data audit items to be retrieved from the medical records will answer the clinical audit objectives. Revisions were undertaken based on the validation procedure and sent back to the experts for approval.
Pilot testing the audit data collection process
The clinical audit data collection will be pilot tested to ensure validity and reliability of the procedures.15,17 More specifically, the purposes of the pilot testing are as follows:
- Test feasibility of the data collection methods
- Estimate the amount of time and resources required to collect data
- Check data for completeness.
Data collectors
Two to three data collectors will be identified to retrieve the audit items from the medical records. They should have experience in data recording or management to ensure ability to reliably extract the information needed. An orientation to the clinical audit project and training for data collection will be conducted with the data collectors. A reliability procedure will also be undertaken by asking the data collectors to complete data extraction of five sample cases independently. The inter-rater reliability for percentage of agreement recommended by Dixon and Pearce will be used to compute the reliability of the data collectors.15 This is done by dividing the number of bits of data for which there was complete agreement among the data collectors and the total number of bits of data (for example, 25 bits of data per case ×5 cases). Further training will be provided as needed based on the results of the reliability procedure.
Data handling
A purpose built MSExcel file will be constructed, which restricts the type of data which can be entered into each column. This will reduce data entry errors and ensure efficiency of data amalgamation. All patient cases to be included in the clinical audit will be provided with a code. This code will be used and entered as the patient case in the MSExcel file including all audit items retrieved from the patient medical records.
Auditing guidelines
Table 4 lists the quality indicators that will be used later to evaluate the outcome of current practice (relevant items extracted from the European Society of Breast Cancer Specialists Quality indicators in breast cancer position paper by Del Turco et al).18
Data analysis
This will be undertaken by an independent statistician. Data will be reported using means and percentages as appropriate. Missing data will also be reported in order to identify strategies to ensure completeness of medical records in the future particularly when assessing adherence to guidelines.
Confidentiality
All data to be obtained from the medical records shall be kept confidential and will only be available to the working group.
Disclosure
The authors have no conflicts of interest to declare.
References
Howlader N, Noone AM, Krapcho M, et al. SEER cancer statistics review, 1975–2009 (vintage 2009 populations). Bethesda, MD: National Cancer Institute (2012). | |
World Health Organization [homepage on the Internet]. Available from http://www.who.int/features/qa/15/en/index.html. Accessed April 17, 2013. | |
World Health Organization [homepage on the Internet]. Available from http://www.who.int/mediacentre/factsheets/fs297/en/index.html. Accessed April 17, 2013. | |
Ngelangel C, Wang E. Cancer and the Philippine Cancer Control Program. J JClin Oncol. 2002;32(1):S52–S61. | |
Philippine Council for Health Research and Development. The ABCs of breast cancer. [webpage on the Internet]. Available from http://www.pchrd.dost.gov.ph/index.php/2012-05-23-07-46-36/2012-05-24-00-03-06/5689-the-abcs-of-breast-cancer. Accessed April 17, 2013. | |
Philippines’ Department of Health. Available from http://www.philhealth.gov.ph/news/2013/zbenefits_saves.html. Accessed April 20, 2013. | |
The Varsitarian. Available from http://www.varsitarian.net/news/cancer_institute_launched. Accessed April 20, 2013. | |
National Comprehensive Cancer Network guidelines for treatment of breast cancer. Available from https://www.nccn.org/store/login/login.aspx?ReturnURL=http://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed May 30, 2014. | |
Schwentner L, Wöckel A, König, et al, for the Brenda study group. Adherence to treatment guidelines and survival in triple-negative breast cancer: a retrospective multi-center cohort study with 9156 patients. BMC Cancer. 2013;13:487. | |
Chagpar R, Xing Y, Chiang Y, Feig W, Chang G, You N, et al. Adherence to stage-specific treatment guidelines for patients with colon cancer. J Clin Oncology. 2012;30(9):972–979. | |
Barni S, Venturini M, Molino A, et al. Importance of adherence to guidelines in breast cancer clinical practice. The Italian experience (AIOM). Tumori. 2011;97:559–563. | |
Hershman D, Kushi L, Shao T, et al. Early discontinuation and nonadherence to adjuvant hormonal yherapy in a cohort of 8,769 early-stage breast cancer patients. J Clin Oncology. 2010;28(27):4120–4128. | |
Wensing M, van der Weijden T, Grol R. Implementing guidelines and innovations in general practice: which interventions are effective? Brit J Gen Pract. 1998;48:991–997. | |
Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients’ care. The Lancet. 2003;362: 1225–1230. | |
Dixon N, Pearce M. Clinical Audit Manual. Romsey: Healthcare Quality Quest Ltd; 2010. | |
National Health Survey. Available from http://www.institute.nhs.uk/quality_and_service_improvement_tools/quality_and_service_improvement_tools/process_mapping_-_an_overview.html Accessed April 23, 2013. | |
Banks NJ. Designing medical record abstraction forms. Int J Qual Health Care. 1998;10(2):163–167. | |
Del Turco M, Ponti A, Bick U, et al. Quality Indicators in breast cancer care. Eur J Cancer. 2010:2344–2356. |
Supplementary material
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.






