Back to Journals » International Journal of Women's Health » Volume 13
Clinical Application of Noninvasive Prenatal Testing for Pregnant Women with Assisted Reproductive Pregnancy
Authors Jin XX, Xu YF, Ying X, Qian YQ, Jin PZ, Dong MY
Received 1 September 2021
Accepted for publication 18 November 2021
Published 30 November 2021 Volume 2021:13 Pages 1167—1174
DOI https://doi.org/10.2147/IJWH.S337249
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Xiao-Xiao Jin,1,2 Yan-Fei Xu,2 Xiang Ying,1 Ye-Qing Qian,2 Peng-Zhen Jin,2 Min-Yue Dong2
1Prenatal Diagnosis Center of Taizhou Hospital, Wenzhou Medical University, Taizhou, 317000, People’s Republic of China; 2Key Laboratory of Reproductive Genetics, Ministry of Education, Department of Reproductive Genetics, Women’s Hospital, Zhejiang University School of Medicine, Hangzhou, 310006, People’s Republic of China
Correspondence: Min-Yue Dong
Department of Reproductive Genetics, Women’s Hospital, Zhejiang University School of Medicine, Hangzhou, 310006, People’s Republic of China
Tel +86 18957100183
Fax +86-571-87061878
Email [email protected]
Objective: This paper analyzes the clinical significance of noninvasive prenatal testing (NIPT) for fetal chromosome aneuploidy in the screening of in vitro fertilization–embryo transfer (IVF) pregnancies.
Methods: The study subjects consisted of 3163 IVF-pregnant women who underwent NIPT at the Women’s Hospital, School of Medicine, Zhejiang University and Taizhou Hospital, Zhejiang Province from February 2015 to June 2019. Fetal or neonatal karyotype analysis was carried out in high-risk patients, with subsequent follow-up on pregnancy outcomes.
Results: NIPT results of 3163 pregnant women suggested 20 cases of high-risk fetal chromosome aneuploidy, of which 2185 cases were a single pregnancy. Of the 13 cases of high-risk chromosome aneuploidy in single pregnancies, seven were true positive, and six were false positive according to fetal or newborn chromosomal karyotype diagnosis. Twin pregnancies accounted for 978 cases in which NIPT indicated seven cases of high-risk chromosome aneuploidy; six of these cases were true positive, and one case was false positive according to fetal or newborn chromosomal karyotype diagnosis. The specificity, positive predictive value, and false-positive rate of trisomy 21 syndrome in IVF single embryo NIPT were 99.86%, 62.5%, and 0.14%, respectively. The specificity, positive predictive value, and false-positive rate of trisomy 18 syndrome were 99.95%, 66.67%, and 0.05%, respectively. The specificity of trisomy 13 syndrome was 99.91%, and the false-positive rate was 0.09%. The specificity of trisomy 21 syndrome in IVF twin NIPT was 99.89%, the positive predictive value was 83.33%, and the false-positive rate was 0.11%. The specificity and positive predictive value of fetal trisomy 18 syndrome were 100.00%, and the false-positive rate of it were 0.00%. Sensitivity and false-negative rates were 100% in all cases.
Conclusion: NIPT is an ideal prenatal test for IVF-pregnant women due to its high sensitivity and specificity in screening for fetal aneuploidy.
Keywords: in vitro fertilization–embryo transfer, pregnancy, noninvasive prenatal testing, chromosome, aneuploidy, amniotic fluid
Introduction
With changes in work–life rhythms and the social environment, the incidence of infertility is increasing year by year, and the current global incidence of infertility is thought to be as high as 15–20%.1 Results from a large sample study in China show that among 10,742 women who tried to get pregnant, the prevalence of infertility was 25%.2 In recent years, in vitro fertilization and embryo transfer (IVF–ET) technology in China has developed considerably, in clinical practice to explore the appropriate ovulation promotion program and more accurate screening of infertility causes, the success rate for infertile couples using IVF for pregnancy is increasing. IVF-pregnant women of more advanced age have significantly higher rates of twin pregnancies than those occurring in natural pregnancy.1,3 Due to the influence of internal and external factors, women aged ≥35 years tend to experience ovarian aging, and the incidence of nonsegregation during meiosis increases. Therefore, advanced age is a high-risk factor for chromosomal disease.4 In 2011, guidelines published by the Society of Obstetricians and Gynecologists of Canada and the Canadian College of Medical Genetics recommended mid-trimester serological screening combined with nuchal translucency (NT) thickness testing as one of the options for the prenatal screening of twin pregnancies. However, a serological screening study of a large sample of women in the second trimester, which included 11,040 cases of twin pregnancy, shows this method to be far from ideal. While the detection rate of trisomy 21 was 71%, the false-positive rate was as high as 10.8%.5 Due to a lack of supportive data, serological screening in the second trimester is not recommended for twin pregnancies in China. In addition, births following IVF pregnancy are precious, and pregnant women and their families are often concerned about the risk of interventional prenatal diagnosis, so their compliance is low. Invasive prenatal diagnosis can cause intrauterine infection, abortion infection and other risks, which also reduces patients’ compliance with invasive prenatal diagnosis.6 Therefore, it is necessary to find an efficient, reliable, and economical method of prenatal pregnancy screening for use following assisted reproduction.
Clinically, noninvasive prenatal testing (NIPT) based on high-throughput sequencing is mainly used to screen trisomy 13, 18, and 21 syndromes. This valuable prenatal screening technology demonstrates high sensitivity and specificity and is increasingly widely used. However, there have been some doubts about its detection efficiency when used in IVF pregnancy, and, in 2016, the National Health and Family Planning Commission of the People’s Republic of China urged caution when using NIPT in assisted fertility pregnancies. To evaluate the efficiency of NIPT detection in pregnant women with assisted reproduction, we analyze the NIPT results of 3163 women with IVF pregnancies and perform prenatal diagnosis and subsequent follow-up on high-risk pregnant women to investigate the clinical significance of NIPT in the prenatal screening of fetal chromosome aneuploidy during IVF pregnancy.
Materials and Methods
Research Objects
The study consisted of 3163 IVF-pregnant women who underwent NIPT at the Women’s Hospital, School of Medicine, Zhejiang University and Taizhou Hospital, Zhejiang Province, from February 2015 to June 2019. The inclusion criteria for the study were as follows: ① women who were pregnant following IVF, ② a gestational age of 12–26+6 weeks, ③ a live intrauterine fetus with B-ultrasound prior to examination, and ④ subsequent completion of labor and clinical follow-up. Cases that may substantially affect the accuracy of the results were excluded according to the 2016 “Technical specification for prenatal screening and diagnosis of fetal-free DNA in maternal peripheral blood,” published by the National Health and Family Planning Commission of the People’s Republic of China.7
Among them, 1248 cases (39.46%) were senior pregnant women (aged 35 years or above at the expected date of confinement), 2185 cases (69.08%) were single pregnancies, and 978 cases (30.92%) were twin pregnancies. The gestational age of the pregnant women was calculated according to menstrual cycle history and early pregnancy ultrasound prior to NIPT. In addition, the women’s medical history was rechecked to exclude any structural abnormalities or family history of hereditary diseases indicated by allogeneic blood transfusion, transplantation, allogeneic cell therapy, or fetal imaging examination within the past year. Peripheral blood was then collected voluntarily after obtaining informed consent.
After NIPT was performed on all women in the study, amniotic fluid chromosome karyotype analysis was recommended for those subjects deemed high risk. Three high-risk women refused amniotic fluid puncture, and so peripheral blood examination of their newborns was performed following delivery.
Peripheral Blood Noninvasive Prenatal Testing
NIPT was performed at 12–26+6 weeks of gestation using a semiconductor sequencing platform (BioelectronSeq 4000), with an average effective read number of 3.5M and an average genome coverage of 0.25x.8 The test kits were provided by Guangzhou Biotechnology Co., Ltd. A 5 mL sample of maternal venous peripheral blood was extracted and placed in an anticoagulant tube containing EDTA. The sample underwent 1600 × g centrifugation for 10 minutes at 4°C to separate the plasma. Cell-free fetal DNA was then extracted using the QIAamp DSP DNA Blood Mini Kit (Qiagen) and stored at –80°C. To construct a DNA library for sequencing, Ion Plus Fragment Library Kit V3, Ion Plus Fragment Library Adapters Kit (Life Technologies, USA), and AMPure XP beads were used. Twelve library samples of 100 pM were mixed and loaded onto Ion PI™ Chip v2, following enrichment with the Ion One Touch™ 2 Instrument (Life Technologies, USA). The Ion P1 HI-Q200 V3 Kit (Life Technologies, USA) was then used for machine sequencing on a semiconductor sequencing platform. Samples with effective read numbers less than 2.5M or an absolute Z-value of less than 1.96–3 were reconstructed. Z-values between –3 and 3 (Z ≥ 3 or Z ≤ −3) were deemed to indicate high risk, and further prenatal diagnosis was recommended.
Karyotype Analysis of Amniotic Fluid Cell Culture by Amniocentesis
For those at a high risk of fetal trisomy 13, 18, or 21 syndromes as indicated by NIPT, interventional prenatal diagnosis was made following genetic counseling and informed consent. Amniocentesis was carried out using ultrasound, and cell culture was performed in accordance with prenatal diagnostic procedures. After centrifugation, the samples were inoculated in 50 mL culture bottles containing Ham’s F10 (Hangzhou Biosan, Inc.). The fluid was changed every six days and harvested when the number of cell colonies exceeded 15. For late gestational specimens, the fluid was changed again and the culture prolonged if the number of cell colonies was insufficient for harvest at day 12. Following colchicine treatment, digestion, hypotension, fixation, and banding, karyotype analysis was performed according to the interpretation standard ISCN 2016.9 Pregnant women without interventional prenatal diagnosis underwent neonatal chromosome karyotype testing instead immediately after delivery.
Follow-Up After Delivery
Follow-up of all study participants was completed after delivery and included both information taken at the time of delivery and from subsequent phone calls completed by the Taizhou Maternal and Child Information Platform. The follow-up information included data on delivery outcomes (ie, survival, induced labor, or abortion), neonatological care, and the presence or absence of birth defects.
Statistical Analysis
SPSS 20.0 statistical software was used to process the data. Data were expressed in terms of the number of cases and percentages (%). Sensitivity was calculated as true-positive number/(true-positive number + false-negative number) x 100%; specificity was calculated as true-negative number/true-negative number + false-positive number) x 100%; the positive predictive value was calculated as true-positive number/(true-positive number + false-positive number); the negative predictive value was calculated as true-negative number/true-negative number + false-negative number) x 100%; and the false positive rate was calculated as false-positive number/gold standard negative number x100%.
Results
Amniotic Fluid Chromosome Karyotype Analysis and Pregnancy Outcomes in High-Risk Pregnant Women
Among 3163 IVF-pregnant women, 20 cases (0.63%) were identified as being at high risk of fetal chromosome aneuploidy. Of these, 13 were single fetuses, and 7 were twin fetuses (all of which were bichorionic). Fourteen cases were identified as being at high risk of trisomy 21, of which eight were single fetuses, and six were twin fetuses. Thirteen cases of amniotic fluid karyotype analysis were performed, and 10 cases of trisomy were found in five single and five twin fetuses. Five women underwent induction of abortion, and another five women who were pregnant with twins underwent a single live birth following selective abortion reduction. The newborn of one high-risk pregnant woman who refused prenatal diagnosis was confirmed to have a normal chromosome type by peripheral blood examination after birth. In three cases (two single and one twin), no abnormality was observed from amniotic fluid karyotype analysis, and this was confirmed by neonatal physical examination and follow-up after birth. No abnormality was found in one case of amniotic fluid chromosome. The amniotic fluid karyotype of one patient is trisomy 18 induced labor. One case was induced due to multiple fetal malformations observed during the B-ultrasound and was confirmed to be trisomy 18 by amniotic fluid analysis performed during the induction. One fetus died following cesarean section, and trisomy 18 was confirmed by neonatal peripheral blood examination. The other newborn was healthy and survived, and no abnormality in growth and development was reported during telephone follow-up. Two single fetuses were identified as being at high risk of trisomy 13, but no abnormal findings were found in the post-birth neonatal physical examinations or subsequent follow-up (Tables 1 and 2).
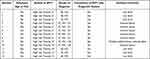 |
Table 1 Aneuploidy Prenatal Screening Results and Delivery Outcomes of 13 Cases of Non-Invasive Prenatal Screening High-Risk Single Fetus Pregnancy Women |
 |
Table 2 Aneuploidy Prenatal Screening Results and Delivery Outcomes of 7 Cases of Non-Invasive Prenatal Screening High-Risk Twins Pregnancy Women |
Follow-Up of Pregnancy Outcomes in Low-Risk Pregnant Women
Of the 3143 low-risk pregnant women in the study, follow-up was conducted with 3059 after delivery, and no false-negative newborns were found. Eighty-four cases (58 single and 26 twin births) were lost to follow-up, a rate of 2.66%. There were 2940 live births, which totaled 3827 newborns. Five instances of birth defects were diagnosed through neonatal physical and health examinations and telephone follow-ups, including one case of hypospadias, one case of auricle malformation, two cases of syndactyly, and one case of congenital heart disease. No testing was performed, nor visual differences observed, in these five children at birth. One hundred nineteen cases did not result in a live birth. There were 45 cases of mid-trimester abortion, 54 cases of induced labor, 18 cases of fetal death, and 2 cases of stillbirth. All cases of mid-term abortion were caused by premature rupture of membranes. In the case of fetal death, umbilical cord factors were responsible in eight cases, placental abruption in three cases, preeclampsia in two cases, placenta previa hemorrhage in one case, and unknown causes for the other four cases. The two stillbirths were caused by severe asphyxia during delivery, and fetal tissue examination in these cases showed no obvious abnormality. No abnormality was found in the B-ultrasound examination during pregnancy, and no unusual facial appearance was observed after birth. Other deceased fetuses also showed no obvious visual abnormalities after delivery. Fetal sex chromosome abnormality induced labor in 12 cases; there were four cases each of 45, X, 47, XXX, and 47, XXY. Fetal malformation induced labor in a further 42 cases, which B-ultrasound diagnosed during pregnancy. Conditions included spina bifida (two cases), limb abnormalities (two cases), facial deformity (two cases), megabladder (one case), microcephaly (two cases), non-formation of the eyeball (one case), cardiac malformation (eighteen cases), anencephalus (two cases), hydrocephalus (four cases), early-onset fetal growth restriction (two cases), edema (one case), and digestive tract malformation (five cases). After obtaining informed consent, amniotic fluid puncture karyotype or fetal tissue examinations were performed in 27 of these cases across a range of conditions. However, no fetal chromosomal abnormality was observed. Of the other 15 cases, which did not undergo chromosome examination following induced labor, none showed visual facial indicators of trisomy 13, 18, or 21 syndromes.
Inspection Efficiency of NIPT in Diagnosing Aneuploidy in IVF Conceived Fetuses
Chromosome aneuploidy was detected by NIPT with a sensitivity of 100.00%, a specificity of 99.77%, a positive predictive value of 65%, a false-positive rate of 0.23%, and a negative predictive value of 100%. For IVF single fetus pregnancies, these values were 100.00%, 99.72%, 53.85%, 0.28%, and 100%, respectively, and for IVF twin fetus pregnancies they were 100.00%, 99.89%, 85.71%, 0.11%, and 100%, respectively. Trisomy 21 syndrome was detected by NIPT with a sensitivity of 100.00%, a specificity of 99.87%, a positive predictive value of 71.43%, a false-positive rate of 0.13%, and a negative predictive value of 100%. For IVF single fetus pregnancies, these values were 100.00%, 99.86%, 62.50%, 0.14%, and 100%, respectively, and for IVF twin fetus pregnancies they were 100.00%, 99.89%, 83.33%, 0.11%, and 100%, respectively. Trisomy 18 syndrome was detected by NIPT with a sensitivity of 100.00%, a specificity of 99.97%, a positive predictive value of 75.00%, a false-positive rate of 0.03%, and a negative predictive value of 100%. For IVF single fetus pregnancies, these values were 100.00%, 99.95%, 66.67%, 0.05%, and 100%, respectively. For IVF twin fetus pregnancies, the sensitivity of trisomy 18 detection was 100.00%, the specificity was 99.95%, the positive predictive value was 100.00%, and the negative predictive value was 100%. The specificity of trisomy 13 was 99.94%, and the false-positive rate was 0.06%. In IVF single fetus pregnancies, the specificity of trisomy 13 was 99.91%, with a false positive rate of 0.09% (Tables 3 and 4).
 |
Table 3 Efficiency of NIPT in Detecting Aneuploidy of IVF Conceived Fetus |
 |
Table 4 Efficiency of NIPT for Trisomy 21/18/13 in IVF Conceived Fetuses |
Discussion
Trisomy 13, 18, and 21 syndromes are the most common fetal chromosomal aneuploidy diseases. Neonatal trisomy 21 syndrome is the most prevalent, occurring approximately once in every 800 live births.10 Amniotic fluid puncture, umbilical cord blood testing, and villus biopsies are the current gold standard for diagnosing fetal chromosomal diseases. However, these tests are all invasive, which may lead to a risk of complications such as abortion, premature delivery, and infection. Some studies have reported that the incidence of embryo loss caused by invasive prenatal diagnosis is 0.5–1.0%.11 Therefore, many pregnant women do not have high compliance with invasive prenatal diagnosis, especially those who become pregnant following IVF.
NIPT is a non-invasive technique for fetal aneuploidy abnormality screening, which involves collecting peripheral blood from pregnant women and the subsequent detection of fetal-free DNA using high-throughput sequencing technology. The technique’s efficiency was first confirmed in 1997,12 and with increased research, the rapid development of high-throughput sequencing technology, and the reduction of detection costs, NIPT has since become more and more established in clinical applications. At present, the detection rate of trisomy 21, 18 and 13 in serological screening is about 60–70%, while the sensitivity of NIPT to trisomy 21, 18 and 13 is up to 99.17%, 98.2% and 100% and the specificity is up to 99.95%, 99.95% and 99.96%.13 NIPT is advantageous compared with traditional serological screening, as it demonstrates high sensitivity, high specificity, and non-invasiveness. So it has good clinical application value and has also been the first choice for pregnant women. Recently, the American Society for Medical Genetics and Genomics suggested that NIPT can be used as an effective screening protocol for aneuploidy in different age groups.14 However, there is a lack of robust, large-sample studies on using NIPT to screen for aneuploidy abnormalities in IVF-conceived fetuses.
IVF-pregnant women tend to be advanced in age, have difficulties conceiving naturally, are particularly protective of the fetus, and have an increased likelihood of twin pregnancy. Most pregnant women who were successfully conceived by IVF would be anxious about the loss of the fetus after invasive operation due to social and family factors.15 The incidence of abnormal fetal chromosomal aneuploidy in pregnant women undergoing IVF is higher than in pregnant women who conceive naturally. Hook16 et al found that with the increase of maternal age, the risk of Down syndrome (DS) and other chromosomal aneuploidy gradually increased. The incidence of chromosomal abnormalities in infants increased with the increase of maternal age, and the incidence was 1/500 under 30 years old, 1/270 in 30 years old, 1/80 in 35 years old, 1/60 in 40 years old, and 1/20 in 45 years old. In addition, many IVF-pregnant women, especially those who are older or expecting twins, refuse invasive examination because serological examination is of little significance to their clinical examination, and they also worry about the complications of prenatal diagnosis. In a study of 502 IVF-pregnant women who received NIPT, a high risk of trisomy 18 was indicated in one case (1.99‰) and confirmed by prenatal diagnosis. In the control group of 8838 women who had conceived naturally, NIPT identified 61 cases (6.90‰) to be at a high risk of trisomy 13, 18, and 21. This indicates that NIPT is a valuable tool in screening fetal trisomy 13, 18, and 21 syndromes in IVF.17 In our study, the results show that the specificity of NIPT in detecting trisomy 13, 18, and 21 syndromes in IVF fetuses is 99.94%, 99.97%, and 99.87%, respectively, and the false positive rate is 0.06%, 0.03%, and 0.13%, respectively, which is essentially consistent with previous reports and suggests that NIPT demonstrates high accuracy in detecting IVF fetal aneuploidy.
In this study, trisomy 21 syndrome was detected by NIPT in twin pregnancies with a sensitivity of 100.00%, a specificity of 99.87%, and a positive predictive value of 83.33%. For trisomy 18, these values were all 100.00%. Due to the small sample size, trisomy 13 was not detected, so no statistics are available. In single pregnancies, trisomy 21 syndrome was detected by NIPT with a sensitivity of 100.00%, a specificity of 99.86%, and a positive predictive value of 62.50%, and for trisomy 18, these values were 100.00%, 99.95%, and 66.67%, respectively. Again, due to the small sample size, trisomy 13 was not detected. Studies show that in monochorionic diamniotic twin pregnancies, the genetic information of the two fetuses in the peripheral blood is consistent and that the NIPT detection accuracy is similar to that of a single fetus. However, in dichorionic diamniotic twin pregnancies, the genetic information of the two fetuses is different. Therefore, if one fetus is abnormal, the NIPT result may be erroneous due to an insufficient proportion of free DNA from the abnormal fetus.18 In this study, NIPT of twin pregnancies revealed seven positive samples, of which one case with a high risk of trisomy 21 underwent amniotic fluid puncture, and no obvious abnormality was found. Postpartum follow-up showed no abnormal phenotype. Due to the small number of cases in this study, further data are needed to assess the NIPT detection rate in IVF twin pregnancies accurately.
In this study, NIPT was performed on 3163 IVF-pregnant fetuses, and 20 pregnant women were found to be at a high risk of fetal chromosome aneuploidy following chromosome karyotype analysis of fetuses and postnatal newborns. Results showed 13 confirmed fetal aneuploidy abnormalities (10 cases with trisomy 21 syndrome and 3 cases with trisomy 18 syndrome). Seven cases were false positive, and the false-positive rate was 0.23%. Factors such as localized placental chimerism, maternal somatic chimerism, and fetal placental chimerism may be responsible for the incompatibility between NIPT detection and reality in this study.19,20 Therefore, for IVF-pregnant women with abnormal NIPT results, amniocentesis and other invasive prenatal diagnostic tests should be carried out for further clarification to avoid false-positive results resulting in the unnecessary termination of pregnancy.
Through this study, it can be found that NIPT for prenatal screening of IVF pregnant fetus can obtain higher positive predictive value, sensitivity and specificity, and has higher screening significance in clinical practice. Meanwhile, as NIPT is widely accepted by IVF pregnant women as non-invasive, it can be considered as the preferred method for prenatal screening of pregnant women after IVF. It should be recognized that this study has several limitations. Among the 3163 cases sampled, 84 cases were lost to follow-up, a rate of 2.66%. A failure to promptly update contact information was responsible for most of the losses, meaning that the delivery outcome inquiry and telephone follow-up could not be carried out. Since 2009, a child health handbook has been established in China, which requires the examination of newborns one week after birth and 30 days after birth. Therefore, lost newborns should establish a health handbook in the community. If there are abnormal physical examination results, newborns should be taken to maternity hospitals for follow-up examination. At present, no feedback has been received from the 84 cases lost to follow-up, so it is considered that there was no abnormal delivery outcome in these cases. In addition, this paper did not compare NIPT detection results between IVF and naturally conceived fetuses, which is a notable shortcoming of this study. One study compared NIPT detection in 476 cases of post-IVF twin pregnancies with 402 cases of natural twin pregnancies, and found that the concentration of fetal free DNA in natural twin pregnancies was significantly higher than that in IVF twin pregnancies. Therefore, it is considered that there may be certain differences between false positive and false negative of NIPT in IVF pregnancy and natural pregnancy detection.21
In conclusion, NIPT has a high screening efficiency for fetal aneuploidy in IVF pregnancy. Therefore, based on informed and voluntary choice, IVF-pregnant women can receive NIPT, while high-risk pregnant women should receive an interventional prenatal diagnosis. Such screening strategies help improve screening efficiency, reducing the probability and risk of interventional prenatal diagnosis.
Ethics Approval and Consent to Participate
The study was conducted in accordance with the Declaration of Helsinki (as was revised in 2013). The study was approved by Ethics Committee of the Women’s Hospital, Zhejiang University School of Medicine. Written informed consent was obtained from all participants.
Acknowledgments
We are particularly grateful to all the people who have given us help on our article.
Funding
This study was funded by the Taizhou science and technology plan class A (21ywa09) and Basic public welfare research program of Zhejiang Province (LGF19H040008).
Disclosure
The authors declare that they have no competing interests.
References
1. Pellestor F, Andréo B, Arnal F, Humeau C, Demaille J. Maternal aging and chromosomal abnormalities: new data drawn from in vitro unfertilized human oocytes. Hum Genet. 2003;112(2):195–203. doi:10.1007/s00439-002-0852-x
2. Zhou Z, Zheng D, Wu H, et al. Epidemiology of infertility in China: a population-based study. BJOG. 2018;125(4):432–441. doi:10.1111/1471-0528.14966
3. Leridon H. Can assisted reproduction technology compensate for the natural decline in fertility with age? A model assessment. Hum Reprod. 2004;19(7):1548–1553. doi:10.1093/humrep/deh304
4. Spencer K. Screening for trisomy 21 in twin pregnancies in the first trimester using free beta-hCG and PAPP-A, combined with fetal nuchal translucency thickness. Prenat Diagn. 2000;20(2):91–95. doi:10.1002/(SICI)1097-0223(200002)20:2<91::AID-PD759>3.0.CO;2-X
5. Garchet-Beaudron A, Dreux S, Leporrier N, et al. Second-trimester Down syndrome maternal serum marker screening: a prospective study of 11 040 twin pregnancies. Prenat Diagn. 2008;28(12):1105–1109. doi:10.1002/pd.2145
6. Evans MI, Wapner RJ. Invasive prenatal diagnostic procedures[J]. Semin Perinatol. 2005;29(4):215–218. doi:10.1053/j.semperi.2005.06.004
7. National Health and Family Planning Commission of the People’s Republic of China. Technical specification for prenatal screening and diagnosis of fetal-free DNA in maternal peripheral blood [Z/OL]; 2019. Available from: http://www.nhc.gov.cn/ewebeditor/uploadfile/2016/11/20161111103703265.docx.
8. Yin AH, Peng CF, Zhao X, et al. Noninvasive detection of fetal subchromosomal abnormalities by semiconductor sequencing of maternal plasma DNA. Proc Natl Acad Sci U S A. 2015;112(47):14670–14675. doi:10.1073/pnas.1518151112
9. McGowan-Jordan J, Simons A, Schmid M. An international system for human cytogenomic nomenclature. Reprint Cytogenet Genome Res. 2016;149:1–2.
10. Affymetrix “Data Sheet: the CytoScan® 750K Cytogenetics Solution”. Available from: http://media.affymetrix.com/support/technical/datasheets/cytoscan750k_datasheet.pdf.
11. Tabor A, Alfirevic Z. Update on procedure-related risks for prenatal diagnosis techniques. Fetal Diagn Ther. 2010;27(1):1–7. doi:10.1159/000271995
12. Lo YM, Corbetta N, Chamberlain PF, et al. Presence of fetal DNA in maternal plasma and serum. Lancet. 1997;350(9076):485–487. doi:10.1016/S0140-6736(97)02174-0
13. Zhang H, Gao Y, Jiang F, et al. Non-invasive prenatal testing for trisomies 21, 18 and 13: clinical experience from 146,958 pregnancies. Ultrasound Obstet Gynecol. 2015;45(5):530–538. doi:10.1002/uog.14792
14. Mao J, Wang T, Wang BJ, et al. Confined placental origin of the circulating cell free fetal DNA revealed by a discordant non-invasive prenatal test result in a trisomy 18 pregnancy. Clin Chim Acta. 2014;433:190–193. doi:10.1016/j.cca.2014.03.011
15. Hong XL. Exploring the influence of psychological nursing on pregnancy outcome in assisted reproduction. Med Theory Practice. 2017;30(8):1233–1234.
16. Hook EB, Cross PK, Schreinemachers DM. Chromosomal abnormality rates at amniocentesis and in live-born infants. JAMA. 1983;249(15):2034–2038. doi:10.1001/jama.1983.03330390038028
17. Gregg AR, Skotko BG, Benkendorf JL, et al. Noninvasive prenatal screening for fetal aneuploidy, 2016 update: a position statement of the American College of Medical Genetics and Genomics. Genet Med. 2016;18(10):1056–1065. doi:10.1038/gim.2016.97
18. Fosler L, Winters P, Jones KW, et al. Aneuploidy screening by non-invasive prenatal testing in twin pregnancy. Ultrasound Obstet Gynecol. 2017;49(4):470–477. doi:10.1002/uog.15964
19. Lau TK, Cheung SW, Lo PS, et al. Non-invasive prenatal testing for fetal chromosomal abnormalities by low-coverage whole-genome sequencing of maternal plasma DNA: review of 1982 consecutive cases in a single center. Ultrasound Obstet Gynecol. 2014;43(3):254–264. doi:10.1002/uog.13277
20. Cheung SW, Patel A, Leung TY. Accurate description of DNA-based noninvasive prenatal screening. N Engl J Med. 2015;372(17):1675–1677. doi:10.1056/NEJMc1412222
21. Wang DM, Yang JX. Application value of noninvasive prenatal screening in chromosomal aneuploidy screening of assisted fertility twin pregnancy. Chine J Prenatal Diagnosis. 2019;011(004):31–36.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
