Back to Journals » Infection and Drug Resistance » Volume 15
Clinical and Microbiological Characteristics of Klebsiella pneumoniae Bloodstream Infection in a Chinese Hospital: Hypervirulent and Multiclonal
Authors Sheng Z, Li J, Chen T, Zhu Y, Yu X, He X, Zheng Y, Ma C, Zheng M, Wang P, Li Z, Xu Y, Xie Q, Su Z, Chen S
Received 3 May 2022
Accepted for publication 20 July 2022
Published 26 July 2022 Volume 2022:15 Pages 3981—3990
DOI https://doi.org/10.2147/IDR.S371477
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Zike Sheng,1,* Junjie Li,2,* Tingting Chen,3 Yan Zhu,4 Xueping Yu,5 Xiuhua He,5 Yijuan Zheng,5 Cuiping Ma,6 Minghui Zheng,5 Peiyun Wang,1 Ziqiang Li,1 Yumin Xu,7 Qing Xie,1 Zhijun Su,5 Sumei Chen5
1Department of Infectious Diseases, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China; 2Department of Respiratory and Critical Care Medicine, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China; 3Department of Pharmacy, The First Hospital of Quanzhou Affiliated to Fujian Medical University, Quanzhou, People’s Republic of China; 4Clinical Laboratory, The First Hospital of Quanzhou Affiliated to Fujian Medical University, Quanzhou, People’s Republic of China; 5Department of Infectious Diseases, The First Hospital of Quanzhou Affiliated to Fujian Medical University, Quanzhou, People’s Republic of China; 6Department of Infection Control, The First Hospital of Quanzhou Affiliated to Fujian Medical University, Quanzhou, People’s Republic of China; 7Department of Infection Control, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhijun Su; Sumei Chen, Department of Infectious Diseases, The First Hospital of Quanzhou Affiliated to Fujian Medical University, Licheng District, Quanzhou, People’s Republic of China, Tel +86-595-22277011 ; +86-595-22277173, Fax +86-595-222781, Email [email protected]; [email protected]
Purpose: Hypervirulent Klebsiella pneumoniae (hvKP) is emerging globally and can cause various infections. This study aimed to investigate the clinical and microbiological characteristics of bloodstream infection (BSI) caused by hvKP.
Patients and Methods: The clinical data of hospitalized patients with K. pneumoniae BSI were retrospectively analyzed. The K. pneumoniae strains were collected and re-identified, and antimicrobial susceptibility testing was performed using the broth microdilution method. Capsular serotypes and virulence genes were detected using polymerase chain reaction, and hvKP was defined as aerobactin positive. Molecular typing was done by multilocus sequence typing. The hvKP and classic K. pneumoniae (cKP) subgroups were compared.
Results: Of the 66 nonrepetitive BSI K. pneumoniae strains included, 29 (43.9%) were hvKP. In these BSI hvKP strains, salmochelin and yersiniabactin accounted for 86.2% and 72.4%, respectively. The prevalence of rmpA, iroBCD cluster, ybtS, clbA, and allS was 89.7%, 86.2%, 72.4%, 51.7%, and 41.4%, respectively, which were all significantly different between the hvKP and cKP subgroups. Serotypes K1 and K2 were strongly associated with hypervirulence (P < 0.05). Nineteen sequence types were scattered in the 29 hvKP strains, and the most common was ST23 (24.1%). None of the hvKP strains were carbapenem resistant. Compared with cKP, hvKP was more capable of developing a liver abscess. However, the 30-day mortality rate was lower (13.8% vs 21.6%) in the hvKP subgroup than in the cKP subgroup.
Conclusion: This study demonstrated a high proportion of hvKP in BSI K. pneumoniae, most of which were RmpA and siderophore producing, and of multiclonal origin.
Keywords: capsular serotypes, hypervirulence, infection, mortality, sequence type
Introduction
Klebsiella pneumoniae is one of the major nosocomial pathogens, which can cause various severe infections, including bloodstream infection (BSI). BSI is a systemic infection and usually results in relatively high mortality due to the virulence factors of K. pneumoniae.
Recently, hypervirulent K. pneumoniae (hvKP), as a variant of K. pneumoniae, has emerged as a major threat to individuals. hvKP has several unique characteristics compared with the classic K. pneumoniae (cKP). Hypermucoviscosity is regarded as an important feature of hvKP, which is mainly mediated by rmpA and/or rmpA2 with overproduction of capsular polysaccharide. Previously, hypermucoviscosity has been used to define hvKP.1,2
Siderophore production is another distinguishing trait of hvKP. Siderophores are dominantly responsible for iron acquisition, contributing to bacterial virulence. Four kinds of siderophores have been reported in K. pneumoniae: aerobactin, salmochelin, yersiniabactin, and enterobactin. Of these, the siderophore aerobactin is dominantly produced (>90%) and has been established as an essential virulence factor in hvKP.3,4 In addition, hvKP infections are more common in healthy individuals from the community, with invasive and metastatic lesions.
The definition of hvKP has not reached a consensus. The hypermucoviscous phenotype has been used to define hvKP in earlier publications.1,2 However, this designation of hvKP by the mucoid phenotype alone is imperfect because not all hvKP strains are hypermucoviscous,5 and some cKP can be hypermucoviscous.6
A few recent studies have defined hvKP based on the genetic background.7–11 Still, many knowledge gaps exist regarding hvKP, and hence the awareness about hvKP needs to be increased urgently. Furthermore, the characteristics of hvKP strains and their differences from cKP are less well-known. Actually, data on hvKP in BSI are extremely limited.2,7 This retrospective study mainly aimed to investigate the clinical and molecular characteristics of patients with K. pneumoniae BSI, especially to delineate the virulence-associated factors. The hvKP and cKP subgroups were compared.
Patients and Methods
Patients
Patients hospitalized at the First Hospital of Quanzhou, a teaching hospital located in Eastern China, from January 2019 to March 2020, with a positive blood culture of K. pneumoniae were enrolled. Clinical data were extracted from the electronic medical records system, including demographic characteristics, site of infections, underlying diseases, intensive care unit (ICU) stay, length of hospital stay, organ failure, prior hospitalization, and clinical outcomes. The 30-day mortality was used to evaluate the clinical outcomes of K. pneumoniae BSI. A community-acquired BSI was defined as a positive blood culture within 48 h after admission, and a hospital‐acquired BSI was designated as a positive culture beyond 48 h after admission.2,10,12 The clinical and microbiological data were compared between patients with cKP BSI and those with hvKP BSI. The present study complied with the Declaration of Helsinki and was approved by the Research Ethics Board at the First Hospital of Quanzhou (212–2018) with a waiver of informed consent for the following reasons: (1) the retrospective nature of the study, (2) the patient data was anonymous, and (3) the strains used in this study were part of the routine hospital laboratory procedure.
Strains
During the study period, all K. pneumoniae strains isolated from blood cultures were collected, and only the first isolation of K. pneumoniae from the same patient was included for further assessment. The strains were re-identified using matrix-assisted laser desorption ionization–time-of-flight mass spectrometry (bioMérieux, Marcy-l’Étoile, France) and stored at −80℃ for further use. Strains with aerobactin positive were defined as hvKP.3,8,9
Antimicrobial Susceptibility Testing
Antimicrobial susceptibility testing was carried out using the broth microdilution method, and 15 antimicrobial agents were tested, including cefotaxime, ceftazidime, cefepime, aztreonam, ampicillin-sulbactam, amoxicillin-clavulanic acid, piperacillin-tazobactam, imipenem, meropenem, amikacin, gentamicin, ciprofloxacin, levofloxacin, chloramphenicol, and colistin. The results were interpreted according to the Clinical and Laboratory Standards Institute.13 Escherichia coli ATCC25922 was used as a quality control strain for determining antimicrobial susceptibility.
Identification of the Hypermucoviscous Phenotype
The string test was used to detect the hypermucoviscous phenotype of K. pneumoniae strains as described in previous studies.1,14 It was considered positive when the viscous string was more than 5 mm in length.
Detection of Capsular Serotypes and Virulence Genes
Six capsular serotypes (K1, K2, K5, K20, K54, and K57) and 14 virulence genes (including rmpA/rmpA2 for mucoviscosity, iroBCD cluster for siderophore salmochelin, iucABCD cluster for siderophore aerobactin, ybtS for siderophore yersiniabactin, clbA/clbB/clbN/clbQ for colibactin, wabG for the biosynthesis of the outer core lipopolysaccharide (LPS), uge for biosynthesis of the capsule and smooth LPS, fimH for type 1 fimbrial adhesin, mrkD for type 3 fimbrial adhesin, and alls for allantoin metabolism) were amplified by polymerase chain reaction (PCR) as described in previous studies.1,10,15–21 The primers used in this study are summarized in Table S1. The PCR products were visualized and analyzed by agarose gel electrophoresis and sequencing.
Multilocus Sequence Typing
Multilocus sequence typing (MLST) was performed as described in a previous study.8 New alleles and sequence types (STs), which did not completely match with those of STs in the MLST database, were temporarily designated as a new ST (nST) in this study.
Statistical Analysis
Categorical variables were recorded as frequency rates and percentages, and continuous variables were expressed as median and interquartile range (IQR) values. SPSS (version 19.0, IBM SPSS Statistics for Windows, IBM Corp., Armonk, New York, United States) was used for analyzing the data. The chi-square test or Fisher’s exact test was used for categorical variables. The Student t-test or Mann–Whitney U-test was used for continuous variables. A P value <0.05 indicated a statistically significant difference.
Results
Distribution and Prevalence of Virulence Genes in BSI K. pneumoniae Strains
During this study period, 66 patients with a positive blood culture of K. pneumoniae were included, and 66 nonrepetitive K. pneumoniae strains were collected. Among these strains, 29 (43.9%) were positive for siderophore aerobactin and consequently designated as hvKP strains. The remaining 37 (56.1%) K. pneumoniae were considered as cKP. Another two siderophores, salmochelin and yersiniabactin, accounted for 53.0% (n = 35) and 54.5% (n = 36), respectively, in all these BSI K. pneumoniae strains (Table 1). Forty-three (65.2%) strains were positive for rmpA and/or rmpA2 (both rmpA and rmpA2, n = 32; rmpA only, n = 2; and rmpA2 only, n = 9). Of note, 26 of the 32 (81.3%) strains co-carrying rmpA and rmpA2 were hvKP strains, while 11 strains with rmpA or rmpA2 only were all cKP strains. Two genes (clbA and clbB) of the pks colibactin gene cluster together with another two genes (clbN and clbQ) were simultaneously detected in 18 (27.3%) strains. A relatively low prevalence of alls (22.7%, n = 15) was noted. On the contrary, a high prevalence of uge (98.5%, n = 65) and wabG (84.8%, n = 56) was found. Interestingly, 65 (98.5%) strains had an mrkD gene, whereas 26 (39.4%) harbored a fimH gene.
 |
Table 1 Microbiological Characteristics of K. pneumoniae Causing Bloodstream Infection |
As shown in Table 1, the iroBCD gene cluster (86.2% vs 27.0%), ybtS (72.4% vs 40.5%), rmpA (89.7% vs 21.6%), clbA (51.7% vs 8.1%), and allS (41.4% vs 8.1%) were significantly more prevalent in hvKP than in cKP (P ≤ 0.001). Nonetheless, the prevalence of uge (96.6% vs 100%), wabG (86.2% vs 83.8%), fimH (41.4% vs 37.8%), and mrkD (96.6% vs 100%) genes was similar in both the hvKP and cKP groups.
Antimicrobial Susceptibility of BSI K. pneumoniae
The tested antibiotics had good antibacterial activity against the BSI K. pneumoniae strains in vitro (Table 2). The susceptibility of hvKP to seven β-lactam agents was significantly higher than that of cKP (P < 0.05). Notably, no hvKP strain was found resistant to imipenem and meropenem.
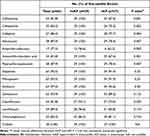 |
Table 2 Antimicrobial Susceptibility of Hypervirulent and Classic K. pneumoniae Causing BSI |
String Test
A total of 29 (43.9%) BSI K. pneumoniae strains were string test positive in the present study. The positive rate was 75.9% (n = 22) in hvKP strains and 18.9% (n = 7) in cKP strains (P < 0.001, Table 1), suggesting that defining hvKP by string test only was not suitable.
Serotype Identification
Of the 66 BSI K. pneumoniae strains, 14 (21.2%) K1, 12 (18.2%) K2, 3 (4.5%) K5, 1 (1.5%) K20, 1 (1.5%) K54, and 2 (3.0%) K57 capsular serotypes were identified. In hvKP strains, K1, K2, K5, K20, K54, and K57 capsular serotypes accounted for 41.4% (n = 12), 31.0% (n = 9), 0 (n = 0), 3.4% (n = 1), 0 (n = 0), and 6.9% (n = 2), respectively, and only 5 (17.2%) strains were K-nontypable (Table 1). Nevertheless, the prevalence of these six serotypes was quite low (5.4%, 8.1%, 8.1%, 0, 2.7%, and 0) in cKP BSI K. pneumoniae strains (Table 1). Taken together, these results suggested a good correlation between hypervirulence and K1/K2 capsular serotypes.
MLST
Among the 66 BSI K. pneumoniae strains, 43 had known STs (involving 30 STs), and the remaining 23 strains each had an nST (Table S2), indicating high diversity of these BSI strains. The most common ST was ST23 (n = 7, 10.6%) belonging to clonal complex (CC) 23, followed by ST86 (n = 3). Four strains (6.1%) were categorized as CC65, containing two ST65, one ST25, and one ST375. CC23 and CC65 were the most common CCs in this study.
Nineteen STs were scattered in the 29 hvKP strains, including ST23 (n = 7), ST65 (n = 2), ST86 (n = 2), ST380 (n = 2), ST412 (n = 2), and other 14 distinct STs (Table S2), while 39 different STs were distributed in the 39 cKP strains (Table S2).
Interestingly, of the 14 K. pneumoniae strains with K1 serotype (hvKP, n = 12), 7 (50%) belonged to ST23, which were all hvKP strains (Table S2), indicating a strong correlation between ST23 and K1 serotype in hvKP strains. Differently, among the 12 K2 serotype strains (9 hvKP and 3 cKP), ST86 (n = 3, 25%) was the most common ST, followed by ST380 (n = 2) and ST65 (n = 2). In a word, the present study indicated an association between certain STs and K serotypes (eg, ST23-K1 and ST86-K2).
Clinical Characteristics of BSI Caused by K. pneumoniae Strains
The demographic and clinical data of the 66 enrolled patients with K. pneumoniae BSI are summarized in Table 3. These patients were divided into hvKP and cKP subgroups based on their corresponding isolated K. pneumoniae strains. Of the 66 patients, the median age was 63 years (ranging from 0 to 90 years; IQR, 50–74), and 39 patients (59.1%) were male. Forty-eight (72.7%) patients had a community-acquired BSI, of which 24 were in the hvKP subgroup. Although the percentage of the community-acquired BSI in the hvKP subgroup was higher than that in the cKP subgroup (82.8% vs 64.9%, respectively), no significant difference existed between the two subgroups (P > 0.05; Table 3).
 |
Table 3 Clinical Characteristics of Patients with K. pneumoniae Bloodstream Infection |
Seventeen (25.8%) patients developed abscesses, including liver abscess (n = 14), skin abscess (n = 1), peripancreatic abscess (n = 1), and abdominal wall abscess (n = 1). The percentage of patients with a liver abscess was significantly higher in the hvKP subgroup than in the cKP subgroup (P < 0.001), indicating the ability of hvKP to develop a liver abscess. Besides abscesses, pneumonia (n = 26), urinary tract infection (n = 15), abdominal infection (n = 10), and skin and soft tissue infection (n = 3) afflicted 39 patients (Table 3), which were all more common in the cKP subgroup, although no statistical difference except for abdominal infection was found between the two groups. Actually, most (n = 52, 78.8%) of the 66 patients had ≥2 sites of infections.
Underlying diseases were noted in all 66 patients (Table 3), including diabetes (n = 38, 57.6%), hypertension (n = 11, 16.7%), coronary heart disease (n = 7, 10.6%), chronic kidney disease (n = 6, 9.1%), and cancer (n = 15, 22.7%). Among these underlying diseases, diabetes, coronary heart disease, and chronic kidney disease were more prevalent in the hvKP subgroup, while hypertension and cancer were more prevalent in the cKP subgroup (Table 3). However, no significant statistical differences existed between the hvKP and cKP subgroups in these diseases (P > 0.05). Interestingly, of the 38 patients with diabetes, 12 (31.6%) developed a liver abscess. Among the remaining 28 patients without diabetes, only 2 (7.1%) developed a liver abscess (P = 0.016), demonstrating a strong association between diabetes and liver abscess.
Additionally, 19 (28.8%) patients had a history of hospitalization within 90 days prior to admission. A significant difference in hospitalization within recent 90 days was found between the hvKP subgroup and the cKP subgroup, with 10.3% and 43.2%, respectively (P = 0.003; Table 3).
Although no statistical significance was noted, the cKP subgroup seemed to have a higher percentage of ICU stay, septic shock, and organ failure (30.3%, 27.3%, and 21.2%, respectively) and longer median hospital stay in this study (Table 3), suggesting that patients with cKP were prone to develop a severe disease and have a longer hospital stay.
The 30-day mortality rate of K. pneumoniae BSI was 18.2% in this study, and it was higher (21.6%) in the cKP subgroup (Table 3). After discharge from the hospital, 13 (24.1%) patients were readmitted to the hospital in the following 90 days, with 6 in the hvKP subgroup and 7 in the cKP subgroup (Table 3). Of them, four patients (4/13, 30.8%) were due to bacterial infection, including three (3/6, 50%) in the hvKP subgroup and one (1/7, 14.3%) in the cKP subgroup.
Discussion
The present retrospective study provided insights into the clinical and microbiological characteristics of patients with K. pneumoniae BSI, especially revealing the distribution of virulence genes in hvKP. A relatively high percentage (43.9%) of hvKP in BSI K. pneumoniae strains was found to carry multiple virulence genes in this study, and these pathogens were of multiclonal origin.
The hypermucoviscosity and the iron acquisition systems (siderophores) are common in hvKP strains, which are considered as the main features of hvKP. In the present study, strains with iucA gene (for siderophore aerobactin) were defined as hvKP, and a relatively higher proportion of BSI hvKP was found compared with previous studies (21.6–31.4%).2,7,10 The prevalence of hvKP in BSI was relatively high in China, but varied in different regions, which might partially result from the geographical difference and the inconsistent definition of hvKP. Recently, Harada et al revealed that 25.5% (n = 26) of BSI K. pneumoniae strains at hospitals across Japan were hvKP (defining hvKP as positive for any of rmpA, rmpA2, iroBCDN, iucABCD, and iutA).22
Previous studies showed that various virulence factors could concurrently be present in hvKP.3 This study revealed that BSI hvKP strongly related to rmpA, iroBCD cluster, ybtS, clbA, and allS. The siderophore aerobactin is a dominant and critical siderophore for hvKP, which plays an important role in systemic infection.3 In this study, 43.9% of BSI hvKP strains carried the iucABCD cluster, which was consistent with a recent study from South Korea (41.5% of BSI K. pneumoniae carried iucA gene).23 Lan et al from China reported that a lower percentage of BSI K. pneumoniae was iucA positive (28.9%).10 In this study, more than half of the BSI K. pneumoniae were also found to possess genes for other two siderophores (salmochelin and yersiniabactin). The exact role of these siderophores in BSI hvKP needs to be further investigated.
Colibactin, which is encoded by the pks gene cluster and exerts as genotoxins, was first found in E. coli and was associated with BSI.24 The presence of the pks gene cluster has been related to early mortality in patients with BSI caused by K. pneumoniae.23 The real role of colibactin in the pathogenesis of hvKP remains to be explored. Colibactin was detected in 27.3% of BSI K. pneumoniae strains in the present study, consistent with the studies by Lan et al and Kim et al (26.8% and 27.3%, respectively).10,23 Putze et al reported a much lower rate (3.5%) of clinical K. pneumoniae being colibactin positive in Europe.25 Additionally, the colibactin-positive rate was 16.7% in K. pneumoniae isolated from various clinical samples in Taiwan.26
Interestingly, in this study, all colibactin-producing hvKP strains except one co-carried ybtA. Kim et al reported that 27.3% (n = 158) of BSI K. pneumoniae strains co-harbored the pks gene cluster and ybtA.23 Additionally, although allantoin metabolism genes do not seem to be important for systemic infection,6 this study demonstrated 22.7% of BSI K. pneumoniae strains with allS, suggesting a potential role of allS in BSI. Taken together, more studies are needed to clarify the real role of these virulence factors in BSI.
The present study suggested the association between hypervirulence and K1/K2/K20/K57 capsular serotypes, consistent with other studies from China.2,8,9 Additionally, this study revealed that 72.4% of hvKP strains were K1 and K2 capsular serotypes, while only 13.5% of cKP belonged to these two serotypes. These findings indicated that K1 and K2 capsular serotypes played key roles in hvKP BSI. K5 and K54 capsular serotypes were not detected in BSI hvKP strains in the present study, consistent with previous studies.2,7
In this study, the BSI-causing K. pneumoniae strains were of multiclonal origin, despite the most common ST (ST23) accounting for 10.6%. Similarly, Liu et al reported that 42 STs were identified in the 70 BSI K. pneumoniae strains.2 Wu et al demonstrated that more than 36 STs were established in 79 BSI K. pneumoniae strains.27
This study revealed that hvKP strains were more susceptible to tested antibiotics than cKP, consistent with previous studies.1,8,10 The confluence of hypervirulence and multidrug resistance, especially carbapenem resistance, is extremely alarming. Although carbapenem-resistant hvKP has been described in previous studies,7,9,28–30 it was not found in the present study. This might be partially attributed to the regional difference.
Although various infections had developed in patients with BSI in the present study, a liver abscess was more likely to be associated with hvKP, suggesting the capability of hvKP to develop a liver abscess, which was in agreement with previous studies.1,8,11 The results of this study also indicated a strong association between diabetes and liver abscess (mainly by hvKP, 85.7%), in accordance with an earlier study.16 Thus, it is reasonable to conclude that patients with diabetes may be prone to suffer from hvKP liver abscess and develop hvKP BSI afterward. This was in line with a theory that diabetes is a risk factor for an hvKP infection, and the confluence of diabetes and liver abscess is likely to develop secondary infections.31 Although diabetes was identified as an independent risk factor for hvKP BSI in a previous study,7 more studies are needed to clarify this.
Although no significant difference in the 30-day mortality rate was noted between cKP and hvKP subgroups, the percentage of mortality was higher in the cKP BSI subgroup than in the hvKP BSI subgroup in the present study, consistent with earlier studies in patients with BSI.2,7 Recently, a study reported that the hypermucoviscosity (as a marker for defining hvKP in several studies) displayed an inverse association with 30-day mortality in BSI K. pneumoniae strains.23 Similarly, Hwang et al recently reported that the 30-day mortality in patients with cKP pneumonia (26.9%) was higher than that in patients with hvKP pneumonia (17.9%).32 This might be attributed to patients in the cKP subgroup usually having more and much severe underlying diseases, as well as greater age. Additionally, a higher percentage (43.2% in cKP vs 10.3% in hvKP) of a history of hospitalization in recent 90 days may be partially contributed to the higher mortality in the cKP subgroup. Finally, in the present study cKP BSI strains were more resistant to the common empiric antibiotics and then likely caused treatment failure, which might also be contributed to the higher mortality in those patients.33 More prospective studies are needed to confirm the real role of hvKP in the mortality of patients with BSI.
This study had several limitations. First, the presence of the aerobactin gene was detected, and hvKP was defined on the basis of aerobactin positivity. However, the aerobactin production was not assessed. Further studies defining hvKP by assessing the quantitative production of aerobactin would be warranted, and studies in vitro and in vivo may be needed to confirm the real virulence of K. pneumoniae. Second, this was a single-center experience with a relatively small study sample. Multicenter studies with a larger population are required.
Conclusions
This study demonstrated a high proportion of hvKP in BSI K. pneumoniae. These hvKP strains had a strong correlation with various virulence factors and were of multiclonal origin. It provided insights into the clinical and microbiological features of BSI caused by K. pneumoniae strains, highlighting the significance of clinical awareness, and might be helpful in the clinical management of hvKP BSI.
Ethics Statement
This study was approved by the Research Ethics Board at the First Hospital of Quanzhou (2012–2018) with a waiver of informed consent.
Acknowledgments
This study was supported by the funding from the Science and Technology Project of Quanzhou (NO. 20181N043S to S. Chen), the National Natural Science Foundation of China (NO. 81703567 to J. Li, and NO. 81603166 to Z. Sheng), and the Shanghai Municipal Key Clinical Specialty (Infectious disease, YW20190002 to Q. Xie).
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Li W, Sun G, Yu Y, et al. Increasing occurrence of antimicrobial-resistant hypervirulent (hypermucoviscous) Klebsiella pneumoniae isolates in China. Clin Infect Dis. 2014;58:225–232. doi:10.1093/cid/cit675
2. Liu YM, Li BB, Zhang YY, et al. Clinical and molecular characteristics of emerging hypervirulent Klebsiella pneumoniae bloodstream infections in mainland China. Antimicrob Agents Chemother. 2014;58:5379–5385. doi:10.1128/AAC.02523-14
3. Russo TA, Olson R, MacDonald U, et al. Aerobactin, but not yersiniabactin, salmochelin, or enterobactin, enables the growth/survival of hypervirulent (Hypermucoviscous) Klebsiella pneumoniae ex vivo and in vivo. Infect Immun. 2015;83:3325–3333. doi:10.1128/IAI.00430-15
4. Russo TA, Olson R, Macdonald U, et al. Aerobactin mediates virulence and accounts for increased siderophore production under iron-limiting conditions by hypervirulent (hypermucoviscous) Klebsiella pneumoniae.. Infect Immun. 2014;82:2356–2367. doi:10.1128/IAI.01667-13
5. Shi Q, Lan P, Huang D, et al. Diversity of virulence level phenotype of hypervirulent Klebsiella pneumoniae from different sequence type lineage. BMC Microbiol. 2018;18:94. doi:10.1186/s12866-018-1236-2
6. Russo TA, Marr CM. Hypervirulent Klebsiella pneumoniae. Clin Microbiol Rev. 2019;32:e00001–e00019. doi:10.1128/CMR.00001-19
7. Li J, Ren J, Wang W, et al. Risk factors and clinical outcomes of hypervirulent Klebsiella pneumoniae induced bloodstream infections. Eur J Clin Microbiol Infect Dis. 2018;37:679–689. doi:10.1007/s10096-017-3160-z
8. Zhang Y, Zhao C, Wang Q, et al. High prevalence of hypervirulent Klebsiella pneumoniae infection in China: geographic distribution, clinical characteristics, and antimicrobial resistance. Antimicrob Agents Chemother. 2016;60(10):6115–6120. doi:10.1128/AAC.01127-16
9. Liu C, Shi J, Guo J. High prevalence of hypervirulent Klebsiella pneumoniae infection in the genetic background of elderly patients in two teaching hospitals in China. Infect Drug Resist. 2018;11:1031–1041. doi:10.2147/IDR.S161075
10. Lan Y, Zhou M, Jian Z, et al. Prevalence of pks gene cluster and characteristics of Klebsiella pneumoniae -induced bloodstream infections. J Clin Lab Anal. 2019;33:e22838. doi:10.1002/jcla.22838
11. Wu H, Li D, Zhou H, et al. Bacteremia and other body site infection caused by hypervirulent and classic Klebsiella pneumoniae.. Microb Pathog. 2017;104:254–262. doi:10.1016/j.micpath.2017.01.049
12. Shi Q, Quan J, Lan P, et al. Prevalence and characteristics of pks gene cluster harbouring Klebsiella pneumoniae from bloodstream infection in China. Epidemiol Infect. 2020;148:e69. doi:10.1017/S0950268820000655
13. CLSI. Performance Standards for Antimicrobial Susceptibility Testing.
14. Zhou C, Wu Q, He L, et al. Clinical and molecular characteristics of carbapenem-resistant hypervirulent Klebsiella pneumoniae Isolates in a tertiary hospital in Shanghai, China. Infect Drug Resist. 2021;14:2697–2706. doi:10.2147/IDR.S321704
15. Fang CT, Lai SY, Yi WC, et al. Klebsiella pneumoniae genotype K1: an emerging pathogen that causes septic ocular or central nervous system complications from pyogenic liver abscess. Clin Infect Dis. 2007;45:284–293. doi:10.1086/519262
16. Ye M, Tu J, Jiang J, et al. Clinical and genomic analysis of liver abscess-causing Klebsiella pneumoniae identifies new liver abscess-associated virulence genes. Front Cell Infect Microbiol. 2016;6:165. doi:10.3389/fcimb.2016.00165
17. Yeh KM, Kurup A, Siu LK, et al. Capsular serotype K1 or K2, rather than magA and rmpA, is a major virulence determinant for Klebsiella pneumoniae liver abscess in Singapore and Taiwan. J Clin Microbiol. 2007;45:466–471. doi:10.1128/JCM.01150-06
18. Turton JF, Baklan H, Siu LK, et al. Evaluation of a multiplex PCR for detection of serotypes K1, K2 and K5 in Klebsiella sp. and comparison of isolates within these serotypes. FEMS Microbiol Lett. 2008;284:247–252. doi:10.1111/j.1574-6968.2008.01208.x
19. Bachman MA, Oyler JE, Burns SH, et al. Klebsiella pneumoniae yersiniabactin promotes respiratory tract infection through evasion of lipocalin 2. Infect Immun. 2011;79:3309–3316. doi:10.1128/IAI.05114-11
20. Yu WL, Ko WC, Cheng KC, et al. Association between rmpA and magA genes and clinical syndromes caused by Klebsiella pneumoniae in Taiwan. Clin Infect Dis. 2006;42:1351–1358. doi:10.1086/503420
21. Luo Y, Wang Y, Ye L, et al. Molecular epidemiology and virulence factors of pyogenic liver abscess causing Klebsiella pneumoniae in China. Clin Microbiol Infect. 2014;20:O818–O824. doi:10.1111/1469-0691.12664
22. Harada S, Aoki K, Yamamoto S, et al. Clinical and molecular characteristics of Klebsiella pneumoniae isolates causing bloodstream infections in Japan: occurrence of hypervirulent infections in health care. J Clin Microbiol. 2019;57:e01206–e01219. doi:10.1128/JCM.01206-19
23. Kim D, Park BY, Choi MH, et al. Antimicrobial resistance and virulence factors of Klebsiella pneumoniae affecting 30 day mortality in patients with bloodstream infection. J Antimicrob Chemother. 2019;74:190–199. doi:10.1093/jac/dky397
24. Johnson JR, Johnston B, Kuskowski MA, et al. Molecular Epidemiology and Phylogenetic Distribution of the Escherichia coli pks Genomic Island. J Clin Microbiol. 2008;46:3906–3911. doi:10.1128/JCM.00949-08
25. Putze J, Hennequin C, Nougayrede JP, et al. Genetic structure and distribution of the colibactin genomic island among members of the family Enterobacteriaceae. Infect Immun. 2009;77:4696–4703. doi:10.1128/IAI.00522-09
26. Chen YT, Lai YC, Tan MC, et al. Prevalence and characteristics of pks genotoxin gene cluster-positive clinical Klebsiella pneumoniae isolates in Taiwan. Sci Rep. 2017;7:43120. doi:10.1038/srep43120
27. Wu X, Shi Q, Shen S, et al. Clinical and bacterial characteristics of Klebsiella pneumoniae affecting 30-day mortality in patients with bloodstream infection. Front Cell Infect Microbiol. 2021;11:688989. doi:10.3389/fcimb.2021.688989
28. Zhang Y, Jin L, Ouyang P, et al. Evolution of hypervirulence in carbapenem-resistant Klebsiella pneumoniae in China: a multicentre, molecular epidemiological analysis. J Antimicrob Chemother. 2020;75:327–336. doi:10.1093/jac/dkz446
29. Yao H, Qin S, Chen S, et al. Emergence of carbapenem-resistant hypervirulent Klebsiella pneumoniae.. Lancet Infect Dis. 2018;18:25. doi:10.1016/S1473-3099(17)30628-X
30. Gu D, Dong N, Zheng Z, et al. A fatal outbreak of ST11 carbapenem- resistant hypervirulent Klebsiella pneumoniae in a Chinese hospital: a molecular epidemiological study. Lancet Infect Dis. 2018;18:37–46. doi:10.1016/S1473-3099(17)30489-9
31. Choby JE, Howard-Anderson J, Weiss DS. Hypervirulent Klebsiella pneumoniae-clinical and molecular perspectives. J Intern Med. 2020;287:283–300. doi:10.1111/joim.13007
32. Hwang JH, Handigund M, Hwang JH, et al. Clinical features and risk factors associated with 30-day mortality in patients with pneumonia caused by hypervirulent Klebsiella pneumoniae (hvKP). Ann Lab Med. 2020;40:481–487. doi:10.3343/alm.2020.40.6.481
33. Chan KS, Shelat VG. Klebsiella pneumoniae bacteremia is associated with higher mortality in acute calculous cholangitis as compared to Escherichia coli bacteremia. World J Surg. 2022;46:1678–1685. doi:10.1007/s00268-022-06559-0
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
