Back to Journals » Integrated Blood Pressure Control » Volume 14
Clinical and Angiographic Prophesy of Hemodynamic Status in Patients with Acute Anterior Wall ST-Segment-Elevation Myocardial Infarction and Totally Occluded Left Anterior Descending Artery
Authors Otaal PS , Shah A, Batta A , Sood A, Pal A
Received 10 April 2021
Accepted for publication 28 May 2021
Published 18 June 2021 Volume 2021:14 Pages 89—97
DOI https://doi.org/10.2147/IBPC.S315050
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Turgay Celik
Parminder Singh Otaal,1 Amit Shah,2 Akash Batta,3 Ashwani Sood,4 Arnab Pal5
1Department of Cardiology, Advanced Cardiac Centre, Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, India; 2Department of Internal Medicine, Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, India; 3Department of Cardiology, Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, India; 4Department of Nuclear Medicine, Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, India; 5Department of Biochemistry, Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, India
Correspondence: Parminder Singh Otaal
Department of Cardiology, Advanced Cardiac Centre, Post Graduate Institute of Medical Education and Research (PGIMER), Sector-12, Chandigarh, 160012, Punjab, India
Tel +91 9814526747
Email [email protected]
Background: Left anterior descending artery (LAD) is the most common occluded vessel in a patient presenting with acute anterior wall ST-segment elevated myocardial infarction (STEMI). Acute occlusion of LAD usually results in hemodynamic compromise. However, some patients maintain hemodynamic stability despite its proximal occlusion. As the factors associated with hemodynamic status in such patients are poorly understood, our study sought to determine the clinical and angiographic parameters associated with hemodynamic stability in these patients.
Methods: In this prospective observational study, 60 consecutive patients of acute anterior wall STEMI with completely occluded LAD on coronary angiography were included. Various clinical and angiographic parameters associated with hemodynamic status were evaluated.
Results: Of the 60 patients, 30 patients each were included in the hemodynamically stable (group I) and hemodynamically unstable group (group II). The mean age of the patients in group I and group II was 51.07± 13.78 years and 55.47± 11.69 years, respectively. The hemodynamically unstable group had a significantly higher number of patients with diabetes mellitus, elevated Troponin T level, and lower left ventricular ejection fraction as compared to the stable group (p< 0.05). In contrast, 11 (36.7%) patients in the hemodynamically stable group had rich collaterals compared to 4 (13.3%) patients in the hemodynamically unstable group. The difference was statistically significant (p=0.037).
Conclusion: The present study showed that the presence of diabetes, severe LV systolic dysfunction, elevated Troponin-T level, and poor collaterals were associated with hemodynamic instability, whereas the presence of better collaterals predicted hemodynamic stability in patients presenting with anterior wall STEMI and total LAD occlusion.
Keywords: STEMI, left anterior descending artery, occlusion, hemodynamic stability, angiographic, clinical predictors
Introduction
With an estimated 17.9 million deaths in the year 2017, cardiovascular disease (CVD) is the number one cause of death worldwide.1 Coronary artery disease (CAD), including acute coronary syndrome (ACS), accounts for nearly 40% of deaths associated with CVD.2 The spectrum of ACS includes a clinical presentation with unstable angina, non-ST-segment elevated myocardial infarction (NSTEMI), and ST-segment elevated myocardial infarction (STEMI). STEMI is the most severe form of ACS and requires prompt restoration of flow in the infarct-related artery either using fibrinolytic agents and/or revascularization with percutaneous coronary intervention (PCI)/coronary artery bypass graft surgery (CABG). The usual culprit vessel in a patient presenting with anterior wall STEMI is the left anterior descending artery (LAD). As it supplies a large area of the myocardium, patients with infarcts related to the left main or proximal LAD occlusion tend to have hemodynamic instability, low residual left ventricular ejection fraction (LVEF), and worse prognosis as compared to non-LAD or distal LAD related infarcts.3 Similarly, anterior wall STEMI is more likely to be associated with cardiogenic shock,4 thus portending a worse prognosis. Moreover, while acute, proximal LAD occlusion associated with STEMI is more likely to cause hemodynamic compromise, some patients remain hemodynamically stable despite unsuccessful thrombolysis/or no thrombolysis and completely occluded LAD on an angiogram.
Various factors which influence the presenting hemodynamic status in an acute anterior wall STEMI with a completely occluded culprit artery do so by mainly affecting the amount of ischemic myocardium at jeopardy. Older age, female sex, diabetes, hypertension, prior myocardial infarction (MI) or angina, pre-existent heart failure or reduced Left Ventricular Ejection Fraction (LVEF), delay in treatment initiation, left bundle-branch block on electrocardiogram have all been associated with increased incidence of hemodynamic instability.5 Cardiac troponins are sensitive for the early detection of myocardial cell injury in ACS with a strong negative correlation between Troponin T level and LVEF.6 Higher cardiac troponins and a lower LVEF at presentation portend worse long-term outcomes.7 In a study by Nguyen et al, high Troponin T levels at 48 and 72 hours were independent predictors for a major adverse cardiovascular endpoint.8 A 10-fold increase in troponin level predicted increased incidence of cardiac arrest, unstable ventricular arrhythmias, cardiogenic shock, heart failure, and death after myocardial infarction. Also, the degree of troponin elevation correlated with increased short- and long-term mortality.9 Angiographic predictors of hemodynamic status include the presence of multivessel CAD, complete occlusion of LAD,10 and absence of collateral circulation to the culprit vessel.11 The presence of coronary collaterals in a patient with pre-existing stable CAD protects the myocardium during acute ischemia, thereby providing a better prognosis. In a study by Pérez-Castellano et al, 64% of acute MI patients without collateral circulation to LAD had a more frequent incidence of complications such as cardiogenic shock, mechanical complications, arrhythmias, and even deaths.12 Another factor that can potentially influence the hemodynamic status in STEMI is the amount of viable myocardium despite complete occlusion of the culprit artery. The ideal imaging modality to determine myocardial viability is a matter of debate. Various modalities, including echocardiography, single-photon emission computed tomography (SPECT), cardiac magnetic resonance (CMR), and positron emission tomography (PET), exist. PET is considered a gold standard technique for assessing myocardial viability, but its widespread use has been limited due to expense and availability constraints.
Although unstable STEMI patients benefit from urgent revascularisation, evidence from Occluded Artery Trial (OAT) showed that routine opening of occluded infarct-related artery (IRA) beyond 48 hours in stable patients did not confer clinical benefit over optimal medical therapy.13 These findings were also confirmed in a recent meta-analysis.14 This is reflected in the 2017 European Society of Cardiology (ESC) guidelines, and routine opening of occluded IRA >48 hours in a hemodynamically stable condition was given a class III recommendation.15
While most of these pre-existing studies have identified individual parameters associated with hemodynamic stability in acute STEMI,5,7 no study conducted so far has correlated various parameters to the presenting hemodynamic status among STEMI patients with completely occluded culprit artery. The objective of our study was to assess various clinical and angiographic parameters associated with hemodynamic status at presentation in patients with acute anterior STEMI and an occluded culprit vessel.
Materials and Methods
This prospective, cross-sectional, observational study was carried out from 1st July 2018 till 31st December 2019 at the Postgraduate Institute of Medical Education Research (PGIMER), Chandigarh, a tertiary care institute in Northern India. The study was approved by Institutional Ethics Committee (Intramural) of Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh and conducted according to the ethical principles stated in the latest version of the Helsinki Declaration and the applicable guidelines for good clinical practice. A well-informed written consent was obtained from all the participants.
Patient Selection
Patients of either sex, aged 18 years or older, with acute anterior wall STEMI presenting within 72 hours of the onset of chest pain who underwent coronary angiography were eligible for the study. Angiographically, the patients were required to have a single vessel disease in the form of a totally occluded LAD. Patients with acute occlusion of coronaries other than LAD and the presence of multi-vessel disease, pregnancy, or renal failure were excluded from the study. Criteria for hemodynamic instability were patients in congestive heart failure, systolic BP less than 90 mmHg, and the presence of cardiac arrhythmia, especially ventricular tachycardia or ventricular fibrillation. Patients without congestive heart failure, hypotension, or cardiac arrhythmia were considered hemodynamically stable.
Methods and Outcomes
The STEMI patients with occluded LAD on coronary angiography with hemodynamic stability were taken into group I, and patients with hemodynamic instability were taken into group II. Patients were further managed as per ACC/AHA guidelines for revascularization.
The study’s primary objective was to assess the clinical and angiographic parameters associated with hemodynamic stability at presentation in patients with STEMI. This also included a quantitative assessment of troponin T level, which was done in all the patients to assess the correlation of troponin T level with hemodynamic status. This was done by COBAS e601 analyzers by electrochemiluminescence method after doing proper calibration and quality control as per the manufacturer’s recommendation. Angiographically, collaterals were assessed on coronary angiogram using Rentrop’s classification as Grade 0,1,2,3.16 Kilian et al, graded collateral circulation to the occluded artery as poor collaterals when no or incomplete filling and rich collaterals when complete filling.17
The study’s secondary objective was to assess the myocardial viability using PET scan only in group I of hemodynamically stable patients presenting >24 hours after onset of STEMI without an indication for urgent revascularization as per ACC/AHA guidelines. Gated rest myocardial perfusion imaging (MPI) was done with 13-N ammonia in all patients as the first step, followed by injection of 10–12 mCi of 13NH3 in resting condition and immediate PET imaging for assessment of perfusion of the LV myocardium. The reconstructed images were assessed for perfusion defects. If there was a perfusion defect, patients were prepared for cardiac 18F-FDG imaging on the same day or another day. For cardiac 18F-FDG PET, patients were kept fasting for at least 6–12 hours, and oral glucose loading was done before 18F-FDG injection. Administration of 18F-FDG, 5–8 mCi intravenously was done if the blood glucose level was ≤150 mg/dl. Imaging was done after 45–60 minutes of the tracer injection with standard imaging procedures and ECG gating whenever feasible. The perfusion and viability imaging were then visually interpreted by segment-to-segment comparison. FDG uptake was assessed in all regions of LV myocardium where there was reduced/absent perfusion and wall motion abnormality.
Statistical Analysis
All data were prospectively collected by trained physicians (study authors) and entered into a spreadsheet (Microsoft Excel 2016TM; Microsoft Corporation, USA). Statistical analysis was done via statistical package for social sciences (SPSS Inc., version 23.0TM; IBM Corporation, Chicago, USA). The measurable data was checked for their normality using the Kolmogorov–Smirnov test within each group. Continuous variables are presented as mean ± SD or median (inter-quartile range), whereas the categorical variables are presented as a percentage. Independent sample t-test was applied for between-group comparisons of normally distributed data, whereas non-normally distributed data were compared using the Mann–Whitney U-test. Chi-square test or Fisher’s exact test, whichever was applicable, was applied for categorical variables. All tests are two-sided, and a p-value < 0.05 is taken as the level of significance.
Results
Sixty patients (44 men and 16 women) of anterior wall STEMI with single-vessel disease (total occlusion of LAD artery) on coronary angiography were included. Of the 60 patients, 30 patients each were included in group I (hemodynamically stable) and group II (hemodynamically unstable), depending upon their status at presentation. Of the 30 patients in the hemodynamically stable group, a PET scan for assessment of myocardial viability could be done in only 17 participants.
Baseline Patient Characteristics
Baseline characteristics were matched between the two groups (Table 1).
 |
Table 1 Baseline Clinical Characteristics of Hemodynamically Stable (Group I) and Hemodynamically Unstable (Group II) Group of Patients |
Clinical Characteristics
The mean age of the patients in the hemodynamically stable group (group I) and hemodynamically unstable group (group II) was 51.07±13.78 years and 55.47±11.69 years, respectively. Although the hemodynamically unstable group patients were older as compared to the stable group, the difference was not statistically significant (p=0.188). There were more patients with diabetes mellitus in the unstable group, and the difference was statistically significant between the two groups (p=0.020). Similarly, Troponin T level was significantly greater in the unstable group than the stable group (p= 0.0001). Furthermore, a significantly higher number of patients in the unstable group had lower LVEF than the stable group (p=0.02).
Angiographic Characteristics
Site of Occlusion
In our study, no statistically significant difference between the hemodynamically stable group (I) or unstable group (II) was observed based on the site of LAD occlusion: proximal versus non-proximal (p=0.592). (Table 2)
 |
Table 2 Angiographic Characteristics of Hemodynamically Stable (Group I) and Hemodynamically Unstable (Group II) Group of Patients |
Collaterals
In our study, collaterals to the occluded artery were graded as poor collaterals for Grade 0,1,2 and rich collaterals for Grade 3 collaterals on coronary angiography. In group I, 11 (36.7%) patients had rich collaterals compared to 4 (13.3%) patients in group II. The difference was statistically significant (p=0.037), with stable patients having significantly better collaterals than unstable patients (Table 2).
Site of Occlusion and Collaterals
While comparing the level of LAD occlusion with grades of collateral, it was observed that 26 (68.4%) and 12 (31.6%) patients each with proximal LAD occlusion had poor and rich collaterals, respectively, whereas 19 (86.4%) and 3 (13.6%) patients each with non-proximal LAD occlusion had poor and rich collaterals respectively. Therefore, comparatively, a greater number of patients with proximal LAD occlusion had rich collaterals as compared to non-proximal occlusion; however, the results were not statistically significant (p=0.122). (Table 3)
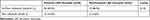 |
Table 3 Correlation Between Grade of Collaterals and Site of LAD Occlusion |
Viable Myocardium
In the stable group, the percentage of viable myocardium was seen in numerically higher number of patients with proximal LAD occlusion than the non-proximal LAD occlusion. However, the difference was not statistically significant (p=0.060). Similarly, the percentage of non-viable myocardium and site of LAD occlusion also did not reveal any statistical significance (p=0.189). (Table 4) The results showed a trend towards significance but did not meet the desired endpoints. This could be explained on the basis of the fact that only a small number (17/30) of patients in the hemodynamically stable (I) group underwent PET scan for viability assessment. The viability assessment could not be done in the unstable group (II) as these patients underwent immediate coronary revascularisation after angiography.
 |
Table 4 Correlation of Myocardial Viability with Site of LAD Occlusion |
Discussion
Anterior wall STEMI has been associated with worse short- and long-term outcomes compared to any other MI. Despite the usage of fibrinolytic, finding a completely occluded artery on angiography is not uncommon in our setting.18 Acute occlusion of LAD tends to cause hemodynamic deterioration, but some patients remain stable despite proximal occlusion. Whereas hemodynamically unstable STEMI patients often require urgent revascularisation, uncertainty exists regarding the opening of an occluded artery in a stable patient, especially after 24 hours of onset. Why patients with similar angiographic profiles vary vastly in terms of hemodynamic status remains to be answered. Although there are few studies on individual parameters associated with hemodynamic stability in acute STEMI, we could not find any published study correlating various clinical and angiographic parameters with presenting hemodynamic status in STEMI patients with total occlusion culprit vessel.
Accordingly, the present study evaluated various clinical parameters (like age, gender, diabetes mellitus, hypertension, smoking, troponin T level, LV dysfunction) and angiographic parameters (like the site of coronary artery occlusion, grades of collateral and angiographic parameters) with the hemodynamic status of patients presenting with acute anterior wall STEMI and occluded LAD. Interestingly, we identified some factors reflecting hemodynamic stability/instability among these patients. Early identification of high-risk features can guide treatment strategies, predict clinical course and outcomes, and reduce morbidity and mortality from the disease.
Clinical Parameters and Hemodynamic Stability
Diabetes Mellitus
Diabetes mellitus poses an increased risk of developing multivessel disease and hemodynamic instability. In a study by Lin et al, on 1676 patients with CAD, patients with diabetes had the highest rates of all-cause mortality and cardiovascular mortality (p<0.001).19 However, in the present study of patients with single-vessel disease, 4 (13.3%) patients in the hemodynamically stable group and 12 (40%) patients in the hemodynamically unstable group had diabetes. More patients with diabetes mellitus developed hemodynamic instability with a statistically significant difference (p=0.020), signifying the effect of diabetes on hemodynamic status in STEMI patients even in the presence of single-vessel disease. Structural changes of microcirculation and endothelial dysfunction may be the contributory factors in patients with diabetes mellitus. On the other hand, the effect of diabetes on coronary collateral growth is controversial. In a study by Zbinden et al, the coronary collateral flow does not differ between diabetic and non-diabetic patients with stable CAD, although data in patients with ACS is limited.20 Another reason for worse outcomes in patients with diabetes is the frequent presentation with atypical symptoms, leading to delays in treatment initiation.21
LV Dysfunction
A study by Klein et al reported a significant association between severe LV systolic dysfunction (EF<35%) and hemodynamic instability as compared to EF>35% (p<0.0001).10 In addition to being a strong predictor for hemodynamic instability in acute STEMI, LVEF of <35% is also associated with increased mortality.22 In our study, 12 (40%) and 21 (70%) patients, respectively, in the hemodynamically stable and unstable group, had an ejection fraction of less than 35%. Further, a higher number of patients with severe LV systolic dysfunction were hemodynamically unstable than the stable population, and the difference was statistically significant (p=0.02). Therefore, it can be concluded that the presence of severe left ventricular systolic dysfunction is associated with hemodynamic instability in anterior wall STEMI patients who have total occlusion of LAD.
Quantitative Troponin T Level
Troponin level in ACS may be markedly elevated, especially if associated with reduced left ventricular systolic function and hemodynamic instability. Additionally, higher Troponin T levels reflect higher mortality in such patients.23 In a study by Ohman et al, elevated Troponin T level was strongly associated with 30-day mortality (p<0.001).24 Similarly, in our study, elevated Troponin T level was associated with hemodynamic instability compared to the stable group, and the difference was statistically significant (p= <0.0001). Hence, our study reiterates that the degree of troponin elevation is linearly related to the amount of myocardial damage and reflects presenting hemodynamics in anterior wall STEMI and a totally occluded LAD.
Age
In the present study, the mean age of presentation was 51.07±13.78 years in the hemodynamically stable group and 55.47±11.69 years in the hemodynamically unstable group. Although advanced age has been associated with increased incidence of cardiogenic shock and subsequent mortality in some studies,4 our result did not show a statistically significant association between the age of the patients and hemodynamic stability (p-value= 0.188). This finding could be explained by the small sample size and inclusion of patients with single-vessel disease, which excludes most of the elderly.
Gender
Although a survey by Rosengren et al on 10,253 patients with ACS revealed a statistically higher number of men presented with STEMI as compared to women (p<0.0001),25 literature points to worse outcomes in females compared to men after STEMI, mainly due to delayed presentation, higher comorbidities, advanced age and also less utilization of reperfusion strategies.26 With 73.3% men and 26.66% women, the results of our study corroborate the survey findings, but the correlation between gender and hemodynamic stability was not statistically significant (p-value=0.243)
Smoking and Hypertension
Our study found no significant association between hemodynamic status at presentation and smoking (p-value =0.781) or history of hypertension (p-value =1.00) in anterior wall STEMI patients with totally occluded LAD.
Angiographic Parameters and Hemodynamic Stability
Site of Total LAD Occlusion
Anterior wall STEMI caused by left-main occlusion or proximal LAD occlusion carries an increased risk of mortality compared to mid- or distal LAD occlusion as it supplies a large area of the myocardium. Hemodynamic instability is directly proportional to the proximity of LAD occlusion.27 In our study, 20 (66.7%) patients had LAD occlusion in the proximal segment, and 10 (33.3%) patients had in the non-proximal segment in the hemodynamically stable group, whereas LAD occlusion was proximal in 18 (60%) patients and non-proximal in 12 (40%) patients in the hemodynamically unstable group. Overall, our data did not reveal a significant association between the site of total LAD occlusion and hemodynamic status (p value=0.592). Although theoretically, we expected a significant relationship between the site of LAD occlusion and hemodynamic status, this study may not be conclusive due to the small sample size. The other hypothetical explanation may be the presence of better collaterals with proximal LAD occlusion, good enough to sustain viability and hemodynamic stability compared to the distil occlusion. However, a more extensive study is required to address the issue conclusively.
Grades of Collateral
Some pre-existing data suggest that in acute STEMI patients with significant coronary artery occlusion, the presence of collateral circulation provides hemodynamic stability as compared to the absence of collaterals.12 Out of 30 patients in our hemodynamically stable group, 11 (36.7%) had rich collaterals, and 19 (63.3%) had no/poor collaterals on coronary angiography. On the other hand, in the hemodynamically unstable group, only 4 (13.3%) patients had rich collaterals, and 26 (86.7%) had no/poor collaterals, and the overall difference was statistically significant (p value=0.037). Thus, the presence of better collateral supply to the culprit artery sustains better hemodynamically stability during acute occlusion than the ones with inadequate collateral supply. In one similar study done by Wang et al, even the mortality was lower in patients with collateral circulation as compared to those without collateral circulation (1% vs 8%, P =0.049).28
Myocardial Viability and Site of Total LAD Occlusion
In a study by Fukai et al, it was found that the presence of coronary collaterals contributes to minimize the infarct size and predict the presence of viable myocardium in patients with myocardial infarction.29 In contrast, another study by Dong et al found no significant correlation was found between the severity and the extent of perfusion defect, viability of the myocardium as well as the grade of collateral circulation. Thus, collaterals on angiography do not seem to be an effective way to predict the viability of the myocardium.30 Due to the limited number of patients with an assessment of myocardial viability having collateral circulation, a meaningful analysis was not possible in our study. Instead, we compared myocardial viability with the site (proximal and non-proximal) of occlusion and found a numerically higher amount of viable myocardium with the proximal site of occlusion (mean of 25.8±11%) as compared to non-proximal occlusion (mean of 12.0±2.0%); however, it did not reach statistical significance (p-value=0.060). Similarly, the percentage of non-viable myocardium with a mean of 32.50±11.35 with proximal occlusion and a mean of 19.0±1.41 with non-proximal occlusion did not reveal any statistical significance (p value=0.189). The observed numerical difference in the percentage of viable or non-viable myocardium, although not significant, may be hypothetically due to the availability of more sites for collateral circulation in proximal than non-proximal occlusion. Possibly patients with proximal occlusion and rich collaterals tend to retain more viable myocardium than distal occlusion. Similarly, patients with proximal occlusion and poor collaterals suffer more non-viable myocardium than distal LAD occlusion. However, our study does not provide a statistically significant association between the site of total LAD occlusion and myocardial viability. A larger study is required to support this assumption.
Limitations
This is a single-centre observational study with a small sample size. Further, its results are limited to STEMI patients with complete occlusion of culprit vessel and may not be generalizable to all populations. Furthermore, only half of the patients in the hemodynamically stable group underwent PET for viability assessment because of logistic reasons. Also, a multivariate regression analysis could not be performed to evaluate the role of confounding factors on the final results. Finally, as ours is a tertiary care referral institute, we cannot rule out the selection bias with more unstable patients being referred to us. A more extensive study with a post-hoc sample size calculation to overcome the above limitations is required to obtain a conclusive evidence.
Conclusions
The present study showed that diabetes, severe LV systolic dysfunction, elevated Troponin T level, and poor collateralization are more commonly associated with hemodynamic instability, whereas the presence of better collaterals predicted hemodynamic stability in the anterior wall STEMI patients with total occlusion of LAD. We found no significant association between age of the patient, gender, smoking, hypertension, site of total LAD occlusion, and hemodynamic status. Furthermore, despite a favourable trend, no significant association was observed between the myocardial viability and site of LAD occlusion.
Guarantor of Submission
The corresponding author is the Guarantor of Submission.
Acknowledgment
No research support was sought from any commercial agency related directly or indirectly with the outcome of the study.
Funding
There is no funding to report.
Disclosure
The authors declare no conflicts of interest for this work and that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
1. World Health Organization. Cardiovascular diseases (CVDs) [Fact sheet]; 2017 [cited March 01, 2021]. Available from: https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds).
2. Prabhakaran D, Jeemon P, Roy A. Cardiovascular diseases in India: current epidemiology and future directions. Circulation. 2016;133(16):1605–1620. doi:10.1161/CIRCULATIONAHA.114.008729
3. Elsman P, van ‘T Hof AW, Hoorntje JC, et al. Effect of coronary occlusion site on angiographic and clinical outcome in acute myocardial infarction patients treated with early coronary intervention. Am J Cardiol. 2006;97(8):1137–1141. doi:10.1016/j.amjcard.2005.11.027
4. Hochman JS, Boland J, Sleeper LA, et al. Current spectrum of cardiogenic shock and effect of early revascularization on mortality. Results of an International Registry. SHOCK Registry Investigators. Circulation. 1995;91(3):873–881. doi:10.1161/01.CIR.91.3.873
5. Lindholm MG, Køber L, Boesgaard S, Torp-Pedersen C, Aldershvile J; Trandolapril Cardiac Evaluation study group. Cardiogenic shock complicating acute myocardial infarction; prognostic impact of early and late shock development. Eur Heart J. 2003;24(3):258–265. doi:10.1016/S0195-668X(02)00429-3
6. Hamm CW, Goldmann BU, Heeschen C, Kreymann G, Berger J, Meinertz T. Emergency room triage of patients with acute chest pain by means of rapid testing for cardiac troponin T or troponin I. N Engl J Med. 1997;337(23):1648–1653. doi:10.1056/NEJM199712043372302
7. Picard MH, Davidoff R, Sleeper LA, et al. SHould we emergently revascularize Occluded Coronaries for cardiogenic shocK. Echocardiographic predictors of survival and response to early revascularization in cardiogenic shock. Circulation. 2003;107(2):279–284. doi:10.1161/01.CIR.0000045667.11911.F6
8. Nguyen TL, French JK, Hogan J, et al. Prognostic value of high sensitivity troponin T after ST-segment elevation myocardial infarction in the era of cardiac magnetic resonance imaging. Eur Heart J Qual Care Clin Outcomes. 2016;2(3):164–171. doi:10.1093/ehjqcco/qcv033
9. Jolly SS, Shenkman H, Brieger D, et al. Quantitative troponin and death, cardiogenic shock, cardiac arrest and new heart failure in patients with non-ST-segment elevation acute coronary syndromes (NSTE ACS): insights from the Global Registry of Acute Coronary Events. Heart. 2011;97(3):197–202. doi:10.1136/hrt.2010.195511
10. Klein LW, Shaw RE, Krone RJ, et al. Mortality after emergent percutaneous coronary intervention in cardiogenic shock secondary to acute myocardial infarction and usefulness of a mortality prediction model. Am J Cardiol. 2005;96(1):35–41. doi:10.1016/j.amjcard.2005.02.040
11. Yaylak B, Altintas B, Ede H, et al. Impact of coronary collateral circulation on in-hospital death in patients with inferior ST elevation myocardial infarction. Cardiol Res Pract. 2015;2015:242686. doi:10.1155/2015/242686
12. Pérez-Castellano N, García EJ, Abeytua M, et al. Influence of collateral circulation on in-hospital death from anterior acute myocardial infarction. J Am Coll Cardiol. 1998;31(3):512–518. doi:10.1016/S0735-1097(97)00521-4
13. Hochman JS, Lamas GA, Buller CE, et al. Coronary intervention for persistent occlusion after myocardial infarction. N Engl J Med. 2006;355(23):2395–2407. doi:10.1056/NEJMoa066139
14. Ioannidis JP, Katritsis DG. Percutaneous coronary intervention for late reperfusion after myocardial infarction in stable patients. Am Heart J. 2007;154(6):1065–1071. doi:10.1016/j.ahj.2007.07.049
15. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–177. doi:10.1093/eurheartj/ehx393
16. Nathoe HM, Koerselman J, Buskens E, et al. Determinants and prognostic significance of collaterals in patients undergoing coronary revascularization. Am J Cardiol. 2006;98(1):31–35. doi:10.1016/j.amjcard.2006.01.050
17. Kilian JG, Keech A, Adams MR, Celermajer DS. Coronary collateralization: determinants of adequate distal vessel filling after arterial occlusion. Coron Artery Dis. 2002;13(3):155–159. doi:10.1097/00019501-200205000-00004
18. Mohanan PP, Mathew R, Harikrishnan S, et al. Presentation, management, and outcomes of 25 748 acute coronary syndrome admissions in Kerala, India: results from the Kerala ACS Registry. Eur Heart J. 2013;34(2):121–129. doi:10.1093/eurheartj/ehs219
19. Lin MJ, Chang YJ, Chen CY, Huang CC, Chuang TY, Wu HP. Influence of hypercholesterolemia and diabetes on long-term outcome in patients with stable coronary artery disease receiving percutaneous coronary intervention. Medicine (Baltimore). 2019;98(34):e16927. doi:10.1097/MD.0000000000016927
20. Zbinden R, Zbinden S, Billinger M, Windecker S, Meier B, Seiler C. Influence of diabetes mellitus on coronary collateral flow: an answer to an old controversy. Heart. 2005;91(10):1289–1293. doi:10.1136/hrt.2004.041236
21. Timmer JR, Ottervanger JP, de Boer MJ, et al. Primary percutaneous coronary intervention compared with fibrinolysis for myocardial infarction in diabetes mellitus: results from the Primary Coronary Angioplasty vs Thrombolysis-2 trial. Arch Intern Med. 2007;167(13):1353–1359. doi:10.1001/archinte.167.13.1353
22. Esmaeilzadeh M, Parsaee M, Maleki M. The role of echocardiography in coronary artery disease and acute myocardial infarction. J Tehran Heart Cent. 2013;8(1):1–13.
23. Al-Otaiby MA, Al-Amri HS, Al-Moghairi AM. The clinical significance of cardiac troponins in medical practice. J Saudi Heart Assoc. 2011;23(1):3–11. doi:10.1016/j.jsha.2010.10.001
24. Ohman EM, Armstrong PW, Christenson RH, et al. Cardiac troponin T levels for risk stratification in acute myocardial ischemia. GUSTO IIA Investigators. N Engl J Med. 1996;335(18):1333–1341. doi:10.1056/NEJM199610313351801
25. Rosengren A, Wallentin L, Gitt K, Behar S, Battler A, Hasdai D. Sex, age, and clinical presentation of acute coronary syndromes. Eur Heart J. 2004;25(8):663–670. doi:10.1016/j.ehj.2004.02.023
26. Zhang Z, Fang J, Gillespie C, Wang G, Hong Y, Yoon PW. Age-specific gender differences in in-hospital mortality by type of acute myocardial infarction. Am J Cardiol. 2012;109(8):1097–1103. doi:10.1016/j.amjcard.2011.12.001
27. Unai S, Tanaka D, Ruggiero N, Hirose H, Cavarocchi NC. Acute myocardial infarction complicated by cardiogenic shock: an algorithm-based extracorporeal membrane oxygenation program can improve clinical outcomes. Artif Organs. 2016;40(3):261–269. doi:10.1111/aor.12538
28. Wang B, Han YL, Li Y, et al. Coronary collateral circulation: effects on outcomes of acute anterior myocardial infarction after primary percutaneous coronary intervention. J Geriatr Cardiol. 2011;8(2):93–98. doi:10.3724/SP.J.1263.2011.00093
29. Fukai M, Ii M, Nakakoji T, et al. Angiographically demonstrated coronary collaterals predict residual viable myocardium in patients with chronic myocardial infarction: a regional metabolic study. J Cardiol. 2000;35(2):103–111.
30. Dong W, Li J, Mi H, Song X, Jiao J, Li Q. Relationship between collateral circulation and myocardial viability of 18F-FDG PET/CT subtended by chronic total occluded coronary arteries. Ann Nucl Med. 2018;32(3):197–205. doi:10.1007/s12149-018-1234-3
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
