Back to Journals » International Journal of Women's Health » Volume 15
Clear Cell Adenocarcinoma Arising from Endometriosis in Abdominal Wall Cesarean Section Scar: A Case Report and Literature Review
Authors Liu D, Wei H, Huang J, Shen H, Wang X, Hu C
Received 26 July 2022
Accepted for publication 17 December 2022
Published 5 January 2023 Volume 2023:15 Pages 25—32
DOI https://doi.org/10.2147/IJWH.S382235
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Dong Liu,1,* Huanhuan Wei,2,* Jinyu Huang,1 Hailin Shen,3 Ximing Wang,1 Chunhong Hu1
1Radiological Department, The First Affiliated Hospital of Soochow University, Suzhou, People’s Republic of China; 2Academy of Medical Sciences, the People’s Hospital of Zhengzhou University, Zhengzhou, Henan, People’s Republic of China; 3Department of Radiology, Suzhou Kowloon Hospital, Shanghai Jiaotong University School of Medicine, Suzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Chunhong Hu, Email [email protected]
Background: Endometriosis developing in a cesarean section (CS) scar is an unusual event. Malignant transformation arising on the background of scar endometriosis in the abdominal wall is extremely rare. Herein we report a case of clear cell carcinoma (CCC) arising in the abdominal wall from endometriosis tissues following CS and review previous literature.
Case Presentation: A 48-year-old gravida 2 para 1 female presented with an abdominal wall mass at her CS scar, which increased in size and became painful in the last 2 years. Physical examination showed a multilocular solid mass of about 13 cm, at the previous CS scar. Computed tomography (CT) and magnetic resonance imaging (MRI) revealed a 12.8cm × 7.7cm multi-septate cystic lesion on the anterior abdominal wall, and histological examination showed that CCC was caused by the transformation of abdominal wall endometriosis (AWE).
Conclusion: An endometriosis-associated malignancy should be considered in the differential with any enlarging mass in the abdominal wall scar.
Keywords: cesarean section, abdominal wall endometriosis, case report
Introduction
Endometriosis is an inflammatory disorder featured by the existence of normal endometrial glands and extrauterine matrix.1 These pathological changes usually involve the ovaries and, more rarely, ureter, intestine, lung, and abdominal wall.1,2 AWE patients usually have a history of gynecological operation with open uterine cavity.
The incidence rate of abdominal surgical scar endometriosis ranges from 0.03% to 1.08% of women undergoing pelvic surgery.2–4 Women usually account of a periodic menstrual pain, which refers to abdominal wall.
Endometriosis is supposed to a benign disease, and malignant transformation is rare. About 80% of endometriosis-related malignant tumors occur in the ovary, while 20% are limited to extragonadal sites.5 CCC arising from malignant transformation of endometriosis in the abdominal wall after CS is a very rare clinical condition, and the published literature about this subject is frail. Here, we report a case of CCC arising from the abdominal wall at the previous CS scar. In addition, we reviewed the literature on this unusual event.
Case Presentation
A 48-year-old gravida 2 para 1 female presented with progressively growing mass of cesarean scar, regular pain with menstruation for 15 years. She had a caesarean delivery 22 years ago. Seven years after the operation, she noticed a 2cm × 2cm nodule beside the abdominal scar, red, with slight pain during menstruation. The nodule grew rapidly, and the pain became more serious in the previous 2 years. She complained her troubles of severe dysmenorrhea on the first day of the menstrual period, accompanied by abdominal pain and deep pain in the site of uterine scar, with an intensity of six on the pain scale (6/10). There were no gynecological malignancies in her family history, and she had never received hormone therapy.
Physical examination indicated a 13cm mass with multilocular originating from the previous surgical scar without tenderness, red, ulcer with bloody secretions, surrounded by erythema.
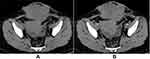
Abdomino-pelvic CT scan and MRI confirmed a lobular, peripherally enhancing lesion in the rectus muscle sheath, extending to the skin surface within the abdominal wall, with images suggestive of internal septation. It measured around 12.8cm × 7.7cm along the major transverse, anteroposterior and longitudinal axes, respectively (Figures 1 and 2), without any abnormalities in the abdominal cavity.
Laboratory findings: tumor marker CA 125 was 164.7 U/mL (the reference range: 0–35 U/mL); her cancer antigen 19–9, α-fetoprotein, and carcinoembryonic antigen were within the reference range.
A punch biopsy of the mass showed CCC, without benign endometriosis presented (Figure 3) (Immunophenotype: CK+, CK7+, CK20-, CD99-, HNF1b+, Napsin A (+)). Suggesting, CCC arising from endometriosis of the abdominal wall.
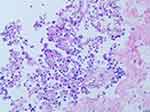 |
Figure 3 Histologically, Hematoxylin and eosin stain, magnification×200 shows typical clear-cell carcinoma with typical tubulocystic and papillary architectures. |
The patient underwent exploratory laparotomy, and found an irregular, cystic and solid mass deep in the rectus muscle of the midline. Extensive resection of the abdominal wall mass was performed with mesh reconstruction of the abdominal wall. The resected specimen was a lobulated mass with a maximum size of 13cm, accompanied by focal hemorrhage and necrosis. It was composed of microcystic spaces, involving the dermis, subcutaneous and skeletal muscle. The pathologic results of the uterus and bilateral accessories (ovary and fallopian tube) were negative.
Microscopic examination of the tumor showed similar histopathology to the biopsy.
The patient underwent six cycles of cisplatinum-based chemotherapy and adjuvant radiotherapy to the abdomen. Twelve months of follow-up, there was no further evidence of disease by imaging or clinical examination.
Discussion
Malignancy arising in association with endometriosis is quite rare. The incidence of abdominal surgical scar endometriosis in women undergoing pelvic surgery ranges between 0.3% and 1% (5), and these cases include endometrioid carcinoma (70%), sarcoma (25%) and CCC (5%), of which abdominal wall CCC due to endometriosis is a rare disease reported in the literature (6).
CCC caused by malignant transformation of AWE after CS is a rare clinical condition. Although rare, the number of reported cases has increased in recent years (7), possibly owing to the increased rates of CS and conservative uterine surgery worldwide (7).
Sampson and John6 proposed three diagnostic criteria for the malignant tumors arising in endometriosis as follows: (i) demonstration of benign and malignant endometrial tissues in the tumor, (ii) the histological type consistent with the origin of endometrium, and (iii) no other primary tumor sites were found. Moreover, Mostoufizadeh et al7 stated that the plain coexistence of tumor and endometriotic tissue is enough to prove the derivation of the endometriosis. According to the literature, even if the presence of endometriosis is the pathological diagnosis of the disease, only 36–42% of cases detected in the transition zone.8
To the best of our knowledge, to date, there are limited literature studies on CCC caused by abdominal wall scarring, and we retrospectively listed and analyzed 12 typical ones (including the present case) (Table 1). In these studies, the average reported age at diagnosis was 45.7 years old, while the mean size of the lesion was 10.9 cm. The literature review showed that 91.7% of cases had a history of CS. The average follow-up time was around 15 months, and about 25% of women died within 15 months of diagnosis. The great majority (our case was included) of cases arose from CS scars, with some exceptions: one case followed myomectomy,9 one case followed hysterotomy,10 and one followed open sterilization.11 All of these procedures would allow endometrium to implant at the surgical incision site. Histological examination showed that more than 66.7% of cases revealed endometriotic tissue. But in our tissue sampling, there was no histological evidence of coexisting endometriosis, either in the peritoneal cavity or in the previous surgical-scar tissue. There are two explanations: 1) all endometrial lesions or ectopic endometrial tissues have been transformed into CCC; 2) primary CCC originated from the abdominal wall scar. In our case, the mass localized to the area of the cesarean scar, which was accompanied by regular pain with menstruation for 15 years, suggesting endometriosis. Therefore, we presumed that CCC was transformed by the pre-existing abdominal-wall endometriosis.
 |
Table 1 Cases of CCC Arising from Abdominal Wall Scar (N = 39) |
The available case reports in the literature differ in terms of disease-free survival and mortality, which may be related to the timing of diagnosis, the extent of tumor burden and its resectability at the time of diagnosis, as well as different therapeutic effects. Reported cases have been treated with radical resection of the tumor with or without the addition of variable chemotherapeutic and radiotherapy regimens. Due to the low incidence rate, it is difficult to generalize the outcomes or to conduct randomized controlled trials to standardize treatment protocols.
Conclusion
Malignant transformation to CCC on the abdominal wall from a focus of endometriosis is a very rare case. For middle-aged women with a history of gynecologic or obstetric surgery, developing an abdominal wall mass, the possibility of a primary malignancy arising from endometriosis should be considered. Due to its rarity, there is no published treatment guideline at present. From the perspective of prevention, it must be stressed that every gynecological operation should be carried out with great care not to leave visible tissue residues on the abdominal wall.
Abbreviations
CS, cesarean section; CCC, clear cell carcinoma; CT, computed tomography; MRI, magnetic resonance imaging; AWE, abdominal wall endometriosis.
Data Sharing Statement
This case report contains clinical data from the medical records in the First Affiliated Hospital of Soochow University. Additional information is available from the first author upon reasonable request.
Ethics Approval and Informed Consent
Writing and publishing this case report was approved by First Affiliated Hospital of Soochow University.
Consent Statement
Written informed consent for publication of details was obtained from the patient.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Johnson NP, Hummelshoj L, Abrao MS. Consensus on current management of endometriosis. Hum Reprod. 2013;28(6):1552–1568. doi:10.1093/humrep/det050
2. Hasan A, Deyab A, Monazea K, et al. Clinico-pathological assessment of surgically removed abdominal wall endometriomas following cesarean section. Ann Med Surg. 2021;62:219–224. doi:10.1016/j.amsu.2021.01.029
3. Francica G. Reliable clinical and sonographic findings in the diagnosis of abdominal wall endometriosis near cesarean section scar. World J Radiol. 2012;4:135. doi:10.4329/wjr.v4.i4.135
4. Kocakusak A, Arpinar E, Arikan S, Demirbag N, Tarlaci A, Kabaca C. Abdominal wall endometriosis: a diagnostic dilemma for surgeons. Med Princ Pract. 2005;14(6):434–437. doi:10.1159/000088118
5. Fehm T, Krawczyk N, Ulrich U, et al. Endometriosis-associated Malignancy. Geburtshilfe Frauenheilkd. 2016;76(2):176–181. doi:10.1055/s-0035-1558239
6. Sampson JA. Endometrial carcinoma of the ovary, arising in endometrial tissue in that organ. Am J Obstet Gynecol. 1925;9(1):111–114. doi:10.1016/S0002-9378(25)90949-0
7. Mostoufizadeh M, Scully RE. Malignant tumors arising in endometriosis. Clin Obstet Gynecol. 1980;23(3):951. doi:10.1097/00003081-198023030-00024
8. Benoit L, Arnould L, Cheynel N, et al. Malignant extraovarian endometriosis: a review. Eur J Surg Oncol. 2006;32(1):6–11. doi:10.1016/j.ejso.2005.08.011
9. Won PS, Mie HS, Gyun WH, Whan HS. Clear cell carcinoma arising in a Cesarean section scar endometriosis: a case report. J Korean Med Sci. 1999;14(2):217–219. doi:10.3346/jkms.1999.14.2.217
10. Miller DM, Schouls JJ, Ehlen TG. Clear cell carcinoma arising in extragonadal endometriosis in a caesarean section scar during pregnancy. Gynecol Oncol. 1998;70(1):127. doi:10.1006/gyno.1998.4989
11. Harry VN, Shanbhag S, Lyall M, Narayansingh GV, Parkin DE. Isolated clear cell adenocarcinoma in scar endometriosis mimicking an incisional hernia. Obstet Gynecol. 2007;110(2):469–471. doi:10.1097/01.AOG.0000260393.46154.5f
12. Schnieber D, Wagner-Kolb D. Maligne entartung einer extragenitalen endometriose. Geburtshilfe Frauenheilkd. 1986;46(09):658–659. doi:10.1055/s-2008-1036277
13. Hitti IF, Glasberg SS, Lubicz S. Clear cell carcinoma arising in extraovarian endometriosis: report of three cases and review of the literature. Gynecol Oncol. 1990;39(3):314–320. doi:10.1016/0090-8258(90)90259-N
14. Ishida GM, Motoyama T, Watanabe T, Emura I. Clear cell carcinoma arising in a cesarean section scar. Report of a case with fine needle aspiration cytology. Acta Cytol. 2003;47(6):1095–1098. doi:10.1159/000326655
15. Sergent F, Baron M, Le Cornec J, Scotté M, Mace P, Marpeau L. Malignant transformation of abdominal wall endometriosis: a new case report. J Gynecol Obstet Biol Reprod (Paris). 2006;35(2):186–190. doi:10.1016/S0368-2315(06)76394-3
16. Alberto V, Lynch M, Labbei F, Jeffers M. Primary abdominal wall clear cell carcinoma arising in a Caesarean section scar endometriosis. Ir J Med Sci. 2006;175(1):69–71. doi:10.1007/BF03169006
17. Razzouk K, Roman H, Chanavaz-Lacheray I, Scotté M, Verspyck E, Marpeau L. Mixed clear cell and endometrioid carcinoma arising in parietal endometriosis. Gynecol Obstet Invest. 2007;63(3):140–142. doi:10.1159/000096437
18. Bats AS, Zafrani Y, Pautier P, Duvillard P, Morice P. Malignant transformation of abdominal wall endometriosis to clear cell carcinoma: case report and review of the literature. Fertil Steril. 2008;90(4):1197.e13–e16... doi:10.1016/j.fertnstert.2007.08.080
19. Rust MM, Susa J, Naylor R, Cavuoti D. Clear cell carcinoma in a background of endometriosis. Case report of a finding in a midline abdominal scar 5 years after a total abdominal hysterectomy. Acta Cytol. 2008;52(4):475–480. doi:10.1159/000325557
20. Thouraya A, Soumaya R, Amel T, et al. Clear cell adenocarcinoma arising from abdominal wall endometriosis. Oncology. 2008;2008:1–3. doi:10.1155/2008/478325
21. Matsuo K, Alonsozana ELC, Eno ML, Rosenshein NB, Im DD. Primary peritoneal clear cell adenocarcinoma arising in previous abdominal scar for endometriosis surgery. Arch Gynecol Obstet. 2009;280(4):637–641. doi:10.1007/s00404-009-0962-y
22. Williams C, Petignat P, Belisle A, Drouin P. Primary abdominal wall clear cell carcinoma: case report and review of literature. Anticancer Res. 2009;29(5):1591–1593.
23. Bourdel N, Durand M, Gimbergues P, Dauplat J, Canis M. Exclusive nodal recurrence after treatment of degenerated parietal endometriosis. Fertil Steril. 2010;93(6):2074.e1–e6... doi:10.1016/j.fertnstert.2009.11.004
24. Yan Y, Li L, Guo J, Zheng Y, Liu Q. Malignant transformation of an endometriotic lesion derived from an abdominal wall scar. Int J Gynecol Obstet. 2011;115(2):202–203. doi:10.1016/j.ijgo.2011.06.018
25. Shalin SC, Haws AL, Carter DG, Zarrin‐Khameh N. Clear cell adenocarcinoma arising from endometriosis in abdominal wall cesarean section scar: a case report and review of the literature. J Cutan Pathol. 2012;39(11):1035–1041. doi:10.1111/j.1600-0560.2012.01982.x
26. Mert I, Semaan A, Kim S, Ali-Fehmi R, Morris RT. Clear cell carcinoma arising in the abdominal wall: two case reports and literature review. Am J Obstet Gynecol. 2012;207(2):e7–e9. doi:10.1016/j.ajog.2012.05.029
27. Sawazaki H, Goto H, Takao N, Taki Y, Takeuchi H. Clear cell adenocarcinoma arising from abdominal wall endometriosis mimicking urachal tumor. Urology. 2012;79(6):e84–e5. doi:10.1016/j.urology.2011.02.034
28. Li X, Yang J, Cao D, Lang J, Chen J, Shen K. Clear-cell carcinoma of the abdominal wall after cesarean delivery. Obstet Gynecol. 2012;120:445–448.
29. Dobrosz Z, Paleń P, Stojko R, Właszczuk P, Niesłuchowska-Hoxha A, Piechuta-Kośmider I. Clear cell carcinoma derived from an endometriosis focus in a scar after a caesarean section–a case report and literature review. Ginekol Pol. 2014;85:10. doi:10.17772/gp/1683
30. Ijichi S, Mori T, Suganuma I, et al. Clear cell carcinoma arising from cesarean section scar endometriosis: case report and review of the literature. Case Rep Obstet Gynecol. 2014;2014:642483. doi:10.1155/2014/642483
31. Heller DS, Houck K, Lee ES, Granick MS. Clear cell adenocarcinoma of the abdominal wall: a case report. Int J Reprod Med. 2014;59(5–6):330–332.
32. Liu H, Leng J, Lang J, Cui Q. Clear cell carcinoma arising from abdominal wall endometriosis: a unique case with bladder and lymph node metastasis. World J Surg Oncol. 2014;12(1):1–6. doi:10.1186/1477-7819-12-51
33. Aust S, Tiringer D, Grimm C, Stani J, Langer PM. Therapy of a clear cell adenocarcinoma of unknown primary arising in the abdominal wall after cesarean section and after hysterectomy. Wien Klin Wochenschr. 2015;127(1):62–64. doi:10.1007/s00508-014-0619-0
34. Paula RM, Lewis WD, Thomas CM. Transformation of abdominal wall endometriosis to clear cell carcinoma. Case Rep Obstet Gynecol. 2015;2015:123740. doi:10.1155/2015/123740
35. Sosa-Durán EE, Aboharp-Hasan Z, Mendoza-Morales RC, García-Rodríguez FM, and Jiménez-Villanueva X. Adenocarcinoma de células claras originado de endometriosis en pared abdominal [Clear cell adenocarcinoma arising from abdominal wall endometriosis]. Cir Cir. 2016;84(3):245–249. Spanish. doi:10.1016/j.circir.2015.05.050
36. Ferrandina G, Palluzzi E, Fanfani F, et al. Endometriosis-associated clear cell carcinoma arising in caesarean section scar: a case report and review of the literature. World J Surg Oncol. 2016;14(1):1–8. doi:10.1186/s12957-016-1054-7
37. Graur F, Mois E, Elisei R, Furcea L, Hajjar NA. Malignant endometriosis of the abdominal wall. Ann Ital Chir. 2017;6:4.
38. Wei C-J, Huang S-H. Clear cell carcinoma arising from scar endometriosis: a case report and literature review. Tzu Chi Med J. 2017;29(1):55. doi:10.4103/tcmj.tcmj_11_17
39. Marques C, Silva TS, Dias MF. Clear cell carcinoma arising from abdominal wall endometriosis – brief report and review of the literature. Gynecol Oncol Rep. 2017;20:78–80. doi:10.1016/j.gore.2017.03.008
40. Almeida G, Renato M, Neubaner K, et al. Malignant transformation of abdominal wall endometriosis to clear cell carcinoma: case report. Sao Paulo Med J. 2017;136:586–590.
41. Lopes A, Anton C, Slomovitz BM, Mattos L, Carvalho FM. Clear cell carcinoma arising from abdominal wall endometrioma after cesarean section. Int J Gynecol Cancer. 2019;29(8):1332. doi:10.1136/ijgc-2019-000808
42. Sadikah B, Paul M, Longwen C, et al. Clear cell carcinoma of the anterior abdominal wall secondary to iatrogenic endometriosis. J Minim Invasive Gynecol. 2019;27(6):1230.
43. Rolon M, Allen D, Richardson G, Clement C. Abdominal wall clear cell carcinoma: case report of a rare event with potential diagnostic difficulties. Case Rep Pathol. 2019;2019(5):1–7. doi:10.1155/2019/1695734
44. Giannella L, Serri M, Maccaroni E, Giuseppe JD, Ciavattini A. Endometriosis-associated clear cell carcinoma of the abdominal wall after caesarean section: a case report and review of the literature. In vivo. 2020;34(4):2147–2152. doi:10.21873/invivo.12021
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.