Back to Journals » Integrated Pharmacy Research and Practice » Volume 5
Chronic care model in primary care: can it improve health-related quality of life?
Authors Aryani F, Lee S , Chua SS , Kok LC, Efendie B, Thomas P
Received 15 July 2015
Accepted for publication 16 November 2015
Published 19 January 2016 Volume 2016:5 Pages 11—17
DOI https://doi.org/10.2147/IPRP.S92448
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Jonathan Ling
Faridah Md Yusof Aryani,1 Shaun Wen Huey Lee,2 Siew Siang Chua,3 Li Ching Kok,4 Benny Efendie,2 Thomas Paraidathathu5
1Pharmaceutical Services Division, Ministry of Health Malaysia, Petaling Jaya, 2School of Pharmacy, Monash University Malaysia, Bandar Sunway, 3Department of Pharmacy, Faculty of Medicine, University of Malaya, 4Clinical Research Centre, Kuala Lumpur Hospital, Kuala Lumpur, 5School of Pharmacy, Taylor’s University, Subang Jaya, Selangor, Malaysia
Purpose: Chronic diseases such as hypertension, diabetes mellitus, and hyperlipidemia are public health concerns. However, little is known about how these affect patient-level health measures. The aim of the study was to examine the impact of a chronic care model (CCM) on the participant’s health-related quality of life (QoL).
Patients and methods: Participants received either usual care or CCM by a team of health care professionals including pharmacists, nurses, dietitians, and general practitioners. The participants in the intervention group received medication counseling, adherence, and dietary advice from the health care team. The QoL was measured using the EQ-5D (EuroQoL-five dimension, health-related quality of life questionnaire) and comparison was made between usual care and intervention groups at the beginning and end of the study at 6 months.
Results: Mean (standard deviation) EQ-5D index scores improved significantly in the intervention group (0.92±0.10 vs 0.95±0.08; P≤0.01), but not in the usual care group (0.94±0.09 vs 0.95±0.09; P=0.084). Similarly, more participants in the intervention group reported improvements in their QoL compared with the usual care group, especially in the pain/discomfort and anxiety/depression dimensions.
Conclusion: The implementation of the CCM resulted in significant improvement in QoL. An interdisciplinary team CCM approach should be encouraged, to ultimately result in behavior changes and improve the QoL of the patients.
Keywords: diabetes mellitus, hypertension, hyperlipidemia, quality of life, EQ-5D
Introduction
Diabetes mellitus, cardiovascular, and chronic kidney diseases are the major causes of mortality, and the prevalence of these diseases is increasing worldwide.1 Despite established national and international clinical guidelines as well as effective pharmacotherapy,2–4 the management of these major diseases remains suboptimal. This situation is a major concern for Malaysia, where these diseases have reached epidemic proportions.5 The data from the recently concluded National Health and Morbidity survey showed that the prevalence of hypertension had increased from 32.2% in 2006 to 32.7% in 2011 for those aged 18 years and above. Similarly, the prevalence of diabetes has also increased by 31% in 5 years, from 11.6% in 2006 to 15.2% in 2011 and hyperlipidemia from 20.6% in 2006 to 35.1% in 2011 in those aged 18 years and above.5,6
Therefore, creative solutions are required to address the increasing health care demand of noncommunicable disease in the country. There is growing evidence worldwide suggesting the integration of health care that provides patient-centered care, such as the chronic care model (CCM) is a feasible solution to this problem.7,8 The CCM is an evidence-based framework that advocates evidence-based health care system changes especially in primary care setting needed to improve the patient outcomes.9,10 In the current study, five of the six key components of CCM were used namely: patient empowerment and self-management support; delivery system design; decision support; clinical information systems, and finally community resources.
We recently conducted a study examining the use of this model in single as well as multiple chronic diseases. The primary prevention program, known as the Community Based Multiple Risk Factors Intervention Strategy (CORFIS) was a prospective, open label, multi-center, cluster-randomized study encompassing the services of general practitioners (GPs), pharmacists, nurses as well as dietitians, working together with 784 participants to improve their health outcomes by providing health education, medication counseling, treatment adherence as well as diet plan. Due to the popularity of CCM as a conceptual tool for quality improvement and health care reorganization, there is a need to determine if such interdisciplinary team approach produces better health status outcome. The objective of this study was to assess the impact of the CCM program on patient health-related quality of life (QoL).
Patients and methods
Study design and setting
This study was part of a larger community-based, controlled study, which has been described earlier.11,12 Briefly, GPs from the Klang valley were invited to participate in recruiting the patients for this study.13 Participating GP clinics were subsequently allocated to either intervention or control in a 2:1 ratio. Any participants aged 18 years and above, diagnosed with either one or more of the following diseases: hypertension, diabetes mellitus, or hyperlipidemia, and treated with pharmacotherapy for one or more of these conditions were eligible for inclusion in the study. All the participants provided written informed consent. Ethical approval was obtained from the Medical Research Ethics Committee, Ministry of Health, Malaysia (NMRR-07-688-960). Trial registration: ClinicalTrials.gov, NCT00490672.
Study procedures
The participants allocated to the intervention cluster were required to attend a monthly check-up during the 6-month follow-up study period, with assessments by the pharmacist who reviewed the participants’ medications and provided counseling on adherence, medication knowledge as well as conducted medication reconciliation of existing prescription medications; dietitians who provided dietary advice including calorie calculations and the importance of regular exercise; and nurses who educated the participants on general health care issues such as the use of a glucose meter and foot care. Participants’ sociodemographic data, lifestyle, medical, and medication history were collected at baseline. In addition, the health-related QoL of each participant was assessed using the EQ-5D (EuroQoL-five dimension, health-related quality of life questionnaire) at baseline and at the end of the 6-month study period.
Outcome measures
The EQ-5D instrument is a standard instrument for measuring health outcome and has been validated for use in the Malaysian population.14,15 This instrument provides a simple descriptive profile and a single index value for assessing health status. It comprises of five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) with three levels of measurement each (no problems, some problems, and severe problems). It has been used in several studies to assess the QoL of patients with diabetes,16–18 hypertension,18–20 and hyperlipidemia.18 The raw values obtained from the dimension scales were subsequently converted into the Malaysian EQ-5D index tariff to obtain an overall health index score, with higher values representing better QoL. This ranges between 0 (represents death) and 1.0 (represents perfect health status).21 The patients also completed the EQ-5D visual analog scale (EQ-VAS), a 20 cm long VAS where the patients marked their current health status ranging from “best imaginable health state” (score of 100) to “worst imaginable health state” (score of 0).
The primary endpoint was a 0.03 point increase in the EQ-5D index and a 3.0 point increase in the EQ-VAS from baseline to 6 months, based on consensus opinion and published recommendations available.22 Secondary outcomes include changes in EQ-5D index and subscales in the various subgroups of participants as well as the EQ-VAS score.
Data analysis
All analyses were carried out with the PASW Statistics for Windows version 18 (SPSS Inc., Chicago, IL, USA). An intent-to-treat analysis was undertaken, whereby missing data were replaced using the last observation carry forward method. Continuous variables were summarized as means and standard deviations while frequencies and percentages were generated for categorical variables. Statistical comparison of endpoints was done using a paired t-test. We subsequently adjusted for age, occupational status, and education status to estimate the effects of intervention on QoL using a generalized estimating equation (GEE). All analyses were conducted separately for the patients with hypertension, diabetes, and hyperlipidemia. Any P-value less than 0.05 was considered as statistically significant.
Results
Demographic characteristics of participants
A total of 784 participants who were diagnosed with hypertension, diabetes mellitus and/or hyperlipidemia, and treated with pharmacotherapy were enrolled into the study: 527 in the intervention arm and 257 in the usual care arm (Figure 1). However, complete data were available for only 468 participants in the intervention group and 225 participants in the usual care group, giving a response rate of 88.4%. Table 1 shows the demographic characteristics of the participants. Men constituted 59.3% (n=411) of the total respondents and almost half of the participants were of Malay ethnic origin (n=312, 45.0%). Most of the participants had some forms of formal education. Smoking of tobacco was reported by 15.3% (n=106) of the participants. As there were significant differences in the baseline characteristics, comparisons between both arms were not performed.
  | Figure 1 Flowchart of participants in the study. |
Quality of life
QoL for intervention groups
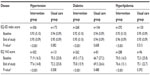
Reported EQ-VAS QoL improved significantly by 6 points in the intervention group from 70.7 to 76.8 (P<0.001) and only by 1.7 points in the usual care group to 72.4 (P=0.314). Mean calculated EQ-5D index score also increased significantly by 0.03 points from 0.92 to 0.95 in the intervention group (P≤0.001). The patients in the usual care group reported an EQ-5D score of 0.94 which increased marginally to 0.95 at the end of the study (Table 2). In addition, the number of participants reporting a minimum meaningful improvement in the QoL was numerically higher in the intervention group compared with the usual care group (24.6% vs 8.0% reporting a 0.03 point improvement in the EQ-5D index score; Table 3). After adjusting for baseline differences, the intervention was associated with an improvement in EQ-VAS score but not EQ-5D scores (Table 4).
QoL for various disease states
The intervention was associated with an improvement in QoL and EQ-VAS score in all the three disease states studied (Table 5). A modest improvement in EQ-VAS score was observed in the usual care group but this did not reach statistical significance. During the study, QoL increased significantly in the intervention group irrespective of disease state, resulting in >80% of the patients reporting no problem for all the five dimensions studied. The biggest improvement was noted in the pain/discomfort dimension where there was a statistical improvement in all the three disease groups studied, followed by anxiety/depression dimension which was significantly improved in the patients with diabetes in the intervention group. No differences were noted in the usual care group at the end of the study (Table 4). The GEE analysis revealed that age and race were strongly associated with better EQ-VAS score and QoL, respectively, in the patients with hyperlipidemia (P<0.05). However, there were no associations between age, education, employment status, and race in the patients with hypertension and diabetes.
Discussion
Metabolic diseases have been shown to negatively impact a person’s QoL.23 In this multi-center study, the involvement of other health care professionals in addition to usual GP care was found to significantly improve the QoL of participants as well as their health status after 6-month participation. These improvements could be attributed to several factors namely: improved patient compliance, modification of diet and lifestyle, psychological support as well as patient empowerment. This combined strategy is simple, culturally acceptable and easily scaled up, and does not require any access to specialist services which may be scarce in a developing country. The data from this study concur and further support those from various other similar studies,17,24 suggesting that these benefits can be realized in clinical practice, which is reflected by an improvement in QoL from a patient’s perspective.
To our knowledge, this is the first community-based controlled trial of its kind in the South East Asian region, where the burden of cardiovascular and chronic kidney diseases is high.25 The study involved a large patient number in a community-based setting, with close follow-up for 6 months. We used the EQ-5D questionnaire, which has been widely used in various studies and validated in the Malaysian population.14,15,20,26 Thirdly, we initiated a study which focused on empowering the patient to manage their own conditions such as providing dietary counseling, training on insulin injection, and self-monitoring of blood glucose to achieve their individual metabolic targets. This is highly novel in Malaysia and was not available at the point of time the study was conducted.
This study has some potential limitations which need to be addressed. Firstly, it included various types of the patients with a wide range of drug regimens. It is possible that the improvement in the patient’s condition or even adherence may have led to this improvement in the QoL. However, as the results of this study reflect actual medical condition, we believe the results will provide useful information and insights into the patient’s concerns and hopes. Secondly, the study was relatively short and hence underpowered to determine its effects on cardiovascular outcomes such as mortality. Nevertheless, the data from other studies suggest that a sustained systolic blood pressure reduction of 5% would reduce the absolute risk of cardiovascular death by 20% over the next 2 decades. Similarly, the UK Prospective Diabetes Study study has shown that a 1% reduction in HbA1c will reduce microvascular and macrovascular complications over the next 10 years.27 Lastly, the allocation of GP clinics to the usual care or intervention group could not be performed at random due to logistic reasons and also the willingness of GP clinics to participate in the study. To encourage participation, a 2:1 ratio of intervention to usual care randomization was adopted. This probably resulted in differences in the baseline characteristics between the two cohorts of participants, which may contribute to the differences in the results.
Conclusion
Implementation of the CCM into GP practice was significantly related to improved QoL of the participants, highlighting the importance of a multi-disciplinary team approach to provide collaborative care to the patients with chronic conditions. An adaptation of the CCM model may serve as a template for future health care system remodeling, to help improve access to quality and effective health care services especially in primary care.
Acknowledgments
We are grateful to the Director General of Health, Malaysia, for permission to publish this article, and to the Clinical Research Centre (CRC), Ministry of Health, Malaysia for supporting this study. Our greatest appreciation goes to the CORFIS team, especially to Dr Lim Teck Onn and Dr Zaki Morad Mohd Zaher, the principal investigators, and to Mr Wilson Low Hong Hoo, Mr Tang Guang Hui, Ms Dan Siew Peng, Ms Kimberly Wong, Ms Nor Fasihah Yahaya, and Ms M Vatsala Nair Manoha for coordinating the CORFIS trial. We also express our utmost gratitude to all the service pharmacists, dietitians, nurses, and GPs for their support, as well as to all the participants in this study for their cooperation.
Author contributions
FMYA conceived, directed, and designed the CORFIS study. SWHL conducted statistical analyses. SSC designed the CORFIS study and assisted in statistical analyses. BE and TP participated in the study design. LCK coordinated the CORFIS study. All authors contributed toward data analysis, drafting and critically revising the paper, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. | |
Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42(6):1206–1252. | |
Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final report. Circulation. 2002;106(25):3143. | |
Members ATF, Mancia G, Fagard R, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;31(7):1281–1357. | |
Amal NM, Paramesarvathy R, Tee GH, Gurpreet K, Karuthan C. Prevalence of chronic illness and health seeking behaviour in Malaysian population: results from the Third National Health Morbidity Survey (NHMS III) 2006. Med J Malaysia. 2011;66(1):36–41. | |
[No authors listed]. NCD Pervention and Control Annual Report 2011. In: Section N-CD. Putrajaya: Ministry of Health Malaysia; 2011:735. | |
Davy C, Bleasel J, Liu H, Tchan M, Ponniah S, Brown A. Effectiveness of chronic care models: opportunities for improving healthcare practice and health outcomes: a systematic review. BMC Health Serv Res. 2015;15(1):194. | |
Stellefson M, Dipnarine K, Stopka C. The chronic care model and diabetes management in US primary care settings: a systematic review. Prevent Chron Dis. 2013;10:E26. | |
Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, part 2. JAMA. 2002;288(15):1909–1914. | |
Bodenheimer T. Interventions to improve chronic illness care: evaluating their effectiveness. Dis Manag. 2003;6(2):63–71. | |
Low W, Seet W, Ramli AS, et al. Community-based cardiovascular Risk Factors Intervention Strategies (CORFIS) in managing hypertension: A pragmatic non-randomised control. Med J Malaysia. 2013;68(2):129–135. | |
Chua S, Kok L, Yusof FA, et al. Pharmaceutical care issues identified by pharmacists in patients with diabetes, hypertension or hyperlipidaemia in primary care settings. BMC Health Serv Res. 2012;12(1):388. | |
[No authors or editors listed]. Demographic Indicators Malaysia. In: Malaysia DoS. Putrajaya: Department of Statistics, Malaysia; 2012. | |
Shafie A, Hassali M, Liau S. A cross-sectional validation study of EQ-5D among the Malaysian adult population. Q Life Res. 2011; 20(4):593–600. | |
Varatharajan S, Chen W-S. Reliability and validity of EQ-5D in Malaysian population. Appl Res Q Life. 2012;7(2):209–221. | |
Morgan CL, McEwan P, Morrissey M, Peters JR, Poole C, Currie CJ. Characterization and comparison of health-related utility in people with diabetes with various single and multiple vascular complications. Diabetic Medicine. 2006;23(10):1100–1105. | |
Currie C, Poole C, Woehl A, et al. The health-related utility and health-related quality of life of hospital-treated subjects with type 1 or type 2 diabetes with particular reference to differing severity of peripheral neuropathy. Diabetologia. 2006;49(10):2272–2280. | |
Sullivan PW, Ghushchyan V, Wyatt HR, Wu EQ, Hill JO. Impact of cardiometabolic risk factor clusters on health-related quality of life in the US [ast]. Obesity. 2007;15(2):511–511. | |
Bharmal M, Thomas J. Comparing the EQ-5D and the SF-6D descriptive systems to assess their ceiling effects in the US general population. Value Health. 2006;9(4):262–271. | |
Ko Y, Coons SJ. Self-reported chronic conditions and EQ-5D index scores in the US adult population. Curr Med Res Opin. 2006; 22(10):2065–2071. | |
Md Yusof FA, Goh A, Azmi S. Estimating an EQ-5D value set for Malaysia using time trade-off and visual analogue scale methods. Value Health. 2012;15(1):S85–S90. | |
Luo N, Johnson JA, Coons SJ. Using instrument-defined health state transitions to estimate minimally important differences for four preference-based health-related quality of life instruments. Med Care. 2010;48(4):365–371. | |
Ford ES, Li C. Metabolic syndrome and health-related quality of life among US Adults. Ann Epidemiol. 2008;18(3):165–171. | |
Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Affairs. 2001;20(6):64–78. | |
Dhillon PK, Jeemon P, Arora NK, et al. Status of epidemiology in the WHO South-East Asia region: burden of disease, determinants of health and epidemiological research, workforce and training capacity. Int J Epidemiol. 2012;41(3):847–860. | |
Shah S, Zilov A, Malek R, Soewondo P, Bech O, Litwak L. Improvements in quality of life associated with insulin analogue therapies in people with type 2 diabetes: Results from the A1chieve observational study. Diabet Res Clin Pract. 2011;94(3):364–370. | |
Chalmers J, Cooper ME. UKPDS and the legacy effect. New Eng J Med. 2008;359(15):1618–1620. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.