Back to Journals » Patient Preference and Adherence » Volume 12
Choosing the appropriate treatment setting: which information and decision-making needs do adult inpatients with mental disorders have? A qualitative interview study
Authors Kivelitz L , Härter M , Mohr J, Melchior H, Goetzmann L, Warnke MH, Kleinschmidt S, Dirmaier J
Received 30 January 2018
Accepted for publication 24 February 2018
Published 15 May 2018 Volume 2018:12 Pages 823—833
DOI https://doi.org/10.2147/PPA.S164160
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Naifeng Liu
Laura Kivelitz,1 Martin Härter,1 Jil Mohr,1 Hanne Melchior,1 Lutz Goetzmann,2 Max Holger Warnke,3 Silke Kleinschmidt,4 Jörg Dirmaier1
1Department of Medical Psychology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany; 2Department of Psychosomatic Medicine and Psychotherapy, Segeberg Hospital, Bad Segeberg, Germany; 3Specialist Clinic for Psychosomatic Medicine and Psychotherapy, MediClin Seepark Klinik, Bad Bodenteich, Germany; 4Specialist Clinic for Psychosomatic Medicine and Psychotherapy, Curtius Klinik, Bad Malente-Gremsmühlen, Germany
Background: Decisions on medical treatment setting are perceived as important but often difficult to make for patients with mental disorders. Shared decision-making as a strategy to decrease decisional conflict has been recommended, but is not yet widely implemented. This study aimed to investigate the information needs and the decision-making preferences of patients with mental disorders prior to the decision for a certain treatment setting. The results will serve as a prerequisite for the development of a high-quality patient decision aid (PtDA) regarding the treatment setting decision.
Methods: We conducted retrospective individual semi-structured interviews with n=24 patients with mental disorders in three psychotherapeutic inpatient care units. The interviews were audiotaped, transcribed, coded, and content-analyzed.
Results: The majority of the patients wanted to be involved in the decision-making process. They reported high information needs regarding treatment options in order to feel empowered to participate adequately in the decision for a certain treatment setting. However, some patients did not want to participate or receive information, for example, because of their high burden of mental disorder. Whereas the majority were satisfied with the extent they were involved in the decision, few participants felt sufficiently informed about treatment options. Most patients reported that a decision aid regarding an appropriate treatment setting would have been helpful for them. Important information that should be included in a PtDA was general information about mental illness, effective treatment options, specific information about the different treatment settings, and access to treatment.
Discussion: The identified information and decision-making needs provide a valuable basis for the development of a PtDA aiming to support patients and caregivers regarding the decision for an adequate treatment setting. As preferences for participation vary among patients and also depend on the current mental state, a flexible approach is needed to meet patients’ individual wishes and needs.
Keywords: mental disorders, needs assessment, psychotherapy, treatment decision, treatment setting, shared decision-making, qualitative interviews
Introduction
Despite the high global prevalence of mental disorders only a small percentage of these patients receive adequate treatment.1–3 Treatment barriers often result from a lack of integration of the different steps involved in care, for example, due to communication and coordination problems between different services and providers.4–7 The problem of treatment access can emerge both at the systemic level (eg, long waiting lists for outpatient psychotherapy) and at the individual level (eg, insufficient patient awareness of symptoms and available treatment options because of a lack of information),4,8 which indicates a need to address treatment barriers. Patient information and involvement are relevant components of patient-centered mental health care, a concept that has gained in importance in recent years.9,10 It also incorporates shared decision-making (SDM), advocated as an important approach in the mental health policy of many countries internationally.11 It is defined as: “a process in which clinicians and patients work together to select tests, treatments, management or support packages, based on clinical evidence and the patient’s informed preferences”.12 Furthermore, SDM comprises the provision of evidence-based information about options, outcomes and uncertainties, along with decision support counseling and a system for recording and implementing patients’ informed preferences.11,12
Evidence suggests that SDM leads to improved outcomes in mental health care, including help-seeking behavior,13 enhanced patient satisfaction and compliance with decisions,14–17 as well as reduced stigma and increased involvement.18 Furthermore, the majority of patients with mental disorders prefer to be involved in treatment decision-making.19–25 Although there is international consensus about the importance of SDM,11 it is not yet widely implemented.11,26–28
As implementation is the current challenge facing SDM practice across all settings and countries,26 research in routine mental health care and development of interventions to support SDM is needed.11,22
Besides the training of health care providers and coaching of patients, methods to support SDM include the use of high-quality patient decision aids (PtDAs). According to the International Patient Decision Aids Standards Collaboration (http://ipdas.ohri.ca), which has provided criteria to judge the quality of PtDAs,29,30 these tools are designed to help people participate in decision-making about health care options. They provide information on the options and help patients clarify the personal value they associate with different option features, which also leads to reduced decisional conflict and a higher proportion of patients with realistic expectations regarding benefits and harms.31 However, the implementation of PtDAs into routine mental health care remains limited.24,32 In the systematic development of high-quality decision aids, assessment of information and decision-making needs is seen as one key element.30,33 Previous research on general information and decision-making needs among people with mental disorders indicates that treatment-related decisions, especially concerning the treatment setting, are perceived particularly important and difficult to make and highlights patients’ requirement to be informed and involved in the decision-making process.24,28,34 In general, there are various effective psychotherapeutic and/or psychopharmacologic treatment options for patients with mental disorders in the health care system. These treatment options can be implemented both in inpatient and outpatient treatment settings.
Objectives
The aim of our study was to identify specific information and decision-making needs of patients with mental disorders prior to the decision for a certain treatment setting (inpatient or outpatient). The following topics were addressed: 1) Decision-making process (involved parties, patients’ preferred and perceived role), 2) Information process (patient satisfaction with received information), 3) Decision aid (information needs, identification of helpful information that should be included). The results will serve as a prerequisite for the development of a PtDA regarding the treatment setting decision.
Ethical approval
The study has been approved by the responsible local Ethics Committee of the Chamber of Physicians in Hamburg (Ref Nr PV5232) and has been conducted according to the principles of the Declaration of Helsinki (2013 version).
Methods
Study design and participant recruitment
In this qualitative multicenter cross-sectional survey, we conducted 24 individual semi-structured interviews in three psychotherapeutic inpatient routine care units in Germany in December 2016. Patients were recruited consecutively by their psychotherapists during their inpatient treatment, which consisted of at least one session of individual psychotherapy and two sessions of group psychotherapy per week. Additionally, patients received psychoeducation, exercise, relaxation training, and psychopharmacotherapy if required. The duration of inpatient treatment ranged from 3 to 6 weeks. Patients were informed and invited to participate during individual and group psychotherapy sessions.
The inclusion criteria were a diagnosed mental disorder according to 10th revision of the International Statistical Classification of Diseases and Related Health Problems and being 18 years of age or older. Primary diagnosis criteria were assessed by treatment providers at admission. Exclusion criteria were an acute risk of suicide, acute psychosis or psychotic symptoms, and insufficient German language skills. Written informed consent was received from all eligible patients, and all agreed to be audiotaped for transcription. The sample size was determined based on the principle of theoretical saturation, according to which the sample is complete when no additional new information is obtained by further interviews.35
Data collection
We collected data through individual semi-structured interviews, as this approach allows a large gain in individual information through an in-depth understanding of a person’s opinion and experiences.36 We developed a semi-structured interview guide based on our research questions and previous research findings.24,28,34 The one-on-one interviews were conducted by LK or JM within the inpatient units. LK and JM had experience in conducting qualitative interviews. LK is a clinical psychologist employed as a research associate and has carried out several qualitative studies. JM is a psychologist at an advanced stage in Master’s degree employed as a research assistant. We started every interview with standardized questions regarding the patients’ demographic and clinical background. Then we asked the patients about their experiences during the decision-making process prior to the current inpatient treatment, focusing on patients’ information and participation needs prior to the decision for a certain treatment setting. Table 1 illustrates the interview guide questions based on the overarching research topics.
  | Table 1 Interview guide questions based on the overarching topics |
The participants were encouraged to describe their experiences regarding the questions in the interview guide. As semi-structured interviews allow flexibility, the respondents’ answers also led to a change in the order of the questions or to follow-up questions from the interviewer. The mean duration of the interviews was 31.1 minutes (SD=7.1). Patients were compensated €30.00 for their time. The 24 interviews were taped and transcribed verbatim.
Data analysis
The text data were analyzed by two researchers (LK and JM) according to the qualitative content analysis approach.37 We combined the theory-based method of “structuring” (deductive category assignment) with the inductive category development approach. The first step in the analysis was the creation of an index category system based on theoretical assumptions from previous studies4,24,34 and on the interview guide (deductive approach). The initial category system comprised the following four main categories (with related questions, which should be answered through the interview data): 1) Decision-making process (Who recommended inpatient treatment? Who was involved in the decision?); 2) Participation needs (Preferred role: passive, shared, or autonomous role? Perceived role? Satisfied yes/no); 3) Information needs: (Received information regarding treatment options yes/no? Satisfied yes/no?); 4) Decision aid (Helpful yes/no? Information that should be included?). In the second step, interview transcripts were carefully read and discussed to obtain an overall sense of the data.
In the third step, the transcripts were initially coded separately by both researchers. During the coding process, in which the interview sequences were assigned to categories, the index category system was complemented and modified based on the data (inductive approach). The final category system consisted of the initial main categories, supplemented by subcategories, for example, 1. Decision-making process, 1.1 involved persons/parties, 1.1.1 psychotherapist, 1.1.2 general practitioner, 1.1.3 medical specialist, 1.1.4 social insurance carrier, and 1.1.5 family members. To develop a consensual category system, the identified categories and subcategories were discussed several times in the research group (LK, JM, JD) as the data were coded three times. Mismatching categorizations were discussed until consensus was reached. The qualitative analysis was performed with MAXQDA 10.38 The focus was on the qualitative analyses; quantitative details reported in the results section have a supplementary descriptive purpose.
Results
Demographic and clinical characteristics
Participant characteristics are shown in Table 2.
  | Table 2 Demographic and clinical characteristics |
Of the 24 participants, 11 (45.8%) were women. The mean age was 48 years (SD 12.0). The majority of the participants was employed full- or part-time (70.8%). Sixteen participants (66.7%) were diagnosed with an affective disorder. The mean duration of illness was 8 years (SD 8.9) and 54.2% of the participants had one or more comorbid mental disorder diagnoses in addition to the first diagnosis. Four participants (16.7%) stated that the current treatment is their first psychotherapeutic treatment. Twenty (83.3%) reported that they already received psychotherapeutic/psychopharmacologic treatment in the past. Of these participants, 66.7% (n=16) said that they have had an outpatient psychotherapeutic treatment before, 41.7% (n=10) stated that they have been in an inpatient treatment, and 25% (n=6) reported that they already received both, outpatient and inpatient treatment, before.
Decision-making process
Making the decision for inpatient treatment setting – involved persons and parties
With regard to the question who was involved in the decision-making process, some participants (n=9) reported that the general practitioner recommended or had the idea of the inpatient treatment.
I hadn’t thought about an inpatient treatment. Not at all, it was my general practitioner’s idea. [P15]
According to some participants (n=11) the advice for an inpatient treatment came from an outpatient psychotherapist.
My private life was a mess. I told my therapist that I don’t feel any change or improvement. Then she came up with the idea of an inpatient treatment, saying it might be helpful to get some distance to the daily routine and struggles and proposed I applied for one. So that’s what I did. [P24]
Some patients (n=6) named a medical specialist (eg, neurologist or psychiatrist) as another party recommending an inpatient treatment.
My neurologist told me to go on sick leave due to this severe depression that has developed over time. That’s when the neurologist said that I should think about doing an inpatient treatment. [P8]
Seven participants stated that their social insurance carrier (n=4 statutory health insurance; n=3 pension fund) recommended an inpatient treatment.
I was receiving sickness benefit. Not for long yet–maybe six weeks, not more than eight. At that point, my health insurance called and instructed me to apply for an inpatient treatment. […] They just wanted to get me out of their costs. [P17]
According to one participant, family members also affected the decision-making process prior to the inpatient treatment.
And then my husband said, “Enough is enough!” I was completely exhausted and he said “It can’t go on like that.” My sister was also putting pressure on me to go inpatient. [P1]
Even the children said “Mommy, you’re starving yourself to death.” They also realized that I wasn’t able to do the household anymore.
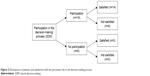
The participants differed regarding the number of named parties involved in the decision-making process prior to the current treatment. Most participants (n=16) named only one party who was involved, while some (n=6) named two parties and a few (n=2) stated that there were three parties involved. The different involved parties named by the participants are shown in Figure 1.
  | Figure 1 Persons/parties involved in the decision-making process regarding the treatment setting named by the participants. |
Patients’ preferred role in the decision-making process
Most participants (n=18) expressed that they generally want to take part in medical decisions and prefer SDM between clinician and patient (collaborative role), which was also expressed regarding the decision for the current inpatient treatment.
I mean, regarding the real medical decisions, I cannot make a decision on my own. But I always think it’s good to be informed as much as possible about the existing options and get involved into the decision-making process. I think fifty-fifty is pretty good. [P17]
Some (n=5) stated that they generally do not want to participate in medical decisions and also did not want to be involved in the present treatment decision, preferring the clinician making decisions alone (passive role).
Definitely the doctor should decide by himself, because one’s own ability to think and to decide is extremely limited by attitudes and personality. Of course every case is individual and it depends on one’s disease. Take me, for instance – due to my anxiety disorder, I was scared a lot. In that case I think it helps when the doctor says “Do this, do that.” [P12]
One participant stated that the patient should generally make medical decisions on his own (autonomous role) but still needs information from the clinician, which he also meant regarding the decision for the current inpatient treatment.
My attitude is that first, I have to see for myself. Of course, if you realize that you are not alright, you have to talk to a doctor about it and you need information. But the decision remains mine to make. [P8]
Patients’ perceived role and satisfaction with involvement
Regarding the participation in the decision-making process prior to the current inpatient treatment, the majority of the participants (n=18) reported that they were involved in the decision. Most of them (n=14) said that they were satisfied with their collaborative role and the extent they were involved (Figure 2).
  | Figure 2 Participation of patients and satisfaction with the perceived role in the decision-making process. |
The decision for doing an inpatient treatment has been discussed together with me, just like the application process. I also discussed this with my family, my wife and then I started the process. I was totally fine with that. [P16]
Some of these participating patients (n=4) stated that they were not satisfied, because they would have needed more information to be able to participate adequately and would have wanted the clinician to be more active and supportive in the decision-making process.
I would have preferred the doctor to be more active instead of just pointing out a single option of inpatient treatment and then leaving me alone with the decision whether to do it or not. [P16]
On the other hand, some participants (n=6) reported that they did not participate in the decision-making process. Some of these participants (n=3) stated that they were satisfied with their passive role of not being involved in the decision because of their high burden of mental disorder.
If your disease is mental, you don’t really care. You just want somebody to help you. I think, I would’ve done everything the doctor had told me. Like, run around the Christmas tree with the drum–I would have done it. [P13]
Due to my helplessness I didn’t know, whether what he said was reasonable or not or whether that’s what I needed. I couldn’t decide on that. [P10]
But I guess the situation is quite irregular if your psyche is so frail, you’ve completely lost your inner sense of competence. I don’t think I could have handled somebody just telling me the options and letting me decide–I might just have been unable to decide. [P10]
Some of these participants (n=3) not involved in the decision reported that they were not satisfied, as they would have wanted to participate more in the decision-making process. These patients said that they felt like they did not have a choice regarding the treatment decision as a noncommitment to the inpatient treatment would have had negative consequences for them, for example, losing insurance coverage.
The decision was already made, since the health insurance refused to cover the costs for sick leave. That was not a shared decision. I don’t endorse them being like “Either you do it or you lose your payment.” Entire existences depend on this decision. [P4]
Matching between preferred and perceived role in decision-making process
Overall, it can be stated that in the majority of cases (n=19), the patients’ preferred role was congruent with the perceived role. Some patients (n=5) reported a mismatch. Some of these patients (n=3) preferred more participation in the decision-making process than perceived, of which one patient was not satisfied and two patients were nevertheless satisfied with the extent they were involved. Others (n=2) preferred less involvement than perceived, but despite the mismatch both patients were satisfied with the extent they were involved.
Information process
Patients’ satisfaction with information regarding treatment options
Some participants (n=8) reported that they were informed about the treatment options and the respective pros and cons of the different treatment settings by a clinician, some (n=3) stated that they were informed by their general practitioner, others (n=3) by a medical specialist, and some (n=2) were informed together by their general practitioner and psychologist. Of these informed patients, some (n=6) stated that they were satisfied with the information they received, whereas others (n=2) did not feel sufficiently informed or, in retrospect, seemed to be ambivalent (Figure 3).
  | Figure 3 Satisfaction with information regarding treatment options. |
I was satisfied with the information received from my doctor. On the one hand he explained why the inpatient treatment would be the best option in his opinion, but he also pointed out that I could alternatively choose a day hospital, possibly even close to my home […]. Taking into account outpatient therapy didn’t work out and that my previous experiences with inpatient treatment were positive, my decision was clear. [P2]
Well, I talked to my therapist about the options I have, but I felt as though she wasn’t too informed or didn’t even know all the options there are, from what I heard about it. [P1]
The majority of the participants (n=16) reported that they received no or very little information regarding treatment options. Many of these participants (n=10) stated that they were not satisfied as they did not feel sufficiently informed.
I felt a strong lack of information. I had to look everything up by myself. I think you need information. Or maybe there are some that don’t want the options, that are glad being told what to do and where to go, but not me. I want to know all about it. I was wishing for more support and detail regarding that matter. [P17]
Some of them (n=6), on the other hand, stated that they nevertheless were satisfied and did not require more information, either because they already had information and experiences from previous treatments (n=5) or because of lacking ability to process information because of the high burden of mental disorder at that time (n=1).
I: Would you, retrospectively, wish to have received more information?
No, I was at a point where I was simply happy to have a treatment at all and was able to calm down, finally. From my point of view, that was okay. [P21]
Decision aid
Patients’ perceived usefulness of a decision aid
In response to the question if they might have benefited from having more information about different treatment options, for example, in the form of a decision aid, most of the patients (n=19) stated that a decision aid might have been helpful for them prior to the decision for the present inpatient treatment.
A decision aid would definitely have been helpful. I’m imagining a brochure or something, where the different treatment options are shown and explained. I think that would have contributed to not feeling as overwhelmed and helpless. Having a list of options is always good when it comes to making decisions. [P10]
Some participants (n=5) reported that a decision aid would not have been helpful for them. Two participants explained that they had no need for information, because of previous treatment experience, but stated that it might be helpful for others with no experience.
Not for myself, no, but I reckon there are patients it would be helpful for. Just to explain how it’d look like, what the daily routine would be like or what the differences between outpatient psychotherapy, day clinics or inpatient treatment are. I would like that. [P2]
One participant said that information in the form of a decision aid would have been an additional burden for him.
Maybe if you touch the general aspects, but in my opinion too much information can be a burden. Since we’re here because of mental reasons, your head is filled with all of that and getting even more on top. I mean it’s not your leg that’s broken, dealing with your head is burden enough and it just makes everything harder. [P14]
Another participant explained that he did not need any information, as he generally trusts his clinician completely and had no interest in participating in the decision-making process. One participant described that a decision aid providing “theoretical” information would have been “useless” for him and that only “something practical,” for example, a “taster week,” would have been helpful regarding the treatment decision.
Information that should be included in the decision aid
Of those participants indicating that a decision aid might have been helpful, many (n=14) stated that a general description of the different outpatient and inpatient treatment options, which are known to be effective (psychotherapy and pharmacotherapy), should be included in the decision aid. Many participants (n=14) said that specific information regarding the different treatment settings, like duration and intensity (n=7) or type of therapy, content, and aim (n=9), would be important for them. Some participants (n=10) described a need for information that helps to decide individually, which treatment setting is adequate for a certain disorder with a certain degree of severity. Some patients (n=8) said that it would be helpful for the individual decision to have a list of advantages and disadvantages regarding the treatment setting related to specific patient characteristics (eg, type of disorder, severity, living conditions). Some participants (n=3) suggested to include experience reports of former patients in the decision aid as they might have benefited from that. In Table 3, we summarized the participants’ information needs in the form of questions that should be answered in a decision aid that intends to help patients to decide between different treatment settings.
  | Table 3 Information that should be included in a decision aid from patients’ perspective |
To be able to distinguish between all these different forms of outpatient psychotherapy would be great. I mean there is behavior therapy, conversational therapy, psychodynamic psychotherapy, gestalt therapy. There are so many different ways to do it. What is it exactly, is it depth psychotherapy, where they are going to poke around in your childhood, or is it behavior therapy, where you get suggestions and measures, so what happens there? [P7]
It’d be important to know what the different methods are aiming at and what situation the patient needs to be coming from. To be able to say “so I’m about this sick as stated here so that’d mean this kind of therapy would be the best” […] For them to point out the best therapy for a certain set of symptoms. [P10]
I was hoping to receive more information about the differences between inpatient and outpatient treatment. The same goes for day clinic. I found it difficult to figure out the differences in goals and organization. [P19]
Discussion
This study aimed to identify specific information and decision-making needs of patients with mental disorders prior to the decision for a certain treatment setting as a prerequisite for the development of a high-quality PtDA.
We conducted individual semi-structured interviews with n=24 patients with mental disorders in three psychotherapeutic inpatient routine care units. Our qualitative approach resulted in a detailed insight of the patients’ preferred and perceived role in the decision-making process prior to their current treatment, the satisfaction with the received information, and their information needs, especially with regard to information that should be included in a PtDA. Whereas previous research on patients’ information needs and decision-making preferences referred more to treatment options in general, the present study focused on the decision for a certain treatment setting, providing new insights into the current state of decision-making in the care of mentally ill patients.
In line with existing research,19–25 the majority of the participants interviewed in our study generally prefer a collaborative role regarding medical decisions. Patients wanted to be involved in the decision-making process prior to their current inpatient treatment and reported high information needs regarding treatment options in order to feel empowered to participate adequately in the decision for a certain treatment setting.
However, it is worth noting that some patients did not want to be actively involved in the decision, which is also known from previous studies indicating that patients’ preferences for participation vary and patients’ preferred and the perceived role in medical decision-making often do not match.19,39 In our study, some patients stated that they preferred a passive role in the decision-making process prior to the current inpatient treatment and did not want to receive information, because of lacking the ability to process information because of their high burden of mental disorder at this time point. Similar results were found in a qualitative focus group study, in which the participants reported that in crisis situations and phases of high disease severity they preferred leaving decisions to their caregiver as they had difficulties to understand the information they received, which made them feel ashamed and behave passive.40 Patients preferring a passive role might be affected by a more severe mental illness and, therefore, probably need even more support regarding the treatment decision. Previous research showed that SDM also leads to improved outcomes in severe mentally ill patients indicating that high symptom severity is not a barrier to SDM.18,21 As SDM does not aim at forcing patients to be active decision-makers but rather offers them a choice, this might lead to increased involvement and reduced stigma.18
Although the decision for the current inpatient treatment seemed to be comprehensible for all participants and the majority reported to be satisfied with the extent they were involved, only a few participants in our study felt informed about treatment options. One explanation for this surprising finding could be social desirability. Here, it might be less accepted to admit that one has not participated to the desired degree, for example, because of staying passive and just doing what the clinician said without knowing why, as this might feel more like one’s “own fault,” than to state that the caregiver just failed to give enough information. The extent of satisfaction probably also depends on patients’ expectations and the congruence between the preferred and the perceived role in decision-making process. The fact that in our study only a few patients (n=5) reported a mismatch between preferred and perceived role might also be a reason for the high satisfaction. It can also be assumed that patients were satisfied with the decision-making process even though they were not sufficiently informed, because they just did not know that there might have been other treatment options besides inpatient treatment. Another explanation might be that 83% of the patients in our sample already received psychotherapeutic treatment in the past and, therefore, might have already been informed regarding different options from previous treatment experiences.
The fact that the participants were interviewed retrospectively when they already started inpatient treatment could also be a reason for this contradiction as it might have led to distortions. We know from previous research39 that the outcomes of studies, measuring decision-making preferences prospectively or retrospectively, differ. It is possible that patients who are satisfied with their current treatment also perceive the preceding decision-making process as satisfying retrospectively, while they might have been less satisfied if we would have asked them right after the decision and before the current treatment started.
Limitations
Even though the qualitative approach enabled us to gather valuable in-depth information, the reduced generalizability needs to be mentioned as a limitation. To increase the external validity and support valid transferability to real-life health care, patients were recruited consecutively from three different care units after being screened for the inclusion criteria. However, we did not comprehensively include patients with diagnoses from the whole spectrum of mental disorders, for example, delusional disorders or schizophrenia. Furthermore, the implementation and analysis of semi-structured qualitative interviews involves multiple subjective decisions. Objectivity might be limited, although the interviews were conducted and coded by two different raters and the category system was discussed several times in the research group in order to minimize subjectivity. Due to the retrospective design of this survey a memory bias also cannot be ruled out. Our sample might also be prone to selection bias as we cannot provide data regarding nonresponders.
Implications
In this study, we interviewed patients currently in inpatient treatment regarding the preceding information and decision-making process. Further research is needed to provide data also for other outpatient or partly inpatient day care treatment settings (eg, also differentiating between acute and rehabilitation treatment). As the German health care system differs from the systems of other countries, especially regarding treatment settings, transferability of our results to other countries and institutions also needs to be verified in further international studies. Future research should also consult relatives of patients as relatives are often involved in the decision-making process as well. Furthermore, interview guides of future studies may also consider system-related, social and cultural influences as these might affect patients’ preferences as well.
As preferences for participation vary among patients and also depend on the current intrapersonal mental state, a flexible approach is needed to meet patients’ individual wishes and needs in the course of their illness. Health care professionals should be sensitive because especially patients with high symptom severity often remain passive, but probably need even more support, for example, by being involved and receiving information in a patient and easy-to-understand manner.
The identified patients’ information and decisional priorities in our study also serve as a prerequisite for a PtDA we are currently developing. The PtDA aims to help patients and caregivers regarding the decision for an adequate treatment setting. Besides concrete contents that should be included, a possible structure and way to present the desired information could also be derived from the data. The patients wished to receive answers to specific questions regarding the different settings, but also wanted to be informed about mental illnesses in general. Here, one possibility could be to present general information in a continuous text and the desired specific information in the form of “frequently asked questions (FAQs)”, for example, in a tabular comparison of the different settings. After developing the PtDA, a survey with experts from the field of treatment and research will be conducted for further evaluation. Subsequently the PtDA will be discussed and evaluated in patient focus groups regarding comprehensibility and clarity, acceptance, and practical utility.
Acknowledgments
We would like to thank the employees from the inpatient care units involved in the study for their cooperation, as well as all the participants who took the time to be part of the study. This project was funded by the German Federal Pension Fund (RSS-2.10.2//Project number: 202).
Disclosure
The authors report no conflicts of interest in this work.
References
Wittchen HU, Jacobi F, Rehm J, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21(9):655–679. | ||
Jacobi F, Höfler M, Strehle J, et al. Mental disorders in the general population: study on the health of adults in Germany and the additional module mental health (DEGS1-MH). Nervenarzt. 2014;85:77–87. | ||
Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62(6):629–640. | ||
Kivelitz L, Watzke B, Schulz H, Härter M, Melchior H. Health care barriers on the pathways of patients with anxiety and depressive disorders–a qualitative interview study. Psychiat Prax. 2015;42(8):424–429. | ||
Klesse C, Bermejo I, Härter M. Innovative care models for treating depression. Nervenarzt. 2007;78:585–596. | ||
Collins KA, Westra HA, Dozois DJA, Burns DD. Gaps in accessing treatment for anxiety and depression: challenges for the delivery of care. Clin Psychol Rev. 2004;24:583–616. | ||
Schulz H, Barghaan D, Koch U, Harfst T. Die Versorgung von Patienten mit Psychischen Störungen [Health care for patients with mental disorders.] In: Clinical Psychology and Psychotherapy. Berlin: Springer; 2011:361–380. | ||
Federal Chamber of Psychotherapists (BPtK). BPtK-Study on waiting times in outpatient psychotherapeutic care. Survey of the State Chamber of Psychotherapists and the BPtK [BPtK-Studie zu Wartezeiten in der ambulanten psychotherapeutischen Versorgung. Umfrage der Landespsychotherapeutenkammern und der BPtK]. Available from: http://www.bptk.de/uploads/media/110622_BPtK-Studie_Langfassung_Wartezeiten-in-der-Psychotherapie_01.pdf. 2011. http://www.bptk.de/fileadmin/user_upload/Publikationen/BPtK-Studien/belastung_moderne_arbeitswelt/Wartezeiten_in_der_Psychotherapie/20110622_BPtK-Studie_Langfassung_Wartezeiten-in-der-Psychotherapie.pdf. Accessed 15 July, 2013. | ||
Scholl I, Zill JM, Härter M, Dirmaier J. An integrative model of patient-centeredness–a systematic review and concept analysis. PLoS One. 2014;9(9):e107828. | ||
Storm M, Edwards A. Models of user involvement in the mental health context: intentions and implementation challenges. Psychiatr Q. 2013;84(3):313–327. | ||
Slade M. Implementing shared decision making in routine mental health care. World Psychiatry. 2017;16(2):146–153. | ||
Coulter A, Collins A. Making Shared Decision-Making a Reality: No Decision About Me, Without Me. London: The Kings Fund; 2011. | ||
Wakefield P, Read S, Firth W, Lindesay J. Clients’ perceptions of outcome following contact with a community mental health team. J Ment Health. 1998;7(4):375–384. | ||
Hamann J, Leucht S, Kissling W. Shared decision making in psychiatry. Acta Psychiatr Scand. 2003;107(6):403–409. | ||
Joosten EAG, DeFuentes-Merillas L, de Weert GH, Sensky T, van der Staak CPF, de Jong CAJ. Systematic review of the effects of shared decision-making on patient satisfaction, treatment adherence and health status. Psychother Psychosom. 2008;77(4):219–226. | ||
Duncan E, Best C, Hagen S. Shared decision making interventions for people with mental health conditions. Cochrane Database Syst Rev. 2010;(1):CD007297. | ||
Loh A, Simon D, Wills CE, Kriston L, Niebling W, Härter M. The effects of a shared decision-making intervention in primary care of depression: a cluster-randomized controlled trial. Patient Educ Couns. 2007;67(3):324–332. | ||
Hamann J, Langer B, Winkler V, et al. Shared decision making for in-patients with schizophrenia. Acta Psychiatr Scand. 2006;114(4):265–273. | ||
Chewning B, Bylund CL, Shah B, Arora NK, Gueguen JA, Makoul G. Patient preferences for shared decisions: a systematic review. Patient Educ Couns. 2012;86(1):9–18. | ||
Schattner A, Bronstein A, Jellin N. Information and shared decision-making are top patients’ priorities. BMC Health Serv Res. 2006;6(1):21. | ||
Adams JR, Drake RE, Wolford GL. Shared decision-making preferences of people with severe mental illness. Psychiatr Serv. 2007;58(9):1219–1221. | ||
Puschner B, Becker T, Mayer B, et al. Clinical decision making and outcome in the routine care of people with severe mental illness across Europe (CEDAR). Epidemiol Psychiatr Sci. 2016;25(1):69–79. | ||
Friedrichs A, Spies M, Härter M, Buchholz A. Patient preferences and shared decision making in the treatment of substance use disorders: a systematic review of the literature. PLoS One. 2016;11(1):e0145817. | ||
Tlach L, Wüsten C, Daubmann A, Liebherz S, Härter M, Dirmaier J. Information and decision-making needs among people with mental disorders: a systematic review of the literature. Health Expect. 2015;18(6):1856–1872. | ||
Michaelis S, Kriston L, Härter M, Watzke B, Schulz H, Melchior H. Predicting the preferences for involvement in medical decision making among patients with mental disorders. PLoS One. 2017;12(8):e0182203. | ||
Scholl I, Barr PJ. Incorporating shared decision making in mental health care requires translating knowledge from implementation science. World Psychiatry. 2017;16(2):160–161. | ||
McCabe R, Khanom H, Bailey P, Priebe S. Shared decision-making in ongoing outpatient psychiatric treatment. Patient Educ Couns. 2013;91(3):326–328. | ||
Freidl M, Pesola F, Konrad J, et al. Effects of clinical decision topic on patients’ involvement in and satisfaction with decisions and their subsequent implementation. Psychiatr Serv. 2016;67(6):658–663. | ||
Elwyn G, O’Connor AM, Bennett C, et al. Assessing the quality of decision support technologies using the international patient decision aid standards instrument (IPDASi). PLoS One. 2009;4(3):e4705. | ||
Elwyn G, O’Connor A, Stacey D, et al. Developing a quality criteria framework for patient decision aids: online international Delphi consensus process. BMJ. 2006;333(7565):417. | ||
Stacey D, Légaré F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;(4). | ||
Elwyn G, Scholl I, Tietbohl C, et al. “Many miles to go …”: a systematic review of the implementation of patient decision support interventions into routine clinical practice. BMC Med Inform Decis Mak. 2013;13(2):S14. | ||
Coulter A, Stilwell D, Kryworuchko J, Mullen PD, Ng CJ, van der Weijden T. A systematic development process for patient decision aids. BMC Med Inform Decis Mak. 2013;13(2):S2. | ||
Liebherz S, Härter M, Dirmaier J, Tlach L. Information and decision-making needs among people with anxiety disorders: results of an online survey. Patient. 2015;8(6):531–539. | ||
Francis JJ, Johnston M, Robertson C, et al. What is an adequate sample size? Operationalising data saturation for theory-based interview studies. Psychol Health. 2010;25(10):1229–1245. | ||
Morgan DL. Focus groups As Qualitative Research. Thousand Oaks, CA: Sage Publications; 1997. | ||
Mayring P. Qualitative Inhaltsanalyse. Grundlagen und Techniken [Qualitative content analysis: theoretical foundation and basic procedures]. Vol 10. Weinheim und Basel: Beltz Verlag; 2008. | ||
MAXQDA. Software for Qualitative Analysis. Berlin: VERBI- Software Consult Sozialforschung; 2010. | ||
Brom L, Hopmans W, Pasman HRW, Timmermans DR, Widdershoven GA, Onwuteaka-Philipsen BD. Congruence between patients’ preferred and perceived participation in medical decision-making: a review of the literature. BMC Med Inform Decis Mak. 2014;14(1):25. | ||
Loos S, Neumann P, Arnold K, et al. Shared decision-making in the treatment of people with severe mental illness–a focus group study. Psychiat Prax. 2013;40(1):23–29. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
