Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 13
Chinese version of the severe respiratory insufficiency questionnaire for patients with COPD receiving long-term oxygen therapy
Authors Guan LL, Xu JW , Wu WL, Chen JH, Li XY , Guo BP, Yang YQ, Huo YT, Zhou LQ, Chen RC
Received 5 November 2017
Accepted for publication 29 January 2018
Published 11 May 2018 Volume 2018:13 Pages 1537—1543
DOI https://doi.org/10.2147/COPD.S156135
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Chunxue Bai
Lili Guan,1,* Jiawen Xu,1,* Weiliang Wu,1,* Jianhua Chen,1,* Xiaoying Li,2,* Bingpeng Guo,1 Yuqiong Yang,1 Yating Huo,1 Luqian Zhou,1 Rongchang Chen1
1State Key Laboratory of Respiratory Disease, Guangzhou Institute of Respiratory Disease, The First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China; 2The First Affiliated Hospital, School of Clinical Medicine of Guangdong Pharmaceutical University, Guangzhou, China
*These authors contributed equally to this work
Purpose: Patients with advanced-stage COPD often experience severe hypoxemia. Treatment with long-term oxygen therapy (LTOT) may relieve patients’ symptoms and increase survival. As COPD is incurable, improving patients’ health-related quality of life is important. The Chinese version of the Severe Respiratory Insufficiency Questionnaire (SRI) is valid for patients with hypercapnic COPD undergoing noninvasive positive airway pressure ventilation at home. However, the reliability and validity of the Chinese SRI for patients with COPD undergoing LTOT have not been investigated.
Patients and methods: We analyzed reliability using Cronbach’s α coefficient. Construct validity was assessed with principal, exploratory, and confirmatory factor analysis. Concurrent validity was evaluated through the correlation between SRI domains and Chronic Respiratory Disease Questionnaire (CRQ) domains. Content validity was assessed by calculating the correlation between each SRI item score and the total score for the relevant domain.
Results: In total, 161 patients participated in this study. The Cronbach’s α coefficient for all SRI domains was >0.7, except for the attendant symptoms and sleep domain. Exploratory and confirmatory factor analysis showed a good model fit for each domain, but the factors extracted from each domain were correlated. SRI and CRQ domains correlated well with respect to similar aspects of health-related quality of life, indicating good concurrent validity. Content validity was indirectly shown by a good correlation between each item score and the total score of the relevant domain.
Conclusion: The Chinese version of the SRI has a good reliability and validity for patients with COPD undergoing LTOT in China.
Keywords: severe respiratory insufficiency questionnaire, long-term oxygen therapy, health-related quality of life, chronic obstructive pulmonary disease
Introduction
COPD is a general, preventable, and treatable disease characterized by sustained respiratory symptoms and airflow limitation. COPD is the main reason for morbidity and mortality worldwide.1 The overall prevalence of COPD in China is 8.2%,2 and it has become the third most common cause of death.3 In addition, the disease burden in China is expected to increase over the next few decades because of continuous exposure to risk factors and population aging.
Advanced-stage COPD is characterized by severe hypoxemia and/or hypercapnia resulting from decreased diffusing capacity, inspiratory muscle fatigue, and alveolar hypoventilation. Long-term oxygen therapy (LTOT) can relieve patients’ symptoms, improve health-related quality of life (HRQL), and increase survival.4 The management of patients with advanced-stage COPD has been receiving increasing attention. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) guideline indicates that advanced-stage COPD is a highly symptomatic disease, and affected patients’ pulmonary function cannot return to the basal level.5 Therefore, it is important to relieve symptoms, slow disease progression, and improve HRQL for patients with COPD. HRQL questionnaires (generic and disease-specific) are used to evaluate the everyday quality of life of patients affected by various diseases.6 Currently, various COPD-specific questionnaires are used to evaluate HRQL among patients with COPD undergoing LTOT, including the Chronic Respiratory Disease Questionnaire (CRQ)7 and the St George’s Respiratory Questionnaire.8 While these questionnaires are designed for general patients with COPD, many important aspects of HRQL for those with advanced-stage COPD may not be included, resulting in a missing part in the assessment of quality of life for COPD patients across the whole spectrum.
The Severe Respiratory Insufficiency Questionnaire (SRI) has been used for patients undergoing domiciliary noninvasive ventilation.9 It has been shown that the SRI has good psychometric properties, and it has been verified in this patient population. Struik et al10 demonstrated that the SRI was the best tool for assessing HRQL among patients with COPD exhibiting chronic respiratory failure. In addition, Walterspacher et al11 showed that the SRI was valid for patients with COPD undergoing LTOT. The SRI was originally developed in German9 and has been translated into many languages, including English, Spanish, Norwegian, French, Portuguese, Japanese, and Chinese.12–18 Our team previously translated the SRI into Chinese and showed that it has a good reliability and validity for patients with COPD undergoing long-term noninvasive ventilation.18 To date, no published work has demonstrated whether the Chinese version of the SRI can be used for patients with COPD undergoing LTOT. Therefore, the purpose of this study aimed to evaluate the reliability and validity of the Chinese version of the SRI in assessing the quality of life among Chinese patients with COPD undergoing domiciliary LTOT.
Patients and methods
This study was part of a multicenter, prospective, randomized controlled clinical trial to assess the effect of noninvasive ventilation among patients with chronic hypercapnic COPD (ClinicalTrials.gov number NCT02499718). Approval for this study was obtained from the Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China. All participating patients provided written informed consent before the study started.
In total, 161 patients were included in this study (126 males, 35 females). Patients were required to complete both the SRI and the CRQ when they were recruited from the outpatient department. Spirometry (Jaeger, Wuerzburg, Germany) was accomplished using a standardized process in line with the guideline of the American Thoracic Society/European Respiratory Society.19 All participating patients had COPD with stable chronic respiratory failure, and had experienced no acute exacerbations for 1 month. Acute exacerbations were defined as new onset or worsening of more than one respiratory symptom lasting for ≥2 consecutive days and leading to any changes in conventional therapy.20 All included patients received regular optimal pharmacological treatments according to the GOLD guideline,5 and were required to undergo home LTOT for >4 weeks before inclusion.11 Exclusion criteria were LTOT due to other lung/pleural diseases, thoracic deformities, and other diseases.
HRQL questionnaires
Translation of the Chinese version of the SRI was consistent with the translation and backtranslation procedure described in our previous study.18 First, the original version of the SRI was independently translated into Chinese by two translators. A committee comprising the two translators and the project manager examined both forward translations and reconciled them into a single forward translation. Next, the reconciled translation was backtranslated into German by a third translator who had not seen the original questionnaire. The committee then examined the back translation to assure the conceptual equivalence of the translation.
The SRI9 (Supplementary materials) contains 49 items relating to the general condition of the patient during the previous week on seven domains: respiratory complaints (RC), physical functioning (PF), attendant symptoms and sleep (AS), social relationships (SR), anxiety (AX), psychological well-being (WB), and social functioning (SF). A summary scale (SS) can be obtained from the mean scores for the seven domains. Each item is rated on a 5-point Likert scale (1 = completely untrue, 2 = mostly untrue, 3 = sometimes true, 4 = mostly true, and 5 = always true). Each domain has a possible score of 0–100 following transformation of raw values. Higher scores imply better HRQL.
The CRQ7 (Supplementary materials) is a COPD-specific questionnaire used worldwide. The scale comprises 20 items on four domains: dyspnea, fatigue, emotional functioning, and mastery. Items are rated on a 7-point Likert scale from 1 (maximum impairment) to 7 (no impairment). Lower scores indicate worse HRQL.
Statistical analysis
The data analysis was performed with SPSS version 21.0 (IBM Corp., Armonk, NY, USA) and Amos 21.0. Data are presented as n (%) or mean (standard deviation). A p-value of <0.05 was considered statistically significant. The percentage of patients with maximal or minimal domain or summary scores was calculated for each questionnaire to determine floor and ceiling effects. The floor or ceiling effects were considered high if these percentages were >15%.21 Reliability was determined by analyzing internal consistency as calculated using Cronbach’s α coefficient. A Cronbach’s α coefficient of >0.70 was considered good.22 Validity was assessed by measuring construct, concurrent, and content validity. After examining the scale structure, construct validity was obtained using principal component analysis (PCA), exploratory factor analysis (EFA), and confirmatory factor analysis (CFA). The test and Bartlett’s test were performed to determine whether the data were amenable to PCA and EFA. PCA and EFA were performed using SPSS (version 21.0; IBM Corp.), and only factors with eigenvalues greater than unity (>1) were extracted. CFA, performed with Amos 21.0, was then used to inspect the results obtained through EFA. If more than one factor was extracted from a domain, CFA was used to determine whether the factors were related to each other. Model fit was assessed with the goodness-of-fit index (GFI) and comparative fit index (CFI). A GFI and CFI of >0.9 indicate good model fit. The concurrent validity of the SRI was tested by comparing each SRI domain with the relevant CRQ domain. Content validity was indirectly obtained by correlating the score for each item with the total score for the relevant domain to determine whether each item reflected the purpose of each domain; R-values of >0.50 and p-values of <0.05 were considered good.
Results
In total, 161 patients with COPD characterized by stable chronic respiratory failure undergoing LTOT were included in this study. Patients’ mean age was 68.54 years (7.43 years), and 126 (78.26%) of them were male. All patients had severe airflow limitation with a predicted mean forced expiratory volume in 1 second of 25.63% (9.59%). Detailed demographic data and clinical features of included patients are shown in Table 1.
Questionnaire scores
Table 2 shows participants’ SRI and CRQ scores. The mean scores for the SRI-SS and CRQ-Summary were 56.02 (11.95) and 4.47 (0.80), respectively. The highest mean domain scores were found in the SRI-SR and CRQ-Emotion domains. The SRI-PF and CRQ-Dyspnea domains had the lowest mean domain scores.
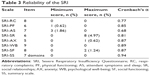
Reliability
The maximum percentage of patients with the maximal or minimal domain score or summary score was 4.97%, indicating no floor or ceiling effects were detected in the SRI. The Cronbach’s α coefficients for the seven SRI domains ranged from 0.68 to 0.89. The coefficient for the SRI-SS domain was higher at 0.94 (Table 3).
Validity
Construct validity
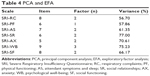
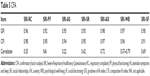
The Kaiser–Meyer–Olkin test values for the seven SRI domains were >0.7. Bartlett’s test showed statistically significant differences (p<0.01), indicating that all domains were suitable for PCA and EFA. One factor was extracted from SRI-PF; two factors from SRI-RC, SRI-AS, SRI-SR, SRI-AX, and SRI-SF; and three factors from SRI-WB. The proportion of the total variance that accounted for the extracted factors in the seven domains varied from 56.70% to 77.00% (Table 4). Based on these results, CFA was performed to confirm validity. Table 5 shows that the GFI and CFI of each domain were >0.9, indicating a good model fit for each domain. However, the extracted factors in each domain were correlated (r-values of 0.22–0.79).
Concurrent validity
The correlation matrix of the SRI and CRQ is shown in Table 6. The SRI-SS was well correlated with all CRQ domains. The best correlations were between SRI-WB and CRQ-Emotion (r=0.78) and between SRI-SS and CRQ-Summary (r=0.77). SRI-AS and SRI-SR were not correlated with CRQ-Dyspnea. Overall, the SRI and CRQ domains were well correlated with respect to similar aspects of HRQL.
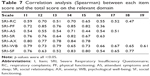
Content validity
Table 7 shows that good content validity was indirectly proven by calculating the correlation between each item score and the total score on the relevant domain. The correlation coefficients were >0.5 among 46 items (93.88%). All correlations were significant (p<0.05).
Discussion
This study is the first to validate the Chinese version of the SRI among patients with COPD exhibiting chronic respiratory failure undergoing LTOT. Our data indicated the Chinese version of the SRI had good reliability and validity.
In this study, the percentage of patients with a maximal or minimal domain score for a respective domain ranged from 0% to 4.97% (all <15%), indicating no floor or ceiling effects in the SRI. Cronbach’s α coefficients for all domains except SRI-AS were >0.7 (range 0.68–0.94). However, the Cronbach’s α coefficient for SRI-AS approximately reached 0.7, which was acceptable and higher compared with other versions of the SRI.9,12–18 Moreover, a previous study demonstrated that the Cronbach’s α coefficients for the German SRI ranged from 0.69 to 0.93 when used for COPD patients with LTOT,11 which was similar to our study. The differences between that study and our study were that our sample size was larger and all of our patients were both hypoxemic and hypercapnic.
We assessed construct, concurrent, and content validity. Construct validity was obtained through PCA, EFA, and CFA. PCA and EFA extracted one factor from one domain, two factors from five domains, and three factors from the remaining domain. Subsequent CFA demonstrated a good model fit for each domain (GFI and CFI for all domains were >0.9). For example, in SRI-WB, one factor represented patients’ anger, another factor represented sorrow, and the remaining factor represented self-perception. The factors extracted from each domain were correlated and not independent; therefore, the primary structure of the SRI could be retained. The CRQ7 is used worldwide to assess HRQL among patients with COPD. The correlation matrix of the SRI and CRQ showed that the best correlation (r=0.78) was between domains focused on emotion (SRI-WB and CRQ-Emotion). This finding is consistent with previous studies23,24 and indicates that emotion accounts for a large part of both the SRI and CRQ. Moreover, SRI-SS and CRQ-Summary were well correlated, and the same finding was obtained when the SRI and CRQ captured similar HRQL characteristics, indicating the SRI had good concurrent validity. However, there was no correlation between the SRI-AS/SRI-SR domains and the CRQ-Dyspnea domain. This may be explained by the fact that the SRI-AS and SRI-SR items did not focus on patients’ dyspnea. Therefore, different domains that focused on different aspects were not significantly correlated, consistent with previous studies.9,12–14,16,17 We also observed that the correlations between each SRI domain and CRQ-Dyspnea were not high when compared with other domains. This may be because the SRI was originally designed for patients with chronic respiratory failure, whereas the CRQ was designed for general use in patients with COPD. Furthermore, the SRI focuses on the effect of dyspnea on patients’ daily life, whereas the CRQ is concerned with the degree of dyspnea. Good content validity was demonstrated through the relationship between each item score and the relevant domain total score. The r-values of all (except three) items were >0.5. However, these three items’ r-values were approximately >0.4, indicating good correlations between these items and the relevant domains.
Several previous studies comparing the effect of noninvasive ventilation and LTOT for patients with COPD produced controversial results with respect to improvement in HRQL.25–28 Moreover, evidence that LTOT can improve HRQL is lacking.4,29–31 This may be because different questionnaires were used to evaluate HRQL, some of which only partly appraise HRQL.
Limitations
This study had two main limitations. First, we only included patients with COPD; we did not evaluate patients requiring LTOT for other diseases. Second, some patients could not stop oxygen therapy before taking arterial blood gas analysis because of the severity of their disease condition.
Conclusion
The Chinese version of the SRI has good reliability and validity for patients with COPD undergoing LTOT in China. The validated SRI is capable of evaluating the HRQL of these patients and can be incorporated in future clinical trials. In future studies, Chinese version of the SRI is needed to evaluate the COPD patient’s HRQL of overseas Chinese, and more versions of the SRI in different languages are needed to evaluate patient’s HRQL in other countries.
Acknowledgments
We thank Prof Mei Jiang, who is a PhD in statistics from the First Affiliated Hospital of Guangzhou Medical University, and Prof Jihui Zhang, who is an epidemiologist from Chinese University of Hong Kong, for confirming the statistic results and editing the English of this manuscript. We also thank Angela Morben, MD, from Liwen Bianji, Edanz Editing China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript. The study was supported by the Science and Technology Project of Guangdong Province (2017A020211018) and the Guangzhou Healthcare Collaborative Innovation Major Project (201604020012) and State’s Key Project of Research and Development Plan (2017YFC1310600).
Author contributions
RC Chen, LQ Zhou, and LL Guan contributed to the conception and design of the study, drafting the submitted article, and revising the draft critically for important intellectual content. WL Wu, JW Xu, JH Chen, and XY Li contributed to the data acquisition, the interpretation of outcomes, data analysis, and drafting the submitted article. RC Chen, LQ Zhou, and LL Guan contributed to the crucial revision of the draft for important intellectual content and providing final manuscript approval. BP Guo, YQ Yang, and YT Huo contributed to following up the patients and collecting, extracting and analyzing the data. All authors contributed to data analysis, drafting the manuscript, amending the paper, and being responsible for all aspects of the work. All the data were accessible to all of the authors, and all of the authors assure the accuracy of the reported data.
Disclosure
The authors report no conflicts of interest in this work.
References
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):2011–2030. | ||
Zhong N, Wang C, Yao W, et al. Prevalence of chronic obstructive pulmonary disease in China: a large, population-based survey. Am J Respir Crit Care Med. 2007;176(8):753–760. | ||
Zhou M, Wang H, Zhu J, et al. Cause-specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet. 2016;387(10015):251–272. | ||
Cranston JM, Crockett A, Moss J, Alpers JH. Domiciliary oxygen for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2005;(4):CD001744. | ||
Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management and Prevention of COPD, 2017. Available from: http://goldcopd.org/gold-2017-global-strategy-diagnosis-management-prevention-copd/. Accessed March 27, 2018. | ||
Higginson IJ. Measuring quality of life: using quality of life measures in the clinical setting. BMJ. 2001;322(7297):1297–1300. | ||
Guyatt G, Berman L, Townsend M, Pugsley S, Chambers L. A measure of quality of life for clinical trials in chronic lung disease. Thorax. 1987;42(10):773–778. | ||
Jones PW, Quirk FH, Baveystock CM. The St George’s respiratory questionnaire. Respir Med. 1991;85:25–31. | ||
Windisch W, Freidel K, Schucher B, et al. The Severe Respiratory Insufficiency (SRI) Questionnaire: a specific measure of health-related quality of life in patients receiving home mechanical ventilation. J Clin Epidemiol. 2003;56(8):752–759. | ||
Struik FM, Kerstjens HAM, Bladder G, et al. The Severe Respiratory Insufficiency Questionnaire scored best in the assessment of health-related quality of life in chronic obstructive pulmonary disease. J Clin Epidemiol. 2013;66(10):1166–1174. | ||
Walterspacher S, July J, Kohlhaufl M, Rzehak P, Windisch W. The Severe Respiratory Insufficiency Questionnaire for subjects with COPD with long-term oxygen therapy. Respir Care. 2016;61(9):1186–1191. | ||
Ghosh D, Rzehak P, Elliott MW, Windisch W. Validation of the english severe respiratory insufficiency questionnaire. Eur Respir J. 2012;40(2):408–415. | ||
López-Campos JL, Failde I, Masa JF, et al. Transculturally adapted Spanish SRI questionnaire for home mechanically ventilated patients was viable, valid, and reliable. J Clin Epidemiol. 2008;61(10):1061–1066. | ||
Markussen H, Lehmann S, Nilsen RM, Natvig GK. The Norwegian version of the Severe Respiratory Insufficiency Questionnaire. Int J Nurs Pract. 2015;21(3):229–238. | ||
Cuvelier A, Lamia B, Molano LC, Muir JF, Windisch W. The French translation and cultural adaptation of the SRI questionnaire. A questionnaire to assess health-related quality of life in patients with chronic respiratory failure and domiciliary ventilation. Rev Mal Respir. 2012;29(5):705–713. | ||
Ribeiro C, Ferreira D, Conde S, Oliveira P, Windisch W. Validation of the portuguese severe respiratory insufficiency questionnaire for home mechanically ventilated patients. Rev Port Pneumol. 2017;23(3):139–145. | ||
Oga T, Taniguchi H, Kita H, et al. Validation of the Japanese Severe Respiratory Insufficiency Questionnaire in hypercapnic patients with noninvasive ventilation. Respir Investig. 2017;55(2):166–172. | ||
Chen R, Guan L, Wu W, et al. The Chinese version of the Severe Respiratory Insufficiency questionnaire for patients with chronic hypercapnic chronic obstructive pulmonary disease receiving non-invasive positive pressure ventilation. BMJ Open. 2017;7(8):e017712. | ||
Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. | ||
Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet. 2007;370(9589):786–796. | ||
Terwee CB, Bot SDM, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42. | ||
Health measurement scales: a practical guide to their development and use (5th edition). Aust N Z J Public Health. 2016;40(3):294–295. | ||
Hajiro T, Nishimura K, Tsukino M, Ikeda A, Koyama H, Izumi T. Comparison of discriminative properties among disease-specific questionnaires for measuring health-related quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157(3 Pt 1):785–790. | ||
Duiverman ML, Wempe JB, Bladder G, Kerstjens HAM, Wijkstra PJ. Health-related quality of life in COPD patients with chronic respiratory failure. Eur Respir J. 2008;32(2):379–386. | ||
McEvoy RD, Pierce RJ, Hillman D, et al. Nocturnal non-invasive nasal ventilation in stable hypercapnic COPD: a randomised controlled trial. Thorax. 2009;64(7):561–566. | ||
Struik FM, Sprooten RTM, Kerstjens HAM, et al. Nocturnal non-invasive ventilation in COPD patients with prolonged hypercapnia after ventilatory support for acute respiratory failure: a randomised, controlled, parallel-group study. Thorax. 2014;69(9):826–834. | ||
Köhnlein T, Windisch W, Köhler D, et al. Non-invasive positive pressure ventilation for the treatment of severe stable chronic obstructive pulmonary disease: a prospective, multicentre, randomised, controlled clinical trial. Lancet Respir Med. 2014;2(9):698–705. | ||
Zhou L, Li X, Guan L, et al. Home noninvasive positive pressure ventilation with built-in software in stable hypercapnic COPD: a short-term prospective, multicenter, randomized, controlled trial. Int J COPD. 2017;12:1279–1286. | ||
Abernethy AP, McDonald CF, Frith PA, et al. Effect of palliative oxygen versus room air in relief of breathlessness in patients with refractory dyspnoea: a double-blind, randomised controlled trial. Lancet. 2010;376(9743):784–793. | ||
Hardinge M, Suntharalingam J, Wilkinson T. Guideline update: The British Thoracic Society Guidelines on home oxygen use in adults. Thorax. 2015;70(6):589–591. | ||
Ekström M. Clinical usefulness of long-term oxygen therapy in adults. N Engl J Med. 2016;375(17):1683–1684. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.