Back to Journals » Drug Design, Development and Therapy » Volume 10
Chinese herbal medicine, Jianpi Ligan decoction, improves prognosis of unresectable hepatocellular carcinoma after transarterial chemoembolization: a retrospective study
Authors Tang CW, Zhu M, Feng WM, Bao Y, Zheng YY
Received 21 May 2016
Accepted for publication 22 June 2016
Published 3 August 2016 Volume 2016:10 Pages 2461—2466
DOI https://doi.org/10.2147/DDDT.S113295
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Wei Duan
Cheng Wu Tang,1 Ming Zhu,2 Wen Ming Feng,1 Ying Bao,1 Yin Yuan Zheng3
1Department of General Surgery, 2Department of Nephrology, 3Department of Radiology, First People’s Hospital Affiliated to Huzhou University Medical College, Huzhou, People’s Republic of China
Objective: This study aimed to investigate the efficacy of Jianpi Ligan decoction (JLD) as an adjuvant therapy for patients with unresectable hepatocellular carcinoma (HCC) treated by transarterial chemoembolization (TACE).
Methods: From March 2007 to March 2013, 103 patients with unresectable HCC who underwent TACE in our center were included in this retrospective study. Among the 103 patients, 53 patients accepted JLD along with TACE (JLD group) and 50 patients accepted TACE alone (control group). Indices including complication, toxicity, treatment success rate, and long-term survival were obtained for analysis and comparison.
Results: There was no significant difference in patient characteristics between the two groups. No procedure-related deaths or encephalopathy occurred. Fewer patients from the JLD group experienced constipation (7/53 vs 15/50, P=0.0377), abdominal bloating (5/53 vs 12/50, P=0.0466), and lack of appetite (35/53 vs 42/50, P=0.0360). The JLD group had lesser and lighter hepatic toxicity (P=0.0265) and gastrointestinal toxicity (P=0.0445) such as nausea and vomiting. The JLD group had a significantly higher treatment success rate than the control group (51/53 vs 40/50, P=0.0103). Three-year overall survival probability was significantly higher in the JLD group than in the control group (37.74% vs 26.00%; hazard ratio [HR] 0.6171; 95% confidence interval [CI], 0.3832–0.9938; P=0.0365 by log-rank test). No significant difference was found in 3-year overall survival probability (39.22% vs 32.50%; HR, 0.7449; 95% CI, 0.4398–1.2614; P=0.2491 by log-rank test) or 3-year intrahepatic recurrence-free survival probability in patients who achieved treatment success (37.25% vs 30.00%; HR, 0.7280; 95% CI, 0.4332–1.2233; P=0.2087 by log-rank test) between the two groups.
Conclusion: Application of JLD was effective for reduction of side effects and improvement of long-term survival for patients with unresectable HCC treated by TACE.
Keywords: hepatocellular carcinoma, transarterial chemoembolization, traditional Chinese medicine, overall survival
Introduction
Hepatocellular carcinoma (HCC), a common malignant tumor, is the fifth leading cause of tumor death in the world with an estimated incidence of more than one million new cases per year.1 Surgical resection and liver transplantation are the potentially curative HCC treatments, but less than 30% of patients are surgical candidates due to tumor extension, poor hepatic functional reserve, or underlying liver cirrhosis.2–4 Hence, new strategies to combat HCC are urgently needed. On the basis of the fact that liver tumors derive their blood supply (90%–95%) mainly from the hepatic artery, whereas blood supply to liver tissues is delivered via the portal system, transarterial chemoembolization (TACE) is considered to be an effective treatment for patients with HCC who are not suitable candidates for surgical operation.5 However, severe side effects including liver and renal failure, bone marrow depression, postembolization syndrome, and liver abscess were observed after TACE. Treatment is discontinued or delayed if intolerable side effects occur, which limits its overall therapeutic effect. Therefore, the long-term efficacy of this treatment is not satisfactory, and 5-year survival rate is lower than 10%.6,7
In contrast to western medicine, there is accumulating evidence suggestive of beneficial effects of plants used in traditional Chinese medicine (TCM) and compounds isolated from medicinal plants.8,9 Increasing number of studies suggested that TCMs could improve the efficacy and relieve the side effects of TACE for patients with unresectable primary liver cancer.10 In clinical practice, we found that the Chinese herbal decoction Jianpi Ligan decoction (JLD) could relieve the side effects caused by TACE. The aim of the present retrospective study was to clarify the efficacy of JLD as an adjuvant therapy for unresectable HCC patients treated with TACE.
Methods
Patients
Between March 2007 and March 2013, 103 patients with unresectable HCC who underwent TACE treatment in First People’s Hospital Affiliated to Huzhou University Medical College were enrolled in this retrospective study. Among those patients, 53 patients accepted JLD along with TACE (JLD group) and 50 patients accepted TACE alone (control group). The diagnosis of HCC was established either by histopathology or typical appearance of HCC on two sets of imaging studies (ultrasonography, computed tomography [CT], angiography, magnetic resonance imaging [MRI]) and based on high plasma levels of a serum alfa-fetoprotein value exceeding 400 ng/mL.11 Inclusion criteria were as follows: 1) age ≤75 years, Karnofsky performance score ≥70; 2) no indication for resection; 3) no previous systemic or local treatment; 4) liver function of Child–Pugh A–B; 5) no portal vein thrombosis or extrahepatic metastasis; 6) no refractory ascites or renal failure; and 7) complete clinicopathologic and follow-up data.
This study was conducted in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice guidelines. Written informed consent was obtained from all the patients. Approval of the study was obtained from the Institutional research ethics committee of First People’s Hospital affiliated to Huzhou University Medical College.
Treatment
TACE was performed according to the Seldinger technique.12 After recognizing the feeding artery of the liver tumor under hepatic arteriography, chemotherapeutic agents (5-fluorouracil 1,000 mg/m2, cisplatin 80 mg/m2) were slowly infused followed by 5–30 mL lipiodol with mitomycin-C (6 mg/m2) emulsion for embolization. The doses of chemotherapeutic agents were adjusted according to liver function and peripheral leukocyte or platelet levels. Stump occlusion of segmental or subsegmental feeding branches was performed with microfibrillar collagen (Avitene; Davol Inc., Cranston RI, USA) as needed to achieve stasis.
TACE was usually repeated every ~4 weeks; each TACE required hospitalization for 7–10 days, and hospitalization time was prolonged in patients with serious damage to liver function, bone marrow depression, or other major complications after TACE procedure.
Treatment efficacy was assessed by enhanced CT within 2 weeks after TACE. Treatment success was defined as no residue tissue in the liver detected by follow-up imaging. Once treatment success was achieved, no more TACE was delivered. TACE treatment was stopped once treatment success was accomplished or life-threatening side effects occurred.
The composition of JLD (Table 1) consisted of Radix Codonopsis 20 g, Rhizoma Atractylodis macrocephala 10 g, Poria cocos 15 g, Radix Glycyrrhizae 5 g, Rhizoma Diosscoreae 15 g, Rhizoma Pinelliae 10 g, Fructus Crataegi 15 g, lotus seed 20 g, Herba Artemisia Scoparia 50 g, and Pericarpium Arecae 25 g, which were purchased from Hangzhou Hu Qing Yu Tang Pharmaceutical Co., Ltd (Hangzhou, People’s Republic of China). Herbal mixtures were made based on remedy menu by an experienced Chinese medicine practitioner. The herbal decoction was initially administered on the day of the performance of TACE and continued for 5 days after TACE.
  | Table 1 Components of Jianpi Ligan decoction with Latin and English names |
Outcome measurements and follow-up
The side effects including complications and toxicities were assessed. A major complication was defined as an event that caused substantial morbidity and disability, increased the level of care required, and resulted in hospital admission or substantial lengthening of hospitalization. All other complications were considered minor.13 Toxicity was assessed before starting each treatment using the Common Toxicity Criteria of National Cancer Institute. According to these criteria, a score of 1 indicates mild adverse effects, a score of 2 indicates moderate adverse effects, a score of 3 indicates severe adverse effects, and a score of 4 indicates life-threatening adverse effects. Patients who failed to achieve treatment success received symptomatic treatment and supportive care instead of TACE after treatment discontinuation.
After the last TACE session, the patients were assessed every 3 months for 2 years and every 6 months thereafter by enhanced CT, ultrasonography, serum biochemistry, and clinical examination. The patients were followed up until the last follow-up or death. Overall survival was measured from the date of treatment initiation to death or the date of last follow-up. Intrahepatic recurrence-free survival of the patients who achieved treatment success was measured from the date of treatment initiation to intrahepatic recurrence, death, or last follow-up, whichever came first. Intrahepatic recurrence was defined as new lesions distant from the initial tumors or local tumor recurrence and was diagnosed on the basis of imaging and, if necessary, cytologic analysis or biopsy. According to our ethical committee, all the patients with relapsing or progressive tumors were treated with the best possible options (such as repeated TACE, radiofrequency ablation, supportive care).
Statistical analysis
All the measurements were expressed as mean ± standard deviation. The statistical analyses were performed using the two-sample Student’s t-test and adjusted chi-square test for the two groups. The exact chi-square test was also used if individual cell size was less than 5 counts. Ridit analysis was used to compare the toxicities of the two groups. Overall survival and intrahepatic recurrence-free survival were analyzed by the Kaplan–Meier method, and survival curves were compared by the log-rank test. P-value <0.05 was considered statistically significant.
Results
Patient characteristics
There were no statistically significant differences between the two groups in patient characteristics, in terms of age, sex, Karnofsky performance score, alfa-fetoprotein level, Child–Pugh class, number of tumors, main tumor size, and background liver disease (Table 2).
  | Table 2 Patient characteristics |
Treatment success
In the JLD group, treatment success was achieved in 51 patients: after three TACE sessions in 30 patients and four TACE sessions in 21 patients. In the control group, treatment success was achieved in 40 patients: after three TACE sessions in 22 patients and four TACE sessions in 18 patients (Table 3). The JLD group had a significantly higher treatment success rate than the control group (51/53 vs 40/50, P=0.0103).
  | Table 3 Treatment success |
Complication and toxicity
No procedure-related deaths or encephalopathy occurred. Complications are shown in Table 4. Fewer patients from the JLD group experienced constipation (7/53 vs 15/50, P=0.0377), abdominal bloating (5/53 vs 12/50, P=0.0466), and lack of appetite (35/53 vs 42/50, P=0.0360). Details of toxicity are shown in Table 5. A total of 12 patients (ten from the control group and 2 from the JLD group) developed grade 4 toxicities, which led to termination of TACE. The JLD group had lesser and lighter hepatic toxicity (P=0.0265) and gastrointestinal toxicity (P=0.0445) such as nausea and vomiting.
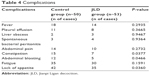  | Table 4 Complications |
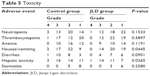  | Table 5 Toxicity |
Overall survival
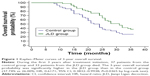
A total of 70 patients died during the first 3 years after treatment initiation, including 37 patients from the control group and 33 patients from the JLD group. In all, 25 patients in the control group and 21 patients in the JLD group died of progression of HCC. Other deaths were caused by hepatic failure. The 3-year overall survival probability was significantly higher in the JLD group than in the control group (37.74% vs 26.00%; hazard ratio [HR], 0.6171; 95% confidence interval [CI], 0.3832–0.9938; P=0.0365 by log-rank test) (Figure 1). Further, we performed survival analysis of the patients who achieved treatment success. Among those patients, 27 patients from the control group and 31 patients from the JLD group died during the first 3 years after treatment initiation. We found that there was no significant difference in the 3-year overall survival probability of patients who achieved treatment success between the two groups (39.22% vs 32.50%; HR, 0.7449; 95% CI, 0.4398–1.2614; P=0.2491 by log-rank test) (Figure 2).
Intrahepatic recurrence-free survival
Intrahepatic recurrence-free survival was analyzed in patients who achieved treatment success. A total of 60 patients developed intrahepatic recurrence during the first 3 years after treatment initiation including 28 of 40 patients from the control group and 32 of 51 patients from the JLD group. There was no significant difference in 3-year intrahepatic recurrence-free survival probability in patients who achieved treatment success (37.25% vs 30.00%; HR, 0.7280; 95% CI, 0.4332–1.2233; P=0.2087 by log-rank test) (Figure 3).
Discussion
TACE has been shown to provide a survival benefit as a palliative treatment modality for patients with unresectable HCC.14 Although a relatively safe procedure, TACE usually causes severe side effects that may halt the treatment and even result in TACE-related deaths or encephalopathy.15 Therefore, it is necessary to seek an approach to reduce the side effects of TACE. TCM, used in the People’s Republic of China for a long time, has a unique theoretical system and practical approach to the treatment of diseases. Various formulas of Chinese herbal medicine were utilized as adjuvant treatment for patients with HCC undergoing TACE, radiofrequency ablation, or surgery and were found to have a positive effect in preventing and treating side effects after TACE.16–18 Therefore, utilization of TCM may effectively improve the tolerability and therapeutic effect of TACE.
JLD in the present study has been used as an adjuvant therapy for unresectable HCC in our hospitals for a long time. In the prescription, Codonopsis pilosula mainly tonifies the spleen and improves immunity, supplemented by Rhizoma Atractylodis macrocephala. Rhizoma Pinelliae, Fructus Crataegi, and Rhizoma Diosscoreae tonify the stomach, improve digestion, and relieve constipation. Poria cocos and Pericarpium Arecae promote urination and eliminate ascites. Lotus seed has the effects of clearing heat and tranquilization. Radix Glycyrrhizae promotes detoxification and liver protection. Herba Artemisia scoparia clears jaundice and promotes the recovery of liver function. All these ingredients are well organized and integrated in JLD with enhanced functions. In present study, we found that JLD significantly reduced occurrence of complications and toxicities caused by TACE including gastrointestinal adverse reaction, hepatic toxicity, lack of appetite, abdominal bloating, and constipation.
Moreover, we found that JLD effectively attenuated the severity of side effects. Among those patients who experienced side effects, two patients from the JLD group and ten from the control group developed grade 4 toxicities and failed to achieve treatment success. Consequently, the JLD group had a significantly higher treatment success rate than the control group.
Several randomized clinical trials reported that patients with unresectable HCC treated by TACE had a 3-year overall survival rates ranging from 26% to 47%.3,19,20 Prognosis was even worse in patients who developed severe complications after TACE.21 In our study, the 3-year overall survival probability was 37.74% in the JLD group and 26.00% in the control group. The results of survival analysis in our study suggested that the JLD group had a significantly higher 3-year overall survival probability than the control group (P=0.0365 by log-rank test). However, we found no significant difference in the 3-year overall survival probability (P=0.2491 by log-rank test) or the 3-year intrahepatic recurrence-free survival probability (P=0.2087 by log-rank test) of patients who achieved treatment success in the two groups. The improvement of prognosis in the JLD group could be associated with a higher treatment success rate of TACE as a result of lesser and lighter side effects.
Conclusion
In conclusion, the application of JLD was effective for the reduction of side effects and improvement of long-term survival for patients with unresectable HCC treated by TACE, though the precise mechanisms of therapeutic effects of JLD on patients require further exploration. Because of the retrospective nature and the small sample size, further prospective studies with large sample size are needed to confirm the results of our study.
Acknowledgment
This work was supported by Zhejiang Applied Research Projects of Public Welfare (grant no 2013C33109).
Author contributions
Cheng Wu Tang, Ming Zhu, and Yin Yuan Zheng designed the study and wrote the manuscript. Cheng Wu Tang and Ming Zhu contributed equally to this study. Wen Ming Feng and Cheng Wu Tang conducted patients’ management and monitoring; Ying Bao provided the collection of all the human materials. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
Ying Bao provided financial support for this work. The authors report no other conflicts of interest in this work.
References
Llovet JM. Updated treatment approach to hepatocellular carcinoma. J Gastroenterol. 2005;40(3):225–235. | ||
Llovet JM, Schwartz M, Mazzaferro V. Resection and liver transplantation for hepatocellular carcinoma. Semin Liver Dis. 2005;25(2):181–200. | ||
Lo CM, Ngan H, Tso WK, et al. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology. 2002;35(5):1164–1171. | ||
Tang C, Shen J, Feng W, et al. Combination therapy of radiofrequency ablation and transarterial chemoembolization for unresectable hepatocellular carcinoma: a retrospective study. Medicine (Baltimore). 2016;95(20):e3754. | ||
Breedis C, Young G. The blood supply of neoplasms in the liver. Am J Pathol. 1954;30(5):969–977. | ||
Liou TC, Shih SC, Kao CR, Chou SY, Lin SC, Wang HY. Pulmonary metastasis of hepatocellular carcinoma associated with transarterial chemoembolization. J Hepatol. 1995;23(5):563–568. | ||
Xiong ZP, Yang SR, Liang ZY, et al. Association between vascular endothelial growth factor and metastasis after transcatheter arterial chemoembolization in patients with hepatocellular carcinoma. Hepatobiliary Pancreat Dis Int. 2004;3(3):386–390. | ||
Ji RL, Xia SH, Di Y, Xu W. Mechanism and dose-effect of Ginkgolide B on severe acute pancreatitis of rats. World J Gastroenterol. 2011;17(17):2241–2247. | ||
Yu WG, Xu G, Ren GJ, et al. Preventive action of curcumin in experimental acute pancreatitis in mouse. Indian J Med Res. 2011;134(5):717–724. | ||
Meng MB, Cui YL, Guan YS, et al. Traditional Chinese medicine plus transcatheter arterial chemoembolization for unresectable hepatocellular carcinoma. J Altern Complement Med. 2008;14(8):1027–1042. | ||
Sturm JW, Keese M. Multimodal treatment of hepatocellular carcinoma (HCC). Onkologie. 2004;27(3):294–303. | ||
Kasugai H, Kojima J, Tatsuta M, et al. Treatment of hepatocellular carcinoma by transcatheter arterial embolization combined with intraarterial infusion of a mixture of cisplatin and ethiodized oil. Gastroenterology. 1989;97(4):965–971. | ||
Kagawa T, Koizumi J, Kojima S, et al. Transcatheter arterial chemoembolization plus radiofrequency ablation therapy for early stage hepatocellular carcinoma: comparison with surgical resection. Cancer. 2010;116(15):3638–3644. | ||
Jianyong L, Lunan Y, Wentao W, et al. Barcelona clinic liver cancer stage B hepatocellular carcinoma: transarterial chemoembolization or hepatic resection? Medicine (Baltimore). 2014;93(26):e180. | ||
Kamran AU, Liu Y, Li FE, Liu S, Wu JL, Zhang YW. Transcatheter arterial chemoembolization with gelatin sponge microparticles treated for BCLC stage B hepatocellular carcinoma: a single center retrospective study. Medicine (Baltimore). 2015;94(52):e2154. | ||
Chen Z, Chen HY, Lang QB, Yuan H. Preventive effects of jiedu granules combined with cinobufacini injection versus transcatheter arterial chemoembolization in post-surgical patients with hepatocellular carcinoma: a case-control trial. Chin J Integr Med. 2012;18(5):339–344. | ||
Wang Z, Zhang G, Wu J, Jia M. Adjuvant therapy for hepatocellular carcinoma: current situation and prospect. Drug Discov Ther. 2013;7(4):137–143. | ||
Cheung F, Wang X, Wang N, et al. Chinese medicines as an adjuvant therapy for unresectable hepatocellular carcinoma during transarterial chemoembolization: a meta-analysis of randomized controlled trials. Evid Based Complement Altern Med. 2013;2013:487919. | ||
Takayasu K, Arii S, Ikai I, et al. Prospective cohort study of transarterial chemoembolization for unresectable hepatocellular carcinoma in 8510 patients. Gastroenterology. 2006;131(2):461–469. | ||
Llovet JM, Burroughs A, Bruix J. Hepatocellular carcinoma. Lancet. 2003;362(9399):1907–1917. | ||
Mason MC, Massarweh NN, Salami A, Sultenfuss MA, Anaya DA. Post-embolization syndrome as an early predictor of overall survival after transarterial chemoembolization for hepatocellular carcinoma. HPB (Oxford). 2015;17(12):1137–1144. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.