Back to Journals » Infection and Drug Resistance » Volume 12
Characterization of antibiotic resistance and virulence factors of Escherichia coli strains isolated from Iranian inpatients with urinary tract infections
Authors Haghighatpanah M, Mojtahedi A
Received 17 June 2019
Accepted for publication 24 August 2019
Published 3 September 2019 Volume 2019:12 Pages 2747—2754
DOI https://doi.org/10.2147/IDR.S219696
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Suresh Antony
Maryam Haghighatpanah1, Ali Mojtahedi2
1Department of Microbiology, Islamic Azad University, Lahijan Branch, Guilan, Iran; 2Department of Microbiology, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran
Correspondence: Ali Mojtahedi
Department of Microbiology, School of Medicine, Guilan University Campus, 7 th Km of Rasht-Tehran Highway, Rasht, Guilan, Iran
Tel +98 133 369 0884
Fax +98 133 369 0036
Email [email protected]
Background: Urinary tract infections (UTIs) are one of the most frequent human infectious diseases causing considerable amount of morbidity and mortality. The present study aimed to investigate the occurrence of antibiotics resistance and virulence genes among Escherichia coli strains isolated from UTIs in the north of Iran.
Methods: This cross-sectional study was performed at 5 teaching hospitals in Rasht in the north of Iran. Totally, 129 E. coli isolates were identified by standard microbiologic tests. Antimicrobial susceptibility pattern was determined using disk diffusion method. The presence of virulence genes was detected by PCR method.
Results: The results of antibiotic susceptibility showed that the highest resistance rates were to ampicillin (78.3%) followed by nalidixic acid (74.4%) and trimethoprim/sulfamethoxazole (69.8%). On the other hand, the highest susceptibility was toward nitrofurantoin (96.1%) and imipenem (92.2%). Further analysis revealed that the rate of ESBL-producing and multiple-drug resistant isolates was 51.2% and 84.5%, respectively. Molecular analysis revealed that traaT (87.6%) gene was the most prevalent virulence factors followed by fyuA (86%) and kpsmt (76%) genes. Also, fimH gene was the most frequently detected adhesion-associated gene with 74.4%.
Conclusion: In summary, our results showed a remarkable rate of drug resistance and heterogeneity for virulence factors among E. coli strains isolated from UTIs in the north of Iran. The emergence of such strains can be a predictive marker for their persistence in the hospital and consequently a significant threat for hospitalized patients.
Keywords: urinary tract infections, Escherichia coli, antibiotics resistance, ESBL, virulence factors
Introduction
Urinary tract infections (UTIs) are one of the most frequently occurring infectious diseases in both hospital and community settings which cause considerable amount of morbidity and mortality.1 Although the UTIs caused by a wide array of pathogens, Escherichia coli is responsible for the majority of infections.2 UTIs nearly recognized to occur in all age groups, but some groups such as neonates, pregnant women or the elderly patients are more vulnerable.3,4
Acquisition of potential virulence markers by E. coli strains might increase their ability to resist and overcome the host immune defenses and subsequently a severe infection.5 These virulence factors are usually carried on the large number of pathogenicity-associated islands which can be easily disseminated by microorganisms through different horizontal gene transfer mechanisms.6 The characterization of virulence factors such as adhesions, toxins and iron uptake systems can be useful to improve our understanding the pathogenicity of symptomatic or complicated UTIs.7
On the other hand, the emergence of antimicrobial-resistant strains has become a serious public health concern and leading to increased mortality and morbidity.8 Excessive and inappropriate use of antibiotics is the main factor for the increasing rate of multiple-drug resistant (MDR) strains which are commonly related to the increasing trend of extended-spectrum beta-lactamase (ESBL)-producing bacteria.8,9 The recent emergence of multi-resistant extraintestinal pathogenic Escherichia coli (ExPEC) strains linked to increasing prevalence of ESBLs in both hospital and community settings. E. coli sequence type 131 is an international high-risk clone, which well known for high ability of horizontal gene transfer that could confer resistance to most of the critically important antimicrobial classes, including fluoroquinolones and third- and fourth-generation cephalosporins.
Due to diversity of virulence patterns among E. coli strains causing UTIs and also the limited therapeutic options for management of infections caused by MDR strains,5 the knowledge about their pathogenicity and antibiotic resistance trends and is a rational way to overcome the risk of treatment failure. Therefore, the present study aimed to investigate the occurrence of antibiotics resistance and virulence genes among E. coli strains isolated from UTIs in the north of Iran.
Materials and methods
Study population and bacterial isolates
This cross-sectional study was performed at five teaching and remedial hospitals in Rasht in the north of Iran. The study design was in accordance with the declaration of Helsinki and approved by the institutional ethics committee of Guilan University of Medical Sciences (Approval No. IR.SUMS. REC.1395.S747). However, because only leftovers from clinical specimens were used, the local ethics committee waived the need for informed consent. Midstream voided urine specimens were collected using the clean-catch method in sterile disposable tube for adult, sterile urine bags for children and catheter or suprapubic needle aspiration for neonates and analyzed immediately in the laboratory. After microscopic examination, urine samples were cultured on 5% blood agar and MacConkey agar using standard quantitative 10 μL loops and incubated aerobically for 24 hrs at 37°C. UTI is defined as the presence of single organism in the urine in quantities of 103–105 colony forming unit (CFU) per milliliter (cfu/mL). The mixed growth of bacteria was considered as contamination. A total of 129 non-duplicate E. coli isolates were isolated from clean-catch midstream urine of studied subjects. The bacteria were identified and confirmed using standard microbiologic biochemical tests including Gram staining, cultivation, and reactions on MacConkey agar, triple sugar iron agar, SIM medium, Simmons’ citrate agar, MR-VP medium.
Antimicrobial susceptibility testing
Antibiotic susceptibility of all isolates to ampicillin, amoxicillin-clavulanate, cefoxitin, cefixime, ceftazidime, ceftriaxone, cefotaxime, cefepime, ciprofloxacin, ofloxacin, nalidixic acid, aztreonam, tetracycline, gentamicin, trimethoprim/sulfamethoxazole, nitrofurantoin, and imipenem (Mast Co., UK) was carried out on Muller-Hinton agar (Oxoid Co., UK) using the disk diffusion method as recommended by the Clinical and Laboratory Standards Institute (CLSI).10 E. coli ATCC 25,922 was used as the quality control strain for antibacterial susceptibility testing. The isolates non-susceptible to ≥1 agent at least three of antibiotic categories were defined as MDR.11
Phenotypic detection of ESBL
All isolates were tested for ESBL production by double-disk synergy test using ceftazidime (30 µg) and cefotaxime (30 µg) disks, and combination with clavulanic acid (10 µg) disk as described by CLSI procedure. According to the CLSI guidelines, an increase of ≥5 mm in the diameter of the inhibition zones around the combination disk as compared to the inhibition zones around the single antibiotic disk indicated as ESBL producers.10 E. coli ATCC 25922 and Klebsiella pneumoniae ATCC 700603 were used as negative and positive control strains, respectively.
DNA extraction and virulence genotyping
Genomic DNA was extracted from all E. coli isolates using High Pure DNA Template preparation kit (Roshe, Germany) according to the manufacturer’s instructions. The targeted genes and nucleotide sequences of the oligonucleotide primers used in this study were chosen as previously described (Table 1).12–14 PCR amplification for detection of virulence genes was carried out on a Veriti 96-well thermal cycler instrument (Applied Biosystems at Life Technologies, Foster City, CA, USA). The PCR program consisted of an initial denaturation step at 95°C for 5 mins, followed by 30 cycles of DNA denaturation at 95°C for 30 s, primer annealing for 30 s. Temperature was depending on the sequences of primers, and primer extension at 72°C for 1 min, followed by a final extension at 72°C for 7 mins. The amplifications were separated on 1.5% agarose gel prepared in 1X Tris/Boric acid/EDTA (TBE) buffer and visualized using ultraviolet light after staining with safe stain dye (CinnaGen Co., Iran).
Data analysis
The analysis of results was performed by using SPSS™ software, version 21.0 (IBM Corp., Armonk, NY, USA). The results are presented as descriptive statistics in terms of relative frequency. The Chi-square (χ2) or Fisher’s exact tests was performed to analyze significant differences. A P-<0.05 was considered to be significant.
Results
Of 129 E. coli isolates included in our study, 90 (69.8%) and 39 (30.2%) were isolated from femaleand male patients, respectively. The mean age ± SD of the patients was 50.1±27.7 years, ranging from 1 to 90 years old. Also, 17.8% of patients were aged 1–18 years, 37.2% aged 19–60 years, and 45% aged more than 60 years old.
The results of antibiotic susceptibility showed that the highest resistance rate was against ampicillin (78.3%) followed by nalidixic acid (74.4%) and trimethoprim/sulfamethoxazole (69.8%). On the other hand, the highest susceptibility was toward nitrofurantoin (96.1%) followed by imipenem (92.2%) and cefoxitin (74.4%). Further analysis revealed that the rate of ESBL-producing isolates was 51.2% (66/129). Moreover, there was a significant correlation between ESBL-producing isolates and their antibiotic resistance to all of the antibiotics, except for nitrofurantoin and imipenem. The full results of antibiotic resistance patterns of isolates are presented in Table 2. Also, the frequency of MDR isolates was estimated at 84.5%. The rate of MDR isolates was significantly higher among ESBLs-producers than non-ESBL producers (100% vs 68.3%, P<0.001).
 |
Table 1 The sequences of used primers |
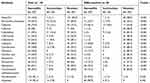 |
Table 2 Distribution of antibiotic resistance pattern according to ESBL production |
Molecular analysis revealed that the traaT (87.6%) was the most prevalent virulence factors followed by fyuA (86%) and kpsmt (76%) genes. Also, fimH gene was the most frequently detected adhesion-associated gene with 74.4%. The full results of the investigated virulence factors distribution in E. coli isolates are presented in Table 3. According to the results, the frequency of 9 genes (fyuA, papC, papG II, fimH, kpsMT, traT, iroN, usp and afa/draBC) was more than 50% among the isolates. In addition, the frequency of bmaE gene was significantly higher among the ESBLs-producing isolates compared to non-ESBL-producing isolates (P<0.001).
 |
Table 3 Distribution of virulence factors according to ESBL production |
Analyzing drug-resistance and gene patterns showed a high heterogeneity among isolates (Table S1). The most prevalent drug-resistance pattern was AZT-GEN-SXT-TET-CIP-OFX-NAL-CAZ-CRO-FEP-CFM-CTX-FOX-CEP-AUG-AMP with 8.5%, while none of the gene pattern exceeded 2%.
Discussion
Characterization of the drug resistance and virulence determinants of E. coli strains, particularly in hospitalized patients allows the physicians to reduce the risk of complications and also optimizing available infection control policies.5 Here, we report the prevalence of antibiotic resistance and virulence factors of ESBL-producing E. coli isolates causing UTIs in the north of Iran.
UTIs are generally treated empirically by physicians, therefore aware of the local epidemiological data for an efficient therapy is necessary and decrease the further uncomfortable outcome.1 In our results, the majority of isolates were resistant to most of tested antibiotics and 84.5% of isolates were also MDR. Although our estimate of MDR isolates were higher than the pooled prevalence of MDR uropathogenic E. coli (UPEC) with 49.4% in Iran, it was also showed that the relative frequency of MDR isolates is varied from 10.5% to 79.2% in different regions.9 Moreover, comparing to others, it seems that Asian and African countries experiencing the highest rates of MDR-UPEC while North America and Europe have the lowest rates. The high rate of resistance to these antibiotics may be because of the inappropriate and overuse of antibiotics in the last decade.15 The majority of our isolates were susceptible to nitrofurantoin (96.1%) and imipenem (92.2%), which was closest with reports from Iran and other countries.5,16–19 However, carbapenems remain as the last-line treatment option against infections caused by drug-resistant strains, since numerous side effects of nitrofurantoin limited its application.5 As a consequence of increased prescription of fluoroquinolones, resistance to these antibiotics in uropathogens has been increasing globally.20 Regarding this phenomenon, the majority of our isolates similar to recent fluoroquinolones resistance reports from central part (61.3%),21 and south (55.6%) of Iran,5 were resistant to fluoroquinolones including ciprofloxacin (53.5%) and ofloxacin (50.4%).
In our results, a remarkable proportion of E. coli isolates was ESBL producers (51.2%), but this rate is consistent with the median values reported from Iran varied form 24% to 72.9% among UPEC.22 These findings indicate to a great discrepancy in the prevalence of ESBL producers which is mainly due to differences in geographical regions, infection control policy, and sample source. ESBLs are a group of plasmid-mediated beta-lactamases with inactivation capability of beta-lactams and no detectable activity against cephamycins and carbapenems.22 Concerning this, the rates of antibiotic resistance among our ESBL producers were significantly higher than non-ESBL producers. Hopefully, based on our results, nitrofurantoin and imipenem still have a promising activity against ESBL-producing isolates of E. coli.
Adhesins associated genes are the most frequently found virulence factors in E. coli strains isolated from UTIs.7 The prevalence of adhesins among UTIs derived E. coli can be greatly heterogeneous; however, it is suggested that type 1 and P fimbriae are the most common type/s.5 In our results, fimH gene encoding of the type 1fimbriae was found in 74.4% of isolates as the most prevalent adhesion. This finding was in agreement with the most previous studies in this field form Iran and other countries.5,16,17,23–25 Moreover, 71.3% of our isolates had papG II which is responsible for encoding PapG adhesion on the tips of P fimbriae. In previous studies, it has been shown that different classes of PapG adhesion are predominant in those E. coli strains isolated from UTIs,5,17,26 which support the results of the present study.
Scarcity of iron in the human urinary tract leading to up-regulation of different iron-transport systems such as aerobactin and yersiniabactin in uropathogens.27 In our results, fyuA gene encoding yersiniabactin receptor with 86% was found as the most frequent iron chelator factor. Previously, consistent with our results, it was suggested that the presence of fyuA as one of the best predictor of UPEC predicts more efficient colonization of E. coli isolates in the bladder.25,28–30
Among the different tested toxins of E. coli in our survey, usp genes which designated for an uropathogenic specific protein was found in 68.2% of isolates, more than other toxins (cnf1, hlyA and ibeA). Previously, several authors showed that usp may contribute to the causation of UTIs and may be considered as a major virulence determinant of UPEC.31–34
Finally, among protective virulence factors, traT which encoding an anti-complementary protein and kpsMT II encoding polysaccharide capsule were found in 87.6% and 76% of isolates, respectively. Previously, in two Iranian studies, the prevalence of kpsMT II in UPEC isolates was reported 9% and 4.1%, respectively.35,36 In Germany, Toval et al reported the prevalence of traT in 67.9% and kpsMT II in 39.3% of UPEC isolates.37 In another study from Brazil, the prevalence of traT in UPEC isolates was estimated at 76%.38 This observation indicating heterogeneity in the distribution of virulence genes in UPEC strains in different regions.
As the main limitations of the present study, the lack of data on community or hospital origin of UTI, and genes expression assay should be acknowledged.
In summary, our results showed a remarkable rate of drug resistance and heterogeneity for virulence factors among E. coli strains isolated from UTIs in the north of Iran. The emergence of such strains can be a predictive marker for their persistence in the hospital and consequently a significant threat for hospitalized patients. These findings provide experimental evidences for the prescription of more effective therapy based on antibiogram and optimizing infection control policies.
Author contributions
Both authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol. 2015;13(5):269–284. doi:10.1038/nrmicro3432
2. Malekzadegan Y, Rastegar E, Moradi M, Heidari H, Sedigh Ebrahim-Saraie H. Prevalence of quinolone-resistant uropathogenic Escherichia coli in a tertiary care hospital in south Iran. Infect Drug Resist. 2019;12:1683–1689. doi:10.2147/IDR.S206966
3. Lim VH, Whitehurst T, Usoro E, Ming NS. Management of urinary tract infections in elderly patients: strategies for improvement. BMJ Qual Improv Rep. 2014;3(1). doi:10.1136/bmjquality.u203314.w1503
4. Arshad M, Seed PC. Urinary tract infections in the infant. Clin Perinatol. 2015;42(1):17–28, vii. doi:10.1016/j.clp.2014.10.003
5. Malekzadegan Y, Khashei R, Sedigh Ebrahim-Saraie H, Jahanabadi Z. Distribution of virulence genes and their association with antimicrobial resistance among uropathogenic Escherichia coli isolates from Iranian patients. BMC Infect Dis. 2018;18(1):572. doi:10.1186/s12879-018-3109-6
6. Bliven KA, Maurelli AT. Evolution of bacterial pathogens within the human host. Microbiol Spectr. 2016;4(1).
7. Firoozeh F, Saffari M, Neamati F, Zibaei M. Detection of virulence genes in Escherichia coli isolated from patients with cystitis and pyelonephritis. Int J Infect Dis. 2014;29:219–222. doi:10.1016/j.ijid.2014.03.1393
8. Shaikh S, Fatima J, Shakil S, Rizvi SM, Kamal MA. Antibiotic resistance and extended spectrum beta-lactamases: types, epidemiology and treatment. Saudi J Biol Sci. 2015;22(1):90–101. doi:10.1016/j.sjbs.2014.08.002
9. Hadifar S, Moghoofei M, Nematollahi S, et al. Epidemiology of multidrug resistant uropathogenic Escherichia coli in Iran: a systematic review and meta-analysis. Jpn J Infect Dis. 2017;70(1):19–25. doi:10.7883/yoken.JJID.2015.652
10. CLSI. Performance Standards for Antimicrobial Susceptibility Testing; 28th Informational Supplement. CLSI Document M100. Wayne, PA: Clinical and Laboratory Standards Institute; 2018.
11. Magiorakos AP, Srinivasan A, Carey RB, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–281. doi:10.1111/j.1469-0691.2011.03570.x
12. Johnson JR, Stell AL. Extended virulence genotypes of Escherichia coli strains from patients with urosepsis in relation to phylogeny and host compromise. J Infect Dis. 2000;181(1):261–272. doi:10.1086/315217
13. Rodriguez-Siek KE, Giddings CW, Doetkott C, Johnson TJ, Fakhr MK, Nolan LK. Comparison of Escherichia coli isolates implicated in human urinary tract infection and avian colibacillosis. Microbiology. 2005;151(Pt 6):2097–2110. doi:10.1099/mic.0.27499-0
14. Bauer RJ, Zhang L, Foxman B, et al. Molecular epidemiology of 3 putative virulence genes for Escherichia coli urinary tract infection-usp, iha, and iroN (E. coli). J Infect Dis. 2002;185(10):1521–1524. doi:10.1086/340206
15. Ventola CL. The antibiotic resistance crisis: part 1: causes and threats. P T. 2015;40(4):277–283.
16. Lee JH, Subhadra B, Son YJ, et al. Phylogenetic group distributions, virulence factors and antimicrobial resistance properties of uropathogenic Escherichia coli strains isolated from patients with urinary tract infections in South Korea. Lett Appl Microbiol. 2016;62(1):84–90. doi:10.1111/lam.12517
17. Qin X, Hu F, Wu S, et al. Comparison of adhesin genes and antimicrobial susceptibilities between uropathogenic and intestinal commensal Escherichia coli strains. PLoS One. 2013;8(4):e61169. doi:10.1371/journal.pone.0061169
18. Tabasi M, Asadi Karam MR, Habibi M, Yekaninejad MS, Bouzari S. Phenotypic assays to determine virulence factors of Uropathogenic Escherichia coli (UPEC) isolates and their correlation with antibiotic resistance pattern. Osong Public Health Res Perspect. 2015;6(4):261–268. doi:10.1016/j.phrp.2015.08.002
19. Lavigne JP, Bruyere F, Bernard L, et al. Resistance and virulence potential of uropathogenic Escherichia coli strains isolated from patients hospitalized in urology departments: a French prospective multicentre study. J Med Microbiol. 2016;65(6):530–537. doi:10.1099/jmm.0.000247
20. Fasugba O, Gardner A, Mitchell BG, Mnatzaganian G. Ciprofloxacin resistance in community- and hospital-acquired Escherichia coli urinary tract infections: a systematic review and meta-analysis of observational studies. BMC Infect Dis. 2015;15:545. doi:10.1186/s12879-015-1282-4
21. Neamati F, Firoozeh F, Saffari M, Zibaei M. Virulence genes and antimicrobial resistance pattern in uropathogenic Escherichia coli isolated from hospitalized patients in Kashan, Iran. Jundishapur J Microbiol. 2015;8(2):e17514. doi:10.5812/jjm
22. Ebrahim-Saraie HS, Nezhad NZ, Heidari H, Motamedifar A, Motamedifar M. Detection of antimicrobial susceptibility and integrons among extended-spectrum beta-lactamase producing uropathogenic Escherichia coli isolates in Southwestern Iran. Oman Med J. 2018;33(3):218–223. doi:10.5001/omj.2018.40
23. Gao Q, Zhang D, Ye Z, et al. Virulence traits and pathogenicity of uropathogenic Escherichia coliisolates with common and uncommon O serotypes. Microb Pathog. 2017;104:217–224. doi:10.1016/j.micpath.2017.01.027
24. Rahdar M, Rashki A, Miri HR, Rashki Ghalehnoo M. Detection of pap, sfa, afa, foc, and fim adhesin-encoding operons in uropathogenic Escherichia coli isolates collected from patients with urinary tract infection. Jundishapur J Microbiol. 2015;8(8):e22647. doi:10.5812/jjm
25. Johnson JR, Porter S, Johnston B, et al. Host characteristics and bacterial traits predict experimental virulence for Escherichia coli bloodstream isolates from patients with urosepsis. Open Forum Infect Dis. 2015;2(3):ofv083. doi:10.1093/ofid/ofv083
26. Johnson JR, Owens K, Gajewski A, Kuskowski MA. Bacterial characteristics in relation to clinical source of Escherichia coli isolates from women with acute cystitis or pyelonephritis and uninfected women. J Clin Microbiol. 2005;43(12):6064–6072. doi:10.1128/JCM.43.12.6064-6072.2005
27. Subashchandrabose S, Mobley HLT. Virulence and fitness determinants of uropathogenic Escherichia coli. Microbiol Spectr. 2015;3(4). doi:10.1128/microbiolspec.UTI-0015-2012
28. Spurbeck RR, Dinh PC
29. Johnson JR, Johnston BD, Porter S, Thuras P, Aziz M, Price LB. Accessory traits and phylogenetic background predict Escherichia coli extraintestinal virulence better than does ecological source. J Infect Dis. 2019;219(1):121–132. doi:10.1093/infdis/jiy459
30. Yun KW, Kim HY, Park HK, Kim W, Lim IS. Virulence factors of uropathogenic Escherichia coli of urinary tract infections and asymptomatic bacteriuria in children. J Microbiol Immunol Infect. 2014;47(6):455–461. doi:10.1016/j.jmii.2013.07.010
31. Kanamaru S, Kurazono H, Ishitoya S, et al. Distribution and genetic association of putative uropathogenic virulence factors iroN, iha, kpsMT, ompT and usp in Escherichia coli isolated from urinary tract infections in Japan. J Urol. 2003;170(6 Pt 1):2490–2493. doi:10.1097/01.ju.0000094185.48467.dc
32. Park HK, Jung YJ, Chae HC, et al. Comparison of Escherichia coli uropathogenic genes (kps, usp and ireA) and enteroaggregative genes (aggR and aap) via multiplex polymerase chain reaction from suprapubic urine specimens of young children with fever. Scand J Urol Nephrol. 2009;43(1):51–57. doi:10.1080/00365590802299338
33. Mao BH, Chang YF, Scaria J, et al. Identification of Escherichia coli genes associated with urinary tract infections. J Clin Microbiol. 2012;50(2):449–456. doi:10.1128/JCM.00640-11
34. Rijavec M, Muller-Premru M, Zakotnik B, Zgur-Bertok D. Virulence factors and biofilm production among Escherichia coli strains causing bacteraemia of urinary tract origin. J Med Microbiol. 2008;57(Pt 11):1329–1334. doi:10.1099/jmm.0.2008/002543-0
35. Mashayekhi F, Moghny M, Faramarzpoor M, et al. Molecular characterization and antimicrobial resistance of uropathogenic Escherichia coli. Iran J Biotechnol. 2014;12(2):32–40.
36. Momtaz H, Karimian A, Madani M, et al. Uropathogenic Escherichia coli in Iran: serogroup distributions, virulence factors and antimicrobial resistance properties. Ann Clin Microbiol Antimicrob. 2013;12:8. doi:10.1186/1476-0711-12-8
37. Toval F, Kohler CD, Vogel U, et al. Characterization of Escherichia coli isolates from hospital inpatients or outpatients with urinary tract infection. J Clin Microbiol. 2014;52(2):407–418. doi:10.1128/JCM.02069-13
38. Oliveira FA, Paludo KS, Arend LN, et al. Virulence characteristics and antimicrobial susceptibility of uropathogenic Escherichia coli strains. Genet Mol Res. 2011;10(4):4114–4125. doi:10.4238/2011.October.31.5
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
