Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 12
Characteristics of COPD patients initiating treatment with aclidinium or tiotropium in primary care in Catalonia: a population-based study
Authors Monteagudo M , Roset M, Rodriguez-Blanco T, Muñoz L, Miravitlles M
Received 23 December 2016
Accepted for publication 9 March 2017
Published 12 April 2017 Volume 2017:12 Pages 1145—1152
DOI https://doi.org/10.2147/COPD.S131016
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Mònica Monteagudo,1,2 Montse Roset,3 Teresa Rodriguez-Blanco,1,2 Laura Muñoz,4 Marc Miravitlles5
1Primary Care University Research Institute Jordi Gol (IDIAP Jordi Gol), Barcelona, Spain; 2Universitat Autònoma de Barcelona, Bellaterra (Cerdanyola del Vallès), Spain; 3IMS Health, Barcelona, Spain; 4Agència de Qualitat i Avaluació Sanitàries de Catalunya (AQuAS), Barcelona, Spain; 5Pneumology Department, Hospital Universitari Vall d’Hebron, CIBER de Enfermedades Respiratorias (CIBERES), Barcelona, Spain
Objective: To describe and compare demographic and clinical profile of patients newly initiated on aclidinium (ACL) or tiotropium (TIO) and identify factors associated with newly initiated ACL in real-life clinical practice during 2013 in Catalonia.
Design: We performed a population-based, retrospective, observational study with data obtained from the Information System for Research Development in Primary Care, a population database that contains information of 5.8 million inhabitants (more than 80% of the Catalan population). Patients over 40 years old, with a recorded diagnosis of COPD and newly initiated treatment with either ACL or TIO during the study period (January to December 2013), were selected. A descriptive analysis of demographic and clinical characteristics was performed, and treatment adherence was also assessed for both cohorts.
Results: A total of 8,863 individuals were identified, 4,293 initiated with ACL and 4,570 with TIO. They had a mean age of 69.4 years (standard deviation: 11.3), a median COPD duration of 3 years (interquartile range: 0–8), and 71% were males. Patients treated with ACL were older, with more respiratory comorbidities, a longer time since COPD diagnosis, worse forced expiratory volume in 1 second (% predicted), and with a higher rate of exacerbations during the previous year compared with TIO. It was found that 41.3% of patients with ACL and 62.3% of patients with TIO had no previous COPD treatment. Inhaled corticosteroid and long-acting β2-agonist were the most frequent concomitant medications (32.9% and 32.6%, respectively). Approximately 75% of patients were persistent with ACL or TIO at 3 months from the beginning of treatment, and more than 50% of patients remained persistent at 9 months.
Conclusion: Patients initiated with ACL had more severe COPD and were taking more concomitant respiratory medications than patients initiated with TIO. ACL was more frequently initiated as part of triple therapy, while TIO was more frequently initiated as monotherapy.
Keywords: COPD, treatment, primary care, adherence
Introduction
Pharmacologic therapy for COPD aims to reduce and control symptoms, reduce the frequency and severity of exacerbations, and improve health status and exercise tolerance.1 Long-acting bronchodilators are the basis of COPD maintenance therapy,1,2 and among them, long-acting antimuscarinic agents (LAMAs) have demonstrated superior efficacy in prevention of exacerbations than long-acting β2-agonists (LABAs),3,4 and therefore, most guidelines recommend LAMAs as initial therapy for management of COPD.1,2
Tiotropium (TIO) was the first once-daily LAMA available, and lately aclidinium (ACL) is a twice-daily LAMA available for maintenance treatment to relieve symptoms in COPD.5 ACL demonstrated similar efficacy and safety compared with TIO for the treatment of stable COPD,6,7 with the twice-daily administration of ACL providing better lung function in the second 12 hours of the day.6 Some studies have suggested that this second administration of the bronchodilator in the evening would result in better symptom control, even in patients with low levels of symptoms.7,8 It is not clear whether these differences are perceived by patients and prescribers in real life and may result in different patterns of prescription.
The diagnosis and management of COPD in Spain is mostly made in primary care, and drug prescriptions for chronic diseases are only managed by primary care physicians. Therefore, the availability of large population-based administrative databases from primary care records allows the evaluation of characteristics of patients receiving different therapies in an unbiased way. This is especially important when new treatments for specific conditions are available. With the administrative health care database of primary care in Catalonia (Spain), we have developed the current study with the objective to describe and compare the baseline characteristics of patients with COPD newly initiated either on TIO or ACL during 2013, 1 year after the launch of ACL in Spain, and identify factors associated with ACL prescription.
Methods
This was a population-based, retrospective, observational study aimed at describing baseline sociodemographic and clinical characteristics of COPD patients who started treatment with ACL or TIO during the study period (from January 1 to December 31, 2013). The index date was defined as the ACL or TIO initiation date and defined the start of the data collection period for each patient. Secondary evaluation included compliance to LAMAs during 1 year after the index date. The data were obtained from the Information System for the Development of Research in Primary Care (SIDIAP) database, which contains anonymized computerized primary care medical records from 5.8 million people in Catalonia, which represents more than 80% of the total population.9 This database has been used and validated for epidemiological research in respiratory diseases including COPD.10
The inclusion criteria in the study were as follows: 1) initiation of treatment with either ACL or TIO during the study period; 2) a recorded diagnosis of COPD in the medical records; 3) age of ≥40 years; and 4) at least 3 months of follow-up after initiation of either treatment (extended COPD population).
A subpopulation analysis including a more restrictive definition of inclusion criteria was performed in order to validate the COPD diagnosis reported in the database (restrictive population). This analysis included patients who had a recorded diagnosis of COPD in the medical records as well as 1) spirometry-confirmed airflow limitation (forced expiratory volume in 1 second [FEV1]/forced vital capacity <0.7) at the time of diagnosis, or 2) were prescribed respiratory medication (Anatomical Therapeutic Chemical [ATC] code: R03) after diagnosis (restrictive COPD population).
The following variables were obtained at baseline: demographic and clinical characteristics, including age, sex, smoking history, and comorbidities. Diagnostic spirometry, exacerbations, and use of vaccines during the year before inclusion in the study and recorded in the database were also collected. Finally, concomitant treatment and type of prescription of the LAMA was assessed at the index date. Exacerbations were identified by diagnostic codes and by treatment when patients received antibiotics and/or oral corticosteroids in the absence of other codified infectious events such as tonsillitis or urinary infection.
Compliance was assessed in terms of persistence and in terms of adherence based on pharmacy records available until December 31, 2014, corresponding to a maximum of 1 year after the index date. Theoretical medication use was calculated using information on dispensing date, total supply, and dosage regimen. Persistence was analyzed in terms of percentage of patients refilling prescriptions of LAMAs at 3, 6, 9, and 12 months since index date. Adherence was analyzed in terms of medication possession ratio (MPR), defined as the number of doses dispensed in relation to the dispensing period. An MPR between 80% and 120% was used to define treatment-adherent patients.
This study was approved by the Ethics and Clinical Research Committee of the Jordi Gol Primary Care University Research Institute (Barcelona, Spain).
Statistical analysis
A descriptive analysis for both study populations (extended COPD population and restrictive population) was performed to describe baseline sociodemographic and clinical characteristics of patients newly initiated on ACL or on TIO. For qualitative variables, absolute frequencies and corresponding percentages were calculated. Quantitative variable following a normal distribution were described by mean and standard deviation, while those that did not follow a normal distribution were describing using the median. We used independent t-tests for continuous data and χ2 tests for categorical data as appropriate for unadjusted comparisons between groups.
Logistic regression model was performed to assess factors independently associated with newly initiated ACL versus TIO. Variables initially considered were: age, sex, time since COPD diagnosis, respiratory comorbidities, smoking history, concomitant COPD treatment, visits to primary care physician, visits to pulmonologist, exacerbations, and spirometry.
All statistical tests were two-sided at the 5% significance level. Analyses were performed using Stata/SE version 14.2 for Windows (Stata Corp. LP, College Station, TX, USA).
Results
A total of 105,727 subjects with recorded diagnosis of COPD were identified in the database during the reference year. Of them, 14,062 (13.3%) were identified as initiating treatment with either ACL or TIO in 2013. Of these patients, 8,863 COPD patients fulfilled the inclusion criteria, 4,293 initiated a treatment with ACL and 4,570 with TIO (Figure 1). Most patients had recommended dose prescribed of LAMA according to the summary of product characteristics (SmPC) (88.6% in patients with ACL and 88.9% with TIO).
  | Figure 1 Selection of the samples of patients included in the study. |
In the extended COPD population, 71% were males, with a mean age of 69.4 years (standard deviation [SD]: 11.3), and a median duration of COPD of 3 years (interquartile range: 0–8). Most patients had smoking history (69.7%), and 40.3% were obese (body mass index ≥30). The most frequent respiratory comorbidities were asthma (14.4%), bronchiectasis (6.6%), and sleep apnea (5.2%). The most common nonrespiratory comorbidities were hypertension (57.3%), diabetes mellitus (24.4%), metabolic syndrome (21.3%), and anxiety or depression (15.1%).
A low percentage of spirometry in the previous year (21.0%), with a mean FEV1 (% predicted) of 62.1% (SD: 20.3%) and a high percentage of patients with previous exacerbations (57.4%) were observed.
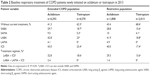
Patients treated with ACL were older, with more respiratory comorbidities, a longer time since COPD diagnosis, worse FEV1 (% predicted), and a higher frequency of patients who suffered from an exacerbation the previous year compared with TIO (Table 1).
In the more restrictive population, there were more males, few never smokers, a higher frequency of spirometry in the previous year with worse FEV1 (%) values, and a higher rate of exacerbations in the previous year compared with the extended COPD population. The differences previously observed between the groups initiated with ACL or TIO persisted in this restrictive population (Table 1).
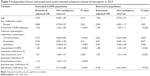
At the index date, 41.3% of patients newly initiated with ACL and 62.3% of patients newly initiated with TIO had no previous COPD treatment. The remaining patients were receiving concomitant COPD treatments. In general, use of concomitant treatments was higher in patients treated with ACL than in patients treated with TIO. Inhaled corticosteroids (ICS) and LABA were the most frequent concomitant medications (32.9% and 32.6%, respectively). All of these baseline characteristics were similar in the restrictive population (Table 2).
Factors significantly associated with newly initiated ACL were male sex, a longer time since the COPD diagnosis, being a current smoker, receiving more concomitant COPD treatments, having an exacerbation in the previous year, and a low percentage of spirometry in the previous year (Table 3).
  | Table 3 Independent factors associated with newly initiated aclidinium instead of tiotropium in 2013 |
We observed a high persistence to the treatment for both LAMAs. Approximately 75% of patients were persistent at 3 months from the beginning of LAMA treatment, and, although this percentage decreased gradually over time, at 9 months more than 50% of patients remained persistent users (Figure 2).
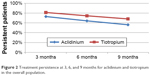  | Figure 2 Treatment persistence at 3, 6, and 9 months for aclidinium and tiotropium in the overall population. |
The proportion of patient with an adequate MPR was also high, with a mean (SD) of MPR of 0.74 (0.35), and a median of 0.83. Using the definition of adherent patients taking into account an 80%≤ MPR ≥120%, 46.4% of patients treated with ACL and 54% of those treated with TIO were classified as treatment adherent (Table 3). The proportion of patients with an adequate adherence between the groups initiated with ACL or TIO in this restricted population was similar to extended COPD population (Table 4).
Discussion
Our study provides a description of the demographic and clinical profile of patients who initiated treatment with LAMAs in real-life clinical practice. The characteristics of patients corresponded to the usual profile of COPD patients who attended primary care in Southern European countries, almost two-thirds were male and mean age was 70 years.11–13 When LAMA was initiated, approximately one-third of patients were already on a LABA/ICS combination, and therefore they were stepped up to triple therapy. Patients newly initiated on treatment with ACL had, in general, more severe COPD than patients newly initiated with TIO. Overall, adherence to treatment with LAMAs was high, especially in the first months of treatment, but decreased to ~50% after 9 months.
Long-acting bronchodilators are the basis of COPD maintenance therapy, among them the LAMAs have demonstrated similar bronchodilator efficacy as LABAs but with superior efficacy in prevention of exacerbations.3,4 Therefore, the recent GOLD strategy recommends LAMAs as initial therapy in virtually all categories of patients from A to D.1 This recommendation is also included in most national guidelines of management of COPD,2 including the Spanish guidelines.14
The first LAMA developed for treatment of COPD was TIO, a once-daily LAMA that demonstrated a significant and persistent bronchodilator effect15 and a significant reduction in the risk of exacerbations.16 More recently, additional LAMAs have been introduced in the armamentarium for the long-term treatment of patients with COPD. Among them, ACL is a twice-daily LAMA, the efficacy and safety of which have been investigated in several studies demonstrating a significant improvement in lung function, health status, and early morning, daytime, and nighttime symptoms in COPD patients.5–7 In comparative clinical trials, treatment with ACL was demonstrated to provide a higher area under the curve (AUC) for FEV1 during the second 12 hours of the day compared to TIO, as a result of the administration of the evening dose.6,7 This improvement in lung function resulted in a better control of symptoms compared with once-daily TIO.7 Although guidelines do not differentiate between different molecules in their recommendation for a LAMA, the different profiles of ACL and TIO may influence the perception of prescribers; therefore, we investigated the demographic and clinical profile of patients newly initiated with these two LAMAs over a period of 1 year. TIO was launched in Spain in 2002 and ACL was launched in 2013, thus during the period of the study they were the only two LAMAs available.
Our results showed that patients who initiated treatment with ACL had a more severe disease compared with patients with TIO. This increased severity was demonstrated by an older age, longer duration of COPD, higher frequency of comorbidities, worse lung function, and more frequent exacerbations in the previous year, among other variables. Furthermore, patients initiated with ACL were more frequently stepped up from previous treatments compared with patients initiated with TIO. Approximately 40% of patients initiating ACL were already on LABA/ICS compared with 23% of patients initiated with TIO. This means that the most frequent indication for ACL was the initiation of triple therapy; but in contrast, up to 62% of patients initiated TIO as monotherapy. This suggests that primary care physicians selected ACL for the more severe patients who were uncontrolled with their usual medication, but prescribed more often TIO in treatment-naïve patients as monotherapy. This observation may be related to the more recent launch of ACL, because newly available drugs tend to be used in more severe patients and those not responding to existing therapies. Moreover, it can be related to the effect of ACL on improvement and control of symptoms.8 Another factor would be that the LABA/ICS combinations available during the period of the study were twice daily, and therefore adding a twice-daily LAMA would be a reasonable option for patients in need of triple therapy.
The introduction of new drugs in more severe patients is illustrated by a French study analyzing the impact of the introduction of TIO in 2006. Similar to our results, the authors found that in 32.5% of cases, the new LAMA was added to LABA/ICS as triple therapy and very infrequently used as monotherapy.17 Also in the UK, the most frequent pathway to triple therapy was the addition of a LAMA to the existing treatment with a LABA/ICS.18 In the same study, the authors observed that 25% of patients initiating therapy for COPD were on triple therapy within 1 year, and the main driver for initiating this therapy was the history of exacerbations.18
Interestingly, only 20% of the study population had a spirometry performed in the previous year, and due to the characteristics of the study it is not possible to know where these spirometries were performed. This low use of spirometry in primary care has been recognized in Spain10,12,13,19 and in other countries.20–22 This indicates that primary care physicians rely on other factors in order to make decisions about treatment. De Miguel et al12 in a large cohort of patients in primary care identified increasing dyspnea and impairment in quality of life as the main drivers for increasing therapy in COPD. In addition, Brusselle et al18 observed that history of exacerbations was the main factor associated with the prescription of triple therapy. All these studies suggest that lung function is not the main factor driving changes in COPD treatment in primary care. In agreement with this reality, the GOLD strategy recommends different treatment options based on history of exacerbations and intensity of symptoms,1 and a new algorithm of pharmacologic treatment has been proposed based on the degree of dyspnea and the frequency and phenotype or exacerbations.23
The administration of bronchodilator treatment twice daily has been associated with a better control of symptoms over the whole day.7,8,24 A recent observational study in Spain showed that 52% of patients experienced respiratory symptoms throughout the day in spite of 62% being treated with triple therapy, and more symptomatic patients had poorer quality of life and more frequent anxiety and depression.25 The high prevalence of symptoms may partly explain the increase in the prescription of twice-daily ACL in more severe patients compared with TIO.
Adherence to treatment and the correct use of the inhaler device are essential for therapeutic success. In general, adherence to inhaled medication in COPD is poor.20 In our study, persistence with LAMAs was initially high and decreased progressively to ~50% after 1 year follow-up. This is very similar to the 53% of persistence with TIO at 1 year observed in a Canadian study.21 A recent Italian study observed a very high rate of discontinuation of bronchodilators and an increased risk of hospitalization and death associated with discontinuation;26 therefore, strategies to increase adherence are necessary to improve outcomes of therapy.20,27 Interestingly, persistence with therapy was very similar for ACL and TIO despite the different posology. This was also observed by Izquierdo et al28 in another population-based study in Spain in which they observed a high rate of compliance with treatment with LAMAs and no differences between the different products. In any case, patients initiating treatment with ACL or TIO in our study differed in variables that have been shown to have an impact on treatment adherence, for example, severity of the disease, age, and number of concomitant medications.20,21,29 Consequently, these important differences did not allow us to formally compare the rates of persistence between both drugs. Similarly, the medication possession ratios (MPR) in our population were high and ranged from 73% to 79%, very similar to the 78% observed in the Netherlands for LAMAs.30
Our study has some limitations. Studies based on large clinical databases are subjected to possible diagnostic and miscoding bias and invalid data.31 In order to ensure the diagnosis of COPD, we used more restrictive selection criteria that included a spirometric diagnosis of COPD and prescription of respiratory medication after diagnosis. Interestingly, the results in this more restrictive population were almost identical to those obtained in the global population.
Persistence of therapy with ACL and TIO was very similar; however, due to the different characteristics of the patients initiated with ACL or TIO it was not possible to compare adherence to treatment in an unbiased way. In addition, we could not investigate the type of device used (Handihaler or Respimat) or the inhalation technique, which could have provided additional information. Studies specifically designed to analyze compliance should be conducted.
Conclusion
In conclusion, our study shows that patients initiated with ACL in primary care had more severe disease and used more respiratory medications than patients initiated with TIO. Adherence and persistence to treatment with LAMAs was high in real-life clinical practice.
Acknowledgment
The current study has been funded by an unrestricted grant from AstraZeneca UK Limited.
Author contributions
MM and MM wrote manuscript drafts and TRB coordinated statistical analyses. All authors contributed to study design and analysis, data analysis, drafting, reviewing, and critically revising the paper, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
Marc Miravitlles has received speaker fees from Boehringer Ingelheim, AstraZeneca, Chiesi, GlaxoSmithKline, Menarini, Teva, Grifols, and Novartis, and consulting fees from Bayer Schering, Boehringer Ingelheim, GlaxoSmithKline, Gebro Pharma, CLS Behring, Cipla, MediImmune, Mereo Biopharma, Teva, Novartis, and Grifols. The authors report no other conflicts of interest in this work.
References
Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. 2017 Report. Available from: htttp://goldcopd.org/gold-2017-global-strategy-diagnosis-management-prevention-copd/. Accessed December 19, 2016. | ||
Miravitlles M, Vogelmeier C, Roche N, et al. A review of national guidelines for management of COPD in Europe. Eur Respir J. 2016;47:625–637. | ||
Vogelmeier C, Hederer B, Glaab T, et al. Tiotropium vesus salmeterol for the prevention of exacerbations of COPD. N Engl J Med. 2011;364:1093–1103. | ||
Decramer ML, Chapman KR, Dalh R, et al. Once-daily indacaterol versus tiotropium for patients with severe chronic obstructive pulmonary disease (INVIGORATE): a randomised, blinded, parallel-group study. Lancet Respir Med. 2013;1:524–533. | ||
Jones PW, Singh D, Bateman ED, et al. Efficacy and safety of twice-daily aclidinium bromide in COPD patients: the ATTAIN study. Eur Respir J. 2012;40:830–836. | ||
Fuhr R, Magnussen H, Sarem K, et al. Efficacy of aclidinium bromide 400 mg twice daily compared with placebo and tiotropium in patients with moderate to severe COPD. Chest. 2012;141:745–752. | ||
Beier J, Kirsten AM, Mróz R, et al. Efficacy and safety of aclidinium bromide compared with placebo and tiotropium in patients with moderate-to-severe chronic obstructive pulmonary disease: results from a 6 week, randomized, controlled Phased IIIb study. COPD. 2013;10(511):522. | ||
Jones PW, Leidy NK, Hareendran A, Lamarca R, Chuecos F, Garcia Gil E. The effect of aclidinium bromide on daily respiratory symptoms of COPD, measured using the Evaluating Respiratory Symptoms in COPD (E-RS: COPD) diary: pooled analysis of two 6-month Phase III studies. Respir Res. 2016;17(1):61. | ||
Bolíbar B, Fina Avilés F, Morros R, et al. SIDIAP database: electronic clinical records in primary care as a source of information for epidemiologic research. Med Clin (Barc). 2012;138:617–621. | ||
Barrecheguren M, Monteagudo M, Ferrer J, et al. Treatment patterns in COPD patients newly diagnosed in primary care. A population-based study. Respir Med. 2016;111:47–53. | ||
Corrado A, Rossi A. How far is real life from COPD therapy guidelines? An Italian observational study. Respir Res. 2012;106:989–997. | ||
de Miguel DJ, Izquierdo Alonso JL, Molina Paris J, Bellon Cano JM, Rodriguez Gonzalez-Moro JM, de Lucas P. Factors affecting drug prescription in patients with stable COPD: results from a multicenter Spanish study (IDENTEPOC). Arch Bronconeumol. 2005;41:63–70. | ||
Miravitlles M, Mayordomo C, Artés M, Sánghez-Agudo L, Nicolau F, Segú JL. Treatment of chronic obstructive pulmonary disease and its exacerbations in General Practice. Respir Med. 1999;93:173–179. | ||
Miravitlles M, Soler-Cataluña JJ, Calle M, et al. Spanish Guideline for COPD (GesEPOC). Update 2014. Arch Bronconeumol. 2014;50(Suppl 1):1–16. | ||
Tashkin DP, Celli B, Senn S, et al. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med. 2008;359:1543–1554. | ||
Anzueto A, Miravitlles M. Efficacy of tiotropium in the prevention of exacerbations of COPD. Ther Adv Respir Dis. 2009;3:103–111. | ||
Roche N, Jebrak G, Caillaud D, et al. Real-life use of long-acting antimuscarinic agents following their approval for COPD treatment. Eur Respir J. 2015;45:260–262. | ||
Brusselle G, Price D, Gruffydd-Jones K, et al. The inevitable drift to triple therapy in COPD: an analysis of prescribing pathways in the UK. Int J COPD. 2015;10:2207–2217. | ||
Monteagudo M, Rodriguez-Blanco T, Parcet J, et al. Variability in the performing of spirometry and its consequences in the treatment of COPD in primary care. Arch Bronconeumol. 2010;47(5):226–233. | ||
Bourbeau J, Bartlett SJ. Patient adherence in COPD. Thorax. 2008;63:831–838. | ||
Cramer JA, Bradley-Kennedy C, Scalera A. Treatment persistent and compliance with medications for chronic obstructive pulmonary disease. Can respir J. 2007;14(1):25–29. | ||
Price D, Miravitlles M, Pavord I, et al. First maintenance therapy for COPD in the UK between 2009 and 2012: a retrospective database analysis. NPJ Prim Care Respir Med. 2016;26:16061. | ||
Miravitlles M, Anzueto A. A new two-step algorihm for the treatment of COPD. Eur Respir J. 2017;49(2):1602200. | ||
Miravitlles M, Chapman K, Chuecos F, Ribera A, Garcia Gil E. The efficacy of aclidinium/formoterol on lung function and symptoms in patients with COPD categorized by symptoms status: a pooled analysis. Int J COPD. 2016;11:2041–2053. | ||
Soler-Cataluña JJ, Sauleda J, Valdés L, et al. Prevalence and perception of 24-h symptom patterns in patients with stable chronic obstructive pulmonary disease in Spain. Arch Bronconeumol. 2016;52:308–315. | ||
Arfè A, Nicotra F, Cerveri I, et al. Incidence, predictors and clinical implications of discontinuing therapy with inhaled long-acting bronchodilators among patients with chronic obstructive pulmonary disease. COPD. 2016;13:540–546. | ||
Blasi F, Raddi F, Miravitlles M. Interactive monitoring service and COPD: is it possible to reduce nonadherence? COPD. 2015;12:227–232. | ||
Izquierdo JL, Paredero JM, Piedra R. Relevance of dosage in adherence to treatment with long-acting anticholinergics in patients with COPD. Int J Chron Obst Pulm Dis. 2016;11:289–293. | ||
Sanduzzi A, Balbo P, Candoli P, et al. COPD: adherence to therapy. Multidiscip Respir Med. 2014;9:60. | ||
Koehorst-ter K, Kort S, van der Palen J, et al. Quality of life and adherence to inhaled corticosterois and tiotropium in COPD are related. Int J Chron Obst Pulm Dis. 2016;11:1679–1688. | ||
Roche N, Reddel H, Martin R, et al. Quality standards for real-world research. Ann Am Thorac Soc. 2014;11:S99–S104. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.