Back to Journals » Transplant Research and Risk Management » Volume 13
Characteristics and Outcomes of Cytomegalovirus Infection in Seropositive Kidney Transplant Recipients in the Era of Antiviral Prophylaxis with Valacyclovir: A Single-Center Study in Morocco
Authors Rezzouk B , Bouattar T, Belkadi B, Razine R, Bayahia R, Ouzeddoun N, Benamar L, Rhou H, Bouihat N, Ibrahimi A, Seffar M, Kabbaj H
Received 25 August 2020
Accepted for publication 5 January 2021
Published 25 January 2021 Volume 2021:13 Pages 1—13
DOI https://doi.org/10.2147/TRRM.S278655
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Qing Yi
Bouchra Rezzouk,1 Tarik Bouattar,2,3 Bouchra Belkadi,1 Rachid Razine,4 Rabia Bayahia,2,3 Naima Ouzeddoun,2,3 Loubna Benamar,2,3 Hakima Rhou,5 Najat Bouihat,6 Azeddine Ibrahimi,3,7 Myriam Seffar,3,6 Hakima Kabbaj3,6
1Laboratory of Microbiology and Molecular Biology, Faculty of Science, University Mohammed V, Rabat, Morocco; 2Department of Nephrology, Dialysis, Renal Transplantation, Ibn Sina University Hospital Center, Rabat, Morocco; 3Faculty of Medicine and Pharmacy, Mohammed V University, Rabat, Morocco; 4Laboratory of Social Medicine, Epidemiology and Clinical Research, Faculty of Medicine and Pharmacy, Mohammed V University, Rabat, Morocco; 5Department of Nephrology, Dialysis, Renal Transplantation, Sheikh Zaid International University Hospital, Rabat, Morocco; 6Central Laboratory of Virology, Hospital of Specialties, Ibn Sina University Hospital Center, Rabat, Morocco; 7Biotech Laboratory (Med Biotech), Faculty of Medicine and Pharmacy, Mohammed V University, Rabat, Morocco
Correspondence: Bouchra Rezzouk 7, Avenue Madagascar, Rabat, Morocco
Tel + 212 64 94 31 25
Email [email protected]
Purpose: Despite the use of antiviral prophylaxis with valacyclovir, cytomegalovirus infection (CMV) can still occur in seropositive kidney transplant recipients. In this study, we aimed to assess the incidence of CMV DNAemia and its risk factors in Moroccan transplant recipients.
Patients and Methods: Sixty kidney recipients with positive cytomegalovirus serostatus, receiving post-transplant prophylaxis were enrolled between 2013 and 2017. In total, 455 plasma samples were collected and tested for CMV DNAemia using PCR-based Abbott RealTime assays.
Results: The incidence of CMV infection in seropositive patients was 63%. In patients with quantifiable DNAemia, the duration of CMV infection was significantly shorter than in those with detectable DNAemia (141.5 ± 96.9 vs 294.1 ± 112.6 days, P < 0.001). During prophylactic treatment, 14 of 30 patients (47.0%) experienced active replication with quantifiable DNAemia, whereas none of eight patients with detectable DNAemia did (P = 0.017). Patients with symptomatic DNAemia were significantly younger than those without symptoms (28.8 ± 5.12 vs 38.1 ± 12.34 years, P = 0.007). The peak viral loads were significantly associated with viral disease (odds ratio: 3.39, 95% confidence interval: 1.21– 9.53, P = 0.02). The duration of DNAemia (21.2 vs 13.4 days, P = 0.028) was significantly longer in symptomatic patients. Significantly higher rates of acute rejection were exclusively observed in recipients with disease (4/8, 50% vs 0/22, 0%, P = 0.003).
Conclusion: Patients with high-level DNAemia were at an increased risk of progression to disease and acute rejection. Monitoring the viral load during the first year post-transplantation is essential, to support current preventive strategies.
Keywords: cytomegalovirus, DNAemia, kidney transplant, disease, acute rejection
Introduction
Human cytomegalovirus (CMV) is a ubiquitous herpesvirus and is a common cause of complications in immunocompromised individuals, including transplant recipients.1–3 In the absence of prophylactic treatment, CMV disease affects up to 60% of transplant recipients.4 In patients receiving a kidney transplant, CMV can induce severe disease5,6 and indirectly decrease graft function, thus increasing morbidities, such as coinfection, cardiovascular disease, malignancies, and graft loss, and leading in the long term to increased mortality.7–10 Previously, serological mismatches between a donor and a recipient, such as occurs with a seronegative recipient and a seropositive donor (D+R–), was an important risk factor for the occurrence of CMV disease.11,12 However, seropositive recipients can also be at high risk because of CMV reactivation, or from reinfection by a novel strain derived from the donor.13 Virus reactivation from latency, or reinfection, is likely to occur in patients receiving intensive immunosuppressive agents, and may have serious clinical effects after kidney transplantation.14
To prevent CMV disease, recent consensus guidelines recommend a prophylactic treatment for three months for R+ patients or up to six months for those receiving potent immunosuppressive induction therapy.5,15 In developed countries, valganciclovir and oral ganciclovir are currently the most common used drugs for prophylaxis in kidney transplant recipients,16,17 and seropositive recipients are generally given prophylactic treatment for short periods. However, at our center, prophylactic treatment with valganciclovir is not available, because it is cost prohibitive for many patients. Patients who are not enrolled in national health insurance or medical assistance programs are not eligible for valganciclovir prophylaxis. We therefore routinely use valacyclovir for the majority of patients over six months of prophylactic treatment instead of the recommended three months, followed by monthly monitoring for CMV DNAemia—the presence of viral load in samples of plasma—during the same period. Valganciclovir prophylaxis is an alternative option.
There is an abundant literature on CMV infection in seropositive patients receiving various forms of induction therapy and antiviral prophylaxis for a short duration. However, there have been few reports on treatment with valacyclovir for six months. Thus, we present our data on the extent of reactivation or reinfection in patients undergoing T cell depletion with the outcome of CMV DNAemia, and the potential risk factors associated with symptomatic CMV infection, as well as the impact of CMV infection on allograft rejection in Moroccan kidney transplant recipients.
Patients and Methods
Study Population
In this retrospective study, patient medical records for all kidney transplants performed between March 2013 and August 2017 at University Hospital Ibn Sina (Rabat, Morocco) were reviewed. In this period, only CMV-seropositive (IgG) recipients who were at least 15 years old at transplantation, and who had received a living- or deceased-donor kidney transplant were included, because these recipients represent an important proportion of our transplanted population (60/62; 97%). The other selection criteria are summarized in a flow chart (Figure 1). The study was approved by the institutional ethics committee of the Faculty of Medicine and Pharmacy, Mohammed V University, Rabat, Morocco (approval number 26/18-2017) and conducted in compliance with the Declaration of Helsinki. For this descriptive study, written informed consent was obtained from all patients. In our center, all organs were donated voluntarily with written informed consent, and the organ donations were conducted in accordance with the declaration of Istanbul.
 |
Figure 1 Flow chart. |
Of the patient cohort in this study, 50 recipients (83.3%) had received rabbit antithymocyte globulin (thymoglobulin) as an induction therapy, at a total dose of 5 mg/kg for five days, and those at high risk of rejection had received of basiliximab (20 mg) intravenously on day zero and day four during the first week post transplantation. The induction therapy was administered in association with a calcineurin inhibitor. Tacrolimus was administered twice daily at an adjusted dose of 0.075 mg/kg according to the ideal body weight, with regular control of plasma drug concentrations. The target concentrations for the first year post transplant were in the range of 8–12 ng/mL. For patients who were administered cyclosporine, the initial posology was 250 mg/5 mL, which was gradually reduced to 100 mg/5 mL as a maintenance treatment. All patients were administered methylprednisolone at a dose of 500 mg IV for a period of three days, and prednisone was prescribed as a loading dose at 20 mg per day in the first week of transplantation, then gradually decreased by 5 mg per week until a dose of 5 mg was reached, six months after kidney transplant. Most of the patients had initially received mycophenolate mofetil, but a few of them were switched to mycophenolate acid or azathioprine for clinical gastrointestinal problems.
For the diagnosis of suspected acute rejection, transplant kidney biopsies were performed. Indications for biopsy were an increased serum creatinine level or delayed graft function. Patients with presumed acute rejection were treated with high-dose intravenous corticosteroids and/or a switch to tacrolimus if they had been initially treated with cyclosporine. Acute rejection episodes were considered to be a result of CMV DNAemia if they occurred at the time of, or after, viral reactivation or reinfection.
Preventive Strategies and Antiviral Treatment
CMV prophylaxis was administrated to all patients for six months after transplantation. Valacyclovir prophylaxis was initiated in 48 of 60 renal transplant patients (80%), with a preventative dose of 1500 mg administered four times per day. Twelve recipients of the transplant group (20%) received valganciclovir at a dose of 450 mg every 12 hours, as recommended by the International Consensus Guidelines.14 Drug dosage was adjusted for renal function when required. All patients receiving antiviral prophylaxis were monitored monthly using Quantitative Nucleic Acid Tests (QNATs) during the first six months. When viral replication was detected in patients with a low viral load without symptoms, regular monitoring by QNAT was performed once weekly until viral clearance was observed, and no patient was treated. Conversely, if a significant symptom (syndrome or disease) or higher viral load values were detected, intravenous ganciclovir 5 mg/kg/dose q 12 h was administered as the main treatment, with the dose adjusted to kidney function. CMV treatment was stopped after CMV DNAemia was not detected in two consecutive tests. One patient with kidney function impairment did not receive antiviral treatment; instead, a reduction of immunosuppression was adopted.
Definition of Outcome Variables
The proposed definitions were based on the Kotton15 and Ljungman18 guidelines. CMV infection is defined as evidence of CMV replication regardless of symptoms (differs from latent CMV) or detection of viral proteins (antigens) or nucleic acid in any body fluid or tissue specimen. Asymptomatic CMV infection was defined as “CMV replication without clinical signs and symptoms of disease”5 CMV disease was defined as “CMV infection associated with clinical signs or symptoms”, and was further categorized as viral syndrome, manifesting as fever, malaise, leukopenia, and/or thrombocytopenia, or tissue-invasive.5,15 CMV reactivation was defined as “active viral DNA replication in a recipient who had been infected by CMV before kidney transplantation” (R+). Reinfection was defined as the presence “of a CMV strain that is distinct from the strain that caused initial infection” and the presence of viral load in samples of plasma was termed DNAemia”.5
Data were collected from the patients’ medical records. These data included age at transplantation, gender, date of transplantation, previous kidney replacement therapy modality (hemodialysis, peritoneal dialysis, or preemptive transplantation), primary renal disease, presence of comorbidities, human leukocyte antigen (HLA) matching (HLA-AB and -DR), induction therapy, and initial immunosuppressive regimen. Follow-up data included liver function test results (alanine aminotransferase, aspartate aminotransferase), immunological follow-up (anti-HLA I and II antibodies), renal function (creatinine and clearance creatine), and blood counts (leukocytes, polynuclear neutrophils, lymphocytes). Data regarding CMV prophylactic treatment included the type of antiviral drug (valacyclovir, valganciclovir) and doses taken, and the duration of prophylaxis treatment. For donors, we recorded demographic characteristics, donor status (living, deceased), pretransplant CMV serostatus, and immunological and serological characteristics.
Information related to DNAemia at the time of follow-up included viral load at diagnosis, peak viral load, duration of quantifiable DNAemia, and number of reactivation or reinfection episodes, after transplantation, at the time of prophylactic treatment, after treatment discontinuation, and during post-transplant follow-up. Data on CMV infection included clinical findings, including clinical syndrome features, such as fever, malaise, vomiting, asthenia, and headaches, and symptoms of disease, including diarrhea, colitis, hepatitis, and pneumonitis.
Data on immunosuppressive treatment during infection covered the type and dosage of immunosuppressive drugs. Other data collected included the antiviral drugs used for curative treatment of CMV infection (ganciclovir, valganciclovir, and valaciclovir), the length of curative treatment, and treatment of second prophylaxis (type of drug, duration). Occurrence of coinfection as viral (BKV, HBV, HCV, EBV), bacterial, or fungal infection, and acute rejection were also evaluated.
CMV Assessment by qPCR
For all patients, plasma was collected during the first month of transplantation. CMV DNAemia was assessed monthly during CMV prophylaxis, and once at the time of prophylaxis discontinuation. After the cessation of prophylaxis, patients were monitored once per month for 90 days. Plasma samples were tested at the Central Laboratory of Virology (Ibn Sina University Hospital Center, Rabat, Morocco) using Abbott RealTime CMV assays (Abbott Molecular Inc., Des Plaines, IL, USA). Viral DNA was isolated from 500 µL of plasma (EDTA) via the automated method Abbott m24sp, according to the manufacturer’s instructions. The amplification of two target genes, UL34 and UL80.5, was performed on an m2000rt thermal cycler, following the instructions provided in the Abbott m2000rt technical manual. The choice of these genes was based on the presence of highly conserved regions. For quantification of the viral load, we used a calibration curve generated from replicate analysis of three of the two calibrators (A and B) whose CMV concentration was expressed in log10 UI/mL versus the threshold cycle (CT), at which a fluorescent signal reagent level was detected.
Quantitative real-time PCR results were calibrated to the World Health Organization (WHO) standard (code 09/162 National Institute for Biological Standards and Control, Hertfordshire, UK).19 The limit of quantification was 1.49 log10 UI/mL (31.20 UI/mL), and our results were reported in log10 UI/mL. In this study, detectable DNAemia was diagnosed when CMV DNA was present, but the result was below the limit of quantification <1.49 log10 UI/mL (31.2 UI/mL), whereas quantitative DNAemia was defined as the results obtained from the quantitation range between 1.49 and 8.19 log10 UI/mL (31. 20–156.000.000 UI/mL).
Statistical Analysis
The results were presented as mean plus or minus standard deviation (SD), or median with range for continuous variables, and as frequencies if variables were categorial. Groups of patients with CMV DNAemia (detectable vs quantifiable, asymptomatic vs with CMV disease) were compared using parametric Student’s t-tests when continuous data were normally distributed. For non-normally distributed data, only non-parametric Mann–Whitney U-tests were used. Categorial data were analyzed using Fisher’s exact tests or chi-squared tests for comparisons between subgroups.
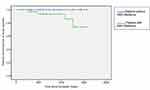
The time of CMV reactivation or reinfection, incidence of CMV disease and acute rejection were calculated using the Kaplan–Meier method, and Log rank tests were used to compare survival between patient groups. Univariate logistic regression models were established to predict symptomatic CMV infection and quantifiable DNAemia, and the most significant variables were selected as risk factors. Logistic regression results are expressed as the odds ratio (OR) and 95% confidence interval (CI). P-values < 0.05 were considered to indicate significance, and all statistical calculations were performed with SPSS v. 13 (SPSS, Inc., Chicago, Il, USA).
Results
Incidence of CMV Reactivation and Reinfection
In the four-year study period 2013–2017, 60 seropositive kidney transplant recipients were treated in our hospital, and were enrolled in this study. Twenty-six patients (43.3%) were female, and mean age was 38.8 ± 12.74 years. Arterial hypertension was the predominant cause of kidney failure (30 patients; 88.2%) and 49 patients (81.7%) had received an organ from a living donor (Table S1a, Table S1b). The mean time of follow-up after transplantation was 795 ± 444 days (range: 120–1580 days). During this period, one patient died (1.7%), and another (1.7%) returned to dialysis. The cause of death was malignancy, and the graft loss resulted from primary hyperoxaluria. Most of the transplant recipients (83%) received thymoglobulin followed by tacrolimus monotherapy (83%), whereas 10 (17%) received only basiliximab (Table S1c). Thirty-eight recipients (63%) developed a first episode of reactivation or reinfection after kidney transplantation. The incidence rate of CMV reactivation or reinfection was 27 per 100 person-years, and the median time to reactivation was 227 days (range 14–1560 days) (Figure S1).
Patients with Quantifiable CMV DNAemia
In the context of CMV DNAemia, 455 plasma samples were collected (eight samples per patient, on average). Eight patients (21.1%) developed one episode of detectable DNAemia below the quantification threshold (<1.49 log10 IU/mL). Thirty of 60 patients (50%) developed at least one episode of quantifiable viral load (mean = 2.4 ± 1.19 log IU/mL) with 1.49 to 6.79 log IU/mL. The first viral replication after transplantation occurred earlier in patients with quantifiable DNAemia than in those with detectable DNAemia (141.5 ± 96.9 vs 294.1± 112.4 days, P < 0.001) (Table 1). Univariate logistic analyses revealed that the time of active replication was a highly significant risk factor for the development of quantifiable CMV DNAemia [OR 0.98 (95% IC 0.98, 0.99), (P = 0.004)]. Patients who had viral replication early, approximately five months after transplantation, were more likely to experience a quantifiable DNAemia than were patients who had later viral replication. In contrast with patients who had delayed replication (approximately 10 months), detectable DNAemia was mainly observed after transplant. During prophylaxis, 14 of 30 patients with quantifiable CMV DNAemia tested significantly positive for CMV DNAemia [14 (47%) vs 0 (0%), P = 0.017] (Table 1).
 |
Table 1 Characteristics of Patients with Detectable DNAemia and Those with Quantifiable DNAemia |
Patients with Symptomatic CMV DNAemia
Twenty-two of the 30 patients with quantifiable DNAemia (73%) remained asymptomatic. Only eight members of this subgroup (27%) developed CMV disease, two of whom (25%) had syndrome, and six (75%) had severe clinical disease. The incidence rate of symptomatic DNAemia was 0.06 cases per person-years at risk. Seven of eight symptomatic patients (87.5%) developed CMV syndrome or disease within the first five months after kidney transplantation. Two patients with CMV syndrome presented with low-grade fever, mild lymphocytopenia, and a slightly increased alanine aminotransferase level. However, in five cases with CMV disease, severe infection was observed as diarrhea, leucopenia, lymphopenia, and low-level renal functional impairment. One patient presented with pneumonia. Patients with CMV disease were significantly younger than those with asymptomatic infection (38.1 ± 12.34 vs 28.8 ± 5.12, P = 0.007) (Table 2).
CMV DNAemia and Peak Viral Load in Recipients with CMV Disease
The median total duration of CMV quantifiable DNAemia was significantly longer in recipients with CMV disease than that in asymptomatic recipients 21.2 days (range 1 to 570 days) vs 13.4 days (range 1 to 42 days), (P = 0.028). In the former, the highest value of CMV DNAemia was detected later after kidney transplantation than in the group without symptoms (190.2 ± 95.72 days vs 140.5 ± 77.13 days, P = 0.15) (Table 3). However, the mean peak viral load was significantly higher in symptomatic patients (3.8 ± 1.59 log UI/mL vs 2.4 ± 0.79, P = 0.003), and was identified as a risk factor for clinical symptomatic DNAemia [OR 3.39 (95% IC 1.21 −9. 53), (P = 0.02)] (Table 4). Log Rank tests revealed that there was a significantly different risk for developing CMV disease during prophylactic treatment in those with peak viral loads (P= 0.004) (Figure 2).
 |
Table 2 Characteristics of Patients with Asymptomatic CMV Infection and Those with CMV Disease |
 |
Table 3 Characteristics of Patients with Asymptomatic DNAemia and Those with Disease DNAemia |
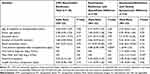 |
Table 4 Analysis of Risk Factors of Reactivation/Reinfection in Seropositive Kidney Transplant Recipients with Quantifiable DNAemia and Their Clinical Symptoms (D+/R+) |
CMV DNAemia and Acute Rejection
Four patients who developed CMV disease and no patient with asymptomatic infection experienced one episode of acute rejection, confirmed by biopsy (50% vs 0%, P = 0.003) (Table 3). Acute rejection was detected after the occurrence of CMV DNAemia in three cases, whereas in one patient, acute rejection and CMV DNAemia were detected simultaneously. Among these patients, the mean time from transplantation to rejection was 228.8 ± 144.8 days, whereas the median time from occurrence of initial DNAemia to rejection was 41 days (range 8 to 128 days). Graft survival during post-transplantation follow-up did not show any difference in patients with or without DNAemia (P = 0.12) (Figure 3). In contrast, patients with symptomatic DNAemia had a significantly increased risk of developing acute rejection in less than 500 days after transplantation, compared to asymptomatic patients (P = 0.001) (Figure 4).
CMV DNAemia and Coinfection
Coinfection was significantly more prevalent in patients with CMV disease than in those with asymptomatic infection [6/8 (75%) vs 5/22 (23%), P = 0.028] (Table 3). Polyoma BK virus infection was more prevalent in the first group, but there was no significant difference in the incidence rate between the two groups.
Antiviral Therapy
For CMV prophylaxis, comparing the effect of valacyclovir with that of valganciclovir, there was similar efficacy between patients with DNAemia and those without (P = 0.33) (Table S1). The choice of antiviral agent for prophylaxis did not produce any difference in the occurrence of CMV disease between symptomatic patients and those without clinical symptoms (75% vs 12.5%, P = 0.39) (Table 2). For treatment of CMV high DNAemia or disease, the median total treatment duration was significantly longer in patients with CMV disease than in those without symptoms (median period = 24.3 days, ranging from 21 to 55 days vs 12.3 days, ranging from 15 to 30 days, P < 0.001) (Table 3). To treat the disease, six of eight patients with CMV disease (75%) received intravenous ganciclovir for CMV DNAemia, and one patient in this subgroup (12.5%) received valganciclovir. Another patient did not receive any medical therapy, owing to his severe renal dysfunction. In all of these patients, the dose of mycophenolate mofetil was temporary reduced. In the asymptomatic group, ganciclovir was administered to five recipients (22.7%) who exhibited a high viral load (mean peak viral load: 3.59 ± 0.49 log UI/mL) and one patient (4.5%) required only valaciclovir therapy. In 17 of 22 patients (77%) who remained asymptomatic, prophylactic treatment was not changed.
Discussion
This study revealed that virus replication is common in CMV-seropositive kidney transplant recipients receiving prophylaxis; the first episode of infection was observed in 38 of 60 patients (63%). This finding was in accordance with the findings of recent studies, in which 43–61.9% of seropositive patients experienced CMV DNAemia.20,21 The replication of viral CMV has been described by other studies. Chou22 demonstrated that seropositive patients are more likely to be re-infected with new strains than to have active replication of the latent virus. Harvala23 and Reusing24 suggested that R+ patients might be at risk of viral infection, as they receive high-dose immunosuppressive treatment during the first three months of follow-up. However, our data did not support this finding in patients treated with lymphocyte-depleting agents such as thymoglobulin or other immunosuppressive drugs.
qPCR-based monitoring of CMV DNAemia revealed that 30 of 38 (~79%) of patients had a quantifiable CMV DNAemia. These patients generally experienced viral replication earlier than those with only detectable DNAemia below 1.49 log10 UI/mL. Previous studies have suggested that early onset of infection is a risk factor for the occurrence of quantifiable DNAemia.25,26 Although most patients presented a quantifiable CMV viral load, the incidence of CMV disease was relatively low (8/60; 13%). Similar results have been reported in a previous study using a similar patient population.24
Higher peak viral loads were correlated with an increased risk of CMV disease, an observation which is consistent with the results of a meta-analysis by Natori.25 They reported that the mean viral load remained significantly high in patients with CMV disease (OR: 9.3; 95% CI: 4.6–19.3). Consequently, these patients had substantially prolonged DNAemia, with a longer time to viral clearance, compared with symptom-free patients (21 vs 13 days on average; P = 0.028). However, high CMV loads were also observed in some patients with asymptomatic infection. Similarly, in a previous study, 13 patients without CMV-related clinical signs showed a high viral load.27 These discrepancies may be explained by various factors, such as the presence of re-stimulated CMV-specific cellular immunity in the host, limited virus dissemination, source of reactivated CMV strains, and possibly, concomitant reactivation of several strains. Patients who developed high-level DNAemia without evidence of organ-invasive disease may have been exposed to the indirect effects of CMV.
The establishment of a viral load threshold is crucial not only for pre-emptive treatment but also for the identification of other opportunistic infections, acute rejection, or graft dysfunction. Accordingly, multiple centers have aimed to establish cut-offs of viral loads for qPCR assays for initiating antiviral therapy in patients at risk of CMV infection.26,28 Previous studies have shown that stratification of CMV infection according to viral load is important, in order to differentiate between patients with high-level DNAemia that will develop CMV disease, and those that will not. Although we used qPCR assays according to international guidelines,19 we were not able to establish viral load thresholds as recommended by Kotton.15 The number of total patients (N = 60) in the follow up was relatively small.
However, our qPCR results cannot be compared, because in several studies, the viral load thresholds were obtained by specific laboratory tests, which were not calibrated in accordance with the WHO International Standard Unit (IU/mL). Thus, to initiate pre-emptive therapy, future studies should determine appropriate thresholds, especially for seropositive patients.
Several studies have shown that advanced age is associated with the occurrence of invasive CMV disease.9,29,30 The elderly generally have weakened immunity, which is exacerbated by immunosuppression treatment.20,31 However, in our cohort, young patients were more likely to experience symptomatic DNAemia (28.75 ± 5.12 vs 38.09 ± 12.34; P < 0.007). Although our population was composed mainly of young patients, the frequency of clinical manifestations does not exclude the possibility of interference from immunological factors. Thompson32 demonstrated, based on the QuantiFERON-CMV test, that regardless of age, patients with low levels of anti-CMV immune cells were more likely to experience intensive DNAemia associated with severe clinical manifestations. We cannot currently explain this finding in our study, because of a lack of data on immunological parameters, such as specific CMV-antibody titers and T lymphocytes.
The efficacy of valacyclovir prophylaxis has been found to be comparable to that of valganciclovir. This result was important in our center, because the use of valacyclovir was not only considered for its clinical advantages, which have been reported in several studies,14,33 but more importantly, for its low cost.34 Our observation suggests that valacyclovir may be used as the first line of prophylactic treatment for patients who do not have an opportunity to be treated with valganciclovir or oral ganciclovir in low- and middle-income countries.
Patients with high viral loads, undergoing immunosuppression treatment, may have an increased risk of developing acute rejection. In our study, all patients experiencing transplant rejection had CMV disease. Several studies have suggested an association between the occurrence of acute rejection and CMV disease.17,35–37 High viral loads (>10.000 copies/mL) were recently reported to be a risk factor for acute rejection.38,39 However, other studies did not reveal any evidence for causal correlation.24,40 In a study by Erdbruegger,40 acute rejection was observed only in patients who received triple immunosuppression therapy. At present, the determinants of acute rejection in symptomatic patients have not been fully elucidated. However, it is possible that dose reduction of mycophenolate mofetil, as well as higher viral load, were important to this observation. CMV has been also implicated in the upregulation of immunological markers such as cytokines, regulatory T cells, and human histocompatibility class II markers.41 Delayed graft function has been also considered to be a risk factor for rejection.40 Therefore, it is important to know whether other immunological parameters interfere with graft survival following a temporary reduction in immunosuppressants at the time of treatment for CMV disease. Finally, we found that patients with CMV disease had more frequent opportunistic infections, with viral infections being the most common. This finding indicates that the antiviral prophylactic treatment used must be continued, to prevent other infections.38
This study had several significant limitations. First, this was a retrospective study with a small sample size, which limits the robust statistical testing of variables to identify risk factors. It is recommended not to include more than one variable per 10 events; accordingly, we could not establish multivariate regression models for all factors with P < 0.2 in univariate analysis. Second, this was a single-center study, which may limit the generalizability of our results. Third, we did not perform tests for monitoring CMV-specific immunity; it is possible that patients with a high viral load without symptoms may have had immune dysfunction during prophylaxis. Lastly, because patients in this study received valaciclovir as primary prophylaxis for six months, with monthly monitoring for CMV DNAemia during the same period, our data cannot be compared to other studies in which different treatments were used for CMV prophylaxis in seropositive recipients, who are most often receiving valganciclovir prophylaxis.
Nevertheless, this study had several strengths. It included a representative population of seropositive kidney transplant recipients. All measurements of CMV DNAemia were performed in plasma using the QNAT assay in the same laboratory, and were expressed using international standard units. The same standardized protocol of immunosuppression and different treatment strategies were adopted in our cohort of kidney recipients.
Conclusions
Our findings demonstrated that CMV infection remains a serious problem in seropositive transplant recipients, who are expected to be on antiviral prophylaxis. Our data suggested that younger patients with high-level DNAemia may be at increased risk of progression to CMV disease and adverse events, such as acute rejection. To support current prevention strategies, intensive viral load monitoring during the first year post-transplantation, as well as the investigation of suspected antiviral resistance, is essential. Therefore, further investigations should be conducted to determine the viral load thresholds at which preemptive therapy must be initiated.
Acknowledgments
The authors thank all patients who participated in the study and staff at the renal service Ibn Sina hospital. Special thanks were addressed to group members at Central Laboratory of Virology for their technical assistance in performing the real-time PCR assays.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Griffiths P, Baraniak I, Reeves M The pathogenesis of human cytomegalovirus. J Pathol. 2015; 235(2): 288–297.
2. Mazeron MC, Alain S, Leruez-Ville M, et al. Infections à cytomégalovirus. EMC. 2015; 12(4): 1–13.
3. Kotton CN CMV: prevention, diagnosis and therapy. Am J Transplant 2013; 13: 24–40.
4. Sagedal S, Hartmann A, Rollag H The impact of early cytomegalovirus infection and disease in renal transplant recipients. Clin Microbiol Infect. 2005; 11: 518–530.
5. Razonable RR, Humar A Cytomegalovirus in solid organ transplant recipients-Guidelines of the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019; 33: 1–23.
6. Emery VC, Asher K, Sanjuan CJ Importance of the cytomegalovirus seropositive recipients as contributor to disease burden after solid organ transplantation. J Clin Virol 2012; 54: 125–129.
7. Kaminski H, Couzi L, De´chanet-Merville J et al. Intérêt de l’immuno-surveillance dans l’infection à cytomégalovirus en transplantation rénale: mise au point et perspectives. Nephrol Ther. 2015.
8. Weclawiak H, Mengelle C, Ould Mohamed A, et al. Effets du cytomégalovirus en transplantation et place de la prophylaxie antivirale. Nephro Ther. 2010; 505–512.
9. Kanter J, Pallardo L, Gavela E, et al. Cytomegalovirus infection renal transplant recipients: risk factors and outcomes. Transplantation Proc. 2009; 41: 2156–2158.
10. Seale H, Dwyer DE, Chapman JR, et al. Cytomegalovirus disease amongst renal transplant recipients in Australia and New Zealand. Virology 2008; 1: 65–73.
11. Schlott F, Steubl D, Hoffmann D, et al. Primary cytomegalovirus infection in seronegative kidney transplant patients is associated with protracted cold ischemic time of seropositive donor organs. PLoS One. 2017; 12(1): e0171035.
12. Becker BN, Becker YT, Leverson GL, et al. Reassessing the impact of cytomegalovirus infection in kidney and kidney pancreas transplantation. Am J Kidney Dis. 2002; 39(5):1088–1095.
13. Kim T, Lee HJ, Kim SM, et al. Diagnostic usefulness of the cytomegalovirus (CMV) – specific T cell-based assay for predicting CMV infection after kidney transplant. Korean J Intern Med. 2018.
14. Kamar N, Mengelle C, Esposito L, et al. Predictive factors for cytomegalovirus reactivation in cytomegalovirus- seropositive kidney- transplant patients. J Med Virol 2008; 80:1012–1017.
15. Kotton NC, Kumar D, Caliendo AM, et al. The third international consensus guidelines on the management of cytomegalovirus in solid organ transplantation. Transplantation. 2018 102(6): 900–931.
16. Rissling O, Naik M, Brakemeier S, et al. High frequency of valganciclovir underdosing for cytomegalovirus prophylaxis after renal transplantation. Clin Kidney J 2017: 1–10.
17. Byrns JS, Pilch NW, Taber D Impact of pharmacist involvement in early identification and enrollment patient assistance programs on CMV outcomes in transplantation. J Pharm Pract 2014: 1–6.
18. Ljungman P, Boeckh M, Hirsch HH, et al. Definitions of cytomegalovirus infection and disease in transplant patients for use in clinical trials. Clin Infect Dis. 2017; 64(1): 87–91.
19. Fryer JF, Heath AB, Minor PD, collaborative study group. A Collaborative Study to Evaluate the Proposed 1st WHO International Standard for Human Cytomegalovirus (HCMV) for Nucleic Acid Amplification (NAT)-Based Assays. World Health Organization. 2010.
20. Iglesias-Escudero M, Moro-Garcia MA, Marcos-Fernandez R, et al. Levels of anti-CMV antibodies are modulated by the frequency and intensity of virus reactivations in kidney transplant patients. PLoS One. 2018; 13(4): 1–16.e0194789.
21. Chitasombat MN, Watcharananan SP Burden of cytomegalovirus reactivation post kidney transplant with antithymocyte globulin use in Thailand: a retrospective cohort study. F1000 Res. 2018; 7: 1568.
22. Chou S Acquisition of donor strains of cytomegalovirus by renal transplant recipients. N Engl J Med. 1986; 314(22): 1418–1423.
23. Harvala H, Stewart C, Muller K, et al. High risk of cytomegalovirus infection following solid organ transplantation despite prophylactic therapy. J Med Virol 2013; 85: 893–898.
24. Reusing JO, Feitosa EB, Agena F, et al. Cytomegalovirus prophylaxis in seropositive renal transplant recipients receiving thymoglobulin induction therapy: outcome and risk factors for late CMV disease. Transpl Infect Dis. 2018; 20(5):e12929. doi:10.1111/tid.12929.
25. Natori Y, Alghamdi A, Tazari M, et al. Use of viral load as surrogate marker in clinical studies of cytomegalovirus in solid organ transplantation: a systematic review and meta-analysis. Clin Infect Dis. 2018; 66 (4): 617–631.
26. David-Neto E, Triboni AHK, Paula FJ, et al. A double -blinded, perspective study to define antigenemia and quantitative real-time polymerase chain reaction cutoffs to start preemptive therapy in low risk, seropositive, renal transplanted recipients. Transplantation. 2014; 98(10):1077–1081.
27. Madi N, Al-Qaser M, Edan R, Al-Nakib W Clinical utility of viral load in the management of cytomegalovirus infection in solid organ transplant patients in Kuwait. Transplant Proc 2015; 47:1802–1807.
28. Martín-Gandul C, Pérez-Romero P, Sánchez M, et al. Determination, validation and standardization of a CMV DNA cut-off value in plasma for preemptive treatment of CMV infection in solid organ transplant recipients at lower risk for CMV infection. J Clin Virol 2013; 56: 13–18.
29. Navarro-Rodríguez V, Herrera-Munoz A, Castro A, Ramos-Esquivel A Risk factors for cytomegalovirus disease in seropositive renal transplant recipients; a single- center case- controlled study. J Nephropathol. 2017; 6(3): 240–245.
30. Nemati E, Eizadi M, Moghani Lankarani M, et al. Cytomegalovirus disease after kidney transplantation: clues to accurate diagnosis. Transplant Proc 2007; 39: 987–989.
31. Zieliński M, Tarasewicz A, Zielińska H, et al. Impact of donor and recipient human cytomegalovirus status on kidney transplantation. Int Immunol. 2017; 29(12): 541–549.
32. Thompson G, Boan P, Baumwol J, et al. Analysis of the QuantiFERON-CMV assay, CMV viraemia and antiviral treatment following solid organ transplantation in Western Australia. Pathology. 2018:1–8.
33. Ko EJ, Yu JH, Yang CW, et al. Usefulness of valacyclovir prophylaxis for cytomegalovirus infection after anti-thymocyte globulin as rejection therapy. Korean J Int Med. 2019; 34: 375–382.
34. Kacer M, Kielberger L, Bouda M, et al. Valganciclovir versus valacyclovir prophylaxis for prevention of cytomegalovirus: an economic perspective. Transplant Infec Dis 2015; 17:334–341.
35. Reischig T, Jindra P, Svecova M, et al. The impact of cytomegalovirus disease and asymptomatic infection on acute renal allograft rejection. J Clin Virol 2006; 36: 146–151.
36. Keven K, Basu A, Tan HP, et al. Cytomegalovirus prophylaxis using oral ganciclovir or valganciclovir in kidney and pancreas-kidney transplantation under anti-body preconditioning. Transplant Proc 2004; 36: 3107–3112.
37. Toupance O, Bouedjoro-Camus MC, Carquin J, et al. Cytomegalovirus -related disease and risk of acute rejection in renal transplant recipients: a cohort study with case -control analyses. Transpl Int. 2000; 13:413–419.
38. Blasquez-Navarro A, Dang-Heine C, Wittenbrink N, et al. BKV, CMV, and EBV interactions and their effect on graft function one year post- renal transplantation: results from a large multi-center study. EBioMedicine. 2018; 34:113–121.
39. Reischig T, Kacer M, Hruba P, et al. The impact of viral load and time to onset of cytomegalovirus replication on long-term graft survival after kidney transplantation. Antivir Ther. 2017; 22(6):503–513.
40. Erdbruegger U, Scheffner I, Mengel M, et al. Impact of CMV infection on acute rejection and long-term renal allograft function: a systematic analysis in patients with protocol biopsies and indicated biopsies. Nephrol Dial Transplant. 2012; 27:435–443.
41. Cho JH, Yoon YD, Jang HM, et al. Immunologic monitoring of T- lymphocyte subsets and Hla- Dr -positive monocytes in kidney transplant recipients. Medicine. 2015; 94 (44):1–8.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.