Back to Journals » Neuropsychiatric Disease and Treatment » Volume 16
Changes in Demographic and Diagnostic Spectra of Patients with Neurological Symptoms Presenting to an Emergency Department During the COVID-19 Pandemic: A Retrospective Cohort Study
Authors Hoyer C , Grassl N, Bail K, Stein P, Ebert A , Platten M , Szabo K
Received 25 July 2020
Accepted for publication 28 August 2020
Published 30 September 2020 Volume 2020:16 Pages 2221—2227
DOI https://doi.org/10.2147/NDT.S273913
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Roger Pinder
Carolin Hoyer, Niklas Grassl, Kathrin Bail, Patrick Stein, Anne Ebert, Michael Platten, Kristina Szabo
Department of Neurology, Medical Faculty Mannheim and Mannheim Center for Translational Neurosciences (MCTN), Heidelberg University, Mannheim, Germany
Correspondence: Carolin Hoyer
Department of Neurology, University Medical Centre Mannheim, Medical Faculty Mannheim, Heidelberg University, Theodor-Kutzer-Ufer 1-3, 68 167 Mannheim, Germany
Tel +49-621-383-5268
Fax +49-621-383-3807
Email [email protected]
Objective: To analyse the characteristics of patients with neurological complaints seeking evaluation in an interdisciplinary emergency department (ED) during the rise of the COVID-19 pandemic in Germany.
Methods: In this retrospective study, data on the number of ED presentations due to neurological complaints in weeks 1– 15/2020 were collected. In addition, hospital chart data of patients referred for neurological evaluation during weeks 12– 15/2020 when the pandemic began impacting on public life in Germany were analysed regarding demographic information, chief complaints, modes of presentation and disposition and ED discharge diagnosis. Both data sets were compared to respective periods from 2017.
Results: During the surge of COVID-19, we found a significant decrease of the total number of neurological ED patients by 47.6%. Comparing weeks 12– 15 of 2017 and 2020, we found a decrease in the number of patients of < 30 years (p< 0.001) and an increase of those 70 years (p< 0.001). A higher proportion of patients were admitted to escalated care (p=0.03), and fewer patients were discharged against medical advice (p< 0.001). In addition, the ratio of less acute diagnoses (eg, benign headaches) declined significantly.
Conclusion: Our findings suggest that the pandemic has contributed to a – potentially transient – reframing of laypeople’s perception of urgency and necessity for emergency presentation. The establishment and promotion of health-care structures and services like telemedical consultations and the creation of safe ED environments will be essential to enable adequate delivery of care in potential future waves of the pandemic.
Keywords: pandemics, COVID-19, emergency neurology
Introduction
The ongoing COVID-19 pandemic poses novel challenges to health-care systems worldwide. Neurologists are affected in many ways: Disease-associated issues, such as neurological symptoms as the initial manifestation or neurological complications in the course of CoV-SARS2 infection have been identified as relevant aspects of the disease. A completely different observation, however, is the decreasing admission rate for acute neurological disorders, especially acute ischemic stroke that has been reported in temporal association with the pandemic and lockdown measures.1,2 A decline in emergency department (ED) presentations during the pandemic has also been reported in several countries and across different disciplines.3–6 In contrast, pre-COVID-19 assessments have documented a constant rise in the number of patients seeking evaluation and treatment in ED due to neurological symptoms. Neurological patients account for up to 15% of ED admissions in Germany and up to 26% of medical patients in general.7–9
Here we analysed the characteristics of patients presenting with neurological complaints to an interdisciplinary ED during the rise of the COVID-19 pandemic in Germany and compared these to data from a control cohort during the same weeks of the year 2017. These data will provide important insights required to tailor the emergency care for neurological patients in the context of the pandemic and beyond.
Methods and Materials
Study Population and Design
We retrospectively analysed data from patients who consecutively presented or were referred to the interdisciplinary ED for neurological assessment of the University Medical Centre, Mannheim, Germany, between January 2nd, 2017, and April 16th, 2017 (calendar weeks 1–15), and between January 1st, 2020, and April 12th, 2020 (calendar weeks 1–15). Cases were identified by filtering the ED database for patients coded to present with a chief complaint that was evaluated by emergency medical service or ED staff upon arrival to be a neurological symptom or complaint. For weeks 1–15 of each year, absolute numbers of patients presenting to the ED were collected. The year 2017 was chosen because data from ED patients of that year were fully and readily available, allowing for a rapid and timely comparative analysis with the COVID-19 epoch in 2020. It is important to note that there were no structural or organizational differences regarding the prehospital assessment by emergency medical services or ED processes and care between the years 2017 and 2020.
For weeks 12–15, analysed data included basic demographic characteristics (age, gender), chief complaint,10 modes of presentation and disposition as well as ED discharge diagnosis.11 Week 12, beginning March 16, 2020, was defined as the week when the COVID-19 pandemic began to impact public life in Germany. Extended measures for social distancing, for example, through closure of schools or daycare institutions and partial lock-down in all German federal states, were implemented beginning March 16, 2020, and were strongly advocated by the German Chancellor in her television address on March 18, 2020.
In the Mannheim adult interdisciplinary ED, at least one neurology resident is present 24/7 either for first-line assessment if prehospital assessment or evaluation on arrival suggests a neurological condition or second-line if first-line assessment by a non-neurologist ED physician suggests a neurological condition.
Statistical Analysis
Calendar weeks 1 to 11 and 12 to 15 were categorized into a variable epoch for the years 2017 and 2020. Poisson regression was used to test whether the rate of events (ED presentations due to neurological symptoms) changed as a function of year (2017 vs 2020), epoch (weeks 1–11, early; weeks 12–15, late), and the interaction of year and epoch (reflecting the impact of the COVID-19 pandemic). This effect is expressed as an incidence rate ratio (IRR) along with its two-sided 95% confidence interval. For the covariance matrix, a robust estimator was chosen to account for possible overdispersion.
Distributions of continuous variables between groups were compared with Student’s t-test or Mann–Whitney U-test for independent samples, and distributions of categorial variables were compared using chi-square test or Fisher’s exact test, depending on group sizes. In addition to p-values, effect sizes and corresponding 95% confidence intervals (CI) are reported as Cohen’s d or as odds ratio (OR), depending on the type of the dependent variables. Statistical analysis was performed with IBM SPSS Statistics 25.0 and STATA for Macintosh, StataCorp 2017.
Results
In calendar week 1–15 of 2017, a total of 1511 patients presented with neurological symptoms to the ED, while in calendar weeks 1–15 of 2020, there were 1403 neurological ED patients. Patient numbers in the early epochs of 2017 and 2020 were 977 and 1069, respectively, while in late epochs of 2017 and 2020, 424 and 238 patients presented for neurological evaluation. Between early (weeks 1–11) and late (weeks 12–15) investigational periods in 2017 and 2020, a significant decrease by 47.6% (IRR 0.524, 95% CI 0.434–0.631, p<0.001) of the total number of patients presenting for neurological evaluation was noted (Figure 1).
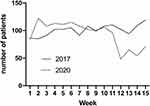 |
Figure 1 Numbers of neurological ED patients during calendar weeks 1–15 of 2017 and 2020. |
When comparing weeks 12–15 of 2017 vs 2020, a significant age difference between the patient samples was found (Table 1), to which both a significant decrease in the number of patients of under 30 years of age (2017: 18.9% vs 2020: 8.8%, OR 0.42 (95% CI 0.24–0.70), p<0.001) and a significant increase of those 70 years and older (2017: 31.8% vs 2020: 47.5%, OR 1.81 (95% CI 1.29–2.54), p<0.001) contributed (Figure 2).
 |
Table 1 Characteristics of the Study Population |
 |
Figure 2 Age distribution of neurological ED patients in calendar weeks 12–15 of 2017 and 2020. |
Regarding modes of presentation, significantly fewer patients were self-presenting in week 12–15 of 2020 (21.8%) when compared to the respective period in 2017 (43.4%, OR 0.36 (95% CI 0.25–0.53), p<0.001). At the same time, the proportion of patients transported to the ED by emergency medical service increased from 44.8% in weeks 12–15 of 2017 to 66.8% in weeks 12–15 of 2020 (OR 2.48 (95% CI 1.76–3.50), p<0.001; Figure 3A).
 |
Figure 3 ED admission (Left) and disposition (Right) modes during calendar weeks 12–15 of 2017 and 2020. |
In the late epoch of 2020, a significantly higher proportion of patients (34.5%) was admitted to escalated care (stroke unit/intermediate care unit/intensive care unit) than in the late epoch of 2017 (26.2%, OR 1.45 (95% CI 1.01–2.08), p=0.03). In contrast, fewer patients were discharged against medical advice in the investigational period of 2020 (0%) than in 2017 (4.5%, OR 0.0 (95% CI 0–0.34), p<0.001; Figure 3B).
The spectrum of chief complaints is presented in Table 1. In the investigational period in 2020, significantly more presentations due to seizures and motor deficits were noted, whereas the number of patients presenting due to headache and visual disturbance decreased.
Two important differences regarding the spectrum of ED discharge diagnoses between the 2017 and 2020 investigational periods were found: The ratio of patients diagnosed with migraines and other types of headaches was significantly lower in 2020 as well as the ratio of patients diagnosed with “other neurological diagnoses”, while an increase of diagnoses with cerebrovascular ischemic events and non-neurological conditions occurred in 2020 (Table 1).
Discussion
In a retrospective analysis of ED patient presentations due to neurological complaints, we observed shifts of age, complaint and diagnostic spectra alongside a dramatic reduction of the overall number of patients during a time when the COVID-19 pandemic had begun to impact on public life in Germany.
Various investigations across several countries and disciplines have highlighted a decrease of ED admissions due to serious medical conditions such as stroke or myocardial infarction.1,2,12,13 Corroborating data from general ED populations,14,15 we found significant changes at either end of the age spectrum as well as changes related to presenting chief complaints and subsequent ED discharge diagnoses. While a direct impact of school closures and social distancing measures on the number of paediatric emergency presentations – in particular, due to lower numbers of admissions for diseases with airborne or oral-faecal modes of transmission16 – could be assumed, reasons for our observation in an adult population are not as straightforward but require a contextualization with additional information: ED admissions due to headache as well as final ED diagnoses of migraine and other types of headache decreased during the COVID-19 epoch. The majority of patients presenting to EDs with headache receive a diagnosis of primary benign headache and usually belong to younger age segments.17,18 Similarly, the number of presentations due to visual disturbances, a broad term covering a wide range of manifestations from blurred vision to symptoms indicating potentially serious pathology such as amaurosis fugax or hemianopia, also decreased. In our ED, there is no clear-cut a priori distinction as to whether patients are referred to the ED neurologist or the hospital’s ophthalmological emergency service. Studies on ophthalmological emergency presentations identified a substantial number of non-urgent ED visits in this patient population with an association of non-urgent reasons for visits with younger age.19,20
In contrast, the ratio of presentations due to motor deficits and ED discharge diagnoses of cerebrovascular ischemic events was significantly more frequent during the COVID epoch in 2020. While prior studies had identified a collateral effect of the COVID-19 pandemic on stroke admissions, in particular on patients presenting with transient, mild or moderate stroke symptoms1,2 as well as the utilization of reperfusion manoeuvres during the pandemic,12,21,22 they did not consider the overall composition of neurological ED admissions. Our finding implies that those patients who did eventually come to the ED were seriously affected, which is also underscored by the fact that a larger percentage of patients had to be admitted to escalated care in the COVID-19 epoch. Significantly fewer patients were discharged against medical advice, which may be mediated by the change in age spectrum23 with a predominance of younger patients leaving against medical advice and the relative paucity of presentations due to headache, a complaint frequent among DAMA patients in general ED populations as well as in the neurological ED clientele.9,24
Previous investigations have found that a large proportion of patients presenting to EDs with neurological symptoms does ultimately not require hospitalization11 and patients’ self-assessment of urgency is strikingly different from the result of a professional evaluation.25 The clinical relevance of neurological complaints thus appears to be difficult to assess for patients and non-neurologists, so prehospital care providers’ safety thinking may lead them to allocate patients to the ED for immediate neurological assessment even with benign conditions.26 Since there is no reason to assume that the prevalence of symptoms like headache has decreased during the pandemic – if anything, headache could occur more frequently as it has been described as a manifesting symptom of CoV-SARS2 infection27 – one may hypothesize that the pandemic has contributed to a – potentially transient – reframing of urgency and necessity for emergency neurological assessment particularly in younger individuals with non-urgent complaints and patients with transient or less impairing symptoms. High levels of perceived threat by COVID-1928 and concomitant fear of in-hospital infection29 as well as the adherence to stay-at-home orders alongside a reduction of general population mobility may be contributing factors. Theoretically, improved public knowledge about serious vs non-serious symptoms could be confounding the results. However, this is rather unlikely because there are no campaigns targeted at increasing public awareness about this specific aspect. It also bears mentioning that neurological signs and symptoms are often non-specific – even transient or subtle symptoms may be indicative of serious underlying pathologies but may be difficult for non-neurological medical professionals to recognize.30 Finally, the effects of public educational programs, which are mainly targeted at the recognition of stroke symptoms, have brought about only modest changes.31,32
It would have been desirable to analyse a longer time-period so as to allow for an assessment during later stages of the pandemic as well as to obtain data from multiple sites. In addition, an investigation into patients’ motivations to come to the ED – and reasons to avoid doing so – as well as potential COVID-19-related concerns and fears in the context of an ED presentation would be informative in order to gain a deeper understanding of changes of health-related behaviours during the COVID-19 pandemic.
In sum, we identified a shift towards an older patient population that is more severely affected with serious conditions in patients presenting with neurological complaints during the COVID-19 pandemic in a German ED. We assume an underlying complex interplay of individual and societal factors during the pandemic, causing a temporary re-calibration of perceived sense of need for an emergency work-up of neurological complaints particularly in younger patients. Given the difficulties in properly assessing the relevance of neurological complaints, it is paramount to establish health-care structures and services like telemedical consultations, to create safe ED environments and to inform the public about these strategies so as to enable adequate delivery of care during potential future waves of the pandemic.
Data Sharing Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The study protocol has been approved by the Ethics Committee II, Medical Faculty Mannheim, Heidelberg University, reference number 2018-502N-MA, and has been performed with ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Due to the retrospective design and lack of study-related interventions, written informed consent was waived. All patient data accessed for the purposes of this investigation complied with relevant data protection and privacy regulations.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work. Carolin Hoyer and Niklas Grassl contributed equally to the manuscript.
Funding
CH receives funding within the Olympia Morata Program of Heidelberg University. CH and KS receive funding within the Sonderförderlinie COVID-19 Forschung of the federal state Baden-Württemberg.
Disclosure
Dr Carolin Hoyer reports grants from the Olympia Morata Programme of Heidelberg University, grants from Sonderfördermaßnahme COVID-19 Forschung, during the conduct of the study. Prof. Dr. Kristina Szabo reports grants from Sonderfördermaßnahme COVID-19 Forschung, during the conduct of the study. The authors report no other potential conflicts of interest for this work.
References
1. Hoyer C, Ebert A, Huttner HB, et al. Acute stroke in times of the COVID-19 pandemic: a multicenter study. Stroke. 2020:STROKEAHA120030395.
2. Diegoli H, Magalhaes PSC, Martins SCO, et al. Decrease in hospital admissions for transient ischemic attack, mild, and moderate stroke during the COVID-19 era. Stroke. 2020:STROKEAHA120030481.
3. Dann L, Fitzsimons J, Gorman KM, Hourihane J, Okafor I. Disappearing act: COVID-19 and paediatric emergency department attendances. Arch Dis Child. 2020;105(8):810–811. doi:10.1136/archdischild-2020-319654
4. Hoyer C, Ebert A, Szabo K, Platten M, Meyer-Lindenberg A, Kranaster L. Decreased utilization of mental health emergency service during the COVID-19 pandemic. Eur Arch Psychiatry Clin Neurosci. 2020. doi:10.1007/s00406-020-01151-w
5. Baum A, Schwartz MD. Admissions to veterans affairs hospitals for emergency conditions during the COVID-19 pandemic. JAMA. 2020;324(1):96. doi:10.1001/jama.2020.9972
6. Bjornsen LP, Naess-Pleym LE, Dale J, Laugsand LE. Patient visits to an emergency department in anticipation of the COVID-19 pandemic. Tidsskr nor Laegeforen. 2020;140(8).
7. Topka H, Pfefferkorn T, Andres F, et al. [Online survey of the organizational structures of emergency neurology in Germany]. Nervenarzt. 2017;88(6):625–634. doi:10.1007/s00115-017-0343-x
8. Steiner D, Renetseder F, Kutz A, et al. Performance of the manchester triage system in adult medical emergency patients: a prospective cohort study. J Emerg Med. 2016;50(4):678–689. doi:10.1016/j.jemermed.2015.09.008
9. Hoyer C, Stein P, Alonso A, Platten M, Szabo K. Uncompleted emergency department care and discharge against medical advice in patients with neurological complaints: a chart review. BMC Emerg Med. 2020;324(1):52. doi:10.1186/s12873-019-0273-y
10. Royl G, Ploner CJ, Mockel M, Leithner C. [Neurological chief complaints in an emergency room]. Nervenarzt. 2010;81(10):1226–1230. doi:10.1007/s00115-010-3020-x
11. Rizos T, Juttler E, Sykora M, Poli S, Ringleb PA. Common disorders in the neurological emergency room–experience at a tertiary care hospital. Eur J Neurol. 2011;18(3):430–435. doi:10.1111/j.1468-1331.2010.03170.x
12. Rudilosso S, Laredo C, Vera V, et al. Acute stroke care is at risk in the era of COVID-19: experience at a comprehensive stroke center in Barcelona. Stroke. 2020:STROKEAHA120030329.
13. Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75(22):2871–2872. doi:10.1016/j.jacc.2020.04.011
14. Comelli I, Scioscioli F, Cervellin G. Impact of the COVID-19 epidemic on census, organization and activity of a large urban emergency department. Acta Biomed. 2020;91(2):45–49.
15. Hartnett KP, Kite-Powell A, DeVies J, et al. Impact of the COVID-19 pandemic on emergency department visits — United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704. doi:10.15585/mmwr.mm6923e1
16. Angoulvant F, Ouldali N, Yang DD, et al. COVID-19 pandemic: impact caused by school closure and national lockdown on pediatric visits and admissions for viral and non-viral infections, a time series analysis. Clin Infect Dis. 2020. doi:10.1093/cid/ciaa710
17. Chu KH, Howell TE, Keijzers G, et al. Acute headache presentations to the emergency department: a statewide cross-sectional study. Acad Emerg Med. 2017;24(1):53–62. doi:10.1111/acem.13062
18. Doretti A, Shestaritc I, Ungaro D, et al. Headaches in the emergency department -a survey of patients’ characteristics, facts and needs. J Headache Pain. 2019;20(1):100. doi:10.1186/s10194-019-1053-5
19. Stagg BC, Shah MM, Talwar N, Padovani-Claudio DA, Woodward MA, Stein JD. Factors affecting visits to the emergency department for urgent and nonurgent ocular conditions. Ophthalmology. 2017;124(5):720–729. doi:10.1016/j.ophtha.2016.12.039
20. Channa R, Zafar SN, Canner JK, Haring RS, Schneider EB, Friedman DS. Epidemiology of eye-related emergency department visits. JAMA Ophthalmol. 2016;134(3):312–319. doi:10.1001/jamaophthalmol.2015.5778
21. Teo KC, Leung WCY, Wong YK, et al. Delays in stroke onset to hospital arrival time during COVID-19. Stroke. 2020:STROKEAHA120030105.
22. Pop R, Quenardelle V, Hasiu A, et al. Impact of the COVID-19 outbreak on acute stroke pathways - insights from the Alsace region in France. Eur J Neurol. 2020;27(9):1783–1787. doi:10.1111/ene.14316
23. Lee CA, Cho JP, Choi SC, Kim HH, Park JO. Patients who leave the emergency department against medical advice. Clin Exp Emerg Med. 2016;3(2):88–94. doi:10.15441/ceem.15.015
24. Ding R, Jung JJ, Kirsch TD, Levy F, McCarthy ML. Uncompleted emergency department care: patients who leave against medical advice. Acad Emerg Med. 2007;14(10):870–876. doi:10.1197/j.aem.2007.06.027
25. Harenberg L, Osswald HM, Jaschonek H, Nagel S. [Self-assessment of treatment urgency on presentation to a neurological emergency department: results of a patient survey]. Nervenarzt. 2019;90(2):175–182. doi:10.1007/s00115-018-0623-0
26. Moeller JJ, Kurniawan J, Gubitz GJ, Ross JA, Bhan V. Diagnostic accuracy of neurological problems in the emergency department. Can J Neurol Sci. 2008;35(3):335–341. doi:10.1017/S0317167100008921
27. Bolay H, Gul A, Baykan B. COVID-19 is a real headache! Headache. 2020;60(7):1415–1421. doi:10.1111/head.13856
28. Teufel M, Schweda A, Dorrie N, et al. Not all world leaders use Twitter in response to the COVID-19 pandemic: impact of the way of Angela Merkel on psychological distress, behaviour and risk perception. J Public Health. 2020;42(3):644–646. doi:10.1093/pubmed/fdaa060
29. Wong LE, Hawkins JE, Langness S, Murrell KL, Iris P, Sammann A. Where are all the patients? Addressing Covid-19 fear to encourage sick patients to seek emergency care. NEJM Catalyst. 2020.
30. Newman-Toker DE, Moy E, Valente E, Coffey R, Hines AL. Missed diagnosis of stroke in the emergency department: a cross-sectional analysis of a large population-based sample. Diagnosis. 2014;1(2):155–166. doi:10.1515/dx-2013-0038
31. Rau R, Mensing M. Evaluation der Public-Health-Intervention “Gesunder Niederrhein … gegen den Schlaganfall” durch Telefonbefragungen. Med Klin. 2009;104(10):799–805.
32. Worthmann H, Schwartz A, Heidenreich F, et al. Educational campaign on stroke in an urban population in Northern Germany: influence on public stroke awareness and knowledge. Int J Stroke. 2013;8(5):286–292. doi:10.1111/j.1747-4949.2012.00809.x
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
