Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 14
Changes in COPD inhaler prescriptions in the United Kingdom, 2000 to 2016
Authors Bloom CI , Elkin SL, Quint JK
Received 8 October 2018
Accepted for publication 28 December 2018
Published 22 January 2019 Volume 2019:14 Pages 279—287
DOI https://doi.org/10.2147/COPD.S190086
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Chloe I Bloom,1 SL Elkin,2 JK Quint1
1National Heart and Lung Institute, Imperial College London, London SW3 6LR, UK; 2Department of Respiratory Medicine, Imperial College NHS Trust, London, UK
Background: Over the past two decades, there have been significant changes in the pharmacological management of COPD, due to an explosion of inhaler trials, and timely updation of national and international guidelines. We sought to describe temporal changes in prescribing practices in the United Kingdom, and some of the factors that may have influenced them.
Patients and methods: COPD patients were identified from UK primary care nationally representative electronic healthcare records (Clinical Practice Research Datalink), between 2000 and 2016. Prescription data were described by the three maintenance inhaled medication classes used, inhaled corticosteroids (ICS), long-acting beta agonist (LABA), long-acting muscarinic antagonist (LAMA), and their combinations, dual LABA-ICS, dual LAMA-LABA, or triple therapy LABA-ICS-LAMA. Differing patient characteristics across the six different therapy regimens were measured in 2016.
Results: COPD patients were identified: 187,588 prevalent and incident inhaler users and 169,511 incident inhaler users. Since 2002, LAMA showed increasing popularity, while ICS alone exhibited an inverse trend. Triple therapy prescriptions rapidly increased as the first-line therapy until 2014 when LAMA-LABA prescriptions started to increase. By 2014, 41% of all COPD patients were maintained on triple therapy, and 13% were maintained on LAMA only. Characterizing the patients in 2016 revealed that those on triple therapy were more likely to have more severe disease, yet, over a third of patients on triple therapy had only mild disease.
Conclusion: UK prescribing practices were not in keeping with national guidelines but did appear to align with evidence from major drug trials and updated international guidelines. There has been a huge upsurge in triple therapy but incident data show this trend is beginning to reverse for initial management.
Keywords: COPD, inhalers, UK, prescriptions, electronic healthcare records
Introduction
The global prevalence of COPD is estimated to be around 200 million patients.1 In the United Kingdom, it is estimated that there are over 1.2 million people living with COPD.2 The mainstay of treatment is long-term inhaled medication, requiring up to three different inhaled medication classes depending on disease severity, but the evidence for the most effective medication class depends on many factors, and has been constantly updated due to the proliferation of drug trials over the past two decades.
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) has been developing international guidelines for COPD since 1997, including an algorithm for pharmacological management of stable disease. The international committee of experts regularly reviews the latest evidence and updates the guideline; the latest one was in 2017.3 The algorithm has therefore evolved over time, with increasing emphasis on patient’s symptoms, now assessed using either the COPD Assessment Test score or the Modified British Medical Research Council (MRC) score. Patients must also have an assessment of airflow limitation and record their exacerbation history. The United Kingdom also has its own guidelines and multidimensional treatment algorithm, devised by the National Institute for Health and Care Excellence (NICE).4 The first NICE COPD guideline was published in 2004 (prior to that the British Thoracic Society-produced guidelines) and the latest one was published in 2010. Due to the length of time since the latest guidelines, and the continuous updates in our understanding of how best to manage COPD, it is probable that physicians refer to the more updated GOLD guidelines. However, despite the availability of both national and international guidelines, real-world data suggest that patients are not managed according to their recommendations.5–8
The aim of this study was to describe the temporal pattern of inhaler prescriptions for people with COPD since the millennium. In the United Kingdom, nearly all COPD patients have their medication prescribed within primary care; therefore, we used representative primary care electronic healthcare records between 2000 and 2016. We also wanted to understand if there were differences in the characteristics of people prescribed the different medication classes, and if these were in keeping with the guidelines at that time.
Patients and methods
Data source
We used the Clinical Practice Research Database (CPRD-GOLD) as this is a national representative database of deidentified electronic healthcare records. It contains information on clinical diagnoses, prescriptions, and test results on more than 11 million patients, from over 670 GP practices across the United Kingdom.9 Patients’ data were linked to Hospital Episode Statistics (HES) database, Office of National Statistics (ONS), or Index of Multiple Deprivation (IMD, a socioeconomic marker) when secondary care, mortality, or socioeconomic data were required. HES contains information on all admissions to National Health Service hospitals in England; therefore, only around 60% of all UK practices in CPRD have individual-level linkage to HES, ONS, and IMD.
Study population
All patients included in this study were aged >35 years old, had a history of smoking, had a COPD diagnosis as defined using validated algorithm of clinical codes alone (excluding spirometry),10 and were prescribed inhaled airways medication.
Inhaled medication
Medication regimens included were based on the three medication classes: inhaled corticosteroids (ICS), long-acting beta agonist (LABA), and long-acting muscarinic antagonist (LAMA); combination LABA-ICS or combination LAMA-LABA; or reliever medication class short-acting beta-agonist (SABA). Triple therapy was defined as prescription for all three maintenance medications: LABA, LAMA, and ICS, prescribed as combination and a single component, or three single component inhalers (triple therapy combined in a single inhaler was not available in the United Kingdom during the study time period). Incident inhaler use was defined as inhalers prescribed for COPD patients started for the first time on maintenance medication in that year. Prevalent inhaler use was defined as inhalers prescribed for all COPD patients in the database in that year (thus including prevalent and incident users in that year).
Variables
BMI was measured as kg/m2. COPD severity was classified using GOLD staging classification and the MRC Dyspnea Scale.11,12 Exacerbations, treated within primary care (labeled as moderate) or secondary care (labeled as severe), were identified using a validated algorithm (the algorithm uses a combination of treatment with oral corticosteroids, antibiotics, and codes for exacerbation and symptoms).13,14 Exacerbations recorded within 14 days after the index one were considered part of the same exacerbation. Level of care of each exacerbation was documented as the highest level per episode. Symptom variable included any physician recording of wheeze, dyspnea, or cough (Read codes are available upon request). A history of anxiety, depression, or asthma was recorded using appropriate or validated Read codes (available upon request).15
Statistical analyses
All statistical analyses were performed using STATA 14.2. Data were reported as frequency, percentage, median, or interquartile range. Categorical variables were statistically compared between the different medications classes using chi-squared tests, continuous variables were compared using ANOVA. Level of statistical significance was set at P<0.01.
Ethics
The protocol for this research was approved by the Independent Scientific Advisory Committee (ISAC) for MHRA Database Research (protocol number 18_254R) and the approved protocol was made available to the journal and reviewers during peer review. Generic ethical approval for observational research using the CPRD with approval from ISAC has been granted by a Health Research Authority Research Ethics Committee (East Midlands – Derby, REC reference number 05/MRE04/87). Linked pseudonymized data were provided for this study by CPRD. Data are linked by NHS Digital, the statutory trusted third party for linking data, using identifiable data held only by NHS Digital. Select general practices consent to this process at a practice level with individual patients having the right to opt out.
Results
Number of inhalers prescribed
A vast number of inhalers are prescribed each year for COPD patients (Figure 1). The number of COPD patients fell from 2013 onward due to a change in which practices contribute to CPRD. The total number of SABA prescriptions has paralleled the pattern of the number of COPD patients in the database. Whereas, the number of combination LABA-ICS inhalers increased rapidly after 2004, until around 2012, whereafter they also paralleled the COPD population. The number of single-component LABA and LABA-LAMA combination prescriptions has remained low. However, single-component LAMA prescriptions have increased considerably since their introduction in the United Kingdom in 2002. Single-component ICS were prescribed in low numbers in 2000, and fell even further after 2005.
Pattern of pharmacological disease management
Incident prescriptions
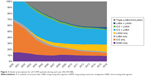
Between 2002 and 2016, 169,511 COPD patients were identified as starting initial maintenance treatment. Since the introduction of LAMA in 2002, the proportion of patients started on LAMA alone in their first year increased hugely (2002: <1%, 2016: 29%; Figure 2), while patients started on an ICS and LABA as the first-line treatment decreased (2002: 38%, 2016: 26%). Patients started on triple therapy increased from 2002 until 2014, after which the percentage dropped (2002: <1%, 2014: 28%, 2016: 22%). The decrease in triple therapy as the first-line treatment seems to parallel the increase in LABA and LAMA as the first-line treatment, as there was an increase from 2% in 2014 to 8% in 2016. By 2016, 9% of COPD patients were still prescribed ICS alone as their first maintenance treatment; of these patients, half had a co-diagnosis of asthma at some point in their records, but half did not.
Prevalent prescriptions
Totally, 187,588 COPD patients were identified as prevalent inhaler users. The pattern of inhaler prescriptions differed between prevalent users (Figure 3) and incident users (Figure 2). There was a steady increase in patients maintained on LAMA alone (2002: 0.1%, 2016: 13%), and patients maintained on triple therapy (2002: 1%, 2016: 41%; Figure 3). The large increase in triple therapy appears to reflect the drop in ICS alone (2002: 40%, 2016: 1%). The proportion maintained on ICS and LABA have also decreased (2007: 37%, 2016: 24%). There has been a slight decrease in patients maintained only on a SABA (2000: 15%, 2016: 9%). Those maintained on a LABA and a LAMA (or a combination LAMA/LABA) have increased (2002: 1%, 2016: 5%).
Patient characteristics by maintenance therapy regimen in 2016
All characteristics differed significantly between the seven possible maintenance therapy regimens (P<0.01, Table 1); however, clinically there was no difference in age or BMI. Females were more often prescribed an ICS containing regimen than males, except for triple therapy which was distributed equally. Patients on triple therapy were more likely to have characteristics of severe disease than those not on triple therapy, in terms of modified Medical Research Council (mMRC) score, GOLD stage, exacerbation frequency, exacerbation severity, and recorded symptoms. Sixty-four percent of patients on the triple regimen fulfilled guideline criteria for offering triple therapy (during 2016 patients had documented sufficient breathlessness, persistent exacerbations, or a severe exacerbation); in the whole cohort, the proportion that fulfilled these criteria was half, patients prescribed that a LAMA-LABA regimen had the next highest percentage (Triple: 64.0%, LABA-LAMA: 49.9%, All: 49.6%; Table 1). Patients prescribed a regimen containing ICS alone or ICS-LABA more frequently had an asthma co-diagnosis than all other regimens (ICS: 52% asthma, ICS-LABA: 46.5% asthma, All: 30.8%). Patients prescribed either LAMA alone, or LABA-LAMA regimen, were more commonly recently diagnosed (2015 or 2016 diagnosis: LAMA =28.4%, LABA-LAMA =28.6%). Patients prescribed the triple regimen were more commonly diagnosed some time ago than patients prescribed all other regimens (<2009: Triple =55.6%, all: 46.6%).
Discussion
Using the world’s largest longitudinal-national database of patients’ healthcare records, we have been able to show the changing temporal pattern of inhaler prescriptions in the United Kingdom’s COPD population. The predominant feature was the rapid increase in prescriptions of triple therapy regimen, since the availability of the first LAMA in 2002.
From the incident prescribing data, it does not appear that NICE guidelines were well adhered to in primary care. This is perhaps not surprising as the NICE guidelines were/are considerably lagging behind the rapidly changing evidence from the vast number of COPD medication trials in the past decade. Since the 1980s, COPD patients have been using the SABA, ipratropium. The subsequent availability of the first LAMA, tiotropium, allowed much more convenient dosing of an inhaled anticholinergic, which coincided with, and may have contributed toward, both the rapid decline in an ICS-alone regimen, thereafter, and the drop in SABA-alone management that occurred in 2003. The steep fall in prescriptions of ICS alone may have also been influenced by the negative ICS trials carried out, in patients with milder COPD, published just before the turn of the century.16,17 Multiple studies, including a Cochrane systematic review, found LAMA alone to be well tolerated, reduced exacerbations, and improved quality of life.18–23 But it was not until the largest COPD treatment study of its time, the randomized controlled trial TORCH, published in 2007, followed closely by the equally large UPLIFT trial published in 2008, that there was strong evidence that regular prolonged use of LAMA was not associated with worsening mortality or adverse cardiovascular events.24,25 Our incident prescribing data seem to suggest that these trials had a significant impact on the United Kingdom’s prescribing habit, as there was a flourish of LAMA-only-treated patients from 2008 onward. In 2010, the NICE guidelines were updated to recommend that all patients, not just those with an FEV1 predicted ≤50%, could be prescribed LAMA alone as the first-line treatment for dyspnea or persistent exacerbations. Although, it is notable that by this time, the steepest incline in prescription of a LAMA-alone regimen had already occurred. Perhaps, because the GOLD guidelines, since 2006, had already recommended first-line one, or more, long-acting bronchodilator for those with an FEV1 predicted <80%.
The landmark TORCH study, and findings from the INSPIRE study published early in 2008, both found an excess of pneumonias in association with combination LABA/ICS,24,26 the timing of which may explain the prompt reduction in a first-line LABA-ICS regimen from 2008 onward. Over 2 years later, this risk was incorporated into the updated NICE guidelines; notably, it had already been included in the 2008 GOLD guidelines.
The changes in incident prescription practice discussed above were not completely mirrored in prevalent prescription practice. This may have been related to the natural progression of the disease necessitating stepping up of patient’s medication, alongside comparatively lower numbers with incident disease. This resulted in a smaller proportion of the total COPD population on LAMA alone and much larger proportion on triple therapy. The prevalent prescriptions of triple therapy plateaued from 2012; in contrast, incident prescriptions dropped in 2015, and continued to decline in 2016. This fall was matched with an increase in LABA-LAMA regimen as the initial maintenance therapy. During 2014, two potentially significant events occurred: firstly, the WISDOM trial published its findings, suggesting that it was safe to withdraw patients on triple regimen from their ICS,27 and secondly, in the United Kingdom, the first LAMA/LABA combination inhaler became available. But it was only the later event that was likely to have influenced incident prescribing practices. Findings from WISDOM, and other supporting studies,28,29 did not appear to have a significant effect on prevalent inhaler use; however, data beyond 2016 may show a changing trend.
Reassuringly, the patients in 2016 who were prescribed triple therapy did have more severe disease; they were more likely to have a higher GOLD stage, higher mMRC score, higher total number of exacerbations, and more severe exacerbations. However, there was still a considerable proportion of patients with mild disease who were on triple therapy; over a third of patients on triple therapy did not meet NICE or GOLD guideline criteria recommendations. As would be expected, those with a regimen including an ICS were most likely to have a co-diagnosis of asthma; this may also explain why females were more likely to be prescribed an ICS. Patients solely prescribed long-acting bronchodilators had the highest proportion with recently diagnosed disease, likely reflecting both the more recent recommendation to prescribe these as first-line treatments and the earlier stage of disease. In reverse, those with a longer disease history were far more likely to be prescribed triple therapy.
The main strengths of this study are the size of the population included, longevity of their follow-up, and the accuracy and completeness of prescription records. Study limitations to be considered are the lack of information on prescription dispensing, or adherence to medication, although as the main focus of the study was on prescribing practice, these limitations would only have had a mild impact. There were also some missing data when describing patients, particularly affecting the GOLD stage variable.
Conclusion
The availability of an inhaled LAMA since 2002 made a large impact on the management of COPD patients in the United Kingdom, including the enthusiastic adoption of triple therapy, which appears to have replaced the inappropriate prescribing of ICS alone. More recently, triple therapy use has plateaued and encouragingly incident data showed a decline, while prescribing LAMA as initial maintenance therapy has continued to grow. Overall, there appeared little adherence to the United Kingdom’s COPD guidelines, but prescribing practice did seem to be roughly in alliance with international GOLD guidelines and the latest drug trial evidence, probably, reflecting the extended time between updated NICE COPD guidelines and the rapidly evolving pharmacological evidence. Prescribing practices will continue to modify, including due to the developing evidence on the effectiveness of triple therapy, recent availability of combination LAMA/LABA/ICS inhalers, increasing availability of daily dose inhalers, as well as updates in national and international guidelines; real-world data will continue to be instrumental in capturing the response to these changes.
Disclosure
Dr Bloom has no conflict of interest. Dr Elkin has received speaker fees from AZ, Chiesi, and Pfizer in the last 3 years. Dr Quint, outside the submitted work, reports grants from The Health Foundation, MRC, British Lung Foundation, grants and personal fees from GlaxoSmithKline, Boehringer Ingelheim, AstraZeneca, Insmed, and Bayer, personal fees from Chiesi and Teva, and grants from IQVIA. The authors report no other conflicts of interest in this work.
References
GBD 2015 Chronic Respiratory Disease Collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the global burden of Disease Study 2015. Lancet Respir Med. 2017;5(9):691–706. | ||
Snell N, Strachan D, Hubbard R, Gibson J, Gruffydd-Jones K, Jarrold I. S32 Epidemiology of chronic obstructive pulmonary disease (COPD) in the UK: findings from the British Lung Foundation’s ‘Respiratory Health of the Nation’ project. Thorax. 2016;71(Suppl 3):A20. | ||
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease 2018. Available from: https://goldcopd.org/wp-content/uploads/2017/11/GOLD-2018-v6.0-FINAL-revised-20-Nov_WMS.pdf. Accessed January 15, 2019. | ||
National Institute for Health and Care Excellence. Chronic obstructive pulmonary disease in over 16s: diagnosis and management; 2010. Available from: https://www.nice.org.uk/guidance/cg101. Accessed January 15, 2019. | ||
Wurst KE, Shukla A, Muellerova H, Davis KJ. Respiratory pharmacotherapy use in patients newly diagnosed with chronic obstructive pulmonary disease in a primary care setting in the UK: a retrospective cohort study. COPD. 2014;11(5):521–530. | ||
Chalmers JD, Tebboth A, Gayle A, Ternouth A, Ramscar N. Determinants of initial inhaled corticosteroid use in patients with GOLD A/B COPD: a retrospective study of UK general practice. NPJ Prim Care Respir Med. 2017;27(1):43. | ||
Price D, West D, Brusselle G, et al. Management of COPD in the UK primary-care setting: an analysis of real-life prescribing patterns. Int J Chron Obstruct Pulmon Dis. 2014;9:889–904. | ||
Brusselle G, Price D, Gruffydd-Jones K, et al. The inevitable drift to triple therapy in COPD: an analysis of prescribing pathways in the UK. Int J Chron Obstruct Pulmon Dis. 2015;10:2207–2217. | ||
Herrett E, Gallagher AM, Bhaskaran K, et al. Data resource profile: clinical Practice Research Datalink (CPRD). Int J Epidemiol. 2015;44(3):827–836. | ||
Quint JK, Müllerova H, Disantostefano RL, et al. Validation of chronic obstructive pulmonary disease recording in the clinical Practice Research Datalink (CPRD-GOLD). BMJ Open. 2014;4(7):e005540–e005540. | ||
Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the medical Research Council (MRC) Dyspnoea Scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54(7):581–586. | ||
Rabe KF, Hurd S, Anzueto A, et al; Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: gold executive summary. Am J Respir Crit Care Med. 2007;176(6):532–555. | ||
Rothnie KJ, Müllerová H, Thomas SL, et al. Recording of hospitalizations for acute exacerbations of COPD in UK electronic health care records. Clin Epidemiol. 2016;8:771–782. | ||
Rothnie KJ, Müllerová H, Hurst JR, et al. Validation of the recording of acute exacerbations of COPD in UK primary care electronic healthcare records. PLoS One. 2016;11(3):e0151357. | ||
Nissen F, Morales DR, Mullerova H, Smeeth L, Douglas IJ, Quint JK. Validation of asthma recording in the clinical Practice Research Datalink (CPRD). BMJ Open. 2017;7(8):e017474. | ||
Vestbo J, Sørensen T, Lange P, Brix A, Torre P, Viskum K. Long-term effect of inhaled budesonide in mild and moderate chronic obstructive pulmonary disease: a randomised controlled trial. Lancet. 1999;353(9167):1819–1823. | ||
Pauwels RA, Löfdahl CG, Laitinen LA, et al. Long-term treatment with inhaled budesonide in persons with mild chronic obstructive pulmonary disease who continue smoking. N Engl J Med. 1999;340(25):1948–1953. | ||
O’Donnell DE, Flüge T, Gerken F, et al. Effects of tiotropium on lung hyperinflation, dyspnoea and exercise tolerance in COPD. Eur Respir J. 2004;23(6):832–840. | ||
Casaburi R, Mahler DA, Jones PW, et al. A long-term evaluation of once-daily inhaled tiotropium in chronic obstructive pulmonary disease. Eur Respir J. 2002;19(2):217–224. | ||
Barr RG, Bourbeau J, Camargo CA, Ram FS. Inhaled tiotropium for stable chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2005 (2):CD002876. | ||
Casaburi R, Briggs DD Jr, Donohue JF, Serby CW, Menjoge SS, Witek TJ. The spirometric efficacy of once-daily dosing with tiotropium in stable COPD: a 13-week multicenter trial. The US tiotropium Study Group. Chest. 2000;118(5):1294–1302. | ||
Littner MR, Ilowite JS, Tashkin DP, et al. Long-acting bronchodilation with once-daily dosing of tiotropium (Spiriva) in stable chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000;161(4 Pt 1):1136–1142. | ||
Niewoehner DE, Rice K, Cote C, et al. Prevention of exacerbations of chronic obstructive pulmonary disease with tiotropium, a once-daily inhaled anticholinergic bronchodilator: a randomized trial. Ann Intern Med. 2005;143(5):317–326. | ||
Calverley PM, Anderson JA, Celli B, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007;356(8):775–789. | ||
Tashkin DP, Celli B, Senn S, et al; UPLIFT Study Investigators. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med. 2008;359(15):1543–1554. | ||
Wedzicha JA, Calverley PM, Seemungal TA, et al; INSPIRE Investigators. The prevention of chronic obstructive pulmonary disease exacerbations by salmeterol/fluticasone propionate or tiotropium bromide. Am J Respir Crit Care Med. 2008;177(1):19–26. | ||
Magnussen H, Disse B, Rodriguez-Roisin R, et al; WISDOM Investigators. Withdrawal of inhaled glucocorticoids and exacerbations of COPD. N Engl J Med. 2014;371(14):1285–1294. | ||
Rossi A, Guerriero M, Corrado A; OPTIMO/AIPO Study Group. Withdrawal of inhaled corticosteroids can be safe in COPD patients at low risk of exacerbation: a real-life study on the appropriateness of treatment in moderate COPD patients (OPTIMO). Respir Res. 2014;15:77. | ||
Rossi A, van der Molen T, del Olmo R, et al. Instead: a randomised switch trial of indacaterol versus salmeterol/fluticasone in moderate COPD. Eur Respir J. 2014;44(6):1548–1556. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.