Back to Journals » Clinical Interventions in Aging » Volume 13
CHA2DS2-VASc score as a predictor of long-term cardiac outcomes in elderly patients with or without atrial fibrillation
Authors Xing Y , Sun Y, Li H, Tang M , Huang W, Zhang K, Zhang D , Zhang D , Ma Q
Received 1 August 2017
Accepted for publication 21 December 2017
Published 29 March 2018 Volume 2018:13 Pages 497—504
DOI https://doi.org/10.2147/CIA.S147916
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Yunli Xing, Ying Sun, Hongwei Li, Mei Tang, Wei Huang, Kan Zhang, Dai Zhang, Deqiang Zhang, Qing Ma
Department of Geriatrics and Gerontology, Beijing Friendship Hospital, Capital Medical University, Beijing, People’s Republic of China
Background: The CHA2DS2-VASc score is often used for stroke risk stratification in atrial fibrillation (AF) patients. However, its usefulness in patients ≥75 years of age with or without AF is unclear.
Objective: We aimed to investigate whether the CHA2DS2-VASc score can predict ischemic stroke (IS), transient ischemic attack, thromboembolism (TE), and mortality in elderly patients with and without AF.
Materials and methods: During 2013–2014, 1,071 patients (36.3% with concomitant AF) at least 75 years old were enrolled, and the follow-up ended on July 15, 2017. Variables included sociodemographic characteristics, complications, drugs taken, laboratory results, and echocardiographic parameters. The primary end points were IS, transient ischemic attack, and TE, expressed as IS/TE. All-cause mortality was a secondary end point. Survival curves and mortality risks were assessed via Kaplan–Meier survival analysis and compared by log-rank tests.
Results: The average follow-up duration was 2.57±1.37 years. Overall, 167 patients (5.6%) died and 77 (7.2%) developed IS/TE. The CHA2DS2-VASc score was associated with IS/TE in patients 75 years or older with and without AF, and patients with a CHA2DS2-VASc score ≥5 had a higher risk of stroke. However, the CHA2DS2-VASc score was not related to all-cause mortality.
Conclusion: The CHA2DS2-VASc score can predict IS/TE, but not mortality, in elderly patients (≥75 years) with or without AF.
Keywords: CHA2DS2-VASc score, atrial fibrillation, elderly, stroke, survival
Introduction
Age is associated with increased risks of stroke and mortality in patients with either atrial fibrillation (AF) or sinus rhythm.1 Measures to identify individuals with an elevated risk of stroke would facilitate the early application of prevention strategies, and thus, reliable stroke risk prediction schemes are urgently needed.
The CHA2DS2-VASc (congestive heart failure, hypertension, age ≥75 years [double score], diabetes, prior stroke or transient ischemic attack [TIA; double score], vascular disease, age 65–74 years, sex class [female]) scoring system has gained prominent status as a key prediction tool for stroke risk stratification in patients with AF.2 In recent years, the value of the CHA2DS2-VASc score for predicting ischemic stroke (IS) and mortality has been shown to extend beyond the original field to heart failure and myocardial infarction.3–5 In this study, we hypothesized that the CHA2DS2-VASc score can also predict IS and mortality in elderly patients with or without AF.
Materials and methods
A retrospective study was conducted by enrolling consecutive patients aged 75 years or older at Beijing Friendship Hospital between January 1, 2013 and December 31, 2014. The data for all individual patients could be retrieved as all data at our hospital are linked to a unique permanent registration number. Diagnosis of AF was based on electrocardiography, 24-hour Holter monitoring, or the patient’s medical history of AF.6,7 We excluded patients with mechanical prosthetic heart valves, pulmonary embolism, or recent deep vein thrombosis and intraventricular thrombus. Patients who had been on oral anticoagulation therapy within the previous 3 months were excluded from the study.
Ethical approval was obtained from the Ethical Committee of Beijing Friendship Hospital, and all patients provided written informed consent to participate in this research study.
Follow-up was performed by reviewing data in medical records or from telephone interviews that were available in the hospital database. Data collected during the follow-up period, which started from the enrollment date and ended on July 15, 2017, were used to assess the risk of TIA, IS, thromboembolism (TE), and death.
Risk stratification using CHA2DS2-VASc score
The CHA2DS2-VASc score was calculated for each patient according to the current clinical guidelines. The score ranges from 0 to 9 points and includes the following clinical characteristics: congestive heart failure or left ventricular dysfunction (1 point), hypertension (1 point), age ≥75 years (2 points), diabetes (1 point), stroke/TIA (2 points), vascular disease (1 point), age 65–74 years (1 point), and sex category (female; 1 point). The sum of all factors provides the individual patient’s risk score.
Definition of end points
The primary end point was defined as a hospital diagnosis of IS, TIA, or TE (peripheral arterial embolism, pulmonary embolism). IS/TE presents IS, TIA, and TE events combined. All-cause death was included as a secondary end point.
IS was identified by a new, sudden focal neurological deficit with a presumed cerebrovascular cause that persisted for 24 hours and could not be attributed to other identifiable causes. Events that involved symptoms and lasted <24 hours were considered as TIA. Brain imaging was performed to distinguish hemorrhagic stroke from IS. Peripheral artery embolism was defined as abrupt vascular insufficiency associated with clinical or radiographic evidence of peripheral arterial occlusion in the absence of other likely causes. The presence of vascular disease was identified from previous diagnoses, including myocardial infarction, peripheral artery disease, and complex aortic plaque.
Statistical analysis
Statistical analysis was carried out using the software SPSS, version 16.0 (IBM Corp., Armonk, NY, USA).
The baseline characteristics of the patients are described using mean and standard deviation values for continuous measures and percentages for categorical measures. Univariate comparisons were made with the χ2 or two-sample t-test. Post hoc analyses were performed using the Bonferroni test (Table 1). Time at risk was measured from the enrollment date to the time at which an IS, TIA, or TE event occurred, the date of death, or the end of the study (July 15, 2017). Time-to-event analysis was used to describe the association between the CHA2DS2-VASc score and the risk of IS/TE and death separately for the elderly patients with and without AF. The cumulative occurrence of major adverse outcomes was analyzed with the Cox proportional hazard regression model. Relative risks with 95% CIs are reported. Additionally, we measured the cumulative event-free survival by the Kaplan–Meier method and compared unadjusted differences using the log-rank test.
The diagnostic utility of the CHA2DS2-VASc score for detecting major adverse outcomes was determined via receiver-operating characteristic curve analysis. The results are expressed using the concordance (c) statistic. The significance level was set at P<0.05.
Results
Between January 1, 2013 and December 30, 2014, we screened 1,200 consecutive patients, and 139 of them met at least one of the exclusion criteria. The remaining 1,071 patients were eligible and included in the study protocol. They were followed through medical records or telephone contact for 0.04–5.67 years, with a mean follow-up duration of 2.57±1.37 years.
The baseline characteristics of the patients categorized as with or without AF are presented in Table 1. Compared to those without AF, patients with AF had more cardiovascular comorbidities: heart failure (24.9% vs 19.1%), vascular disease (55.5% vs 40.9%), and previous IS (35.7% vs 17.2%). Patients with AF had a lower ejection fraction (62.08%±9.30% vs 64.44%±7.50%, P=0.003), bigger left atrium (40.48±10.17 vs 35.91±5.64 mm, P<0.001), and creatinine (100.87±59.71 vs 90.08±47.98 mg/dL, P=0.03). The mean CHA2DS2-VASc score was 4.7±1.4, and AF patients had higher scores than patients without AF.
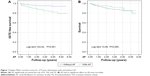
After an average follow-up of 2.57±1.37 years, 77 IS/TE events occurred among the study population. Also, there were 167 all-cause deaths, and among them, 68 patients died of pneumonia, 40 of cancer, 56 of cardiovascular disease, and three of other diseases. Overall, the incidence of major adverse cardiovascular end points was 3.2 per 100 person-years. AF increased the incidence of IS/TE significantly (log-rank =22.62, P=0.000) and had no effect on all-cause mortality (log-rank =3.66, P=0.056; Figure 1).
The incidence rates of different events during the follow-up are listed in Table 2. For the combined ischemic outcome including IS, TIA, and TE, the incidence rate was significantly higher among patients with AF than in those without AF in comparisons of those with CHA2DS2-VASc scores of 2, 3, 4, 5, and ≥6 (with concomitant AF: 0%, 4.05%, 3.5%, 10.22%, and 12.20%, respectively, and without AF: 0%, 0.89%, 2.47%, 3.21%, and 1.14%, respectively). For all-cause death, the incidence rate did not increase significantly with increasing CHA2DS2-VASc score (with concomitant AF: 31.60%, 10.24%, 9.78%, 13.44%, and 14.71%; without AF: 0%, 19%, 18.25%, 16.5%, and 26.58% for scores 2, 3, 4, 5, and ≥6, respectively; Table 2).
The discriminatory properties of the CHA2DS2-VASc score depended on the choice of end point (Figure 2). The CHA2DS2-VASc score showed obvious predictive ability for the end point of IS/TE in the elderly patients ≥75 years of age (c statistic =0.583, 95% CI, 0.518–0.647). The predictive ability of CHA2DS2-VASc score for the end point of IS/TE was a little better for the patients with AF than for those without AF (c statistic =0.598, 95% CI, 0.513–0.683 vs c statistic =0.529, 95% CI, 0.435–0.623, respectively). The CHA2DS2-VASc score had no significant predictive ability for all-cause death in patients either with or without AF (c statistic =0.503, 95% CI, 0.432–0.579 vs c statistic =0.515, 95% CI, 0.449–0.581, respectively).
According to the Cox regression models, hypertension and age were independently associated with all-cause death during long-term observation (P<0.05), with 129% and 8.1% increases, respectively, during follow-up. Elderly age increased the stroke risk by 8.1% and mortality by 7.4%. Previous stroke and age were associated with IS/TE (Table 3).
For the patients over 75 years of age, the CHA2DS2-VASc score of 5 was the cut-off value with a sensitivity of 64% and a specificity of 50%. The incidence of IS/TE in patients with CHA2DS2-VASc score of ≥5 was 4.44 per 100 person-years vs 2.38 for those with a CHA2DS2-VASc score <5, with a relative risk of 1.87. Figure 3 shows the IS/TE event-free survival according to the CHA2DS2-VASc score. A CHA2DS2-VASc score ≥5 increased the incidence of IS/TE significantly.
Discussion
The CHA2DS2-VASc scores were originally developed for stroke risk stratification of patients with nonvalvular AF to guide individualized risk-reduction anticoagulation therapy, especially for patients identified as “low risk”.8–11 To date, its value has been assessed in many patients without AF.12–14 Podolecki et al demonstrated that the CHA2DS2-VASc score is strongly associated with in-hospital mortality in acute myocardial infarction patients.15 Melgaard et al found that for heart failure patients with or without AF, the CHA2DS2-VASc score is associated with the risks of IS and death.16 Polenz et al performed a prospective study of outpatients without AF or flutter and found that the CHA2DS2-VASc score can predict major adverse cardiac outcomes, including stroke and death.5 However, whether the CHA2DS2-VASc score can predict stroke and embolism for patients of age at least 75 years irrespective of AF has not been reported.
Our study demonstrated that for patients aged 75 years or older, the CHA2DS2-VASc score was able to identify patients at high risk for stroke and could be used to quickly evaluate the stroke risk in both AF and non-AF populations, as suggested by Lip et al.8 Some mechanisms may explain the strong predictive value of CHA2DS2-VASc for the elderly patients without AF. First, all the involved risk factors were shown to increase the stroke incidence not only in the AF population but also in patients without AF. Diabetes mellitus, hypertension, and congestive heart failure are associated with endothelial dysfunction, increased thrombin formation, and abundance of adhesion molecules, which all together lead to a prethrombotic state, thereby contributing to imbalance of procoagulants and anticoagulants.17–19 Secondly, a positive association was observed between the number of risk factors and the incidence rates of IS and TIA.20 Our study had a high prevalence of cardiovascular diseases and relevant risk factors such as hypertension (93% of patients), diabetes (35.7%), heart failure (20.9%), and vascular disease (46.2%), which caused the high incidence of stroke.
Age and a previous stroke were independent risk factors for IS/TE events among the very old patients.21 In our study, a CHA2DS2-VASc score of 5 could easily separate individuals with a high risk of stroke from those at lower risk, with a sensitivity of 64% and a specificity of 50%. The incidence of IS/TE was 3-fold greater in patients with a CHA2DS2-VASc score ≥5 compared with that in patients with a score <5. As an independent predictor for stroke, the CHA2DS2-VASc score has the distinct advantage that it can be quickly calculated bedside. For those with higher scores, especially >5, we should strengthen antiplatelet therapy, especially with new oral anticoagulation.22 This therapy should also be applied in future studies to investigate the effect of prophylactic anticoagulation in high-risk patients without AF.23
The CHA2DS2-VASc score showed no predictive value for mortality, consistent with the findings of Clua-Espuny et al24 who found no association between death and AF for patients 80 years or older, and with chronic heart failure. The independent risk factors for annual mortality were male gender, enlarged left ventricular systolic dimension, and dyslipidemia. Notably, our study differed from those that reported an increased risk of mortality in AF patients (both in-hospital and long term) and in special patient populations such as those with heart failure, heart transplant recipients, and those with Takotsubo syndrome.25–27 First, different study populations may explain the different results. In our study, only 46.2% of patients suffered from heart disease. Instead, most of the patients died of pneumonia and cancer, with only 33.5% having died of myocardial infarction, stroke, or another cardiovascular disease. The CHA2DS2-VASc score only had a strong predictive value for the latter. Secondly, the mean patient age differed between this study and previous studies. Most previous studies enrolled middle-aged to elderly patients, whereas our patient population was aged from 75 to 100 years, much older than other studies.
Conclusion
The risk of TE was strongly associated with the CHA2DS2-VASc score for patients 75 years old or older with and without AF. Hence, this scoring system may be useful for identifying patients at high risk for stroke who have no history of AF and for whom additional preventive measures might be beneficial to improving outcomes.
Limitations of the study
Our study had several limitations. The results were derived from a single-center, retrospective study. The small sample size, short follow-up, and small number of events also represent a source of bias. The specificity and sensitivity of the CHA2DS2-VASc score for predicting cardiac events were not high, which is likely because the risk factors for patients without AF differ from those for patients with AF. Also, we did not consider different types of AF (paroxysmal, persistent, and permanent), and perhaps outcomes would have differed among these groups.
Acknowledgments
This study was supported by the Beijing Municipal Science and Technology Commission (Project No 15110000391508), the Central Healthcare Committee Fund (Project No W2013BJ55), and the Beijing Municipal Administration of Hospitals Incubating Program (Project No PX2016033).
Disclosure
The authors report no conflicts of interest in this work.
References
Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–e322. | ||
Camm AJ, Lip GY, De Caterina R, et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation–developed with the special contribution of the European Heart Rhythm Association. Europace. 2012;14(10):1385–1413. | ||
Lip GY, Lin HJ, Chien KL, et al. Comparative assessment of published atrial fibrillation stroke risk stratification schemes for predicting stroke, in a non-atrial fibrillation population: the Chin-Shan Community Cohort Study. Int J Cardiol. 2013;168(1):414–419. | ||
Mitchell LB, Southern DA, Galbraith D, Ghali WA, Knudtson M, Wilton SB; APPROACH investigators. Prediction of stroke or TIA in patients without atrial fibrillation using CHADS2 and CHA2DS2-VASc scores. Heart. 2014;100(19):1524–1530. | ||
Polenz GF, Leiria TL, Essebag V, et al. CHA2DS2-VASc score as a predictor of cardiovascular events in ambulatory patients without atrial fibrillation. Pacing Clin Electrophysiol. 2015;38(12):1412–1417. | ||
Xing Y, Ma Q, Ma X, Wang C, Zhang D, Sun Y. CHADS2 score has a better predictive value than CHA2DS2-VASc score in elderly patients with atrial fibrillation. Clin Interv Aging. 2016;11:941–946. | ||
Xing YL, Ma Q, Ma XY, et al. Characteristics of non-valvular atrial fibrillation patients who benefit most from anticoagulation treatment. Int J Clin Exp Med. 2015;8(10):18721–18728. | ||
Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137(2):263–272. | ||
Mazza A, Pessina AC, Pavei A, Scarpa R, Tikhonoff V, Casiglia E. Predictors of stroke mortality in elderly people from the general population. The Cardiovascular Study in the Elderly. Eur J Epidemiol. 2001;17(12):1097–1104. | ||
Chan YH, Yiu KH, Lau KK, et al. The CHADS2 and CHA2DS2-VASc scores predict adverse vascular function, ischemic stroke and cardiovascular death in high-risk patients without atrial fibrillation: role of incorporating PR prolongation. Atherosclerosis. 2014;237(2):504–513. | ||
Lai HC, Chien WC, Chung CH, et al. Atrial fibrillation, CHA2DS2-VASc score, antithrombotics and risk of traffic accidents: a population-based cohort study. Int J Cardiol. 2015;197:133–139. | ||
Kim KH, Kim W, Hwang SH, et al. The CHA2DS2-VASc score can be used to stratify the prognosis of acute myocardial infarction patients irrespective of presence of atrial fibrillation. J Cardiol. 2015;65(2):121–127. | ||
Santosa F, Nowak T, Moysidis T, et al. CHADS2 and CHA2DS2Vasc-Score in Peripheral Systemic Embolism. J Atr Fibrillation. 2013;6(1):715. | ||
Peguero JG, Issa O, Podesta C, Elmahdy HM, Santana O, Lamas GA. Usefulness of the CHA2DS2VASc score to predict postoperative stroke in patients having cardiac surgery independent of atrial fibrillation. Am J Cardiol. 2015;115(6):758–762. | ||
Podolecki T, Lenarczyk R, Kowalczyk J, et al. Stroke and death prediction with CHA2DS2-vasc score after myocardial infarction in patients without atrial fibrillation. J Cardiovasc Med (Hagerstown). 2015;16(7):497–502. | ||
Melgaard L, Gorst-Rasmussen A, Lane DA, Rasmussen LH, Larsen TB, Lip GY. Assessment of the CHA2DS2-VASc score in predicting ischemic stroke, thromboembolism, and death in patients with heart failure with and without atrial fibrillation. JAMA. 2015;314(10):1030–1038. | ||
Cushman M, Psaty BM, Macy E, et al. Correlates of thrombin markers in an elderly cohort free of clinical cardiovascular disease. Arterioscler Thromb Vasc Biol. 1996;16(9):1163–1169. | ||
Chong AY, Lip GY. Viewpoint: the prothrombotic state in heart failure: a maladaptive inflammatory response? Eur J Heart Fail. 2007;9(2):124–128. | ||
Cha JK, Lim JH, Kim DH, et al. Prognostic factors for long-term poor outcomes after acute ischemic stroke in very old age (>80 years) patients: total cholesterol level might differently influence long-term outcomes after acute ischemic stroke at ages above 80 years. Geriatr Gerontol Int. 2015;15(11):1227–1233. | ||
Yuan Z, Makadia R, Ryan P, Yannicelli D, Nessel C, Sarich T. Incidence of ischemic stroke or transient ischemic attack in patients with multiple risk factors with or without atrial fibrillation: a retrospective cohort study. Curr Med Res Opin. 2015;31(7):1257–1266. | ||
Patti G, Lucerna M, Pecen L, et al. Thromboembolic risk, bleeding outcomes and effect of different antithrombotic strategies in very elderly patients with atrial fibrillation: a sub-analysis from the PREFER in AF (PREvention oF Thromboembolic Events-European Registry in Atrial Fibrillation). J Am Heart Assoc. 2017;6(7):e005657. | ||
Elgendy AY, Mahtta D, Barakat AF, et al. Meta-analysis of safety and efficacy of uninterrupted non-vitamin K antagonist oral anticoagulants versus vitamin K antagonists for catheter ablation of atrial fibrillation. Am J Cardiol. 2017;120(10s):1830–1836. | ||
Odutayo A, Wong CX, Hsiao AJ, Hopewell S, Altman DG, Emdin CA. Atrial fibrillation and risks of cardiovascular disease, renal disease, and death: systematic review and meta-analysis. BMJ. 2016;354:i4482. | ||
Clua-Espuny JL, Panisello-Tafalla A, Lopez-Pablo C, et al. Atrial fibrillation and cardiovascular comorbidities, survival and mortality: a real-life observational study. Cardiol Res. 2014;5(1):12–22. | ||
Li LH, Sheng CS, Hu BC, et al. The prevalence, incidence, management and risks of atrial fibrillation in an elderly Chinese population: a prospective study. BMC Cardiovascular Disorders. 2015;15:31. | ||
Marwan Saad, Islam Y, Elgendy, et al. Incidence, predictors, and outcomes of early atrial arrhythmias after lung transplant: a systematic review and meta-analysis. J Am Coll Cardiol EP. 2017;3:718–726. | ||
Mahmoud AN, Al-Ani M, Saad M, Elgendy AY, Elgendy IY. Development and validation of a simple integer risk score for prediction of in-hospital mortality following Takotsubo syndrome. Heart Lung. 2016; 45(6):510–514. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.