Back to Journals » Journal of Inflammation Research » Volume 16
Case Report: Unusual Cause of Fever in Ulcerative Colitis Treated with Infliximab
Authors Sha S, Shi H, Wu J, Zhang M, Qin B, Yang L, Liu X
Received 2 January 2023
Accepted for publication 9 March 2023
Published 23 March 2023 Volume 2023:16 Pages 1267—1270
DOI https://doi.org/10.2147/JIR.S403371
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Adam D Bachstetter
Sumei Sha,1,* Haitao Shi,1,* Jie Wu,2,* Ming Zhang,3 Bin Qin,1 Longbao Yang,1 Xin Liu1
1Department of Gastroenterology, the Second Affiliated Hospital of Xi’an Jiaotong University, Xi’an, Shaanxi, People’s Republic of China; 2Department of Pathology, the Second Affiliated Hospital of Xi’an Jiaotong University, Xi’an, Shaanxi, People’s Republic of China; 3Department of Respiratory, the Second Affiliated Hospital of Xi’an Jiaotong University, Xi’an, Shaanxi, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xin Liu, Department of Gastroenterology, the Second Affiliated Hospital of Xi’an Jiaotong University, Xi’an, Shaanxi, 710004, People’s Republic of China, Email [email protected]
Introduction: Patients with inflammatory bowel disease are at high risk for opportunistic infections, and fungal infections are relatively uncommon among various infections.
Case: This case is the first reported ulcerative colitis accompanied with Cryptococcus neoformans infection after infliximab treatment. In the course of the disease, the patients had a variety of opportunistic infections, including viruses, fungi and bacteria.
Conclusion: This case highlights the importance of paying continued attention to opportunistic infections for patients with inflammatory bowel disease.
Keywords: ulcerative colitis, Cryptococcus neoformans pneumonia, cytomegalovirus infection, clostridium difficile infection, biological agents, case report
Case Presentation
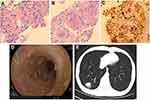
A 51-year-old male patient was admitted to our hospital with aggravated bloody stool and diarrhea for 2 months, accompanied with fever, left lower abdominal pain and tenesmus. Four years before admission, the patient was diagnosed with “colitis” for the similar symptoms not so serious without fever in another hospital. Although mesalazine had been prescribed, he had given up medications and follow-up visit without a doctor’s recommendation before admission. Laboratory tests showed elevated C reactive protein (CRP) of 35.8 mg/L. Hemoglobin was decreased at 125g/L. Colonoscopy revealed extensive colitis, with wide mucosal defect and spontaneous bleeding in the sigmoid colon (Figure 1A). No obvious abnormality was found on chest CT (Figure 1B). Cytomegalovirus (CMV) inclusion bodies showed positivity. After intravenous ganciclovir and methylprednisolone, the symptoms did not improve. Hence, the patient was sequential to infliximab. Although the stool returned to normal with improvement of laboratory tests and lesions under colonoscopy (Figure 1C) after infliximab treatment for 4 times, the patient still had a fever (the temperature is about 38°C), with no other respiratory symptoms. A recheck of the chest CT showed a mass shadow right lower lung lobe (Figure 1D). After antibiotic was administrated according to the drug sensitivity results of sputum culture (which showed Acinetobacter baumannii was positive), the patient no longer had a fever, but there was no change in lung mass. What is the diagnosis?
Answer
The colon lesions were diagnosed as ulcerative colitis (UC). Puncture and biopsy of the lung mass guided by B-ultrasound revealed granulomatous inflammation and necrosis, with multiple variable-sized encapsulated yeast cells present in hematoxylin and eosin staining, hexamine silver staining and periodic acid-Schiff staining (Figure 2A–C), the final diagnosis is Cryptococcus neoformans pneumonia. After the diagnosis was confirmed, antifungal treatment with voriconazole (0.2g oral bid) was given. Medicine for UC was changed to vedolizumab, and the patient had no bloody stool, with the ESR and CRP normalized. After vedolizumab treatment for 3 times, reexamined colonoscopy showed a slight pseudomembranous colitis in rectum sigmoid colon (Figure 2D), followed by positive results of fecal Clostridium difficile toxin test. The patient then received oral vancomycin for 14 days. After 3 months of treatment with voriconazole, the lung lesions were mostly absorbed (Figure 2E). At present, the patient continues to take voriconazole orally and receive vedolizumab treatment according to the course of treatment. There is no cough, expectoration, fever, bloody stool or diarrhea.
Discussion
Cryptococcus neoformans is a yeast widely distributed in nature and animals (especially the intestines of pigeons). Cryptococcus neoformans are infectious to both immunocompromised and immunocompetent hosts, with impaired T lymphocyte function imparting the greatest risk.1 It is speculated that the addition of infliximab provided the additional degree of immunosuppression required to allow cryptococcal dissemination. It mainly invades the central nervous system and respiratory system. The clinical and imaging manifestations of Cryptococcus neoformans pneumonia are lack of specificity, which is easy to cause misdiagnosis, delay and aggravation of the disease. Antifungal drugs include fluconazole, amphotericin and voriconazole as the main therapeutic drugs. Most of the patients have a good prognosis.
Patients with inflammatory bowel disease (IBD) are at high risk of opportunistic infection. We report a case of acute severe UC with no contact history of pigeons. UC improved after treatment with infliximab but occurred with sustained fever. The final diagnosis is Cryptococcus neoformans pneumonia. There are only several cases about Cryptococcus neoformans infection after infliximab treatment. Most of the basic diseases are rheumatoid arthritis and only five cases of IBD (all of them are Crohn’s disease, Table 1). This case is the first reported UC accompanied with Cryptococcus neoformans infection after infliximab treatment. In the course of the disease, the patients had a variety of opportunistic infections, including viruses (CMV), fungi (Cryptococcus neoformans) and bacteria (clostridium difficile). In summary, the case suggests that continued attention is required to identify the clinical risk of opportunistic infections associated with IBD.
 |
Table 1 Case Reports of Cryptococcus neoformans in IBD Patients on TNF-α Inhibitor |
Conclusions
Patients with IBD are at high risk of opportunistic infection. Tumor necrosis factor (TNF) antagonists promote all types of serious and opportunistic infections, whereas vedolizumab promotes intestinal infections. Opportunistic infections should be detected during immunosuppressive therapy, including bacterial, viral, fungal and other opportunistic infections.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author (Xin Liu) upon request.
Ethical Approval and Consent to Participate
The study was approved by the Ethics Committee of the Second Affiliated Hospital of Xi’an Jiaotong University. Written informed consent was obtained from the patient for the publication of all the images and data included in this article. Ethical review and approval were not required to publish the case details in accordance with the institutional requirements.
Consent to Publish
The patient has consented to the submission of the case report to the journal.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by grants from the youth program of Shaanxi Natural Science Foundation (No. 2021JQ-420 and 2022SF-195).
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Levitz SM. The ecology of Cryptococcus neoformans and the epidemiology of cryptococcosis. Rev Infect Dis. 1991;13:1163–1169. doi:10.1093/clinids/13.6.1163
2. Rehman T, Ali J, Lopez FA. A 61-year-old man with asymptomatic, bilateral lung masses. J La State Med Soc. 2008;160:309–14; quiz 349.
3. Hirai F, Matsui T, Ishibashi Y, et al. Asymptomatic pulmonary cryptococcosis in a patient with Crohn’s disease on infliximab: case report. Inflamm Bowel Dis. 2011;17:1637–1638. doi:10.1002/ibd.21564
4. Hussein M, Haq IU, Hameed M, et al. Isolated pulmonary cryptococcosis in a patient with Crohn’s disease treated with infliximab: a case report and literature review. Respir Med Case Rep. 2021;33:101459. doi:10.1016/j.rmcr.2021.101459
5. Osawa R, Singh N. Colitis as a manifestation of infliximab-associated disseminated cryptococcosis. Int J Infect Dis. 2010;14:e436–e440. doi:10.1016/j.ijid.2009.05.019
6. Takazono T, Izumikawa K, Yoshioka S, et al. Possible pulmonary cryptococcosis in a patient with Crohn’s disease during anti-tumor necrosis factor-alpha treatment: a case report and literature review. Jpn J Infect Dis. 2012;65:461–464. doi:10.7883/yoken.65.461
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.