Back to Journals » Cancer Management and Research » Volume 14
Case Report: Misdiagnosis of Lung Carcinoma in Patients with Shrunken Lung Cyst After High Altitude Travel
Authors Xie Y, Zhang D, Zhao H, Lei S, Zhang H, Zhang S
Received 2 May 2022
Accepted for publication 29 July 2022
Published 7 August 2022 Volume 2022:14 Pages 2373—2377
DOI https://doi.org/10.2147/CMAR.S373068
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Bilikere Dwarakanath
Yibing Xie,1,2 Dongmei Zhang,3 Huanfen Zhao,4 Shaoyang Lei,2 Hua Zhang,5 Shuqian Zhang2
1Department of Graduate School, Hebei North University, Zhangjiakou, People’s Republic of China; 2Department of Radiology, Hebei General Hospital, Shijiazhuang, People’s Republic of China; 3Department of Endocrinology, Hebei General Hospital, Shijiazhuang, People’s Republic of China; 4Department of Pathology, Hebei General Hospital, Shijiazhuang, People’s Republic of China; 5Department of Thoracic Surgery, Hebei General Hospital, Shijiazhuang, People’s Republic of China
Correspondence: Shuqian Zhang, Department of Radiology, Hebei General Hospital, 348 Heping West Road, Shijiazhuang, 050051, People’s Republic of China, Tel +8615930153668, Email [email protected]
Background: Lung cancer associated with cystic airspace is a rare disease, and the imaging understanding of lung cancer with cystic cavity is still unclear. Little is known in the literature on whether cystic lung cancer is caused by emphysema or ruptured bullae.
Case Reports: We report the case of a 50-year-old female patient after finishing a business trip in November 2021, when another chest CT demonstrated an unexpected reduction in the cyst, with a solid mural nodule on the posterior wall. The airspace of the cyst is only about 13 mm × 12 mm × 6 mm in size. The size of the mural nodule in the posterior wall is about 10 mm × 6 mm × 5 mm. The patient felt anxious due to suspicion of lung cancer. 2.5 months after the last chest CT, she accepted minimally invasive thoracoscopic surgery on the posterior basal segment of the left lower lobe. The postoperative pathology showed benign lesions.
Conclusion: For radiologists, it is important to recognize the process from lung cysts or bullae to LC-CAS, especially the morphological changes of the cyst airspace and the cyst wall, in order to identify the malignant features of lung cysts in time.
Keywords: bullae, lung cancer associated with cystic airspaces, pulmonary cysts, lung disease
Introduction
Pulmonary cysts are defined on computer tomography (CT) as around parenchymal lucency or low-attenuating area with clear demarcations from the lung parenchyma that may be solitary or appear in a small number in any part of the lung. They are usually thin-walled (<2 mm), and some of their walls are difficult to identify.1 Pulmonary cysts are microscopically lined with epithelial or fibrous wall-like structures.2 The pathogenesis of pulmonary cyst’s formation remains uncertain and there are several proposed mechanisms, including check-valve obstruction with distal overinflation, ischemia and necrosis of the airway wall, and remodeling induced by proteases.3 Although they may occur in normal individuals, they do have a possibility of developing into lung cancer, especially in the classification of lung cancer associated with cystic airspaces (LC-CAS).4,5 The article reports a case of a solitary pulmonary cyst manifested as sudden reduction of the cystic airspace with a mural nodule that was confirmed to be benign after minimally invasive thoracoscopic segmentectomy. Written informed consent of the patient was obtained for this case report and related pictures. This case report was approved by Hebei General Hospital Ethics Committee with study number 2022055.
Case Report
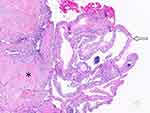
A 50-year-old female patient went to the hospital for an annual physical examination in July 2017. Chest CT revealed a giant pulmonary cyst of approximately 79 × 63 × 23 mm in the posterior basal segment of the left lower pulmonary lobe. Its upper wall was relatively uniform in thickness of about 1.6 mm and its lower wall fitted the diaphragm. This lesion had a clear and smooth interface with lung parenchyma. No emphysema and other abnormal lesions were found in the remaining lung fields. The follow-up chest CT obtained in 2019 showed the lesion was enlarged into a measurement of approximately 86 × 61 × 37 mm, and the upper wall thickness reduced to 1.4 mm (Figure 1). Over the past two years, no chest discomfort was reported. In 2020, the patient had to go to Tibet, northwest China, on business. She accepted a chest CT scan at a local hospital, which also revealed a lung cyst of similar size in the left lower lobe (no images provided). After the business trip in November 2021, another chest CT demonstrated the cyst airspace was shrunk significantly to only 13 × 12 × 6 mm with an eccentric solid mural nodule of approximately 10 × 6 × 5 mm in the posterior wall (Figure 2). The patient received minimally invasive thoracoscopic surgery on the posterior basal segment of the left lower lobe due to the suspicion of lung cancer 2.5 months after the latest chest CT. The postoperative pathology showed hyaline degenerated granuloma with lung cyst wall structure on the lateral side (Figure 3).
The patient reported in detail after the operation that she had a high-altitude trip after accepting chest CT at the local hospital. On the first day, when she reached the campsite at an elevation of 3000 meters, she developed severe chest pain in the left lower chest after picking up a kettle. The pain was relieved two hours later without cough, sputum, hemoptysis, and difficulty breathing. On the next day, the patient arrived at an altitude of 4000 meters for sightseeing. She did not feel uncomfortable even jumping there. Therefore, based on the significant shrinkage of the lung cyst and postoperative pathological manifestations, it was believed that the original lung cyst ruptured and shrank to a small cyst with the mural nodule.
Discussion
According to the patient’s transient high-altitude travel history and sudden chest pain, a series of changes caused by acute exposure to high altitude may account for the rupture of the giant lung cyst. Tibet, an area with high altitude in China, has distinctive environmental characteristics of low air oxygen, low air pressure, and low temperature, which may contribute to airway reactivity, ventilator changes and alterations in pulmonary hemodynamics. Therefore, the airway pressures of local residents are always higher than residents of the plains.6 The one-way valve effect caused by the non-specific inflammation of the terminal bronchiolar orifice could increase the air content of the distal alveoli due to increased airway pressure, leading to a high frequency of lung cysts in local residents. The transpulmonary pressure generated by the reduction of atmospheric pressure can result in rapid expansion of the air sacs or bullae in lungs and rupture eventually.7 Patients who suffered from spontaneous pneumothorax, one of the complications of ruptured lung cysts in the sub-pleural area, may develop sudden chest pain, even dyspnea, but normally mild symptoms. Physical examination can present reduced or absent breath sounds, reduced ipsilateral chest expansion, and hyper-resonant percussion. However, a definite diagnosis of spontaneous pneumothorax often depends on radiological examinations.8 According to the patient’s self-report, it is believed that the original giant lung cyst ruptured when she ascended to the high altitude, resulting in spontaneous pneumothorax. Her symptoms were not severe, possibly due to a small amount of air in the thoracic cavity or no continuous air leakage with rapid encapsulation subsequently. The chest pain relieved significantly within two hours and there was no discomfort even after reaching higher altitude the next day. Unfortunately, the patient had not accepted any examinations to figure out why the sudden chest pain occurred since she went back to the plain. Consequently, it is difficult to make a definite diagnosis of the decreased lung cyst with the mural nodules detected in recent CT scan, leading to too much attention being paid to malignant signs, but ignoring the possibility that the lung cyst with mural nodule was associated with the sudden chest pain.
By the end of the last century, it has been reported that the incidence of the primary pulmonary carcinoma arising from bullae could be as high as 9%.9 However, there was not enough data on the incidence of lung carcinoma arising from lung cysts. Concerns about the possibility that lung cancer was associated with cystic airspace have been raised until a decade later.10 The predominant histological type of LC-CAS is adenocarcinoma, which is up to 88%.11 The evolution from pulmonary cysts or bullae to LC-CAS is a complex process, and regular follow-up imaging plays an essential role in estimating the malignant characteristics of the lung cyst. It has been suggested that limited air flow within the compressed wall-like structures surrounding a lung cyst or bulla may lead to organism accretion on the wall of the bulla and cause repeated infection. And this repeated inflammatory process may result in the formation of fibrous scar around the bulla, leading to the accumulation of carcinogens in the bulla.12 In addition, the presence of cysts may interfere with normal ventilation and clearance of the lungs, which could also aggravate the deposition of carcinogens.13 Therefore, more attention needs to be paid to this special type of lung cancer arising from the wall of a pulmonary cyst. The slow growth of LC-CAS in the early stage also challenges the diagnosis of LC-CAS. Previous longitudinal studies have shown that lung cysts detected in the baseline CT had developed into localized wall nodules 12–118 months (median, 35 months) later.10 The original giant lung cyst may evolve to LC-CAS within two years according to the process above, which is precisely what the patient in this case was worried about. However, this is one of the evolution patterns of LC-CAS, and other patterns might present that the cyst occurred after the carcinoma. The one-way valve effect is the main mechanism for the air-containing cyst formation in a pulmonary tumor. It can be caused by the external compression of the small airway through the fibrous deposits produced by tumor cells, resulting in stenosis and degeneration of the airway. And it also can be triggered when the tumor invades the airway wall directly and leads to structure destruction. However, at this moment, the tumor is too small to be detected by any radiological methods including chest CT.14,15
For patients with suspected LC-CAS, two aspects of the morphological changes in the follow-up chest CT should be focused on. One is the cyst airspace, and the other is the cyst wall, including wall thickness, mural nodule formation, and the surrounding ground-glass opacity. The air cyst of LC-CAS can increase, remain or even shrink during the follow-up.16 In other words, although the diameter of LC-CAS decreases due to the shrinkage of the cyst, it could not be predicted as a benign lesion. The cyst airspace can usually be squeezed by the enlarged solid component of LC-CAS, and eventually disappears to become a total solid mass. Besides, the cyst could also increase with the growth of LC-CAS owing to the one-way valve effect. However, we found that changes in the cyst have important clues to the invasiveness of adenocarcinoma, which is the main histological type of LC-CAS. Previous studies based on CT radiomic features to predict the histological aggressiveness of lung adenocarcinoma in subsolid nodules smaller than 3 cm have shown that the specificity for the changes in the cystic fraction in radiomic features was up to 96.6%. Therefore, the change in the size of the cystic cavity is a sign of invasive adenocarcinoma with high specificity.17 The wall thickening of the cyst, enlarged mural nodule, and peripheral ground-glass opacity enlarging or density increasing are characteristic radiological signs indicating malignancy.4,5,10,16,18,19
For radiologists, it is important to recognize the process from lung cysts or bullae to LC-CAS, especially the morphological changes of the cyst airspace and the cyst wall, in order to identify the malignant features of lung cysts in time. Radiologists and thoracic surgeons should take the possibility of rupture of the original giant pulmonary cyst into consideration before thoracoscopic segmentectomy. A detailed inquiry of high-altitude travel history can avoid unnecessary surgical treatment.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lee KC, Kang EY, Yong HS., et al. A stepwise diagnostic approach to cystic lung diseases for radiologists. Korean J Radiol. 2019;20(9):1368–1380. doi:10.3348/kjr.2019.0057
2. Hansell DM, Bankier AA, MacMahon H, McLoud TC, Muller NL, Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology. 2008;246(3):697–722. doi:10.1148/radiol.2462070712
3. Gupta N, Vassallo R, Wikenheiser-Brokamp KA, McCormack FX. Diffuse cystic lung disease. Part II. Am J Respir Crit Care Med. 2015;192(1):17–29. doi:10.1164/rccm.201411-2096CI
4. Mascalchi M, Attina D, Bertelli E, et al. Lung cancer associated with cystic airspaces. J Comput Assist Tomogr. 2015;39(1):102–108. doi:10.1097/RCT.0000000000000154
5. Shen Y, Xu X, Zhang Y, et al. Lung cancers associated with cystic airspaces: CT features and pathologic correlation. Lung Cancer. 2019;135:110–115. doi:10.1016/j.lungcan.2019.05.012
6. Stream JO, Luks AM, Grissom CK. Lung disease at high altitude. Expert Rev Respir Med. 2009;3(6):635–650. doi:10.1586/ers.09.51
7. Alifano M, Forti Parri SN, Bonfanti B, et al. Atmospheric pressure influences the risk of pneumothorax: beware of the storm! Chest. 2007;131(6):1877–1882. doi:10.1378/chest.06-2206
8. Tschopp JM, Bintcliffe O, Astoul P, et al. ERS task force statement: diagnosis and treatment of primary spontaneous pneumothorax. Eur Respir J. 2015;46(2):321–335. doi:10.1183/09031936.00219214
9. Hanaoka N, Tanaka F, Otake Y, et al. Primary lung carcinoma arising from emphysematous bullae. Lung Cancer. 2002;38(2):185–191. doi:10.1016/S0169-5002(02)00186-1
10. Farooqi AO, Cham M, Zhang L, et al. Lung cancer associated with cystic airspaces. AJR Am J Roentgenol. 2012;199(4):781–786. doi:10.2214/AJR.11.7812
11. Mendoza DP, Heeger A, Mino-Kenudson M, et al. Clinicopathologic and longitudinal imaging features of lung cancer associated with cystic airspaces: a systematic review and meta-analysis. AJR Am J Roentgenol. 2021;216(2):318–329. doi:10.2214/AJR.20.23835
12. Kaneda M, Tarukawa T, Watanabe F, Adachi K, Sakai T, Nakabayashi H. Clinical features of primary lung cancer adjoining pulmonary bulla. Interact Cardiovasc Thorac Surg. 2010;10(6):940–944. doi:10.1510/icvts.2010.233551
13. Snoeckx A, Reyntiens P, Carp L, et al. Diagnostic and clinical features of lung cancer associated with cystic airspaces. J Thorac Dis. 2019;11(3):987–1004. doi:10.21037/jtd.2019.02.91
14. Tan Y, Gao J, Wu C, et al. CT characteristics and pathologic basis of solitary cystic lung cancer. Radiology. 2019;291(2):495–501. doi:10.1148/radiol.2019181598
15. Zhang J, Deng H, Wu CC, et al. The mechanism of formation of thin-walled cystic lung cancer. Medicine. 2019;98(14):e15031. doi:10.1097/MD.0000000000015031
16. Fintelmann FJ, Brinkmann JK, Jeck WR, et al. Lung cancers associated with cystic airspaces: natural history, pathologic correlation, and mutational analysis. J Thorac Imaging. 2017;32(3):176–188. doi:10.1097/RTI.0000000000000265
17. Wu YJ, Liu YC, Liao CY, Tang EK, Wu FZ. A comparative study to evaluate CT-based semantic and radiomic features in preoperative diagnosis of invasive pulmonary adenocarcinomas manifesting as subsolid nodules. Sci Rep. 2021;11(1):66. doi:10.1038/s41598-020-79690-4
18. Lindell RM, Hartman TE, Swensen SJ, et al. Five-year lung cancer screening experience: CT appearance, growth rate, location, and histologic features of 61 lung cancers. Radiology. 2007;242(2):555–562. doi:10.1148/radiol.2422052090
19. Araki T, Nishino M, Gao W, et al. Pulmonary cysts identified on chest CT: are they part of aging change or of clinical significance? Thorax. 2015;70(12):1156–1162. doi:10.1136/thoraxjnl-2015-207653
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.