Back to Journals » Infection and Drug Resistance » Volume 15
Carriage of Neisseria meningitidis Among Umrah Pilgrims: Circulating Serogroups and Antibiotic Resistance
Authors Yezli S, Yassin Y , Mushi A, Bukhari M, Banasser T, Khan A
Received 17 May 2022
Accepted for publication 1 August 2022
Published 23 August 2022 Volume 2022:15 Pages 4685—4696
DOI https://doi.org/10.2147/IDR.S375096
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Saber Yezli,1 Yara Yassin,1 Abdulaziz Mushi,1 Mamdouh Bukhari,2 Talib Banasser,2 Anas Khan1,3
1The Global Centre for Mass Gatherings Medicine, Ministry of Health, Riyadh, Saudi Arabia; 2Regional Laboratory, Makkah City General Directorate of Health Affairs, Ministry of Health, Makkah, Saudi Arabia; 3Department of Emergency Medicine, College of Medicine, King Saud University, Riyadh, Saudi Arabia
Correspondence: Saber Yezli, Global Centre for Mass Gatherings Medicine, Public Health Directorate, Ministry of Health, Riyadh, Saudi Arabia, Tel +96611401555 ext 1863, Email [email protected]
Background: Meningococcal disease and outbreaks are a risk during mass gatherings such as the Umrah religious pilgrimage to the Kingdom of Saudi Arabia (KSA). We aimed to investigate the carriage of Neisseria meningitidis among the 2019 Umrah pilgrims and determine the circulating serogroups and their antibiotic susceptibility profiles.
Methods: We conducted a cross-sectional study among adult Umrah pilgrims from 17th to 29th April 2019 in Mecca city, KSA. A questionnaire was administered to each participant, and an oropharyngeal swab was obtained. Microbiological techniques were used to isolate, identify and serogroup N. meningitidis from the swabs. E-tests were used to determine the susceptibility of the isolates to nine antibiotics.
Results: The study enrolled 616 pilgrims from 17 countries with a mean age of 53.8 years (± 13.1, range = 19– 91) and a male-to-female ratio of 1.1:1. Nearly 39% of the respondents had no formal education, 32.5% declared having an underlying health condition and 17.2% were current or past smokers. During their Umrah stay, most pilgrims reported sharing accommodation (98.5%) and never using a face mask (98.5%). Also, 34.6% reported suffering from influenza-like symptoms and 11.8% used antibiotics. N. meningitidis was isolated from three pilgrims (carriage rate of 0.49%), two were serogroup A and one was serogroup B. Antibiotic susceptibility results were available for one isolate (serogroup B) which showed resistance to ciprofloxacin and decreased susceptibility to trimethoprim-sulfamethoxazole.
Conclusion: Carriage of N. meningitidis among Umrah pilgrims was low. However, invasive serogroups were identified, including an isolate resistant to ciprofloxacin used for chemoprophylaxis. Meningococcal disease preventive measures for Umrah should be regularly reviewed and updated accordingly to reduce the risk of the disease and future pilgrimage-associated outbreaks.
Keywords: mass gatherings, meningococcal disease, antibiotic resistance, public health, vaccine
Introduction
Meningococcal disease is a serious public health issue globally with significant morbidity and mortality burdens.1 Among survivors, up to 20% suffer from complications and sequelae. Meningococci are spread through direct contact with oropharyngeal secretions, and asymptomatic carriers are the primary source of Neisseria meningitidis transmission.2 However, only a minority of those who acquire carriage go on to develop meningococcal disease, most of which is caused by six serogroups (A, B, C, W, X, and Y).3 Given the seriousness of the disease, its rapid progression, its high mortality rate and sequelae, and its outbreak potential, meningococcal disease is a significant public health threat in crowded settings and mass gatherings.4,5
The Hajj and Umrah religious mass gatherings take place in Mecca in the Kingdom of Saudi Arabia (KSA). Over 10 million Muslim pilgrims from around the world attend these events each year. More than 2 million participate in Hajj, which takes place over five specific days of the 12th month in the Islamic calendar.6 Compared to Hajj, Umrah is performed almost all year-round, and its rituals are shorter in duration. The number of foreign Umrah visitors has increased significantly in the last decade, and according to the Saudi Vision 2030, the number is expected to reach 30 million by 2030.6 The international nature of the Hajj and Umrah, their scale and demographic characteristics, as well as the crowded settings and shared living at these events increase the risk of meningococcal disease and its transmission.4 As such, a number of local and international outbreaks of the disease were associated with these mass gatherings.7 These include serogroup A disease outbreaks in 1987 and throughout the 1990s and two international serogroup W outbreaks in 2000 and 2001.7 Comprehensive preventive measures including compulsory vaccination with the quadrivalent vaccine significantly reduced meningococcal disease cases in KSA and eliminated pilgrimage-associated outbreaks.7,8
Although meningococcal disease and outbreaks associated with Umrah have been reported in the past,7 little is known about N. meningitidis carriage during the pilgrimage or the circulating serogroups and their antibiotic susceptibility profiles.9,10 Given the current lack of meningococcal disease cases associated with Umrah, continued surveillance of the characteristics of the N. meningitidis carrier state among Umrah pilgrims will assist in understanding the changing epidemiology of the organism and in predicting and possibly preventing outbreaks during future pilgrimages. This is particularly relevant given that the current compulsory meningococcal vaccination measures for Umrah do not cover serogroups B or X.11 The present study aims to investigate the carriage of N. meningitidis among Umrah pilgrims in 2019, circulating serogroups and antimicrobial resistance of the carried isolates.
Methods
Study Design, Location and Population
This is a prospective cross-sectional carriage study conducted from the 17th-29th April 2019 in Mecca city, KSA. The study population included adult (≥18 years) Umrah visitors attending the pilgrimage during the study period. The sample size was calculated based on an estimated population size during the study period of 500,000 and using a margin of error of 2%, a confidence interval of 95% and an estimated carriage rate of 5%, based on the results of the most recent carriage study conducted among Umrah pilgrims.10 The minimum sample size estimated for the study was 457. We enrolled a larger sample size of 616 pilgrims to account for errors and non-respondents.
Enrolment and Data Collection
Convenience sampling methodology was used to enroll Umrah pilgrims at their places of residence. After obtaining informed consent, a questionnaire was administered to pilgrims by the study team, collecting demographic, health and travel data as well as other information related to their stay in KSA. The questionnaire was produced and administered in English or Arabic. In case the pilgrim did not speak either languages, the questionnaire was administered through the pilgrim’s native language, via the study team or with the aid of a translator.
Sample Collection and Processing
For each participating pilgrim, an oropharyngeal swab was taken by trained staff and placed into transport media (∑-Transwab® MW176S, Medical Wire & Equipment, Wiltshire, UK). Swabs were transferred to be processed at the laboratory within 5 hrs (from collection to processing).
Microbiological Identification of Neisseria meningitidis
Swabs were plated on Neisseria selective agar plates (Thayer-Martin with VCNT antibiotic supplement, Merck Life Science UK Limited, Dorset, UK) and incubated for 48 hrs at 37°C in 5% CO2. The bacterial isolates were examined for purity and colony morphology and tested using Gram stain (Quimica Clinica Aplicada, S.A., Tarragona, Spain) and Kovac’s oxidase test (Biomerieux SA, Marcy l’Etoile, France). Gram-negative, oxidase-positive cocci of potential meningococcal colonies were subcultured on blood agar plates at 37°C in 5% CO2 for 24 hrs for biochemical identification using API® NHI test (Biomerieux SA, Marcy l’Etoile, France). N. meningitidis isolates were stored by freeze preservation at −80°C in tryptone soya broth (TSB) with skim milk and 15–20% glycerol.
Serogrouping of the Isolates
Capsular antigenic typing of isolated N. meningitidis was performed using slide coagglutination test using commercially available N. meningitidis antisera and according to the manufacturer’s instructions (Difco, Sparks, USA). Serogrouping was performed for the following serogroups: A, B, C, D, W, Y, X, and Z. Positive controls (provided by the Saudi Ministry of Health, Riyadh, KSA) were included for quality control.
Antimicrobial Susceptibility Testing
E-tests were used to determine susceptibility to nine antibiotics according to the manufacturer’s instructions (Biomerieux SA, Marcy l’Etoile, France). Briefly, isolates were first subcultured onto blood agar plates, and a standard inoculum (0,5 McFarland) was used for the tests. Plates were inoculated and then incubated in an inverted position in a 5% CO2 atmosphere for 24 hrs at 37°C. The minimum inhibitory concentration (MIC), in µg/mL, for each antibiotic was then determined. The antibiotics tested were as follows: Benzylpenicillin, Azithromycin, Cefotaxime, Ceftriaxone, Trimethoprim-Sulfamethoxazole, Ciprofloxacin, Rifampicin, Amoxicillin and Ampicillin. Breakpoints of the Clinical & Laboratory Standards Institute (CLSI) (Performance Standards for Antimicrobial Susceptibility Testing, 31st Edition, 2021) were used for azithromycin and trimethoprim-sulfamethoxazole. The interpretive standards and MIC breakpoints recommended by the European Committee on Antimicrobial Susceptibility Testing (EUCAST) (Version 11, 2021) were used for the rest of the antibiotics.
Results
Characteristics of the Study Population and Stay in KSA
The study enrolled 616 Umrah pilgrims originating from 17 countries in the Middle East, South Asia, Africa and Europe (Table 1), mainly Algeria, Iraq and Sudan (Figure 1). The study population had a mean age of 53.8 years (± 13.1, range = 19–91) and a male-to-female ratio of 1.1:1. Nearly 39% of the respondents had no formal education and 32.5% declared having an underlying health condition (Table 1). Hypertension and diabetes were the most common comorbidities present, respectively, in 58.9% and 53.8% of those with underlying health conditions. A minority of pilgrims (4.7%) reported having a status that increases their risk of N. meningitidis carriage (ie, healthcare worker, student, and military recruit).
 |  |  |
Table 1 Characteristics of the Umrah Pilgrims Enrolled in the Study |
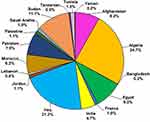 |
Figure 1 Country of residence of the enrolled 2019 Umrah pilgrims. |
Nearly 8% of the respondents declared that they were smokers and have been smoking for 2–50 years (mean = 25.7 years, ±13.5). Another 9% reported having smoked in the past but had stopped. Travel information indicated that 36 (5.9%) respondents had traveled outside their country of residence in the previous 6 months, visiting countries in Africa, Asia, the Middle East, Europe and the USA. Similarly, 9.3% of pilgrims declared visiting Saudi Arabia in the previous year, mainly to perform Umrah (Table 1).
Information on vaccination status was available for a minority of pilgrims, all of whom declared having received meningococcal (56 pilgrims), yellow fever (55 pilgrims), or influenza (12 pilgrims) vaccines. Of those reporting meningococcal vaccination, eight also reported the type of vaccine taken, all of whom received the conjugate ACWY vaccine. The reported mean time between meningococcal vaccination and arrival to KSA was 44.1 days (±51.1, range 10–202). The majority (87.3%) of pilgrims reporting yellow fever vaccination were from Sudan.
With the exception of six KSA residents, at the time of recruitment, pilgrims had spent a mean of 9 days in Saudi Arabia (±4.5, range 1–45 days). Most pilgrims (95.5%) declared that they did visit or plan to visit the holy city of Medina as part of their Umrah. Similarly, the majority of pilgrims (98.5%) reported never using a face mask during their Umrah stay and 34.6% declared suffering from influenza-like symptoms at the time of enrolment (Figure 2). These were mainly cough (50.7%), sore throat (28.7%) and muscle/joint ache (21.5%). Antibiotic use was reported by 11.8% of pilgrims, mainly ciprofloxacin (50%) and amoxicillin (22.4%). Pilgrims who reported having taken ciprofloxacin were mostly from Iraq (55.5%) or Sudan (33.3%).
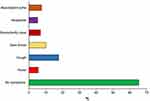 |
Figure 2 Influenza-like symptoms among the enrolled 2019 Umrah pilgrims. |
Culture results
Of the 616 swabs cultured on Thayer-Martin selective agar, 61 (9.9%) showed bacterial growth (Table 2). Neisseria genus was the most common accounting for 54.1% of all growth on the selective agar, followed by Haemophilus (24.6%) and Moraxella (21.3%). N. meningitidis represented only 4.9% of all growth on Thayer-Martin agar and its carriage rate among the Umrah pilgrims was 0.49% (3/616). The most commonly carried organisms were Neisseria spp. (3.25%), H. influenzae (2.27%) and Moraxella spp. (1.62%). Among the identified N. meningitidis, 2 (66.7%) were serogroup A, and 1 (33.3%) was serogroup B. Hence, the overall carriage rates of these serogroups among pilgrims were 0.32% and 0.16%, respectively.
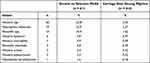 |
Table 2 Bacteria Isolated from Oropharyngeal Swabs Obtained from Umrah Pilgrims |
Antimicrobial Susceptibility
Only one of the three N. meningitidis isolates (serogroups B) was available for antimicrobial susceptibility testing (Table 3). The isolate was sensitive to the tested penicillins, 3rd-generation cephalosporins, rifampicin and the macrolide azithromycin but was resistant to ciprofloxacin and showed decreased susceptibility to trimethoprim-sulfamethoxazole.
 |
Table 3 Antimicrobial Susceptibility of Neisseria meningitidis Serogroup B Isolated During the Umrah Study |
Characteristics of N. meningitidis Carriers
Characteristics of the three N. meningitidis carriers are presented in Table 4. Pilgrims were older in age, nationals of Algeria, India and Afghanistan and had spent 8–12 days in KSA at the time of enrolment. None of the carriers had formal education, traveled outside their country of residency in the previous 6 months or traveled to KSA in the previous year. At the time of the study, one carrier was a smoker and another declared having influenza-like symptoms. None of the carriers used antibiotics, and all shared accommodation with 3–4 people during their Umrah stay. Carriers did not report their vaccination status.
 |
Table 4 Characteristics of Neisseria meningitidis Carriers During Umrah |
Discussion
In this cross-sectional study, we investigated the carriage of N. meningitidis among Umrah pilgrims in 2019. We report a low carriage rate and identified three isolates: two serogroup A and one serogroup B. The latter was sensitive to antibiotics used for meningococcal disease therapy but showed resistance or reduced susceptibility to some agents used for chemoprophylaxis including ciprofloxacin. Most Umrah pilgrims reported sharing accommodation and visiting Medina during their pilgrimage. Also, the majority did not wear facemasks during the event and a sizable proportion reported suffering influenza-like symptoms and taking antibiotics.
Meningococcal disease and outbreaks have been reported in various mass gatherings including during the Hajj and Umrah pilgrimages.5,7,12 Umrah-associated outbreaks occurred mainly during the early 1990s and were principally due to serogroup A.7 Strict preventive measures including compulsory vaccination with the quadrivalent vaccine eliminated such outbreaks at these events.7,8 However, meningococcal disease remains an important public health threat at Umrah due in part to the evolving epidemiology of the disease and the presence of risk factors. In addition, the current Umrah meningococcal disease preventative measures do not protect against all invasive serogroups and do not necessarily affect carriage and transmission as the polysaccharide vaccine is still widely used.8,11 Moreover, increased prevalence of antibiotic resistance among N. meningitidis isolates worldwide, including Muslim-majority countries, is concerning.12–14 Given the lack of meningococcal disease cases in Umrah in recent years, surveillance and tracking of carrier state among pilgrims and investigating the antimicrobial susceptibility profiles of carried isolates are important.
In the current study, carriage rate of N. meningitidis among Umrah pilgrims was low (0.5%), and all isolates were invasive serogroups. The rate is lower than those previously reported among Umrah or Hajj pilgrims but in line with low carriage rates found in recent studies among these populations.9,10,15,16 Wilder-Smith et al investigated 160 Singaporean pilgrims returning from Umrah in 2001,9 post the serogroup W Hajj-associated outbreak.7 The carriage rate was only 1.3%, significantly lower than that found in returning Singaporean Hajj pilgrims (17%; p < 0.001) in the same year.17 None of the Umrah pilgrims carried serogroup W, whereas 90% of the isolates from returning Hajj pilgrims were serogroup W. Ashgar et al reported an overall carriage rate of N. meningitidis of 4% among Umrah visitors compared to 7.3% (p < 0.0001) among Hajj pilgrims in 2009.10 The carriage rate increased from 2.4% before Umrah to 5.7% after Umrah. Out of the 80 N. meningitidis isolated from Umrah pilgrims, 10% were serogroup B and 2.5% were serogroup W, respectively. The differences in carriage rates observed between Hajj and Umrah may be explained by the fact that the length and intensity of interaction among pilgrims during the Hajj is greater than that during the Umrah. The use of only culture methods to detect N. meningitidis, the fact that most of our study population were older adults, and the increased use of the conjugate vaccine among pilgrims in recent years, could all have contributed to the low carriage rate observed in our study compared to older reports.
All isolates in our study were invasive serogroups including one serogroup B. The current compulsory Hajj and Umrah meningococcal vaccines do not cover serogroup B.11 The latter has been increasingly isolated at higher proportions among Hajj pilgrims, both before Hajj and among returning pilgrims.15,16,18,19 Tezer et al investigated N. meningitidis carriage among 229 Turkish Hajj pilgrims vaccinated with the quadrivalent conjugate vaccine pre and post the 2018 Hajj. Carriage rate was 3.9% at the time of departure with all positive samples being serogroup B. Upon returning to Turkey,1 (0.4%) pilgrim, who was not a carrier before the pilgrimage, was positive for serogroup B.18 Importation, acquisition and transmission of serogroup B is a major threat at both Hajj and Umrah given the potential for serogroup B disease and outbreaks at these events and the increase prevalence of serogroup B disease worldwide.4,11 Due to lack of information on vaccination among carriers in our study, it is not possible to ascertain the impact of the meningococcal vaccine technology on carriage. A recent study did not find a significant association between the type of vaccine used and N. meningitidis carriage among Hajj pilgrims.16 Moreover, a systematic review conducted in 2020 did not find evidence of reduction in carriage for multivalent ACWY or serogroup B vaccines.20
Umrah pilgrims in our study originated from 17 countries in South Asia, Africa, Europe and the Middle East, reflecting the international nature of the pilgrimage.6,10,21 Pilgrims were generally older males, with a significant proportion having low or no formal education and underlying health conditions (mainly diabetes and hypertension). These results are similar to what was reported from other Hajj and Umrah studies.21–24 In one cross-sectional survey among 1012 Umrah pilgrims in 2019, participants represented 41 nationalities, 65% were male, 33% were ≥50 years old, and 38.5% had secondary or lower education.21 In our study, 32.5% of participants reported having underlying health conditions which is comparable to that reported in studies of Umrah pilgrims from Egypt (35%),24 Malaysia (25%),23 and various nationalities (38%).21
Data on vaccination status was collected from a small number of pilgrims who reported being vaccinated against meningococcal disease, yellow fever or influenza. Rates of vaccination with the mandatory meningococcal vaccine were reported to be high among Hajj pilgrims, but lower among Umrah pilgrims.15,21,25 One study in 2019 found that only 41.3% of Umrah pilgrims reported meningococcal disease vaccination, while the rate was even lower (30%) among Malaysian pilgrims in 2018.21,25 For other vaccines, studies from both Hajj and Umrah report a low uptake of non-compulsory vaccination among pilgrims, although the uptake is slightly higher among the at-risk populations.21,23,26–28 For instance, recent studies among Umrah pilgrims reported that the uptake rate of influenza and pneumococcal vaccinations were 14.5–51% and 12–27.6%, respectively.21,23,25,26 In light of the above, the small number of respondents in our study and the potential for recall bias, our results are likely to be an overestimation, particularly for non-compulsory vaccinations.
Given the small number of isolates identified, we did not investigate factors associated with carriage of N. meningitidis. A recent report among Hajj pilgrims found that gender, age, education level, smoking status, antibiotic use, length of stay in KSA, vaccine type and timing as well as the number of pilgrims in shared accommodation had no statistically significant impact on N. meningitidis carriage.16 However, many of the above factors, including crowding, age, gender and smoking, have been reported as risk factors for meningococcal carriage and disease in other settings.2,29–31 We found that the majority of pilgrims shared accommodation during Umrah, visited or planned to visit Medina and reported never wearing a mask during the pilgrimage. In another study from Umrah 2019, all respondents reported visiting Medina during their pilgrimage and 30.1% never wore a face mask in crowded areas during Umrah.21 These factors can increase the risk of transmission of respiratory pathogens among pilgrims. The lack of mask wearing in our study is particularly relevant given that more than a third of pilgrims were suffering from influenza-like symptoms and that concurrent upper respiratory infections increase the risk of meningococcal carriage and disease.2,32 Studies from Hajj reported that use of face masks can lead to a substantial decrease in the incidence of influenza-like illness among pilgrims.33,34 Therefore, pilgrims’ attitude to face mask wearing requires further investigations to improve uptake.
The one isolate investigated for antibiotic susceptibility was sensitive to the tested penicillins, 3rd-generation cephalosporins, rifampicin and azithromycin but exhibited resistance to ciprofloxacin and decreased susceptibility to trimethoprim-sulfamethoxazole. In a study conducted in 2009, all 80 N. meningitidis isolates from Umrah pilgrims were susceptible to cefotaxime, ceftriaxone and meropenem. Resistance to ciprofloxacin, azithromycin and rifampicin was reported in 3.8%, 6.3% and 3.8% of the isolates, respectively.10 Although antibiotic use is associated with lower N. meningitidis carriage rate,35,36 overuse and misuse of these agents is driving antibiotic resistance worldwide. We report that 11.2% of participants used antibiotics during Umrah, which is slightly higher than what reported in 2001 (7%) but lower than what is observed in Hajj.9,37 Ciprofloxacin resistance is mainly linked to mutation in the gyrA gene, while resistance to trimethoprim-sulfamethoxazole or sulfisoxazole has been attributed to folP gene polymorphisms.38,39 Ciprofloxacin-resistant N. meningitidis is an ongoing concern with isolated identified worldwide in recent years.39 Identification of ciprofloxacin-resistance in our study is particularly relevant as the agent is the antibiotic of choice used for chemoprophylaxis as part of the Hajj and Umrah meningococcal disease preventive measures.8
Our study has a number of limitations. The cross-sectional study design and the enrollment strategy, including the potential for volunteer bias, limit the generalizability of our findings. In addition, we used questionnaires to collect data; therefore, responses obtained were prone to information bias and some sections of the questionnaire, such as vaccination status, had a low response rate. Also, we used culture-based methods to isolate N. meningitidis. Using molecular techniques in combination with culture would have resulted in a better sensitivity. Finally, we were able to subculture only one of the three N. meningitidis isolates for antimicrobial susceptibility testing, hence we did not report results for the other two isolates.
In summary, we investigate meningococcal carriage among Umrah pilgrims in 2019 just before the height of the COVID-19 pandemic. We report low carriage rate of N. meningitidis but the presence of invasive serogroups including serogroup B, which is not covered in the current compulsory vaccines for the pilgrimage. Umrah conditions such as crowding, shared accommodations and travel between holy sites can facilitate transmission of N. meningitidis among pilgrims and local residents and could potentially lead to disease and outbreaks including internationally via returning pilgrims. Preventive measures against respiratory infections are currently heightened, given the COVID-19 pandemic; however, these should be monitored post pandemic to ensure pilgrims continue to exhibit good practice. Health awareness campaigns on meningococcal disease preventive measures among Umrah pilgrims should aim to improve knowledge and affect practice and should be administered to pilgrims before departure to KSA and information reinforced during their stay in the country. In addition, given reports of non-optimum uptake of the meningococcal vaccine, ensuring the stricter implementation of compulsory vaccination among Umrah pilgrims is a priority.
Ethics Approval and Consent to Participate
The study was approved by the King Fahad Medical City Ethics Committee and the Institutional Review Board (IRB log: 18-423E) and was performed in accordance with the relevant guidelines and regulations and in compliance with the Declaration of Helsinki. The Ethics Committee and IRB approved verbal consent process for participation given the observational nature of the study and the use of anonymous questionnaires, which did not include any identifiers or personal information of the participants. Trained researchers obtained verbal consent from all participants and documented it on the survey forms.
Funding
This work was supported by Pfizer Pharmaceuticals (grant number WI224461).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Rouphael NG, Stephens DS. Neisseria meningitidis: biology, microbiology, and epidemiology. Methods Mol Biol. 2012;799:1–20.
2. Yazdankhah SP, Caugant DA. Neisseria meningitidis: an overview of the carriage state. J Med Microbiol. 2004;53(Pt 9):821–832. doi:10.1099/jmm.0.45529-0
3. Harrison LH, Trotter CL, Ramsay ME. Global epidemiology of meningococcal disease. Vaccine. 2009;27(Suppl 2):B51–B63. doi:10.1016/j.vaccine.2009.04.063
4. Yezli S. The threat of meningococcal disease during the Hajj and Umrah mass gatherings: a comprehensive review. Travel Med Infect Dis. 2018;24:51–58. doi:10.1016/j.tmaid.2018.05.003
5. Badahdah AM, Rashid H, Khatami A, Booy R. Meningococcal disease burden and transmission in crowded settings and mass gatherings other than Hajj/Umrah: a systematic review. Vaccine. 2018;36(31):4593–4602. doi:10.1016/j.vaccine.2018.06.027
6. Yezli S, Yassin Y, Awam A, Attar A, Al-Jahdali E, Umrah AB. An opportunity for mass gatherings health research. Saudi Med J. 2017;38(8):868–871. doi:10.15537/smj.2017.8.20124
7. Yezli S, Assiri AM, Alhakeem RF, Turkistani AM, Alotaibi B. Meningococcal disease during the Hajj and Umrah mass gatherings. Int J Infect Dis. 2016;47:60–64. doi:10.1016/j.ijid.2016.04.007
8. Yezli S, Bin Saeed AA, Assiri AM, et al. Prevention of meningococcal disease during the Hajj and Umrah mass gatherings: past and current measures and future prospects. Int J Infect Dis. 2016;47:71–78. doi:10.1016/j.ijid.2015.12.010
9. Wilder-Smith A, Paton NI, Barkham TM, Earnest A. Meningococcal carriage in Umrah pilgrims returning from Saudi Arabia. J Travel Med. 2003;10(3):147–149. doi:10.2310/7060.2003.35751
10. Ashgar S, El-Said H, Johargy A, et al. Prevalence of nasal carriage of Neisseria meningitidis among Umrah visitors and pilgrims during Umrah and Hajj season. Glo Adv Res J Microbiol. 2013;2:141–149.
11. Yezli S, Alotaibi B. Meningococcal disease during the Hajj and Umrah mass gatherings: a, C, W, Y may be covered but don’t forget the B and X factors! Travel Med Infect Dis. 2017;15:5–7. doi:10.1016/j.tmaid.2017.02.001
12. Aye AMM, Bai X, Borrow R, et al. Meningococcal disease surveillance in the Asia-Pacific region (2020): the global meningococcal initiative. J Infect. 2020;81(5):698–711. doi:10.1016/j.jinf.2020.07.025
13. Willerton L, Lucidarme J, Walker A, et al. Antibiotic resistance among invasive Neisseria meningitidis isolates in England, Wales and Northern Ireland (2010/11 to 2018/19). PLoS One. 2021;16(11):e0260677. doi:10.1371/journal.pone.0260677
14. Vacca P, Fazio C, Neri A, Ambrosio L, Palmieri A, Stefanelli P. Neisseria meningitidis antimicrobial resistance in Italy, 2006 to 2016. Antimicrob Agents Chemother. 2018;62(9):e00207–e00218.
15. Yezli S, Wilder-Smith A, Bin Saeed AA. Carriage of Neisseria meningitidis in the Hajj and Umrah mass gatherings. Int J Infect Dis. 2016;47:65–70. doi:10.1016/j.ijid.2015.11.014
16. Alasmari A, Houghton J, Greenwood B, et al. Meningococcal carriage among Hajj pilgrims, risk factors for carriage and records of vaccination: a study of pilgrims to Mecca. Trop Med Int Health. 2021;26(4):453–461. doi:10.1111/tmi.13546
17. Wilder-Smith A, Barkham TM, Earnest A, Paton NI. Acquisition of W135 meningococcal carriage in Hajj pilgrims and transmission to household contacts: prospective study. BMJ. 2002;325(7360):365–366. doi:10.1136/bmj.325.7360.365
18. Tezer H, Gulhan B, Simge Gisi A, et al. The impact of meningococcal conjugate vaccine (MenACWY-TT) on meningococcal carriage in Hajj Pilgrims returning to Turkey. Hum Vaccin Immunother. 2020;16(6):1268–1271. doi:10.1080/21645515.2019.1680084
19. Memish ZA, Al-Tawfiq JA, Almasri M, et al. Neisseria meningitidis nasopharyngeal carriage during the Hajj: a cohort study evaluating the need for ciprofloxacin prophylaxis. Vaccine. 2017;35(18):2473–2478. doi:10.1016/j.vaccine.2017.03.027
20. McMillan M, Chandrakumar A, Wang HLR, et al. Effectiveness of meningococcal vaccines at reducing invasive meningococcal disease and pharyngeal Neisseria meningitidis carriage: a systematic review and meta-analysis. Clin Infect Dis. 2021;73(3):e609–e619. doi:10.1093/cid/ciaa1733
21. Tobaiqy M, Alhasan AH, Shams MM, et al. Assessment of preventative measures practice among Umrah Pilgrims in Saudi Arabia, 1440H-2019. Int J Environ Res Public Health. 2020;18(1):257.
22. Yezli S, Mushi A, Almuzaini Y, Balkhi B, Yassin Y, Khan A. Prevalence of diabetes and hypertension among Hajj pilgrims: a systematic review. Int J Environ Res Public Health. 2021;18(3):1155.
23. Goni MD, Naing NN, Hasan H, et al. Uptake of recommended vaccines and its associated factors among Malaysian pilgrims during Hajj and Umrah 2018. Front Public Health. 2019;7:268. doi:10.3389/fpubh.2019.00268
24. Aziz MM, Abd El-Megeed HS, Abd Ellatif MAM. Pre-travel health seeking practices of Umrah pilgrims departing from Assiut International Airport, Egypt. Travel Med Infect Dis. 2018;23:72–76. doi:10.1016/j.tmaid.2018.04.012
25. Goni MD, Naing NN, Hasan H, et al. A confirmatory factor analysis of the knowledge, attitude and practice questionnaire towards prevention of respiratory tract infections during Hajj and Umrah. BMC Public Health. 2020;20(1):1684. doi:10.1186/s12889-020-09756-5
26. Dauda Goni M, Hasan H, Naing NN, et al. Assessment of knowledge, attitude and practice towards prevention of respiratory tract infections among Hajj and Umrah pilgrims from Malaysia in 2018. Int J Environ Res Public Health. 2019;16(22):4569.
27. Edouard S, Al-Tawfiq JA, Memish ZA, Yezli S, Gautret P. Impact of the Hajj on pneumococcal carriage and the effect of various pneumococcal vaccines. Vaccine. 2018;36(48):7415–7422. doi:10.1016/j.vaccine.2018.09.017
28. Alqahtani AS, Althimiri NA, BinDhim NF. Saudi Hajj pilgrims’ preparation and uptake of health preventive measures during Hajj 2017. J Infect Public Health. 2019;12(6):772–776. doi:10.1016/j.jiph.2019.04.007
29. Miglietta A, Innocenti F, Pezzotti P, et al. Carriage rates and risk factors during an outbreak of invasive meningococcal disease due to Neisseria meningitidis serogroup C ST-11 (cc11) in Tuscany, Italy: a cross-sectional study. BMC Infect Dis. 2019;19(1):29. doi:10.1186/s12879-018-3598-3
30. Davies AL, O’Flanagan D, Salmon RL, Coleman TJ. Risk factors for Neisseria meningitidis carriage in a school during a community outbreak of meningococcal infection. Epidemiol Infect. 1996;117(2):259–266. doi:10.1017/S0950268800001436
31. Stuart JM, Cartwright KA, Robinson PM, Noah ND. Effect of smoking on meningococcal carriage. Lancet. 1989;2(8665):723–725. doi:10.1016/S0140-6736(89)90781-2
32. Rosenstein NE, Perkins BA, Stephens DS, Popovic T, Hughes JM. Meningococcal disease. N Engl J Med. 2001;344(18):1378–1388. doi:10.1056/NEJM200105033441807
33. Choudhry AJ, Al-Mudaimegh KS, Turkistani AM, Al-Hamdan NA. Hajj-associated acute respiratory infection among hajjis from Riyadh. East Mediterr Health J. 2006;12(3–4):300–309.
34. Barasheed O, Almasri N, Badahdah AM, et al. Pilot randomised controlled trial to test effectiveness of facemasks in preventing influenza-like illness transmission among Australian Hajj Pilgrims in 2011. Infect Disord Drug Targets. 2014;14(2):110–116. doi:10.2174/1871526514666141021112855
35. He F, Yang HM, Li GM, et al. Neisseria meningitidis carriage and risk factors among teenagers in Suizhou city in China. Epidemiol Infect. 2020;148:e227. doi:10.1017/S0950268820002113
36. Cooper LV, Robson A, Trotter CL, et al. Risk factors for acquisition of meningococcal carriage in the African meningitis belt. Trop Med Int Health. 2019;24(4):392–400. doi:10.1111/tmi.13203
37. Hoang VT, Nguyen TT, Belhouchat K, et al. Antibiotic use for respiratory infections among Hajj pilgrims: a cohort survey and review of the literature. Travel Med Infect Dis. 2019;30:39–45. doi:10.1016/j.tmaid.2019.06.007
38. Fiebelkorn KR, Crawford SA, Jorgensen JH. Mutations in folP associated with elevated sulfonamide MICs for Neisseria meningitidis clinical isolates from five continents. Antimicrob Agents Chemother. 2005;49(2):536–540. doi:10.1128/AAC.49.2.536-540.2005
39. Alderson MR, Arkwright PD, Bai X, et al. Surveillance and control of meningococcal disease in the COVID-19 era: a Global Meningococcal Initiative review. J Infect. 2021;84(3):289–296. doi:10.1016/j.jinf.2021.11.016
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
