Back to Journals » Risk Management and Healthcare Policy » Volume 15
Caries Risk Assessment and Dental Referral by Paediatric Primary Care Physicians in Sichuan Province, China: A Cross-Sectional Study
Authors Wang Q, Qu X , Houser SH, Zhang Y, Tian M, Zhang Q, Zhang W
Received 17 February 2022
Accepted for publication 8 August 2022
Published 3 September 2022 Volume 2022:15 Pages 1641—1650
DOI https://doi.org/10.2147/RMHP.S362004
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Kyriakos Souliotis
Qingyu Wang,1,2 Xing Qu,3 Shannon H Houser,4 Yan Zhang,5 Meirong Tian,3 Qiong Zhang,6,7 Wei Zhang3
1West China School of Public Health and West China Fourth Hospital, Sichuan University, Chengdu, People’s Republic of China; 2HEOA Group, Institute for Healthy Cities and West China Research Center for Rural Health Development, Sichuan University, Chengdu, People’s Republic of China; 3Institute of Hospital Management, West China Hospital, Sichuan University, Chengdu, People’s Republic of China; 4Department of Health Services Administration, the University of Alabama at Birmingham, Birmingham, AL, USA; 5Department of Maternity and Child Health Management, Sichuan Provincial Maternity and Child Health Care Hospital, Chengdu, People’s Republic of China; 6Department of Pediatric Dentistry, West China Hospital of Stomatology, Sichuan University, Chengdu, People’s Republic of China; 7State Key Laboratory of Oral Diseases & National Clinical Research, Sichuan University, Chengdu, People’s Republic of China
Correspondence: Xing Qu, Institute of Hospital Management, West China Hospital, Sichuan University, No. 37 Guoxue Lane, Chengdu, 610041, People’s Republic of China, +86 13880713452, Email [email protected]
Background: Limited information is known about dental implementation by pediatric primary care physicians (PCPs) at the primary care level in China. This study aimed to explore the current status of primary oral care implementation and related influencing factors.
Methods: A cross-sectional survey was conducted among PCPs in Sichuan Province, China. Multivariable logistic regression was used to analyse factors associated with CRA and dental referral for high caries-risk children.
Results: A total of 504 out of 524 questionnaires remained for analysis. In all, 93.8% of PCPs reported that they usually or sometimes performed dental screening for children, 31.3% performed CRA, and 49.0% referred high caries-risk children to dentists. More CRA activities were associated with PCPs who encountered a greater number of children with caries during systematic care (adjusted OR: 2.37, 95% CI:[1.08,5.18], had dental knowledge training by pediatric dentists (aOR: 2.26, 95% CI:[1.36, 3.75], and learned pediatric dental knowledge on their own (aOR: 2.87, 95% CI: [1.51, 5.45]). In addition to the above associators, a higher rate of dental referrals for high caries-risk children was associated with having a dental department in the same work institute (aOR: 1.72, 95% CI: [1.09, 2.70] and having more confidence in their dental knowledge (aOR: 1.29, 95% CI: [1.04, 1.61]).
Conclusion: Paediatric PCPs commonly implement dental screening but perform fewer CRAs and dental referrals for high caries-risk children during systematic health management in western China. To increase CRA activities and dental referral by paediatric PCPs, health policymakers could encourage interdisciplinary cooperation between dental professionals and paediatric PCPs.
Keywords: caries risk assessment, dental referral, paediatric physicians, primary care, China
Background
Early childhood caries (ECC) is one of the most prevalent diseases in children worldwide, especially in low-income and middle-income countries.1,2 The Fourth Chinese National Oral Health Survey in 2015 reported that 71.9% of 5-year-old children suffered dental caries, yet 95.9% of them were untreated.3 ECC produces pain and difficulty chewing, which may lead to malnutrition, gastrointestinal disorders, difficulty sleeping and social interactions.4 Multiple factors contribute to the prevalence of ECC, such as excessive intake of sugary food interacting with salivary Streptococcus mutans,5 poor oral hygiene habits, lower dental office accessibility, lower family income and other sociobehavioural risk factors.6 Many comprehensive interventions could be implemented to prevent ECC. Public health approaches as one of the interventions, including the education of parents on knowledge of dental health, promotion of parental oral-related behaviours, increasing dental care access, and strengthening interdisciplinary cooperation, would help to prevent the common risk factors for ECC.7–10 For example, during the initial years of the Childsmile intervention programme funded by the Scottish government, which aimed to facilitate the provision of appropriate needs-based oral health support to infants and their families from the earliest age, reductions in the prevalence and morbidity of dental decay were seen in all socioeconomic groups.11 A study from Hong Kong also implied that educated parents with oral health knowledge in kindergarten may prevent ECC among preschool children.12 Multidisciplinary work, such as dental practice implementation by primary care workers addressing common risk factors, could promote even better results regarding caries prevention and control for younger children.13,14 The number of factors to adopt preventive dental procedures in primary care practices is associated with dental care implementation.15,16 Understanding the gaps in dental implementation by pediatric primary care physicians (PCPs) is important to establish public health strategies and multidisciplinary cooperative plans to improve children’s oral health from the perspective of primary care.
In China, there were 8 million 0- to 4-year-old children in 2019.17 The prevention and control of ECC for Chinese children are critical to contributing to a decrease in the global dental caries burden. As the Chinese economy has developed rapidly in recent years, sugar consumption has risen, along with living standards.18 Prevention of ECC remains a great challenge. Realizing this situation, the Chinese Health Committee raised the Healthy China Programme and Healthy Oral Action Plan 2019–2025 to emphasize the prevention of ECC in early life.19,20 The target of this Action Plan aimed to reduce dental caries from 34.5% in 2016 to 30% in 2025 among 12-year-old children. Meanwhile, the Chinese government issued the “National Children’s Oral Disease Comprehensive Intervention Project Work Specifications”, which requires all PCPs involved in intervention projects to be trained and obtain a physician’s medical licence.21,22 The government regularly monitored the effectiveness of intervention in the community health centre, such as PCPs’ oral health knowledge, the rate of dental screening, dental caries prevalence, and fit and sealant rate. Before these oral health-targeted programs, a systematic health management program, as an essential component of the National Public Health Services for children in China, covered all children under six years old in primary care settings.23 According to the National Standard for Basic Public Health Services for Children, pediatric PCPs should examine, evaluate, give appropriate dental advice, and make necessary dental referrals for enrolled children during systematic health management visits.23 This project required that the rate of dental screening for children reach 90%. The government budget for community health centres would be curtailed if the PCPs did not pass the spot check. In 2018, the national coverage of systematic management for children under three reached 91.2%.24 However, no study has reported current dental examination-related behaviours by Chinese paediatric PCPs until now. Identifying the real situation of oral care implementation will help to make targeted promotion strategies.
In this study, we aimed to 1) identify the implementation of dental screening, dental caries risk assessment (CRA), and dental referral activities by PCPs and 2) explore the factors associated with CRA and dental referrals for high caries-risk children in western China.
Methods
Ethical Approval
Ethical approval was obtained from the Institutional Review Board of Stomatology School, Sichuan University (IRB reference number: WCHSIRB-D-2019-013). A written informed consent form was sent to the respondents to explain the content of the survey. Each respondent signed an electronic informed consent form.
Study Population
We conducted a cross-sectional survey to collect information about CRA and dental referral behaviours by paediatric PCPs in August 2021 in Chengdu, Sichuan Province, China. An electronic structured questionnaire was sent through the WeChat work group, which is one of the most common multipurpose platforms used for communication in China,25 of the Sichuan Maternal and Child Health Academic Association. Such an association is a professional academic association gathering pediatric physicians and assistance for daily work communication in Sichuan Province. Since not all pediatric PCPs were in the WeChat group of the Sichuan Maternal and Child Health Academic Association, we used snowball sampling as an assistant sampling method.26 All active pediatric PCPs could be enrolled. To guarantee enough participants, we sent questionnaires two times a week during August 2021. The sample size was calculated via the formula 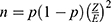 , where Z is the value from the standard normal distribution reflecting the confidence level that will be used (Z = 1.96 for 95%) and E is the desired margin of error (E = 0.5). P is the proportion of successes in the population. The value of p that maximizes p(1-p) is p = 0.5. We had no information on the proportion of pediatric primary care patients who received dental care, so we used 0.5 to estimate the maximum sample size. Since there are no statistical data for pediatric PCPs, we used the number of pediatricians and general physicians for estimation. According to the Statistical Yearbook 2018 of the Sichuan Health Commission,27 the number of pediatricians was 6467, and the number of general physicians was 2745. We took 80% of them as the primary physicians (N=7370). The minimum sample size in this study was 366. Before the formal survey, we conducted a pilot survey among a limited population. We asked five paediatric PCPs and two dentists to complete the questionnaire and collect feedback. Then, we made a revision to ensure that the questions could be fully understood.
, where Z is the value from the standard normal distribution reflecting the confidence level that will be used (Z = 1.96 for 95%) and E is the desired margin of error (E = 0.5). P is the proportion of successes in the population. The value of p that maximizes p(1-p) is p = 0.5. We had no information on the proportion of pediatric primary care patients who received dental care, so we used 0.5 to estimate the maximum sample size. Since there are no statistical data for pediatric PCPs, we used the number of pediatricians and general physicians for estimation. According to the Statistical Yearbook 2018 of the Sichuan Health Commission,27 the number of pediatricians was 6467, and the number of general physicians was 2745. We took 80% of them as the primary physicians (N=7370). The minimum sample size in this study was 366. Before the formal survey, we conducted a pilot survey among a limited population. We asked five paediatric PCPs and two dentists to complete the questionnaire and collect feedback. Then, we made a revision to ensure that the questions could be fully understood.
Measurements of Dental Screening, Caries Risk Assessment Activities, and Dental Referral
We measured dental screening activities by the question “Did you check dental caries for children who came for systematic health visits?” Likert scale options were set to the question “usual, sometimes, occasional, and never”.
The activities of CRAs were measured according to the Caries-risk Assessment Form for 0- to 3-year-olds from the American Academy of Pediatric Dentistry (AAPD).28 The following questions were used to collect CRA activities information:
Have you asked parents the following questions: 1) how often did your child eat sugary foods in a recent month; 2) does your child use fluoride toothpaste in a recent month; 3) did you take your child visit a dentist regularly; 4) does your child sleep with a bottle in a recent month, and 5) does child’s mom have any untreated dental caries.
The options were “usual”, “sometimes”, “occasional”, and “never”. The options “usual” and “sometimes” were assigned a value of one; “occasional” and “never” were assigned a value of zero during analysis. Therefore, the range of the CRA score was 0–5. We considered the PCPs to have complete CRA activities if the cumulative scores were equal to 5, which is the highest score, to eliminate social desirability bias.29
The dental referral was represented by the questions
Would you refer the child to a dentist if the child was in the following situation: (1) when the child’s teeth were erupting; (2) when the child is approaching his/her 1st birthday; (3) when white spots were on the child’s teeth; (4) the child had dental caries by dental screening; (5) when the child had dentition problems; (6) when child’s parents said sleeping with a bottle; and (7) never brushes his teeth.
The options “usual” and “sometimes” were assigned a value of one, and “occasional” and “never” were assigned a value of zero. Questions (1)(2) represent the recommended time to establish a dental home,30 (3)(6)(7) represent children with high caries risk, and (4)(5) represent children who have existing caries. If the cumulative scores of (3), (6), and (7) equal 3, we considered that the PCPs had good dental referral activities for high caries-risk children.
Covariates
According to previous studies, dental screening and referral behaviour by PCPs for high caries-risk children may be associated with many factors.16,31 We adjusted these variables as covariates. Demographic information included sex (male or female), age (18–30 y, 31–40 y, 41–50 y, or 51–60 y), education level (two-year college and below, bachelor’s, master’s and above), length of work (<5 y, 5–10 y, 10–15 y, 15–20 y, or >20 y), and serve children counts per week (continuous variable). The working environments of PCPs included work institute level (community health service centre, township health centres, or well-child department in hospital), work institute type (public or private), whether they have a dental department in the same facility (yes or no), and whether there is cooperation with another dental clinic (yes or no). The self-confidence of PCPs concerning their dental knowledge (not at all, some confident, normal, very confident, or extremely confident (scored 1–5), whether they had pediatric dental knowledge training (by dental professionals, pediatric dentists, or yourself), and subjective feelings about dental referral difficulties (not at all, some difficult, normal, very difficult, or extremely difficult) were collected.
Furthermore, an open question, “Do you have any comments or suggestions about dental health promotion for children?”, was intended to collect qualitative information about dental care from the perspective of the pediatric PCP.
Statistical Analysis
Chi-squared test statistics were calculated to compare differences in demographic characteristics between those who performed different types of dental care activities among PCPs. Multivariable logistic regression was then used to analyse the associated factors for both CRA and dental referral for high caries-risk children. We used Cronbach’s alpha to estimate the reliability of the questionnaire and the Kaiser–Meyer–Olkin (KMO) measure of sampling adequacy to test the validation before multivariable analysis. The open-ended question was used to obtain further information about the dental care behaviour of PCPs. Their views about dental care behaviour were identified primarily in the process of collating and merging.
All data were analysed using SPSS 23.0 (IBM. Co). A value of P < 0.05 was considered statistically significant.
Results
A total of 524 questionnaires were collected. A total of 504 out of 524 questionnaires were maintained for analysis. Participants who chose to “serve no children per week” were excluded. If the participants chose “had no dental department in the same work facility” and then chose “prefer dental department in the same work facility”, the following question was considered an illogical response and was discarded. Then, we randomly selected forty-five (9%) participants to verify the response; 2 of them corrected a few pieces of information, and 43 were confirmed. Cronbach’s alpha was 0.882, indicating a high-level internal scale consistency. The KMO revealed an excellent value of 0.81, and Bartlett’s test of sphericity value was significant (3735, p =0.000), which indicated that the sampling was adequate.
Demographic Information of the Sampled Population
There were 471 (93.5%) females out of 504 PCPs who completed the questionnaire (Table 1). Of those, most participants (231, 45.8%) were aged 31–40 years. Two hundred and five (47.2%) participants had a bachelor’s or above education, 275 (55.5%) had more than ten years of work experience, 165 (32.7%) worked in community health centres, 137 (27.2%) worked in township health centres, and 202 (40.1%) worked in well-child departments of hospitals. The average number of children served by each PCP was 119 per week (SD: 114.1).
 |
Table 1 Chi-Square Analysis of Dental Care Practice in Different Demographic Groups |
Frequency of Dental Screening, CRA and Dental Referral
Among the total samples, almost all the PCPs reported that they performed dental screening for children during systematic health management (93.8%). Most PCPs asked children about bottle sleep status (81.9%) and frequency of sugar food intake (79.8%), and fewer PCPs cared about the mother’s caries status (49%). Only 31.3% of PCPs reported that they “usually or sometimes” had a complete CRA. Most PCPs reported that they usually or sometimes referred children who already had dental caries to dentists (96.2%). For children who were at high caries risk, 88.7% of PCPs reported they referred the children who had white spots on their teeth to the dentist but referred less for children who had bottle sleep (58.9%) and did not brush their teeth yet (60.7%). No more than half (49.0%) of the respondents could refer all high caries-risk children to the dentist (Table 2).
 |
Table 2 Frequency of Dental Screening, Caries Risk Assessment and Dental Referral for High Caries-Risk Children in the Total Sample |
Factors Associated with CRA and Dental Referral
Table 3 shows several factors associated with CRA and dental referral for high caries-risk children. Columns 2–4 indicate that a higher rate of CRA activities was significantly associated with encountering a greater amount of caries during visits for systematic care (aOR: 2.37, 95% CI: 1.08–5.18), having dental knowledge training by paediatric dentists (aOR: 2.26, 95% CI: 1.36–3.75), and learning paediatric dental knowledge on their own (aOR: 2.87, 95% CI: 1.51–5.45).
 |
Table 3 Results of Multivariable Logistic Regression of Factors Associated with Caries Risk Assessment and Dental Referral for High Caries-Risk Children |
Columns 5–7 indicate that a higher rate of dental referral for high caries-risk children was associated with having a dental department in the same work institute (aOR: 1.72, 95% CI: 1.09–2.70), a long distance from the capital city (aOR: 1.00, 95% CI: 1.00–1.00), usually encountering caries during well-child care visits (aOR: 1.88, 95% CI: 1.01–3.50), having training by a dentist (aOR: 1.86, 95% CI: 1.15–3.01), having pediatric dental knowledge training (aOR: 1.69, 95% CI: 1.04–2.74), and having more confidence about dental knowledge (aOR: 1.29, 95% CI: 1.04–1.61).
Qualitative Information Analysis
A total of 154 responses to the open-ended questions were analysed. Most respondents showed a positive attitude towards dental care for children. Typical answers included the following:
Dental Care Trainings and Communications
Lacking systematic paediatric dental knowledge hinders me from giving the correct information to parents. Training from dentists is needed.
Online training or face-to-face training is needed to increase professional dental care knowledge for us.
Cooperation between physicians and dentists is needed to increase dental referral convenience.
Primary Care Related Policy Improvements
We need more time to communicate with parents to improve their dental home care behaviours for their children.
Covering the primary dental care for children, such as fluoride varnish, in the Primary Public Health Care Package would be good for children who live in areas far away from the central city.
Concern about deciduous teeth is not emphasized by some parents. Publicizing dental care knowledge to parents should be implemented more to change their dental misconceptions.
Discussion
The primary finding of this study was that dental screening by paediatric PCPs was well implemented, but CRA and dental referral for high caries-risk children were insufficient during systematic health management in western China. More CRA activities and dental referrals for high caries-risk children were associated with dental knowledge training performed by dental professionals among paediatric PCPs. Considering multidisciplinary cooperation between dental professionals and PCPs is a possible way to increase the CRA and dental referral behaviours of paediatric PCPs.
This study had several limitations. First, the main limitation was the sample representativeness issue of this study. The respondents were selected from the Children Health Academic Association of Sichuan Province, which made the result unable to represent the situation of the whole country because of the vast diversity in China, especially in more developed eastern areas. Second, participant bias was inevitable because we conducted an online survey through the WeChat work group. The persons who do not usually check their WeChat messages may miss the survey. In addition, the respondents who answered the questionnaire were more interested in oral health because they may have done more dental practice. To avoid participant bias, dental care implementation activities by PCPs during health systematic care should be included in the regular administrative monitoring. Depth interviews to key opinion persons may help to provide more information about dental care activities by PCPs. Third, dental practice information was self-reported, which may cause social desirability bias and memory bias.32 This may overestimate dental activities compared to reality. Further studies should evaluate dental implementation’s effectiveness on dental health outcomes of children. The early childhood caries prevention effect should be considered an indicator to evaluate dental care activities by PCPs.
The findings of this study indicated that dental screening was performed more often than CRA and dental referral for high caries-risk children, which is consistent with previous studies. A US study indicated that almost every pediatric provider screened for dental problems; half of them referred in at least half of well-child visits.14 Another US study reported that the average dental referral rate was 40%.33 In this study, five questions were used to measure CRA behaviours. More PCPs asked parents about sugar food intake and milk bottles to sleep, but few PCPs asked about the mother’s caries situation. In addition, the results showed that most PCPs refer children with mild and high caries risk to dentists. These situations may relate to a restriction in dental knowledge among PCPs or an inadequate workforce.34,35 Some updated pediatric dental knowledge is not diffused on time to PCPs. The following analysis proved this hypothesis. We found that the PCPs who implemented more dental practices for high caries-risk children were associated with dental knowledge training by paediatric dental professionals, following previous studies.36,37 Simultaneously, most PCPs mentioned training and cooperation with paediatric dentists according to open-ended questions. Since oral health is always neglected, health policymakers should consider increasing training to help PCPs acquire more oral knowledge so they pay more attention to children’s oral health, conduct more dental screenings, and give corresponding suggestions.
This study expanded the knowledge about the current dental practices of pediatric primary care providers in China. To the best of our knowledge, this was the first study identifying dental implementations by pediatric PCPs at the primary care level in China. Dental health remains a public health challenge and is always neglected worldwide.38 An integrated care approach in primary healthcare settings is a way to provide and maintain universal access to oral healthcare services.39 Many professional academics highlight that collaborations between oral health and medical professionals, along with the promotion of early visits and interventions, contribute to a reduction in ECC.40 Therefore, understanding the gap between PCPs and dentists is important to develop further public health strategies. This study highlights a possible way to prevent ECC by controlling common risk factors through interdisciplinary cooperation in middle- and low-income countries.41 There are many reasons to encourage more CRA and dental referral implementation by paediatric PCPs. First, pediatric PCPs are usually the first health professionals the child meets in early life; they have more chances to monitor children’s dental health regularly and educate parents with targeted advice.42 In China, systematic health management for children aged 0–6 years is an essential component of national primary public health care services.43 The systematic health management for children incorporates regularly monitoring and evaluating children’s overall health status, providing guidance and implementing interventions that can maintain children’s quality of health and assessing influential factors to children’s growth and development. In 2018, 93.6% of children under six years old were covered in systematic health management,24 which means that PCPs could have sustained opportunities to educate parents on the correct dental care at home and identify early caries signals based on CRA. Second, considering the shortage of pediatric dentists and the cost of hiring dentists to work with pediatric PCPs, the dental implementation by PCPs was proven to be a cost-effective feasible strategy for primary preventive dental care.30,44 In China, the density of dentistry personnel (per 1000 population) was approximately 0.129 in 2018, while the WHO standard was 0.2.45 There was a huge gap between the pediatric dentist supply and caries treatment needs. It costs too much to rely solely on dentists to prevent ECC. Notably, there are no standard guidelines for dental screening or CRA for paediatric PCPs, and the selected measurement variables in this study are drawn from the AAPD, which is not the practice guideline for Chinese PCPs. We may set a very high standard to measure PCP behaviours beyond the current requirements, especially for low economic areas. Health policymakers should consider how to eliminate the practical difficulties faced by pediatric PCPs, such as workload, performance evaluation, and dental knowledge limitations, to increase oral examination behaviors.
Conclusions
Compared to dental screening, caries risk assessment activities and dental referrals for high caries-risk children were insufficiently implemented by pediatric PCPs in western China. Health policymakers should consider supplying preventive dental knowledge training for PCPs and encourage interdisciplinary cooperation between PCPs and dental professionals to increase the dental implementation behaviours of paediatric PCPs.
Abbreviations
ECC, Early childhood caries; PCPs, Primary care physicians; CRA, Caries risk assessment; AAPD, American Academy of Pediatric Dentistry.
Data Sharing Statement
The datasets used during the current study are available from the corresponding author on reasonable request.
Acknowledgment
We are particularly grateful for the professional comments from Dr. Jay Pan, who works in the public health school of Sichuan University, China.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the National Natural Science Foundation of China (No. 71904136) and the National Social Science Fund of China (Grant No. 21ZDA104). The funding organizations had no role in the study design, implementation, analysis or interpretation of the data.
Disclosure
The authors declare that they have no conflicts of interest in relation to this work.
References
1. Tinanoff N, Baez RJ, Diaz Guillory C, et al. Early childhood caries epidemiology, aetiology, risk assessment, societal burden, management, education, and policy: global perspective. Int j Paediatric Dentistry. 2019;29(3):238–248. doi:10.1111/ipd.12484
2. Phantumvanit P, Makino Y, Ogawa H, et al. WHO Global Consultation on Public Health Intervention against Early Childhood Caries. Community Dent Oral Epidemiol. 2018;46(3):280–287. doi:10.1111/cdoe.12362
3. China NHCotPsRo. The Report of the Fourth National Oral Health Survey. China NHCotPsRo; 2017.
4. Martins-Junior PA, Vieira-Andrade RG, Correa-Faria P, Oliveira-Ferreira F, Marques LS, Ramos-Jorge ML. Impact of early childhood caries on the oral health-related quality of life of preschool children and their parents. Caries Res. 2013;47(3):211–218. doi:10.1159/000345534
5. Zhang Q, Ma Q, Wang Y, Wu H, Zou J. Molecular mechanisms of inhibiting glucosyltransferases for biofilm formation in Streptococcus mutans. Int J Oral Sci. 2021;13(1):30. doi:10.1038/s41368-021-00137-1
6. Anil S, Anand PS. Early Childhood Caries: prevalence, Risk Factors, and Prevention. Frontiers in Pediatrics. 2017;5:157. doi:10.3389/fped.2017.00157
7. Vamos CA, Thompson EL, Avendano M, Daley EM, Quinonez RB, Boggess K. Oral health promotion interventions during pregnancy: a systematic review. Community Dent Oral Epidemiol. 2015;43(5):385–396. doi:10.1111/cdoe.12167
8. Jiang EM, Lo ECM, Chu CH, Wong MCM. Prevention of early childhood caries (ECC) through parental toothbrushing training and fluoride varnish application: a 24-month randomized controlled trial. J Dent. 2014;42(12):1543–1550. doi:10.1016/j.jdent.2014.10.002
9. Naidu RS, Nunn JH, Pahel B, Niederman R. Editorial: promoting Oral Health in Early Childhood: the Role of the Family, Community and Health System in Developing Strategies for Prevention and Management of ECC. Front Public Health. 2021;9:716695. doi:10.3389/fpubh.2021.716695
10. WHO. Strategies and approaches in oral disease prevention and health promotion. Site; 2013. Available from: http://wwwwhoint/oral_health/strategies/cont/en/.
11. Kidd JBR, McMahon AD, Sherriff A, et al. Evaluation of a national complex oral health improvement programme: a population data linkage cohort study in Scotland. BMJ open. 2020;10(11):e038116. doi:10.1136/bmjopen-2020-038116
12. Chai HH, Gao SS, Chen KJ, et al. Health Preventive Approach for Hong Kong Preschool Children. Healthcare. 2020;8(4):545.
13. Gauger TL, Prosser LA, Fontana M, Polverini PJ. Integrative and collaborative care models between pediatric oral health and primary care providers: a scoping review of the literature. J Public Health Dent. 2018;78(3):246–256. doi:10.1111/jphd.12267
14. Do LG, Scott JA, Thomson WM, et al. Common risk factor approach to address socioeconomic inequality in the oral health of preschool children - a prospective cohort study. BMC Public Health. 2014;14:14. doi:10.1186/1471-2458-14-14
15. Zhu Y, Close K, Zeldin LP, White BA, Rozier RG. Implementation of Oral Health Screening and Referral Guidelines in Primary Health Care. JDR Clin Translational Res. 2018;4(2):167–177. doi:10.1177/2380084418810332
16. Close K, Rozier RG, Zeldin LP, Gilbert AR. Barriers to the Adoption and Implementation of Preventive Dental Services in Primary Medical Care. Pediatrics. 2010;125(3):509. doi:10.1542/peds.2009-1008
17. Chinese National Bureau of Statistics. Statistical year book of China, 2019; 2020. Available from: http://www.stats.gov.cn/tjsj/ndsj/2020/indexch.htm.
18. Daily CHINA DEVELOPS ITS SWEET TOOTH; 2019. Available from: http://www.chinadaily.com.cn/global/2019-07/15/content_37491419.htm.
19. Kong LZ. China’s Medium-to-Long Term Plan for the Prevention and Treatment of Chronic Diseases (2017-2025) under the Healthy China Initiative. Chronic Dis Transl Med. 2017;3(3):135–137. doi:10.1016/j.cdtm.2017.06.004
20. National Health Commitment of China. Healthy oral action program (2019-2025); 2019. Available from: http://www.gov.cn/xinwen/2019-02/16/content_5366239.htm.
21. CDC C. National Children’s Oral Disease Comprehensive Intervention Project Work Specifications; 2014. Available from: https://www.chinacdc.cn/zxdt/201403/t20140321_94580.html.
22. Sun X, Bernabé E, Liu X, Zheng S, Gallagher JE. Meeting the oral health needs of 12-year-olds in China: human resources for oral health. BMC Public Health. 2017;17(1):586. doi:10.1186/s12889-017-4384-7
23. National Health Commitment of China. National Standard for Basic Public Health Services.
24. Chinese National Bureau of Statistics. 2018 Statistical Monitoring Report on the Implementation of China National Program for Child Development (2011–2020); 2020. Available from: http://www.stats.gov.cn/english/PressRelease/202001/t20200103_1721247.html.
25. Montag C, Becker B, Gan C. The Multipurpose Application WeChat: a Review on Recent Research. Front psychol. 2018;9:2247. doi:10.3389/fpsyg.2018.02247
26. Johnson TP. Snowball Sampling: Introduction. Wiley StatsRef: Statistics Reference Online. 2018.
27. Health Commitment of Sichuan Province, China. Statistical Year Book 2018. Available from: http://wsjkw.sc.gov.cn/scwsjkw/njgb/2021/3/15/5dc2167777c54a8a931396c3d9b6c715/files/fec87923dac44f3a8aa5899d29ef4923.pdf.
28. Council O. Guideline on Caries-risk Assessment and Management for Infants, Children, and Adolescents. Pediatr Dent. 2016;38(6):142–149.
29. Grimm P. Social Desirability Bias. Wiley International Encyclopedia of Marketing; 2010.
30. AAPD. Policy on the Dental Home. Pediatr Dent. 2018;40(6):29–30.
31. Dela Cruz GG, Rozier RG, Slade G. Dental screening and referral of young children by pediatric primary care providers. Pediatrics. 2004;114(5):e642–652. doi:10.1542/peds.2004-1269
32. Larson RB. Controlling social desirability bias. International Journal of Market Research. 2019;61(5):534-547. doi:10.1177/1470785318805305
33. Zhu Y, Close K, Zeldin L, Quinonez RB, White BA, Rozier RG; Zhu Y, Close K, Zeldin L, Quinonez RB, White BA, Rozier RG. A Clinical Vignette-Based. Study of Physicians’ Check for Adherence to Guidelines for Dental Referrals of Young Children. Acad Pediatr. 2019;19(2):195–202.
34. Zhu Y, Close K, Zeldin L, Quinonez RB, White BA, Rozier RG; Zhu Y, Close K, Zeldin L, Quinonez RB, White BA, Rozier RG. A Clinical Vignette–Based. Study of Physicians’ Adherence to Guidelines for Dental Referrals of Young Children. Acad Pediatr. 2019;19(2):195–202. doi:10.1016/j.acap.2018.05.013
35. Dickson-Swift V, Kenny A, Gussy M, McCarthy C, Bracksley-O’Grady S. The knowledge and practice of pediatricians in children’s oral health: a scoping review. BMC Oral Health. 2020;20(1):211. doi:10.1186/s12903-020-01198-0
36. Herndon JB, Tomar SL, Catalanotto FA. Effect of Training Pediatricians and Family Physicians in Early Childhood Caries Prevention. J Pediatr. 2015;166(4):1055–1061.e1051. doi:10.1016/j.jpeds.2014.12.040
37. Alshunaiber R, Alzaid H, Meaigel S, Aldeeri A, Adlan A. Early childhood caries and infant’s oral health; pediatricians’ and family physicians’ practice, knowledge and attitude in Riyadh city, Saudi Arabia. Saudi Dental J. 2019;31:S96–S105. doi:10.1016/j.sdentj.2019.01.006
38. Peres MA, Macpherson LMD, Weyant RJ, et al. Oral diseases: a global public health challenge. Lancet. 2019;394(10194):249–260. doi:10.1016/S0140-6736(19)31146-8
39. Harnagea H, Couturier Y, Shrivastava R, et al. Barriers and facilitators in the integration of oral health into primary care: a scoping review. BMJ open. 2017;7(9):e016078. doi:10.1136/bmjopen-2017-016078
40. Health NIo. Oral Health in America: Advances and Challenges. Health NIo; 2021.
41. Watt RG, Sheiham A. Integrating the common risk factor approach into a social determinants framework. Community Dent Oral Epidemiol. 2012;40(4):289–296. doi:10.1111/j.1600-0528.2012.00680.x
42. Wigen TI, Wang NJ. Referral of young children to dental personnel by primary care nurses. Int J Dent Hyg. 2017;15(3):249–255. doi:10.1111/idh.12238
43. Mao P, Feng H, Xu S, et al. Well-child care delivery in the community in China: related factors and quality analysis of services. PLoS One. 2018;13(1):e0190396. doi:10.1371/journal.pone.0190396
44. Domejean S, Banerjee A, Featherstone JDB. Caries risk/susceptibility assessment: its value in minimum intervention oral healthcare. Br Dent J. 2017;223(3):191–197. doi:10.1038/sj.bdj.2017.665
45. Sun XY, Yuan C, Wang XZ, et al. Report of the National Investigation of Resources for Oral Health in China. Chinese j Dental Res. 2018;21(4):285–297. doi:10.3290/j.cjdr.a41087
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
