Back to Journals » Neuropsychiatric Disease and Treatment » Volume 10
Caregiver burden and coping strategies in caregivers of patients with Alzheimer’s disease
Authors Iavarone A, Ziello A, Pastore F, Fasanaro AM, Poderico C
Received 22 November 2013
Accepted for publication 10 March 2014
Published 29 July 2014 Volume 2014:10 Pages 1407—1413
DOI https://doi.org/10.2147/NDT.S58063
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Alessandro Iavarone,1,2 Antonio Rosario Ziello,3,4 Francesca Pastore,3 Angiola Maria Fasanaro,3 Carla Poderico5
1Neurological and Stroke Unit, CTO Hospital, 2Italian Association on Alzheimer's Disease (AIMA), 3Memory Clinic, Neurological Unit, AORN Cardarelli Hospital, Naples, Italy; 4Clinical Research, Telemedicine and Telepharmacy Centre, University of Camerino, Camerino, Italy; 5Department of Psychology, Second University of Naples, Caserta, Italy
Background: Alzheimer’s disease (AD) causes considerable distress in caregivers who are continuously required to deal with requests from patients. Coping strategies play a fundamental role in modulating the psychologic impact of the disease, although their role is still debated. The present study aims to evaluate the burden and anxiety experienced by caregivers, the effectiveness of adopted coping strategies, and their relationships with burden
and anxiety.
Methods: Eighty-six caregivers received the Caregiver Burden Inventory (CBI) and the State-Trait Anxiety Inventory (STAI Y-1 and Y-2). The coping strategies were assessed by means of the Coping Inventory for Stressful Situations (CISS), according to the model proposed by Endler and Parker in 1990.
Results: The CBI scores (overall and single sections) were extremely high and correlated with dementia severity. Women, as well as older caregivers, showed higher scores. The trait anxiety (STAI-Y-2) correlated with the CBI overall score. The CISS showed that caregivers mainly adopted task-focused strategies. Women mainly adopted emotion-focused strategies and this style was related to a higher level of distress.
Conclusion: AD is associated with high distress among caregivers. The burden strongly correlates with dementia severity and is higher in women and in elderly subjects. Chronic anxiety affects caregivers who mainly rely on emotion-oriented coping strategies. The findings suggest providing support to families of patients with AD through tailored strategies aimed to reshape the dysfunctional coping styles.
Keywords: Alzheimer’s disease, distress, caregiver burden, stress, coping strategies
Introduction
The growing number of aged people in Western countries carries with it an increase in age-related disorders. Among these, Alzheimer’s disease (AD) is the most serious because of its epidemiologic, economic, and social impact. For instance, in Italy, families are the main source of care, providing daily assistance to persons with dementia. Data from the Italian Statistical Institute1 report that the majority of patients with dementia (80%) live at home, where informal care (unpaid and not professionally trained) is given in about 70% of cases by female relatives, whose burden and stress become heavier as the disease progresses.
Within the family context, the challenges faced by caregivers contribute heavily to the psychologic, physical, and financial burden.2 In caregivers, this is often associated with clinically significant anxiety (10%–35%) and depression (10%–34%).3 The role of chronic distress may also contribute to worsening the physical health status of caregivers, by increasing their vulnerability to develop diseases and reducing life expectancy itself.4,5 These findings are also confirmed by data from a study of a large sample of US caregivers,6 which indicate a high prevalence of hypertension among caregivers, associated with an increased risk of cardiovascular disease.
The caregiver’s condition should be seen as a paradigm of the “general adaptation syndrome”.7 In this framework, stress may be viewed as a general and nonspecific biological response of the whole body. This response appears when requests from the environment exceed the subject’s resources. In this perspective, a great deal of attention has been given to the study of coping strategies adopted by the subject when having to face distressing situations.8–11 Coping may be defined as a process of adaptation to stressful situations, which includes the allocation of cognitive and behavioral resources in response to specific internal and/or external demands that are deemed to exceed the subject’s normal requests.12 Although there is some disagreement about how coping strategies may be categorized,10 coping may be classified into three broad main types, ie, task-focused, emotion-focused, and avoidance-focused strategies.9,13
Task-focused coping seeks to actively perform a task that will remove the problem or make the problem better; typically, if the frequency of task-focused coping increases, the distress decreases.13,14 Emotion-focused coping seeks to regulate distressing emotions and can include emotional expression, fantasizing, and reflecting on positive or negative thoughts.15 Avoidance-focused coping involves avoiding the adverse situation, and includes social diversion.14 Several studies have shown that emotion-focused and avoidance-focused coping strategies may be dysfunctional, since they divert from understanding or managing requests, with the consequence of increased physiologic and psychologic distress.9,14–16
As far as the role of coping strategies in AD caregivers is concerned, some studies have highlighted the role of effective coping in reinforcing cohesion and improving relationships within the family context.17–20 Other studies have pointed out the negative impact of caregiving on health status and psychologic conditions.11,21–23 It has also been shown that in AD caregivers there is an association between coping styles and stress levels.10,11,24,25 In particular, dysfunctional coping, mainly underlying avoidance strategies, would be associated with the development of burnout and high levels of sadness. On the other hand, effective and adaptive coping strategies may play a protective role in reducing the caregiver’s distress.26 These findings receive further support from other studies showing that an approach based upon task-focused strategies may help to reduce physiologic stress.27 Finally, a longitudinal study reported that emotion-focused coping strategies could prevent the development of high levels of anxiety11 and depression.28,29
The aim of the present study is to describe the relationships between psychologic distress and coping strategies adopted by a group of caregivers of persons with AD. To this end, we evaluated the burden and anxiety experienced by caregivers, the relationship between distress and sociodemographic and clinical variables, the type and effectiveness of the coping strategies adopted by caregivers, and the relationships between coping strategies and both burden and anxiety.
Materials and methods
Participants
The study involved a sample of 86 caregivers of corresponding patients with AD (National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association [NINCDS-ADRDA] criteria),30 seen consecutively at the Memory Clinic of the Neurological Unit of AORN Cardarelli Hospital in Naples. Inclusion criteria were being a relative of the patient and having constant, daily contact with the patient. Conversely, persons not fulfilling such criteria, namely professional caregivers, were not considered for inclusion in the study. All subjects gave their informed consent to the study, which was carried out according to the Declaration of Helsinki and approved by the local ethics committee.
Assessment tools
Autonomy in activities of daily living in all the patients was assessed using the Barthel Index.31 The Barthel Index is a 10-item self-report and the total possible score ranges from 0 to 100, with lower scores indicating increased disability.31 All caregivers underwent a semistructured interview, the aim of which was to evaluate burden and anxiety by means of the Caregiver Burden Inventory (CBI)32 and the State-Trait Anxiety Inventory (STAI Y-1 and Y-2).33 Coping strategies were evaluated by the Coping Inventory for Stressful Situations (CISS).34
The CBI consists of five sections evaluating the impact of caregiving on the caregiver: time-dependence burden, which gives a measure of flexibility with time and caregiver’s time restriction; developmental burden, which evaluates the impact of failing to catch opportunities and pursue goals; physical burden, a measure of the physical consequences of caregiving (eg, fatigue and somatic complaints); social burden, which assesses the impact on interpersonal and social relationships within the family and working environment; and emotional burden, which evaluates feelings of shame and embarrassment with respect to the patient. Each dimension consists of five items, and the score for each item ranges from 0 (factor with a minimum value) to 4 (factor with a maximum value), giving a total that ranges from 0 to 20 for each dimension with the exception of the physical burden, which has four items and a correction factor of 1.25 must be applied. The total score ranges from 0 to 100, and the scores grow proportional to the severity of the problem perceived by the caregiver.32
The STAI is a validated tool to evaluate anxiety. It includes two dimensions, ie, state anxiety (Y-1), which evaluates the emotional state of an individual in a particular situation, and trait anxiety (Y-2), which refers to a relatively stable characteristic of personality. It is based on a 4-point Likert scale and consists of 40 questions on a self-report basis. The total score of each dimension ranges from 20 to 80, but the significant scores are equal or greater to the 95th percentile.33
The CISS is a 48-item self-report and has been developed to describe cognitive styles and behavioral resources in response to a specific stressor. It assesses three coping strategies: task-oriented coping (16 items), which refers to purposeful efforts aimed at solving and/or restructuring the problem in an attempt to improve the situation; emotion-oriented coping (16 items), which refers to self-oriented reactions including emotional responses, self-preoccupation, and fantasizing; and avoidance-oriented coping (16 items), which refers to activities and cognitive changes aimed at avoiding the stressful situation by distracting oneself with other situations or tasks, or via social diversion as a means of alleviating stress. Each item ranges from 1 to 5 (1 rates as “not at all” and 5 rates as “very much”). Subjects are asked to think about a variety of stressful and upsetting situations and the rating scales are used to indicate how often the respondent engages in the behaviors presented, which is how the range of 1–5 is used. The total score for each dimension ranges from 16 to 80.34
Data analysis
Descriptive statistics were used to summarize variables. Within each group, comparison on the CBI and CISS was evaluated by Friedman’s analysis of variance with the post hoc (Nemenyi) test. The effects of independent variables such as age, sex, and family ties on CBI and CISS scores were checked by means of multiple regression analyses, with the significance level corrected by the number of independent variables. Correlation analyses were performed using a partial correlation matrix with significance level corrected by the number of comparisons. The dimensions of burden in their relationships with coping strategies were explored by means of a factor analysis. Computation was supported by the statistical packages StatView 5.0 and MedCalc 12.7, running on PC.
Results
The sample of 86 caregivers included 37 men and 49 women, with a mean age of 57.5±12.3 years and a mean education (years of schooling) of 12.0±4.3. The family ties of caregivers were: spouse in 37, offspring in 39, and other in the remaining ten persons. The 86 subjects with dementia consisted of 34 men and 52 women with a mean age of 72.6±8.15 years. According to the Clinical Dementia Rating,35 the staging of dementia was mild in eleven, moderate in 29, moderately severe in 29, and severe in the remaining eleven subjects. The mean duration of disease was 4.01±2.12 years. The mean Barthel Index score was 66.33±26.67. The mean CBI overall score for caregivers was 37.05±20.37.
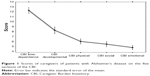
Friedman’s analysis of variance on the five CBI sections was significant [F(4.34)=45.611; P<0.00001]. Post hoc analysis showed time dependence scores to be significantly higher than those of all the remaining sections. Developmental scores were higher than those of physical, social, and emotional; no difference approached significance within these last sections (see Figure 1).
The multiple regression analysis assuming CBI overall scores versus three independents (age, sex, and family tie of caregivers) was significant [F(3.82)=7.488; P=0.0002], and showed the effect of sex (P=0.0044) and age (P=0.0027), thus indicating that a heavier global burden weighs on women and older caregivers. The type of family tie was not significant. Using the same procedure, the effects of the independent variables were evaluated for each of the five sections of the CBI (see Table 1).
The developmental burden mainly affected women, whereas the time dependence burden was related to older age of the caregivers. Further, both physical burden and emotional burden were heavier in women and older caregivers. None of the CBI sections was influenced by the type of family tie.
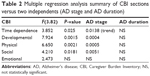
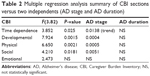
The effect of the severity of dementia and duration of illness on overall CBI scores was checked by multiple regression analysis. The regression model was significant [F(2.82)=7.616; P=0.0009], but this was only due to the influence of dementia severity (P=0.0003). The same section-by-section analyses confirmed that the duration of disease was not always significant, whereas severity of dementia affected almost all the CBI sections (see Table 2).
The mean STAI Y-1 score was 44.53±7.48, and quite similar to that of STAI Y-2 (44.75±7.08). No effect of demographic variables (age, sex, or family tie) or of clinical aspects of dementia (staging and duration) was observed on either STAI Y-1 or Y-2 scores (multiple regression analyses). A significant correlation was observed only between trait anxiety (STAI Y-2) and overall CBI scores (r=0.529; P<0.0001). Among the CBI sections, strong correlations were observed between STAI Y-2 and developmental (r=0.488; P<0.0001), physical (r=0.589; P<0.0001), and social (r=0.440; P<0.0001) burden.
Friedman’s analysis of variance on the three CISS sections was significant [F(2.17)=44.287; P<0.00001]. Post hoc analysis showed task-focused scores were significantly higher than those for emotion-focused and avoidance-focused strategies, whereas no difference was observed in the last two sections (see Figure 2).
The effects of age, sex, and type of family tie on the three CISS sections were evaluated by multiple regression analyses; these revealed that some caregivers had higher task-focused scores, whereas emotion-focused scores were higher in female caregivers (Table 3). A similar procedure was conducted to evaluate the effect on CISS sections of the stage of dementia and duration of illness. The regression model [F(2.82)=3.487; P=0.036] was significant only for emotion-focused scores, which were influenced by dementia severity (P=0.011). Correlation analysis turned out to be significant only between emotion-focused and overall CBI scores (r=0.618; P<0.0001). Finally, no correlation approached significance between CISS sections and anxiety measures, with the exception of emotion-focused, which correlated with STAI Y-2 (r=0.563; P<0.0001).
The five scores of CBI were entered, together with scores of the CISS, in a principal component analysis with varimax rotation (method of extraction: roots >1). The principal component analysis had a Bartlett’s chi-square value of 306.213 (P<0.0001). The analysis generated two factors that explained about 63% of the variance. The factorial matrix after rotation showed that factor 1 loaded on all CBI items plus the emotion-focused. Factor 2 loaded on task-focused and avoidance-focused scores (Table 4).
Discussion
The aim of this study was to contribute to giving a picture of the caregiving phenomenon of persons with AD. In particular, we intended to better define the relationships between the characteristics of caregivers’ distress (burden and anxiety) and the types of coping strategies adopted in facing the disease on a daily basis. In our sample, the majority of caregivers were women, without significant differences between the number of spouses and sons. This is consistent with findings already reported in the literature.36,37
A first result is that the global burden in our sample is extremely high when compared with those reported in other studies.25,38 Among the burden dimensions, time dependence seems to be the more important. Further, AD caregivers experience feelings of failure about their personal expectations and opportunities typical of the phase of life they are living (developmental burden). On the other hand, relatively little impact comes from negative feelings toward the patient and their illness (emotional burden). These results are consistent with data from Italian surveys carried out using the same burden assessment tool.25,39
The global burden was shown to be heavier in women and older caregivers of AD patients. However, a more analytical evaluation highlights that time dependence and physical burden are greater in older caregivers, whereas developmental and emotional burden predominate in women caregivers. This suggests that women probably organize the time they devote to caregiving better, but this carries with it a negative impact on the emotional dimension and lifestyle. Further, the lack of any effect of the type of family tie is consistent with the view that the burden is heavily perceived by relatives regardless of the role they play inside the family group.
In AD caregivers, the burden was highly influenced by the severity of dementia, both overall and in most of the CBI sections. A similar effect was not observed for disease duration. The last finding may be somewhat unexpected, given the parallelism usually reported between duration and grading of dementia. A possible interpretation of this discrepancy is that the severity of dementia, independent of the time it takes to reach a given stage, plays the main role in determining the burden. Further, the influence of severity of dementia on burden seems to preserve the emotional dimension, thus suggesting that negative feelings toward the patient do not belong to the typical profile of an AD caregiver.
The AD caregiver burden correlated strongly with trait (but not state) anxiety symptoms. A possible interpretation is that trait anxiety is a risk factor that leads to a greater burden for the caregiver. However, such an interpretation is less plausible if we consider the lack of any correlation between anxiety and emotional burden and, conversely, the strong correlations with developmental, physical, and social burden. Consequently, a more plausible interpretation would be that the burden induces stable anxiety in caregivers which, in turn, amplifies the perceived burden.40,41
Interesting data come from an evaluation of coping strategies. The AD caregivers exhibit strategies that are mainly task-focused; they seem to be more prone to “go toward” the patient, both in the behavioral and emotional sense. This finding is consistent with previous studies,11,25 in which caregivers preferred to actively perform tasks in response to persistent requests.
Emotion-focused strategies are clearly influenced by sex, because they are mainly adopted by women, and strongly related to burden, trait anxiety and, to a lesser extent, dementia severity. Taken together, these results point to female caregivers who are required by cultural context to play the role of “persons who take care”.42 The same role is not usually played by men, with the result that they receive more endorsement by the community. Conversely, women often have to pay the cost in terms of their unfulfilled expectations, which implies their physical and psychologic resources become exhausted.43,44
The factorial matrix after rotation showed that factor 1 loaded on all CBI items plus the CISS emotion. This finding indicates that the reliance on emotion-focused strategies leads caregivers to higher level of distress, whereas successful caregiving seems related to task-focused and avoidance-focused strategies. Although many studies point to task-focused strategies as a positive attitude,20,25,45 the effectiveness of avoidance behaviors is still unclear.20,46 Several reasons may account for these discrepancies, eg, the numerosity and characteristics of both patients and caregivers and the setting of patients (ie, hospital, rehabilitation ward, outpatients). Further, a potent source of distortion could stem from the type of tools adopted to assess coping strategies, since many of these instruments do not specifically address problems of caregivers of patients with dementia. Finally, an agreement about the classification of coping strategies is still lacking.10
On the whole, our data confirm that dysfunctional strategies, without acceptance-based coping styles, are associated with anxiety and depression.40 From the clinical standpoint, the results of our study would encourage paying attention to caregiver burden, distress, and coping strategies and to consider their assessment, by means of validated tools, as part of diagnostic procedures.
From the clinical management point of view, our results would support the development of psychologic interventions for carers with a view to modifying coping styles. These interventions should be carried out from the perspective of cognitive reframing for family carers of persons with dementia, in order to reduce psychologic morbidity and subjective stress.47
Our study is not free from criticism. One limitation is the lack of assessment of behavioral and psychologic symptoms associated with dementia, given their role in determining caregivers’ burden and distress. However, in contrast with other forms of dementia, such as frontotemporal lobe degeneration, the behavioral and psychologic symptoms associated with dementia in AD are not by definition core symptoms of the disease, nor are they included in the criteria for diagnosis. Further limitations ensue from the relatively small size of the sample, as well as the cross-sectional nature of the study. Because of these limitations, precise causal mechanisms between burden and coping strategies or vice versa cannot be established, although it is worth highlighting that the relationship between burden and coping is indeed bidirectional.
Conclusion
Our data confirm that the main caregiver of the AD patient is more often a woman, usually the wife or the daughter of the ill person. Taking on this role of caregiver carries with it an increasing burden, in particular in developmental and physical dimensions. The time restriction experienced by relatives, along with the loss of many opportunities, are the aspects most commonly and strongly perceived. The coping strategy adopted by the female caregiver tends to be emotion-focused. These types of strategies seem to predispose the caregiver to a higher burden and distress. AD caregiving is associated with negative effects, and an increase in burden is associated with a higher increase in assistance. This confirms the data in the literature indicating that these individuals are physically, emotionally, and financially overwhelmed by their role. This burden, however, could be lessened if interventions tailored to caregivers were provided and then adopted, with a view to reshaping each specific dysfunctional cognitive style in the caregiver.
Disclosure
The authors report no conflicts of interest in this work.
References
La mortalità per demenze e morbo d’Alzheimer. [The mortality rate in dementia and Alzheimer's disease]. Available from: http://www.serveneto.it/public/File/documents/rapporti/rapportomortalita0007/07_DemenzeAlzheimer.pdf. Accessed December 10, 2012. | ||
Jonker L, Greef AP. Resilience factors in families living with people with mental illnesses. J Community Psychol. 2009;37:859–873. | ||
Cooper C, Balamurali T, Livingston G. A systematic review of the prevalence and associates of anxiety in caregivers of people with dementia. Int Psychogeriatr. 2007;19:175–195. | ||
Kannan H, Bolge SC, Del Valle M, Alvir J, Petrie CD. The association between Alzheimer’s disease symptom severity and caregiver outcomes: a cross-sectional study. Prim Care Companion CNS Disord. 2011:13(3). | ||
Von Känel R, Dimsdale JE, Patterson TL, Grant I. Association of negative life event stress with coagulation activity in elderly Alzheimer caregivers. Psychosom Med. 2003;65:145–150. | ||
Aschbacher K, von Känel R, Dimsdale JE, et al. Dementia severity of the care receiver predicts procoagulant response in Alzheimer caregivers. Am J Geriatr Psychiatry. 2006;14:694–703. | ||
Selye H. The stress concept. Can Med Assoc J. 1976;115:717–718. | ||
Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York, NY, USA: Springer; 1984. | ||
Endler NS, Parker JD. Multidimensional assessment of coping: a critical evaluation. J Pers Soc Psychol. 1990;58:844–854. | ||
Powers DV, Gallagher-Thompson D, Kraemer HC. Coping and depression in Alzheimer’s caregivers: longitudinal evidence of stability. J Gerontol B Psychol Sci Soc Sci. 2002;57:205–211. | ||
Cooper C, Katona C, Orrell M, Livingston G. Coping strategies, anxiety and depression in caregivers of people with Alzheimer’s disease. Int J Geriatr Psychiatry. 2008;23:929–936. | ||
Folkman S, Lazarus RS. An analysis of coping in a middle aged community sample. J Health Soc Behav. 1980;21:219–239. | ||
Folkman S, Lazarus RS. If it changes it must be a process: study of emotional coping during three stages of a college examination. J Pers Soc Psychol. 1985;48:150–170. | ||
Higgins JE, Endler NS. Coping, life stress, and psychological and somatic distress. Eur J Pers. 1995;9:253–270. | ||
Bauman EM, Haaga DA, Dutton MA. Coping with intimate partner violence: battered women’s use and perceived helpfulness of emotion-focused coping strategies. J Aggress Maltreat Trauma. 2008;17:23–41. | ||
Thompson SN. Coping styles of African American youth living in poverty: understanding the role of coping in resiliency. College of Liberal Arts and Social Sciences Theses and Dissertations. Available from: http://via.library.depaul.edu/cgi/viewcontent.cgi?article=1002&context=etd. Accessed May 21, 2014. | ||
Beach SR, Shulz R, Yee JL, Jackson S. Negative and positive health effects of caring for a disabled spouse: longitudinal findings from the caregiver health effects study. Psychol Aging. 2000;15:259–271. | ||
Cohen CA, Colantonio A, Vermich L. Positive aspects of caregiving: rounding out the caregiver experience. Int J Geriatr Psychiatry. 2002;17:184–188. | ||
Bayat M. Evidence of resilience in families of children with autism. J Intellect Disabil Res. 2007;51:702–714. | ||
Wilks SE, Croom B. Perceived stress and resilience in Alzheimer’s disease caregivers: testing moderation and mediation models of social support. Aging Ment Health. 2008;12:357–365. | ||
Butcher HK, Holkup PA, Buckwalter KC. The experience of caring for a family member with Alzheimer’s disease. West J Nurs Res. 2001;23: 33–55. | ||
Ekwall AK, Sivberg B, Hallberg IR. Older caregivers’ coping strategies and sense of coherence in relation to quality of life. J Adv Nurs. 2007;57:584–596. | ||
Alzheimer’s Association. 2010 Alzheimer’s disease facts and figures. Available from: http://www.alz.org/alzheimers_disease_facts_figures.asp. Accessed August 4, 2013. | ||
García-Alberca JM, Cruz B, Lara JP, Garrido V, Lara A, Gris E. Anxiety and depression are associated with coping strategies in caregivers of Alzheimer’s disease patients: results from the MÁLAGA-AD study. Int Psychogeriatr. 2012;24:1325–1334. | ||
Zucchella C, Bartolo M, Pasotti C, Chiapella L, Sinforiani E. Caregiver burden and coping in early-stage Alzheimer disease. Alzheimer Dis Assoc Disord. 2012;26:55–60. | ||
Gardinali A, Campanili E, Prunai A, Regonesi MG, Cappa S. Progetto di intervento per lo studio dello stress e del coping nei familiari di pazienti affetti da demenza: Indagine preliminare sulle proprietà psicometriche del “Caregiver Burden Inventory” (CBI). Fondazione Benefattori Cremaschi ONLUS, A.I.M.A. Crema; Università Vita Salute San Raffaele, Dipartimento di Psicologia della Salute; Università degli Studi di Milano Bicocca, Dipartimento di Psicologia; Università Vita Salute San Raffaele, Dipartimento di Neurologia; 2008:56–72. | ||
Aschbacher K, Patterson TL, von Känel R, et al. Coping processes and hemostatic reactivity to acute stress in dementia caregivers. Psychosom Med. 2005;67:964–971. | ||
Fingerman KL, Gallagher-Thompson D, Lovett S, Rose J. Internal resourcefulness, task, demands, coping, and dysphoric affect among caregivers of the frail elderly. Int J Aging Hum Dev. 1996;42: 229–248. | ||
Williamson GM, Schulz R. Coping with specific stressors in Alzheimer’s disease caregiving. Gerontologist. 1993;33:747–755. | ||
McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34:939–944. | ||
Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J. 1965;14:61–65. | ||
Novak M, Guest C. Application of a multidimensional caregiver burden inventory. Gerontologist. 1989;29:798–803. | ||
Spielberger CD. S.T.A.I. (State-Trait-Anxiety Inventory). Inventario per l’ansia di stato e di tratto. Forma Y. Organizzazioni Speciali, Firenze. 1989:9–22. | ||
Endler NS, Parker JD. Multidimensional assessment of coping: a critical evaluation. J Pers Soc Psychol. 1990;58:844–854. | ||
Berg L. Clinical Dementia Rating (CDR). Br J Psychiatry. 1984; 145:339. | ||
Ducharme F, Lévesque L, Lachance L, Kergoat MJ, Coulombe R. Challenges associated with transition to caregiver role following diagnostic disclosure of Alzheimer disease: a descriptive study. Int J Nurs Stud. 2011;48:1109–1119. | ||
Gelman CR, Greer C. Young children in early-onset Alzheimer’s disease families: research gaps and emerging service needs. Am J Alzheimers Dis Other Demen. 2011;26:29–35. | ||
Akpinar B, Küçükgüçlü O, Yener G. Effects of gender on burden among caregivers of Alzheimer’s patients. J Nurs Scholarsh. 2011;43: 248–254. | ||
Carbone G, Barreca F, Mancini G, et al. A home assistance model for dementia: outcome in patients with mild-to-moderate Alzheimer’s disease after three months. Ann Ist Super Sanita. 2013;49:34–41. | ||
Li R, Cooper C, Bradley J, Shulman A, Livingston G. Coping strategies and psychological morbidity in family carers of people with dementia: a systematic review and meta-analysis. J Affect Disord. 2012;139: 1–11. | ||
Li R, Cooper C, Austin A, Livingston G. Do changes in coping style explain the effectiveness of interventions for psychological morbidity in family carers of people with dementia? A systematic review and meta-analysis. Int Psychogeriatr. 2013;25:204–214. | ||
Rinaldi P, Spazzafumo L, Mastriforti R, et al. Predictors of high level of burden and distress in caregivers of demented patients: results of an Italian multicenter study. Int J Geriatr Psychiatr. 2005;2:168–174. | ||
Rose-Rego SK, Strauss ME, Smyth KA. Differences in the perceived well-being of wives and husbands caring for persons with Alzheimer’s disease. Gerontologist. 1998;38:224–230. | ||
Hooker K, Manoogian-O’Dell M, Monahan DJ, Frazier LD, Shifren K. Does type of disease matter? Gender differences among Alzheimer’s and Parkinson’s disease spouse caregivers. Gerontologist. 2000;40:568–573. | ||
Kneebone II, Martin PR. Coping and caregivers of people with dementia. Br J Health Psychol. 2003;8:1–17. | ||
Mausbach BT, Aschbacher K, Patterson TL, et al. Avoidant coping partially mediates the relationship between patient problem behaviors and depressive symptoms in spousal Alzheimer caregivers. Am J Geriatr Psychiatry. 2006;14:299–306. | ||
Vernooij-Dassen M, Draskovic I, McCleery J, Downs M. Cognitive reframing for carers of people with dementia. Cochrane Database Syst Rev. 2011;9:CD005318. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.